Abstract
Background and Aims
Epidemics pose a great challenge to health care of patients. However, the impact of unprecedented situation of COVID‐19 outbreak on health care of inflammatory bowel disease (IBD) patients in real‐world setting has seldom been investigated.
Methods
We performed an observational study in a tertiary referral IBD center in China. The mode of health care and medication use was compared before and after COVID‐19 outbreak. Electronic questionnaire surveys were performed among gastroenterologists and IBD patients to investigate the impact of COVID‐19 outbreak on their attitudes towards telemedicine.
Results
COVID‐19 outbreak resulted in substantial decrease of patients participating in standard face‐to‐face visit during 1 month post‐outbreak (n = 51) than pre‐outbreak (n = 249), whereas the participation in telemedicine was significantly higher than comparable period in 2019 (414 vs 93). During the 1 month after COVID‐19 outbreak, 39 (39/56, 69.6%) patients had their infliximab infusion postponed with the mean delay of 3 weeks. The immunomodulator use was similar between pre‐outbreak and post‐outbreak. Six elective surgeries were postponed for a median of 43 days. In post‐outbreak period, 193 (193/297, 64.98%) of the surveyed physicians have used telemedicine with an increase of 18.9% compared with 46.13% (137/292) in the pre‐outbreak period (P < 0.001); 331 (331/505, 65.54%) of the surveyed IBD patients supported that the use of telemedicine should be increased in future health care.
Conclusion
COVID‐19 outbreak resulted in a great change in health‐care access among IBD patients including decrease in standard face‐to‐face visit and delay of biologics use. There was an increased use and need of telemedicine after COVID‐19 outbreak.
Keywords: COVID‐19, health care, inflammatory bowel disease
Introduction
The outbreak of COVID‐19 has been tremendously impacting the entire world. Given the extensive use of immunosuppressive agents, much attention has been paid to the risk of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection in patients with inflammatory bowel disease (IBD). In the SECURE‐IBD registry that aims to prospectively collect data of patients with IBD infected with SARS‐CoV‐2, more than 1000 IBD subjects had COVID‐19. 1 However, whether patients carry a higher risk for COVID‐19 than general population remains controversial.
Epidemics pose a great challenge to health care of patients with many chronic diseases including gastrointestinal (GI) diseases. IBD has become a global disease with an accelerating incidence in newly industrialized countries. 2 Characterized by a relapsing and remitting course, patients with IBD need close monitoring and therapy adjustment for an optimal disease management, which requires high health‐care resource utilization and costs. 3 However, the impact of such unprecedented situation of COVID‐19 outbreak on health care of patients with IBD in real‐world setting has seldom been investigated. The aim of this study was to investigate the impact of COVID‐19 outbreak on the health‐care access of patients with IBD by comparing the data before and after the outbreak of COVID‐19 in a tertiary referral center in China. In addition, electronic questionnaire surveys were performed among GI physicians and IBD patients in China to investigate the change in attitudes of physicians and patients towards telemedicine due to COVID‐19 outbreak.
Methods
Study design
This was an observational cohort study performed in the IBD center of The First Affiliated Hospital, Sun Yat‐sen University, Guangzhou, Guangdong, China. The IBD center is a tertiary facility that has registered more than 4000 IBD patients coming from all regions of China (the majority come from South China), and the center is a member of the Chinese IBD Elite Union (incorporating the seven largest IBD referral centers in China with > 20 000 IBD patients) (Fig. 1). 4 This study protocol was approved by the Clinical Research Ethics Committee, and patient informed consent was waived due to anonymous information used in the study.
FIGURE 1.
