ABSTRACT
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) as the name suggests was initially thought to only cause a respiratory illness. However, several reports have been published of patients with ischemic strokes in the setting of coronavirus disease 2019 (COVID‐19). The mechanisms of how SARS‐CoV‐2 results in blood clots and large vessel strokes need to be defined as it has therapeutic implications. SARS‐CoV‐2 enters the blood stream by breaching the blood‐air barrier via the lung capillary adjacent to the alveolus, and then attaches to the angiotensin‐converting enzyme II receptors on the endothelial cells. Once SARS‐CoV‐2 enters the blood stream, a cascade of events (Steps 1‐8) unfolds including accumulation of angiotensin II, reactive oxygen species, endothelial dysfunction, oxidation of beta 2 glycoprotein 1, formation of antiphospholipid antibody complexes promoting platelet aggregation, coagulation cascade, and formation of cross‐linked fibrin blood clots, leading to pulmonary emboli (PE) and large vessel strokes seen on angiographic imaging studies. There is emerging evidence for COVID‐19 being a blood clotting disorder and SARS‐CoV‐2 using the respiratory route to enter the blood stream. As the blood‐air barrier is breached, varying degrees of collateral damage occur. Although antiviral and immune therapies are studied, the role of blood thinners in the prevention, and management of blood clots in Covid‐19 need evaluation. In addition to ventilators and blood thinners, continuous aspiration and clot retrieval devices (approved in Europe, cleared in the United States) or cyclical aspiration devices (approved in Europe) need to be considered for the emergent management of life‐threatening clots including PE and large vessel strokes.
Keywords: Antiphospholipid antibodies, blood clots, COVID‐19, stroke, thrombectomy
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection was initially thought to only cause a respiratory illness. 1 However, two reports have been recently published of patients with ischemic strokes in the setting of corona virus disease 2019 (COVID‐19). 2 , 3 The first report 2 from Wuhan describes strokes associated with anticardiolipin antibodies, a known risk factor for blood clots and stroke. 4 The second report 3 from New York City describes strokes in young patients, associated with clots in large vessels supplying the brain requiring vacuum aspiration devices or clot retrieval devices and blood thinning medications. This raises the question, whether SARS‐CoV‐2 causes a blood clotting disorder and uses the respiratory route mainly for human‐to‐human transmission to enter the blood stream.
ACE2 Receptors: Key to the Lock
SARS‐CoV‐2 shares nearly 80% of its genome to the initial SARS‐CoV, 1 with a similar trimeric viral spike protein (key) that uses the same human cell entry receptor (lock)—angiotensin converting enzyme II (ACE2). 5 ACE2 receptors are found across the body including the alveolar cells within lungs as well as endothelial cells within blood vessels, namely, the arteries, capillaries, and veins. 6 , 7 To cause blood clots that can lead to strokes, SARS‐CoV‐2 needs to first enter the blood stream, then attach to the ACE2 receptors on the endothelial cells. Serological investigation shows that SARS‐CoV‐2 does enter the blood stream and is present in blood samples of COVID‐19 patients. 8 Postmortem and histologic analysis of COVID‐19 patients have recently shown the presence of SARS‐CoV‐2 within endothelial cells that results in endothelial dysfunction, and a cascade of events that can lead to a procoagulant state and blood clots. 7 How does SARS‐CoV‐2 enter the blood stream in the first place?
Breaching the Blood‐Air Barrier
SARS‐CoV‐2 enters the body predominantly via the respiratory route (Fig 1A). As long as SARS‐CoV‐2 is contained within the upper respiratory tract or the lower respiratory tract, namely, the alveoli within the lungs, it causes a respiratory illness like a mild flu in 81% and a moderate to severe pneumonia in 14% of COVID‐19 patients. 9 However, SARS‐CoV‐2 infection within the alveolar cells lining the alveolar membrane and the subsequent host inflammatory response can damage this thin membrane resulting in a critical illness in 5% of COVID‐19 patients. 9 , 10 This thin membrane interface between the alveolus in the lungs and the adjacent lung capillary is also called the blood‐air barrier. When the blood‐air barrier is breached, SARS‐CoV‐2 can enter the lung capillary that is adjacent to the alveolus (Fig 1B). Because SARS‐CoV‐2 is less than 150 nm (≤.15 microns) in diameter, 7 it can easily pass through the lung capillaries that are 5,000‐8,000 nm (5‐8 microns) in diameter, 11 and enter the left side of the heart to be pumped all over the body including the brain. This allows SARS‐CoV‐2 to enter the blood stream, 8 and the spike protein (key) can attach to the ACE2 receptors (lock) across the body including endothelial cells within blood vessels (Fig 1C). 7 How does SARS‐CoV‐2 then lead to endothelial dysfunction and blood clots?
Fig 1.
