Dear Editor,
Since the Coronavirus Disease 2019 (COVID‐19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) spread out from Wuhan, China, to all over the world, dermatologists had to face department reorganization in order to avoid COVID‐19 infections among outpatients. 1
Dermatologic surgery, including wide local excisions of melanoma, squamous cell, and basal cell carcinoma represents a prominent part of all dermatological activities.
Since both melanoma and nonmelanoma skin cancer (NMSC) are mainly diagnosed in the elderly 2 and coronavirus infection leads to complicated pneumonia most commonly in older patients with comorbidities, 3 our institution had to face the difficult decision to postpone surgical procedures.
After our hospital became a COVID‐19 referral center, the balance between the risk of new contagions and the risk of cancer progression led us to choose from among all our listed outpatients only those suitable for surgery during this emergency.
We completely reorganized surgical appointments by analyzing each patient’s clinical state during a weekly multidisciplinary tumor board with the presence of dermatologists, oncologists, surgeons, and pathologists, with the aim to define, on the basis of tumor‐ and patient‐related characteristics, the ideal candidates for dermatologic surgery during this pandemic (Fig. 1).
Figure 1.
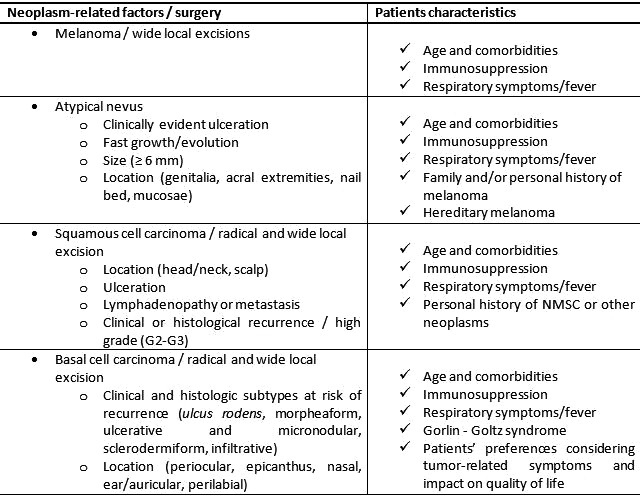
Tumor‐ and patient‐related characteristics of dermatologic surgery high‐need patients during COVID‐19 pandemic
During the briefing, we analyzed tumor burden, time of diagnosis, tumor‐related risk of progression, patient's age, and comorbidities (Fig. 2) in order to decide, case by case, whether to postpone or perform the scheduled surgery.
Figure 2.
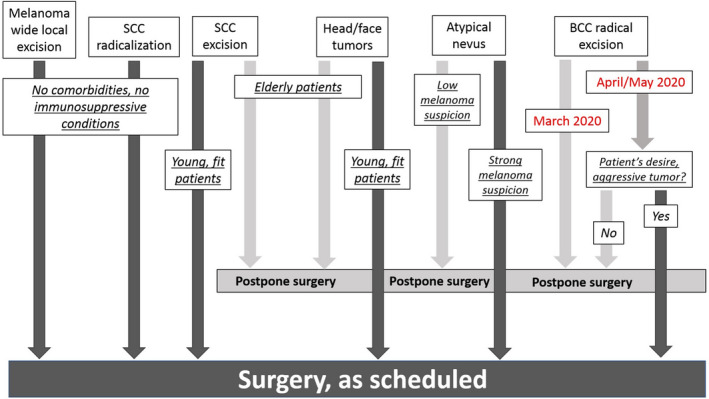
A schematic view of our multidisciplinary board’s model. Each case was discussed individually in order to decide whether to postpone or confirm dermatologic surgeries
Every week, after analyzing each patient’s medical history, with the aid of teledermatology we contacted all patients on the surgical list asking about their general conditions, possible close contacts with COVID‐19 affected relatives, and eventual clinical symptoms in order to decide whether to confirm or postpone surgeries.
As Tagliaferri et al. 4 wrote, the ideal management of cancer patients should ensure the gold standard treatment in the safest conditions. Dermatologists must think about two possible dangerous scenarios: (i) a safe outpatient could get COVID‐19 infection in the hospital and (ii) an unknown COVID‐19 outpatient could infect health professionals or other patients. 4 Despite the risk of new infections among patients, we must consider cancer progression and the impact of the surgical delay on the prognosis.
During the pandemic apex in Italy (March/April 2020), we performed 74 (40%) of 185 scheduled surgeries.
The decision of whether to perform or postpone atypical nevi excisions was made after analyzing patients’ family history of melanoma, hereditary syndromes, age, and neoplasm features (ulceration, fast growth, and location) (Fig. 1). We confirmed 32 radical excisions of atypical nevi and postponed 69 surgeries (31.68% vs. 69.32%).
In consideration of high mortality rates and guidelines’ recommendations, 5 we confirmed all 15 scheduled wide local excisions of melanoma for nonimmunosuppressed patients (Fig. 1).
Given the relevant risk of metastasis for squamous cell carcinoma (SCC), 2 we performed six scheduled wide local excisions (75%), delayed two surgeries (25%) for very old and immunosuppressed patients with multiple comorbidities. Surgical excisions were confirmed for lesions of the head, neck, and scalp and/or with ulceration for patients with a personal history of NMSC or other neoplasms. We guaranteed all surgeries for patients affected by clinical lymphadenopathy and clinical exam/radiological views suspicious of metastasis.
As recurring or at high risk of recurrence and locally advanced metastatic basal cell carcinomas (BCCs) as well as periocular, nasal, auricular, and perilabial lesions with poorly‐defined borders are considered as difficult‐to‐treat neoplasms, 2 we confirmed all scheduled surgeries considering patients’ comorbidities. We excised 15 BCCs (30%), including large ulcerated BCCs in patients affected by Gorlin‐Goltz syndrome, and we postponed 35 (70%) surgeries of small, not infiltrated, and recently diagnosed BCCs (Fig. 1).
In conclusion, facing probably the most difficult pandemic of modern times, we are called to balance the risks and benefits of confirming/postponing skin cancer surgeries and to define which patient is a surgical high‐need candidate in order to avoid a worse impact on life‐long prognosis.
Conflict of interest: None.
Funding source: None.
References
- 1. Gisondi P, Piaserico S, Conti A, Naldi L. Dermatologists and SARS‐CoV‐2: the impact of the pandemic on daily practice. J Eur Acad Dermatol Venereol 2020; 34(6): 1196–1201. 10.1111/jdv.16515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nehal KS, Bichakjian CK. Update on keratinocyte carcinomas. N Engl J Med 2018; 379: 363–374. [DOI] [PubMed] [Google Scholar]
- 3. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID‐19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020; 46: 846–848. 10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tagliaferri L, Di Stefani A, Schinzari G, et al. Skin cancer triage and management during COVID‐19 pandemic. J Eur Acad Dermatol Venereol 2020; 34(6): 1136–1139. 10.1111/jdv.16529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nikolaou V, Stratigos AJ. Emerging trends in the epidemiology of melanoma. Br J Dermatol 2014; 170: 11–19. 10.1111/bjd.12492 [DOI] [PubMed] [Google Scholar]