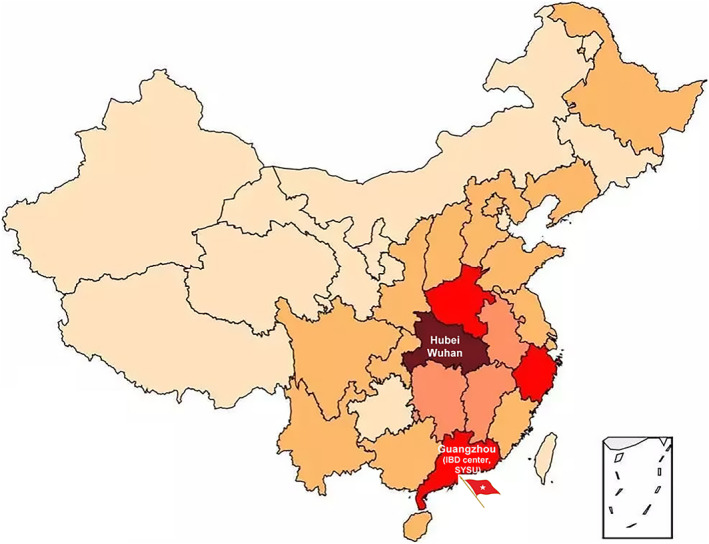
The number of confirmed patients with COVID‐19 in China. The red flag points to the location of inflammatory bowel disease (IBD) center, The First Affiliated Hospital of Sun Yat‐Sen University, Guangzhou, China. The shading from light to dark represents the number of patients with confirmed COVID‐19 on February 5, 2020 ( , > 10 000;
, > 10 000;  , 1000–9999;
, 1000–9999;  , 500–999;
, 500–999;  , 100–499;
, 100–499;  , 1–99). [Color figure can be viewed at wileyonlinelibrary.com]
, 1–99). [Color figure can be viewed at wileyonlinelibrary.com]
The study design was summarized in Figure 2. Given that Level 1 response to COVID‐19 designated by the government was initiated in Guangdong Province where our IBD unit is located on January 24, 2020, and the national vacation of Chinese Lunar New Year (Spring Festival) began on January 24th, we compared the data 1 month before and after 2020 Chinese New Year (December 25, 2019 to January 23, 2020 defined as 1 month pre‐outbreak vs January 31, 2020 to February 29, 2020 defined as 1 month post‐outbreak). For the historic comparison, data were also analyzed 1 month before and after 2019 Chinese New Year (January 5, 2019 to February 3, 2019 vs February 11, 2019 to March 12, 2019). There was no change in telemedicine care policy during the study period.
FIGURE 2.
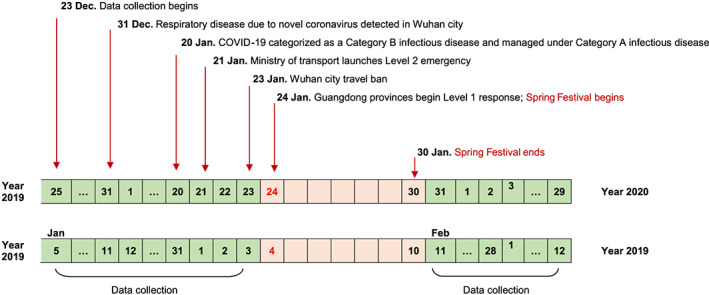
Study design, dates of COVID‐19, and the implementation of control measures in China. [Color figure can be viewed at wileyonlinelibrary.com]
Data collection and outcome measurement
The number of patients using different modes of health‐care delivery including standard face‐to‐face visit and telemedicine visit was collected before and after the outbreak of COVID‐19. In our IBD center, we have 1.5 days of IBD outpatient clinic unit each week, and we have telemedicine health care for our IBD patients including nurse‐led assisted smartphone care, care support based on social interactive app WeChat, and third‐party online telemedicine platforms such as HaoDaiFu. To counteract the potential challenge to health care of IBD patients due to COVID‐19 outbreak, clinician‐led online consultant was initiated in our hospital (a more formal hospital‐based online clinic) after the 2020 Spring Festival, providing not only an additional way for consultation but also drug prescriptions to maintain the treatment.
To investigate the impact of COVID‐19 outbreak on the health‐care needs of IBD patients, the consultation questions recorded on the telemedicine platforms 1 month before and after the COVID‐19 outbreak were analyzed by classifying into COVID‐19 related and non‐related ones.
Other information collected during the COVID‐19 outbreak included (i) the number of patients using steroid and immunomodulators including thiopurines and methotrexate; (ii) delay of infliximab (IFX) infusion, as the agent is the only biological agent approved in China until December 2019; (iii) delayed scheduled lab tests/endoscopy procedure and elective surgery; (iv) disease flare; (v) emergency room visit including emerging surgery because of disease flare or complication; (vi) patients reported COVID‐19‐related respiratory symptoms such as fever and cough; and (vii) diagnosis of COVID‐19.
Questionnaire survey on attitudes of physicians and patients towards telemedicine
To investigate the impact of COVID‐19 outbreak on attitudes of physicians and patients towards telemedicine, electronic questionnaire surveys were carried out among GI physicians and IBD patients in China (Appendix I). The questionnaire for the GI physicians was mainly focused on (i) percentage and modes of telemedicine used before and after the outbreak; (ii) whether they would change their way of practice with more telemedicine in the future; (iii) whether they are satisfied with currently used telemedicine platforms; and (iv) in which way the telemedicine should be improved. The percentage of telemedicine used among all provided patient care in each GI physician (standard face‐to‐face visit and telemedicine) was graded as <10%, 10–30%, 30–50%, and >50%.