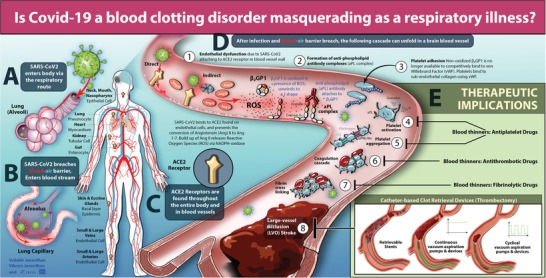
Coronavirus disease 2019 (COVID‐19), blood clots, and stroke—mechanisms and therapeutic implications: In Panel A, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) enters the body predominantly via the respiratory route. In Panel B, SARS‐CoV‐2 breaches the blood‐air barrier, and enters the blood stream via the lung capillary that is adjacent to the alveolus. In Panel C, once SARS‐CoV‐2 enters the blood stream, the spike protein (key) can attach to angiotensin‐converting enzyme 2 (ACE2) receptors (lock) across the body including endothelial cells in neck or brain blood vessels. Mechanisms of blood clots and stroke in COVID‐19: In Panel D, a cascade of events unfolds resulting in blood clots and strokes. In Step 1, endothelial dysfunction can occur either directly by viral entry into the endothelial cell or indirectly with the accumulation of Angiotensin (Ang) II as SARS‐CoV‐2 attaches to ACE2 and is not able to convert Ang II to Ang 1,7. Ang II can result in reactive oxygen species (ROS), oxidative stress, and endothelial dysfunction. In Step 2, oxidation of beta 2 glycoprotein 1 (β2GP1) occurs due to endothelial dysfunction and ROS, and results in the formation of antiphospholipid (aPL) antibody complexes. In Step 3, platelet adhesion occurs and platelets attach to the subendothelial collagen using von Willebrand Factor (vWF). This happens because the non‐oxidized β2GP1 is no longer available to competitively bind vWF. In Step 4, platelet activation occurs due to platelets binding to vWF resulting in granule release (α and dense) and the presence of aPL complexes further promotes platelet activation. In Steps 5‐7, platelet aggregation using vWF or fibrinogen (released by α granules), formation of thrombus via the coagulation cascade, and subsequent cross‐linking of fibrin strands to stabilize the clot occur. In Step 8, a pulmonary embolism (PE) and/or a large vessel occlusion stroke occurs. Therapeutic implications: In Panel E, several blood thinners like antiplatelet drugs can impact Steps 4 and 5 (eg, oral aspirin, oral clopidogrel, etc), antithrombotic drugs can impact Step 6 (antithrombin III binding agent, eg, parenteral heparin, vitamin K antagonist, eg, oral warfarin, newer direct Xa or thrombin inhibitors, etc), and fibrinolytic drugs can impact Step 7 (eg, intravenous tissue plasminogen activator or tenecteplase, etc). Several catheter‐based devices (approved in Europe, and cleared to market in the United States) can impact Step 8 (eg, clot retrieval devices that try to use clot integration, continuous vacuum aspiration pumps, and devices that try to use uniform negative suction pressure to ingest clots) or newer devices (approved in Europe) can impact Step 8 (eg, cyclical vacuum aspiration pumps and devices that use pulsating negative suction pressure to improve complete clot ingestion and reduce clot fragmentation), help remove blood clots, and treat PE and large vessel strokes.
Plausible Mechanisms for Blood Clots in COVID‐19
Once SARS‐CoV‐2 enters the blood stream, a cascade of events unfolds resulting in blood clots and strokes (Fig 1D, Steps 1‐8). After attaching to the ACE2 receptor on endothelial cells in the presence of a serine protease (TMPRSS‐2), 5 SARS‐CoV‐2 enters the endothelial cell to replicate and release numerous copies of itself, 10 and in the process endothelial dysfunction occurs (Fig 1D, Step 1—direct injury). 7 In parallel, as SARS‐CoV‐2 is attached to ACE2, 5 ACE2 is not available within the renin‐angiotensin system to convert angiotensin II (Ang II) to angiotensin‐(1,7) resulting in Ang II to accumulate. 12 Ang II stimulates membrane‐bound nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, which in turn generates reactive oxygen species (ROS) and oxidative stress 13 ; this can also lead to endothelial dysfunction (Fig 1D, Step 1—indirect injury). 12
The presence of reactive oxygen species assists in the transformation of a circulating, nonoxidized, circular‐shaped β2‐glycoprotein 1 (β2GP1) into an oxidized J‐shape (Fig 1D, Step 2). 14 This J‐shape of β2GP1 exposes its immunogenic domain I and is the antigen that binds to antiphospholipid (aPL) antibodies such as anticardiolipin, lupus anticoagulant, and anti‐β2GP1 antibodies. 15 Domain V of β2GP1 (+ charge) binds with the phospholipid layer (– charge) of platelets 15 or endothelial cells via Annexin. 4
Three things happen at this stage. First, the primary mechanisms by which endothelial cells prevent a platelet plug (eg, via nitric oxide, prostacyclins, and ADPase CD39) are overcome because of endothelial dysfunction. 16 Second, platelet adhesion begins at the site of endothelial dysfunction with von Willebrand factor (vWF) binding with subendothelial collagen and platelets (via GPIb) as the nonoxidized form of β2GP1 is no longer available to competitively bind vWF (Fig 1D, Step 3). 15 Third, oxidized β2GP1 and aPL antibody complex is stabilized by platelet factor 4 (PF4) released from alpha (α) granules within platelets and promotes platelet activation (Fig 1D, Step 4). 15 The α granules also release vWF and fibrinogen. The dense granules within platelets release adenosine diphosphate (ADP; acts on P2YP12 receptor) and thromboxane A2 (TXA2; a COX‐1 metabolite).