The questionnaire for the IBD patients was focused on (i) the preference of telemedicine to standard face‐to‐face visit; (ii) whether they are willing to increase the use of telemedicine in the future; and (iii) in which way the telemedicine should be improved.
Statistical analysis
Categorical variables were expressed in frequencies and percentages. Continuous variables were expressed as mean and standard deviation or median and range. P values < 0.05 were considered to be statistically significant.
Results
Change in the health‐care mode before and after outbreak of COVID‐19
As demonstrated in Figure 3, the IBD outpatient clinic visit was similar during the 1 month before and after Spring Festival in 2019 (as comparator). However, in 2020, because of the outbreak of COVID‐19, patients' visit to the IBD clinic reduced substantially by 79% per person (from 249 to 51) and 80% per visit, respectively. On the contrary, the telemedicine visit was not reduced in the whole month after the outbreak of COVID‐19. Moreover, the opening of clinician‐led online consultant in our hospital had attracted 83 patients with a total of 93 e‐visits. In total, there were 414 and 409 patients using telemedicine visit during 1 month pre‐outbreak and post‐outbreak in 2020, compared with 93 and 151 in 2019 before and after Spring Festival, respectively.
FIGURE 3.
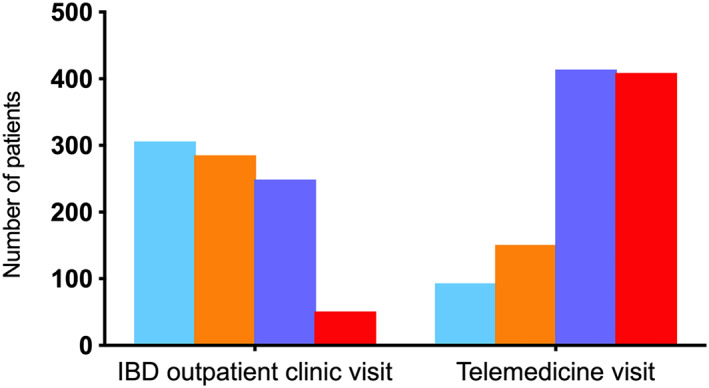
The number of patients using standard face‐to‐face visit and telemedicine visit (including smartphone message, WeChat App, and online consultant) during 1 month before and after Spring Festival in 2019 and 2020 ( , 1 month before 2019 Spring Festival;
, 1 month before 2019 Spring Festival;  , 1 month after 2019 Spring Festival;
, 1 month after 2019 Spring Festival;  , 1 month before 2020 Spring Festival;
, 1 month before 2020 Spring Festival;  , 1 month after 2020 Spring Festival). IBD, inflammatory bowel disease. [Color figure can be viewed at wileyonlinelibrary.com]
, 1 month after 2020 Spring Festival). IBD, inflammatory bowel disease. [Color figure can be viewed at wileyonlinelibrary.com]
Change in the health‐care needs of inflammatory bowel disease patients on telemedicine before and after outbreak of COVID‐19
To investigate the impact of COVID‐19 outbreak on the health‐care needs of IBD patients, we analyzed the consultant questions recorded on the telemedicine platforms 1 month before and after the COVID‐19 outbreak.
There were 414 versus 409 patients with a total of 748 versus 608 consultant questions during 1 month before and after outbreak of COVID‐19. The WeChat was preferred over the smartphone message (274 vs 140 pre‐outbreak and 248 vs 78 post‐outbreak). As detailed in Table 1, in addition to side effects of medications, the most inquired questions during 1 month post‐outbreak in 2020 were about medical adjustment including delay of lab test or colonoscopy or imaging evaluation, IFX infusion, drug delivery/accessibility, and disease flare. Consultation about coping strategies to COVID‐19 (COVID‐19‐related consultation) accounted for 38.5% (234/608) of all consultations. However, the majority of consultations during 1 month pre‐outbreak was about inquiry for lab results, concerns about drug‐related adverse effects, and IBD symptoms. The COVID‐19‐related consultations accounted for 0.9% (7/748) of all consultations during 1 month post‐outbreak compared with 38.5% (234/608) of all consultations during 1 month pre‐outbreak (P < 0.001).
TABLE 1.