This further promotes platelet aggregation (via GPIIb/IIIa), 16 neutrophil extracellular traps (an ideal foundation for binding activated platelets and red blood cells), 17 coagulation cascade, 16 formation of cross‐linked fibrin blood clots, 16 and subsequently leads to large vessel strokes (Fig 1D, Steps 5‐8). 3 , 12
Blood Clots in COVID‐19 Patients
Among hospitalized COVID‐19 patients in New York City (n = 5,700), nearly 9 out of 10 (88%) patients who were on ventilators died. 18 This cannot be accounted for by acute respiratory distress syndrome (ARDS) alone. In a report from Italy, only 20‐30% of critically ill COVID‐19 pneumonia patients had ARDS (low lung compliance, type 2), the rest had a ventilation‐perfusion mismatch due to impaired pulmonary blood flow most likely from pulmonary thrombosis or clots (near normal lung compliance, type 1). 19
In a report from Wuhan, 90% of hospitalized COVID‐19 patients had coagulopathy (without bleeding) with an 18‐fold increase in mortality when d‐dimer level was >1 µg/mL. 20 A procoagulant state with aPL antibodies occurs. 2 , 4 , 21 , 22 , 23 In a report from London, 91% of COVID‐19 patients with a prolonged activated partial‐thromboplastin time had positive lupus anticoagulant (aPL antibody) assays. 21
Clots in the brain (strokes), 2 , 3 , 22 , 23 heart (heart attacks), 24 lungs (pulmonary emboli), 25 gut (mesenteric ischemia), 7 and legs (limb ischemia) 26 have also been reported. The clinical significance of blood clotting in COVID‐19 patients was reported in a Dutch study (n = 184), wherein the incidence of blood clotting complications, namely, the composite outcome of symptomatic acute pulmonary embolism (PE), deep‐vein thrombosis, ischemic stroke, myocardial infarction, or systemic arterial embolism, in all COVID‐19 patients admitted to the intensive care unit (ICU) was high (31%) with PE being the most frequent blood clotting complication. 25
Incidence of Strokes in COVID‐19 Patients
Despite the high incidence of blood clots leading to PE among COVID‐19 patients in the ICU, 25 the incidence of ischemic strokes among hospitalized COVID‐19 patients seems to be lower and variable. 27 , 28 , 29 Similar to a report from Wuhan (n = 4/214, 1.87%), 29 a recent report from New York showed a 1.8% incidence rate of ischemic stroke (n = 31/1,683; 95% confidence interval [CI], 1.3‐2.6%] among all COVID‐19 hospitalized patients in an 8‐week period between March 4 to May 2, 2020 (during the early phase and the initial surge phase). 27 Another report from New York showed a .9% incidence rate of imaging proven ischemic stroke (n = 32/3,556) among all COVID‐19 hospitalized patients in a 4‐week period between March 15, 2020 and April 19, 2020 (during the initial surge phase). 28 Given that the stay at home order was issued in New York on March 22, 2020 during the study period, it is possible that these reports may under estimate the incidence of ischemic stroke in COVID‐19 as patients may have been staying at home and not presenting to the emergency department for stroke treatment. 28 This reduction in stroke admissions is reiterated in a nationwide analysis of data (n = 231,753 patients), on patients who underwent neuroimaging studies for stroke in 856 hospitals in the United States, which showed a 39% reduction in the number of patients who received evaluations for acute stroke in a 2‐week period between March 26, 2020 and April 8, 2020 (during the initial surge phase) compared to the prepandemic era. 30 Similar reductions in stroke admissions due to a possible “bystander effect” have been reported in Michigan and Northwest Ohio (17.8% reduction in March 2020 compared to February 2020), 31 and in Tehran, Iran (40% reduction between February 15, 2020 and April 15, 2020 compared to the period between September 15, 2019 and February 15, 2020). 32
On the other hand, inpatient mortality was higher (32% 27 to 63.6% 28 ) among patients with COVID‐19 with ischemic stroke compared to COVID‐19 patients without ischemic stroke (9.3% 28 to 14% 27 ) suggesting that the severity of illness is much higher in COVID‐19 patients with ischemic strokes. 32 Due to the pandemic, it is also possible that some patients with undiagnosed COVID‐19 and stroke may have died before reaching the hospital (out‐of‐hospital mortality) thereby further under estimating the incidence of ischemic stroke in COVID‐19. 27 This increase in out‐of‐hospital mortality during the COVID‐19 pandemic is reiterated in a population‐based report from Paris and its suburbs, which has shown a twofold increase in the incidence of out‐of‐hospital cardiac arrest from 13.42 (95% CI, 12.77‐14.07) to 26.64 (95% CI, 25.72‐27.53) in a 6‐week period between March 16, 2020 and April 26, 2020 (during the surge phase, Paris Lockdown began March 17) compared to the prepandemic era. 33
Preceding viral infection can be a risk factor for ischemic stroke as thromboinflammatory pathways may be perturbed. 34 Coagulopathy and aPL antibodies (such as anticardiolipin, lupus anticoagulant, and anti‐β2GP1 antibodies) in patients with COVID‐19 may contribute to thromboembolic events including ischemic strokes. 2 , 22 , 23 Ischemic strokes in patients with coronavirus infection have been reported from cities worldwide during prior viral epidemics such as due to SARS‐CoV1 (eg, Singapore 35 ), as well as the current viral pandemic due to SARS‐CoV‐2 (eg, Wuhan [China] 2 , 29 ; London [United Kingdom] 22 ; Trevenans, Strasbourg, and Paris [France] 23 , 36 , 37 ; Leiden, Rotterdam, and Breda [the Netherlands] 25 ; Brescia and Udine [Italy] 38 ; New York [New York, USA] 3 , 27 , 28 , 39 , 40 , 41 , 42 , 43 ; Philadelphia [Pennsylvania, USA] 44 , 45 , 46 ; Detroit [Michigan, USA] 47 ; Michigan and Northwest Ohio [USA] 31 ; and Tehran [Iran] 32 ). This suggests that the thrombotic complications leading to ischemic strokes in COVID‐19 patients are not isolated events but do occur worldwide. Further research is needed to truly understand the population‐based incidence as well as the incidence of large vessel strokes in hospitalized patients with COVID‐19.
Neuroimaging Findings in COVID‐19 Stroke Patients
A recent report from Iran suggests that although the number of stroke admissions have reduced during the pandemic, the proportion of stroke patients with COVID‐19 who had large vessel occlusions (LVOs) on neuroimaging was higher (38.7%) during this pandemic (February 15, 2020 to April 15, 2020), compared to 26.6% in stroke patients without COVID‐19 during the immediate period preceding the pandemic (September 15, 2019 to February 15, 2020), and 14% during the previous year (February 15, 2019 to April 15, 2019) (P = .046). 32 Similar results from Philadelphia (USA) have shown that although there was a 23% reduction in stroke admissions during the pandemic (March 15, 2020 to April 30, 2020), there has been a 50% increase in mechanical thrombectomy procedures for LVOs during the same period (with 25% of these thrombectomy procedures for LVOs being in patients with COVID‐19) compared to prior years. 46
In a report from Philadelphia (USA), stroke patients with COVID‐19 have been reported with blood clots in the arteries (LVOs) or the veins (Cerebral Venous Sinus Thrombosis, CVST). 46 Stroke‐causing blood clots in COVID‐19 patients have also been reported to have higher proportion of tandem occlusions or multiple arterial occlusions (67%) on angiography compared with historical controls (15%). 46 , 47 Similar results were reported from Paris (France), where nearly 50% of stroke patients with COVID‐19 had multi‐territory LVOs. 37 In a report from Detroit (Michigan, USA), intraluminal carotid artery thrombus was noted in stroke patients with COVID‐19 (n = 6) superimposed on an underlying carotid artery stenosis at the cervical internal carotid artery bifurcation detected on computed Tomography (CT) angiography associated with an artery‐to‐artery thromboembolism in nearly 50% of the patients (from the thrombus in the cervical carotid artery to an intracranial LVO location). 47 Reports from Paris, New York, and Philadelphia, have shown that the location of the LVOs identified on angiography have included both proximal LVOs in the carotid, proximal segment of the middle cerebral artery (M1), or basilar artery, as well as distal LVOs in the anterior cerebral artery, distal segment of the middle cerebral artery (M2), or posterior cerebral arteries. 37 , 43 , 46
First Pass Effect is Lower in COVID‐19 Stroke Patients
Large‐vessel strokes (LVOs) have a poor natural history with a high mortality (modified ranking score [mRS] = 6 [41.9%]) and low rate of good functional outcomes (mRS = 0‐2 [20.7%]). 48 Complete vessel reopening based on the Thrombolysis in Cerebral Infarction (TICI) scale (TICI 3, wherein TICI 0 is complete vessel occlusion and TICI 3 is complete vessel re‐opening) in the very first operative attempt during thrombectomy, also known as the TICI 3 first pass effect (FPE) has become the gold standard metric for a successful thrombectomy in patients with large vessel strokes. 49 This is because TICI 3 FPE is associated with the lowest mortality (mRS = 6 [16.3%]) and the best good functional outcomes (mRS = 0‐2 [61.3%]), compared to other angiographic metrics. 49 In a recent report from Paris (France) during the pandemic between March 1, 2020 and April 15, 2020, despite a 90% partial vessel reopening in multiple passes (any TICI 2b or greater, median number of 3.5 passes per patient), none of the large vessel stroke patients with COVID‐19 who underwent mechanical thrombectomy for LVOs had a complete vessel reopening after the first pass (TICI 3 FPE = 0%, n = 0/10). 37 In contrast, LVO stroke patients without COVID‐19 in the same time period at the same institution had a 33% complete vessel reopening after the first pass (TICI 3 FPE = 33%, n = 9/27). 37 Similarly, in a recent report from New York City during the pandemic, large vessel stroke patients with COVID‐19 who underwent mechanical thrombectomy for LVOs (using a combination of a stent retriever and continuous uniform aspiration) also had a lower first pass effect (TICI 3 FPE = 16.7%, n = 1/6 thrombectomies performed in different target vessel territories among 5 patients). 39 This suggests that endovascular removal of thrombus from large vessel stroke patients with COVID‐19 is more difficult that noninfected patients, requiring multiple passes and significantly fewer if any complete revascularizations. 37
COVID‐19‐Associated Clots (eg, Large‐Vessel Strokes) are More Refractory and Susceptible to Rethrombosis and Reocclusions
In addition, 40% of the large vessel stroke patients with COVID‐19 had an early vessel reocclusion on neuroimaging after mechanical thrombectomy suggestive of a procoagulant state in COVID‐19 resulting in high in‐hospital mortality rates (60%) and no clinical improvement among survivors. 37 Figure 2 shows an illustrative example (courtesy: Dr Andrew R. Xavier, Michigan, USA) of a cerebral angiogram (pre‐ and posttreatment, Figs 2A and 2B) in a young stroke patient (47‐year‐old gentleman) with COVID‐19 who had three (3) recurrent reocclusions of the M1 segment of the left middle cerebral artery despite thrombectomy (using a combination of a stent retriever and continuous uniform aspiration). Finally, the fourth pass had partial revascularization due to an extensive clot burden (Fig 2C) suggestive of a prothrombotic state with refractory platelet‐fibrin‐rich clots on histopathology (Fig 2D). Further research is needed to better understand the optimal thrombectomy devices to increase the TICI 3 FPE. 49 Newer devices such as cyclical aspiration aid in complete clot ingestion and have shown great promise in increasing first pass recanalization and reducing distal embolization. 50
Fig 2.