Number of consultant questions recorded in telemedicine visit during 1 month before and after COVID‐19 outbreak
| COVID‐19 | Smartphone message | Online consultant | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | After | Before | After | |||
| Disease evaluation | Related | Delay of lab test | 0 | 0 | 0 | 4 | 0 | 0 | 4 |
| Delay of colonoscopy | 0 | 1 | 0 | 6 | 1 | 0 | 8 | ||
| Non‐related | Preparation for lab test | 1 | 0 | 5 | 2 | 0 | 6 | 2 | |
| Check for lab results | 3 | 1 | 22 | 9 | 0 | 25 | 10 | ||
| Interpreting lab results | 3 | 0 | 51 | 25 | 15 | 54 | 40 | ||
| Medication | |||||||||
| IFX | Related | Delay of IFX infusion | 0 | 12 | 0 | 17 | 3 | 0 | 32 |
| Non‐related | Make an appointment for infusion | 30 | 39 | 52 | 57 | 0 | 82 | 96 | |
| Policy about reimbursement | 32 | 34 | 65 | 24 | 0 | 97 | 58 | ||
| Others | 48 | 9 | 253 | 18 | 6 | 301 | 33 | ||
| Others | Related | Limited access to MTX injection | 0 | 1 | 0 | 4 | 2 | 0 | 7 |
| Alternative purchase approach | 0 | 8 | 0 | 71 | 37 | 0 | 116 | ||
| Drug withdrawal due to outbreak | 0 | 0 | 0 | 2 | 1 | 0 | 3 | ||
| Non‐related | Time of drug withdrawal | 0 | 0 | 2 | 1 | 5 | 2 | 6 | |
| Way of using drugs | 7 | 0 | 3 | 8 | 18 | 10 | 26 | ||
| Adverse events | 2 | 0 | 1 | 4 | 5 | 3 | 9 | ||
| Disease flare | Related | Selective surgery | 0 | 0 | 0 | 6 | 0 | 0 | 6 |
| Non‐related | Flare | 6 | 4 | 26 | 15 | 40 | 32 | 59 | |
| Emergency Operation | 0 | 0 | 0 | 2 | 1 | 0 | 3 | ||
| Hospitalization | 0 | 0 | 0 | 1 | 0 | 0 | 1 | ||
| Self‐management | Non‐related | Diet | 0 | 0 | 2 | 3 | 1 | 2 | 4 |
| Non‐related | Pregnancy/fertility | 0 | 0 | 1 | 3 | 2 | 1 | 5 | |
| Hospital visit | Related | Opening hours of IBD clinic | 0 | 7 | 0 | 13 | 2 | 0 | 22 |
| Self‐protection during hospital visit | 0 | 2 | 0 | 1 | 0 | 0 | 3 | ||
| Online clinic consulting | 0 | 0 | 0 | 5 | 2 | 0 | 7 | ||
| Non‐related | Appointment of hospitalization | 7 | 0 | 8 | 8 | 0 | 15 | 8 | |
| Visiting flow | 10 | 2 | 58 | 10 | 0 | 68 | 12 | ||
| Respiratory symptoms | Related | Cough | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Fever | 1 | 0 | 4 | 5 | 3 | 5 | 8 | ||
| Chest tightness | 0 | 0 | 0 | 2 | 1 | 0 | 3 | ||
| Rhinorrhea, sore throat | 0 | 0 | 2 | 1 | 0 | 2 | 1 | ||
| Travel | Related | Public transport | 0 | 2 | 0 | 1 | 1 | 0 | 4 |
| Self‐protection | 0 | 1 | 0 | 4 | 0 | 0 | 5 | ||
| Non‐related | 2 | 0 | 8 | 3 | 0 | 10 | 3 | ||
| Others | Non‐related | Insurance | 6 | 0 | 27 | 2 | 1 | 33 | 3 |
| Total | 158 | 124 | 590 | 337 | 147 | 748 | 608 | ||
IFX, infliximab; MTX, methotrexate.
Change in medications and procedures during the COVID‐19 outbreak
The adjustment of IBD management during the COVID‐19 outbreak was summarized in Table 2.
TABLE 2.
Impact of COVID‐19 outbreak on health care of patients with IBD during the 1 month after COVID‐19 outbreak
| n | Delayed time until infusion or surgery | |
|---|---|---|
| Routine evaluation delayed | ||
| Lab tests | 4 | |
| Colonoscopy | 8 | |
| MR enterography | 2 | |
| IFX infusion delayed † | 39 | 3.1 ± 1.9 weeks |
| Surgery | ||
| Elective surgery postponed | 6 | 43 (range 27–55) days |
| Emergency surgery | 3 | |
| Emergency department visit | 3 | |
| Disease flare | 14 | |
| Emergency visit | 3 | |
| Hospitalized | 7 | |
| Local hospital | 2 | |
| Our hospital | 5 | |
| Telemedicine provided care | 4 |
There are 59 patients with scheduled IFX infusion during the 1 month after the 2020 Spring Festival.
IBD, inflammatory bowel disease; IFX, infliximab; MR, magnetic resonance.