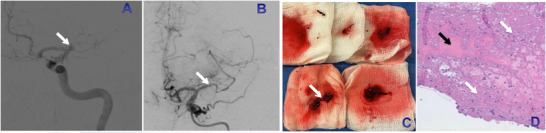
An illustrative example of a cerebral angiogram (pretreatment, see Panel A; posttreatment, see Panel B) in a young stroke patient (47‐year‐old gentleman) with coronavirus disease 2019 who had three (3) recurrent reocclusions of the proximal segment of the left middle cerebral artery (see white arrow in Panel A) despite thrombectomy (using a combination of a stent retriever and continuous uniform aspiration) and finally on the fourth pass had partial revascularization (see white arrow in Panel B) due to an extensive clot burden (see white arrow in Panel C) suggestive of a prothrombotic state with refractory platelet‐fibrin‐rich clots on histopathology (Fig 2D). In Panel D, predominantly there are fibrin‐rich clots (shown as the bluish‐pink areas, see white arrows in Panel D), with interspersed cells, for example, leucocytes (see blue dots around the white arrows in Panel D), and small amounts of red blood cells (shown as the pinkish‐red areas, see black arrow in Panel D). (Courtesy: Dr Andrew R. Xavier, Michigan, USA has given permission to reproduce the figure).
Different Modalities of Thrombectomy Have a Differing Impact on the Vessel Wall and Severity of Endothelial Injury
It is important to understand the biological rationale for the susceptibility to rethrombosis or reocclusions discussed above. Recent reports have raised various concerns about the risk of endothelial injury while withdrawing current stent retrievers, with high radial force, 51 during active strut apposition to the vessel walls. 51 , 52 , 53 In a rabbit model of carotid artery stent retriever thrombectomy, laser‐cut stent retrievers demonstrated histological evidence of disruption and thickening of the intimal layer extending into the media. 52 A comparison of endothelial damage caused by continuous uniform aspiration versus a stent retriever device after thrombectomy in a swine model showed that both techniques caused endothelial damage; however, thrombectomy with a stent retriever appeared to be more harmful to all layers of the arterial wall, particularly the endothelium. 53 In a recent report from New York City during the pandemic, 40% of the large vessel stroke patients (n = 2/5) encountered a reocclusion of the vessel within minutes of recanalization with a stent retriever. 39 This suggests that thrombectomy using current stent retrievers is more susceptible to rethrombosis, especially in COVID‐19 patients where there is endothelial dysfunction, 7 as current stent retrievers may be exacerbating the endothelial inflammatory response causing the rethrombosis and reocclusions.
Given our current understanding of endothelial dysfunction in COVID‐19, 7 the impact of endovascular stroke therapies on the vessel wall and endothelium becomes more relevant. In a randomized study on a rabbit model, the safety profile of cyclical aspiration compared to continuous uniform aspiration on the vessel wall including endothelium was studied. 54 Cyclical aspiration was noted to have an improved safety profile at the end of the procedure with a significant reduction in persistent vasospasm (in M1 and M2 segment of the middle cerebral artery vessel equivalents) of 12.5% in the cyclical aspiration group compared to 56% in the continuous uniform aspiration group (P = .046). 54 In the current COVID‐19 pandemic era, any form of damage or injury to the endothelium or vessel wall has clinical implications and may impact the choice of thrombectomy device for endovascular stroke therapy.
Therapeutic Implications
As seen above on angiographic neuroimaging studies, there is emerging evidence for COVID‐19 being a blood clotting disorder, 55 and SARS‐CoV‐2 using the respiratory route to enter the blood stream. 8 As the blood‐air barrier is breached, varying degrees of collateral damage occurs. 2 , 3 , 7 , 10 , 19 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 31 , 32 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 Although antiviral and immune therapies are studied, 10 the role of blood thinners in the prevention, and management of blood clots in COVID‐19 needs evaluation. 25 , 56
Several blood thinners like antiplatelet drugs can impact Steps 4 and 5 (COX‐1 inhibitor, eg, oral aspirin, P2Y12 inhibitor, eg, oral clopidogrel etc), antithrombotic drugs can impact Step 6 (antithrombin III binding agent, eg, parenteral heparin, Vitamin K antagonist, eg, oral warfarin, newer direct Xa, or thrombin inhibitors etc), and fibrinolytic drugs can impact Step 7 (eg, intravenous tissue plasminogen activator or tenecteplase, etc) (Fig 1E). 12 , 16 , 25 , 56
Several catheter‐based devices (Fig 1E) that are Conformité Européenne (CE) Mark approved in the European Union or cleared to market in the United States by the Food and Drug Administration (FDA) can impact Step 8 (eg, clot retrieval devices or retrievable stents that try to use clot integration, continuous vacuum aspiration pumps, and devices that try to use uniform negative suction pressure to ingest clots) 25 , 56 , 57 or newer devices (that are CE Mark approved in the European Union; Fig 1E) can impact Step 8 (eg, cyclical vacuum aspiration pumps and devices that use pulsating negative suction pressure to improve complete clot ingestion and reduce clot fragmentation) 50 and can help remove and treat blood clots including due to pulmonary emboli and large vessel strokes (Fig 3).
Fig 3.
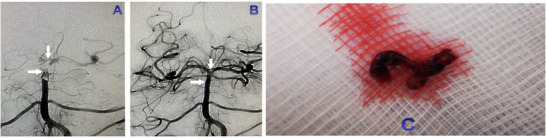
An illustrative example of a cerebral angiogram (pretreatment, see Panel A; posttreatment, see Panel B) in an elderly stroke patient (82‐year‐old lady) with a basilar artery thrombus extending from the mid‐basilar artery proximal to the origin of the bilateral superior cerebellar arteries (see horizontal white arrow in Panels A‐B) to the top of the basilar artery near the bifurcation of the bilateral posterior cerebral arteries (see vertical white arrow in Panels A‐B). Patient with the basilar artery thrombus was treated with one of the newer vacuum suction devices to remove blood clots (CLEARTM Aspiration System, approved in the European Union recently). Cyclical Aspiration was performed with complete vessel reopening (TICI 3) on the first pass (Fig 3B) and successful removal of the basilar artery thrombus (Fig 3C). (Courtesy: Dr Vladimir Kalousek, Zagreb, Croatia, has given permission to reproduce the figure).
Different modalities of mechanical thrombectomy may have differing efficacy (complete vessel reopening, TICI 3 FPE) and safety profiles (impact on the vessel wall or severity of endothelial injury). This will likely impact the choice of modality for mechanical thrombectomy or endovascular stroke therapy in the COVID‐19 era.
Health Policy Implications
We are witnessing countries worldwide in different phases of the COVID‐19 pandemic trajectory, 58 and different cities even within the same country also seem to be in different phases of the COVID‐19 pandemic trajectory. 59 Therefore, understanding the mechanisms of blood clotting can potentially help prevent or mitigate end organ damage beyond the respiratory illness in COVID‐19. This can help physicians, health systems, and public health policy makers better prepare for any potential surge (given the varying trajectories of this pandemic), educate the public when to seek medical care and hospitalization, and support further research to help reduce the morbidity and mortality associated with COVID‐19.
Conclusions
Given our current understanding of the mechanisms of blood clot formation in COVID‐19 and these clots being more refractory, further neuroimaging research is needed to define the complete vessel reopening rates on angiography in the first operative attempt (TICI 3 on first pass) and the optimal modality for mechanical thrombectomy or endovascular stroke therapy in the COVID‐19 era. In addition to ventilators and blood thinners, continuous vacuum aspiration devices, clot retrieval devices, retrievable stents (European CE mark approved, U.S. FDA cleared), 25 , 56 , 57 or cyclical vacuum aspiration devices (European CE mark approved) to remove blood clots need to be considered for the emergent management of life‐threatening blood clots due to COVID‐19 including pulmonary emboli and large vessel strokes. 50 Finally, the appropriate resources and staffing needs for hospitals and stroke centers including for emergency rooms, neuroimaging studies, neurocritical care units, and stroke interventional labs need to considered in the era of the COVID‐19 pandemic. 60 , 61
Acknowledgements and Disclosure: Dr Vallabh Janardhan reports grants from National Science Foundation, other from Insera Therapeutics, Inc, and other from Society of Vascular & Interventional Neurology (SVIN), outside the submitted work. In addition, Dr Janardhan has patents with the United States Patent and Trademark Office (USPTO), over 20+ patents pending, and 65+ USPTO and worldwide patents issued. Dr Vikram Janardhan reports grants from National Science Foundation and other from Insera Therapeutics, Inc, outside the submitted work. In addition, Dr Janardhan has over 20+ patents pending and 65+ USPTO and worldwide patents issued. Dr Vladimir Kalousek reports consultancy from Balt and other from Microvention‐Terumo, outside the submitted work. The preclinical testing was funded in part by the National Science Foundation (NSF Award: 1819491, Principal Investigator: Vallabh Janardhan).
References
- 1. Zhou P, Yang X, Wang X, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID‐19. N Engl J Med 2020;382:e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of COVID‐19 in the young. N Engl J Med 2020;382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Janardhan V, Wolf PA, Kase CS, et al. Anticardiolipin antibodies and risk of ischemic stroke and transient ischemic attack: the Framingham Cohort and Offspring Study. Stroke 2004;35:736‐41. [DOI] [PubMed] [Google Scholar]
- 5. Hoffman M, Kleine‐Weber H, Schroeder S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hamming I, Timens W, Bulthuis MLC, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 2004;203:631‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endothelitis in COVID‐19. Lancet 2020;395:1417‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang W, Du R, Li B, et al. Molecular and serological investigation of 2019‐nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect 2020;9:386‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and prevention. JAMA 2020;323:1239‐42. [DOI] [PubMed] [Google Scholar]
- 10. Sanders JM, Monogue ML, Jodlowski TZ, et al. Pharmacologic treatments for coronavirus disease 2019 (COVID‐19): a review. JAMA 2020;323:1824‐36. [DOI] [PubMed] [Google Scholar]
- 11. Townsley MI. Structure and composition of pulmonary arteries, capillaries, and veins. Compr Physiol 2012;2:675‐709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hess DC, Eldahshan W, Rutkowski E. COVID‐19‐related stroke. Transl Stroke Res 2020;11:322‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garrido AM, Griendling KK. NADPH oxidases and angiotensin II receptor signaling. Mol Cell Endocrinol 2009;302:148‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. El‐Assaad F, Krilis SA, Giannakopoulos B. Posttranslational forms of beta 2‐glycoprotein I in the pathogenesis of the antiphospholipid syndrome. Thromb J 2016;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ho YC, Ahuja KDK, Korner H, et al. β2GP1, anti‐β2GP1 antibodies and platelets: key players in the antiphospholipid syndrome. Antibodies 2016;5:E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood 2019;133:906‐18. [DOI] [PubMed] [Google Scholar]
- 17. Becker RC. COVID‐19 update: COVID‐19‐associated coagulopathy. J Thromb Thrombolysis 2020;50:54‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA 2020;323:2052‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gattinoni L, Chiumello D, Rossi S. COVID‐19 pneumonia: ARDS or not? Crit Care 2020;24:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhou F, Ting Y, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bowles L, Platton S, Yartey N, et al. Lupus anticoagulant and abnormal coagulation in patients with COVID‐19. N Engl J Med 2020;383:288‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID‐19. J Neurol Neurosurg Psychiatry 2020;91:889‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zayet S, Klopfenstein T, Kovẚcs R, et al. Acute cerebral stroke with multiple infarctions and COVID‐19, France, 2020. Emerg Infect Dis 2020;26. 10.3201/eid2609.201791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stefanini GG, Montorfano M, Trabattoni D, et al. ST‐elevation myocardial infarction in patients with COVID‐19: clinical and angiographic outcomes. Circulation 2020;141:2113‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID‐19. Thromb Res 2020;191:145‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bellosta R, Luzzani L, Natalini G, et al. Acute limb ischemia in patients with COVID‐19 pneumonia. J Vasc Surg 2020. 10.1016/j.jvs.2020.04.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Merkler AE, Parikh NS, Mir S, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID‐19) vs patients with influenza. JAMA Neurol 2020. 10.1101/2020.05.18.20105494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yaghi S, Ishida K, Torres J, et al. SARS‐CoV‐2 and stroke in a New York healthcare system. Stroke 2020;51:2002‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020;77:683‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kansagra AP, Goyal MS, Hamilton S, et al. Collateral effect of COVID‐19 on stroke evaluation in the United States. N Engl J Med 2020;383:400‐401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pandey AS, Daou BJ, Tsai JP, et al. Letter: COVID‐19 pandemic—the bystander effect on stroke care in Michigan. Neurosurgery 2020. 10.1093/neuros/nyaa252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mehrpour M, Shuaib A, Farahani M, et al. Coronavirus disease 2019 and stroke in Iran: a case series and effects on stroke admissions. Int J Stroke 2020. 10.1177/1747493020937397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Marijon E, Karam N, Jost D, et al. Out‐of‐hospital cardiac arrest during the COVID‐19 pandemic in Paris, France: a population‐based, observational study. Lancet 2020. 10.1016/S2468-2667(20)30117-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. South K, McCulloch L, McColl BW, et al. EXPRESS: preceding infection and risk of stroke: an old concept revived by the COVID‐19 pandemic. Int J Stroke 2020. 10.1177/1747493020943815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Umapathi T, Kor AC, Venkatasubramanian N, et al. Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol 2004;251:1227‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS‐CoV‐2 infection. N Engl J Med 2020;382:2268‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Escalard S, Maier B, Redjem H, et al. Treatment of acute ischemic stroke due to large vessel occlusion with COVID‐19: experience from Paris. Stroke 2020;51:2540‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Morassi M, Bagatto D, Cobelli M, et al. Stroke in patients with SARS‐CoV‐2 infection: case series. J Neurol 2020;267:2185‐2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang A, Mandigo GK, Yim PD, et al. Stroke and mechanical thrombectomy in patients with COVID‐19: technical observations and patient characteristics. J Neurointerv Surg 2020;12:648‐53. [DOI] [PubMed] [Google Scholar]
- 40. Valderrama EV, Humbert K, Lord A, et al. Severe acute respiratory syndrome coronavirus 2 infection and ischemic stroke. Stroke 2020;51:e124‐7. [DOI] [PubMed] [Google Scholar]
- 41. Fara MG, Stein LK, Skliut M, et al. Macrothrombosis and stroke in patients with mild COVID‐19 infection. J Thromb Haemost 2020. 10.1111/jth.14938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Avula A, Nalleballe K, Narula N, et al. COVID‐19 presenting as stroke. Brain Behav Immun 2020;87:115‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yaeger KA, Fifi JT, Lara‐Reyna J, et al. Initial stroke thrombectomy experience in New York city during the COVID‐19 pandemic. AJNR Am J Neuroradiol 2020. 10.3174/ajnr.A6652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sweid A, Hammoud B, Bekelis K, et al. Cerebral ischemic and hemorrhagic complications of coronavirus disease 2019. Int J Stroke 2020. 10.1177/1747493020937189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sweid A, Hammoud B, Weinberg JH, et al. Letter: thrombotic neurovascular disease in COVID‐19 patients. Neurosurgery 2020. 10.1093/neuros/nyaa254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sweid A, Jabbour P, Tjoumakaris S. Letter to the editor: incidence of acute ischemic stroke and rate of mechanical thrombectomy during the COVID‐19 pandemic in a large tertiary care telemedicine network. World Neurosurg 2020. 10.1016/j.wneu.2020.06.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mohamud AY, Griffith B, Rehman M, et al. Intraluminal carotid artery thrombus in COVID‐19: another danger of cytokine storm? AJNR Am J Neuroradiol 2020. 10.3174/ajnr.A6674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Janardhan V, Venizelos A, Gianatasio RM, et al. Abstract W MP8: the Natural history of acute stroke from large vessel proximal occlusion: a comparison with the IMS III patients. Stroke 2014;45:AWMP8. [Google Scholar]
- 49. Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke 2018;49:660‐6. [DOI] [PubMed] [Google Scholar]
- 50. Arslanian RA, Marosfoi M, Caroff J, et al. Complete clot ingestion with cyclical ADAPT increases first‐pass recanalization and reduces distal embolization. J Neurointerv Surg 2019;11:931‐6. [DOI] [PubMed] [Google Scholar]
- 51. Katz JM, Hakoun AM, Dehdashti AR, et al. Understanding the radial force of stroke thrombectomy devices to minimize vessel wall injury: mechanical bench testing of the radial force generated by a novel braided thrombectomy device compared to laser‐cut stent retrievers in simulated MCA vessel diameters. Interv Neurol 2019;8:206‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Arai D, Ishii A, Chihara H, et al. Histological examination of vascular damage caused by stent retriever thrombectomy devices. J Neurointerv Surg 2016;8:992‐5. [DOI] [PubMed] [Google Scholar]
- 53. Peschillo S, Diana F, Berge J, et al. A comparison of subacute vascular damage caused by ADAPT versus stent retriever devices after thrombectomy in acute ischemic stroke: histological and ultrastructural study in an animal model. J Neurointerv Surg 2017;9:743‐9. [DOI] [PubMed] [Google Scholar]
- 54. Kadirvel R, Dai D, Brinjikji W, et al. Cyclical aspiration has an improved safety profile compared to continuous uniform aspiration: in‐vivo randomized study. Paper presented at 12th Annual Meeting of the Society of Vascular & Interventional Neurology. Atlanta, GA; 2019. https://youtu.be/zqgdII52x5I [Google Scholar]
- 55. Teuwen L, Geldhof V, Pasut A, et al. COVID‐19: the vasculature unleashed. Nat Rev Immunol 2020;20:389‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ 2020;368:16983. [DOI] [PubMed] [Google Scholar]
- 57. Ciampi‐Dopazo JJ, Romeu‐Prieto JM, Sanchez‐Casado M, et al. Aspiration thrombectomy for treatment of acute massive and submassive pulmonary embolism: initial single‐center prospective experience. J Vasc Interv Radiol 2018;29:101‐6. [DOI] [PubMed] [Google Scholar]
- 58. Sahu KK, Mishra AK, Lal A. Trajectory of the COVID‐19 pandemic: chasing a moving target. Ann Transl Med 2020;8:694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. CDC COVID‐19 Response Team . Geographic differences in COVID‐19 cases, deaths, and incidence—United States, February 12‐April 7, 2020. MMWR Morb Mortal Wkly Rep 2020;69:465‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shams T, Zaidat O, Yavagal D, et al. Society of Vascular and Interventional Neurology (SVIN) Stroke Interventional Laboratory Consensus (SILC) criteria: a 7M management approach to developing a stroke interventional laboratory in the era of stroke thrombectomy for large vessel occlusions. Interv Neurol 2016;5:1‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Nguyen TN, Abdalkader M, Jovin TG, et al. Mechanical thrombectomy in the era of the COVID‐19 pandemic: emergency preparedness for neuroscience teams—a guidance statement from the Society of Vascular and Interventional Neurology. Stroke 2020;51:1896‐901. [DOI] [PMC free article] [PubMed] [Google Scholar]