During the 1 month after outbreak of COVID‐19, 39 (39/56, 69.6%) patients had their IFX infusion postponed with the mean delayed time of 3 weeks. Among these 39 patients, five patients had disease relapse with symptoms and elevated C‐reactive protein. The trough level of four patients was subtherapeutic (< 3.5 μg/mL) with a median trough level of 0.4 μg/mL, and three patients had detectable antibody to IFX. However, the symptoms of all these patients were resolved after reinfusion of IFX.
There was one hospitalized patient with acute severe ulcerative colitis (UC) during the 1 month pre‐outbreak, and intravenous corticosteroid was given in this patient. No hospitalized patient with acute severe UC was reported during 1 month post‐outbreak. In the outpatient clinic, there were 22 and 9 patients using oral steroids during 1 month before and after the outbreak, respectively. In 2019, the number of patients on oral steroids was 24 and 12, respectively. Two hospitalized patients received intravenous corticosteroid due to acute severe UC during the 1 month before and after the 2019 Spring Festival, respectively.
The use of immunomodulators including thiopurine (150 vs 145) and methotrexate (21 vs 20) was similar between pre‐outbreak and post‐outbreak.
In addition, 47 patients (pre‐outbreak, n = 27 vs post‐outbreak, n = 20) had fecal calprotectin assays, showing a median of 47 (interquartile range 15–316) μg/g pre‐outbreak and 140 (interquartile range 15–307) μg/g post‐outbreak with no significant difference (P = 0.704).
Disease flare and management
Fourteen patients had disease flare. All of them utilized telemedicine via either message (n = 1) or WeChat (n = 5) or hospital‐based online clinic (n = 8). Supportive advices were given accordingly including medication prescriptions, hospitalize evaluation, or emergency room visit arrangement. As a result, seven of these patients were hospitalized (including two patients in local hospital), three had emergency visits, and four were managed by online clinic. Altogether, 84 patients (51 Crohn's disease, 26 UC, and 7 IBD unclassified) participated in a total of 147 online clinic consultations on hospital‐based online clinic. The majority of (48/147) consulting related to concern about disease flare. More importantly, 11/147 of these consultations were concerns about drug and/or test availability due to COVID‐19 outbreak. In the end, medical opinions including 29 drug prescriptions were given to 84 consulting patients.
Emergency room visit and emergent bowel surgery
Of the three patients who had an emergency room visit due to bowel perforation during the outbreak of COVID‐19, two underwent emergency bowel surgery at the local hospital, and the other one underwent the surgery in our hospital. Six elective surgeries were postponed for a median of 43 days (range 27–55 days), and all these six patients underwent surgery before the time that this manuscript was prepared.
COVID‐19‐related respiratory symptoms
As shown in Table S1, 15 patients reported respiratory symptoms including fever, cough, and chest tightness during the outbreak of COVID‐19. All the patients were ruled out to have COVID‐19 with negative nasopharyngeal swab test and chest computed tomography findings. None of IBD patients in our IBD center has been diagnosed with confirmed COVID‐19 to date.
Attitudes of gastrointestinal physicians towards telemedicine
Among the 297 GI physicians who finished the online questionnaire, 122 (41.08%) were IBD specialists with experience in IBD for more than 10 years, and 96 were from IBD centers with more than 500 IBD patients. There were 137 (46.13%) physicians using telemedicine to provide health care to IBD patients during the pre‐outbreak period. The three most commonly used platforms were WeChat (88, 64.23%), third‐party online clinic such as HaoDaiFu (81, 59.12%), and online clinic at their hospitals (38, 27.74%). In the post‐outbreak period, 193/297 (64.98%) of the surveyed physicians have used telemedicine with an increase of 18.9% compared with 46.13% (137/292) in the pre‐outbreak period (P < 0.001). WeChat and online clinic were still the most used platforms. An increase was observed both in hospital online clinic (84/193 vs 38/137, P = 0.003) and video clinic (21/193, 10.88% vs 5/137, 3.65%, P = 0.016) during post‐outbreak period compared with that in pre‐outbreak.
Importantly, 159 (53.54%) surveyed physicians agreed that the outbreak of COVID‐19 has changed the mode of clinical practice. As demonstrated in Figure 4, there is a significant change in both the amount (P < 0.001) and mode of telemedicine between the pre‐outbreak and post‐outbreak periods. Although 268 (90.24%) surveyed physicians still prefer standard face‐to‐face outpatient clinic visit to telemedicine (Fig. 5), 214 (72.05%) of them agreed that telemedicine should at least replace part of the clinic visit in the future.
FIGURE 4.
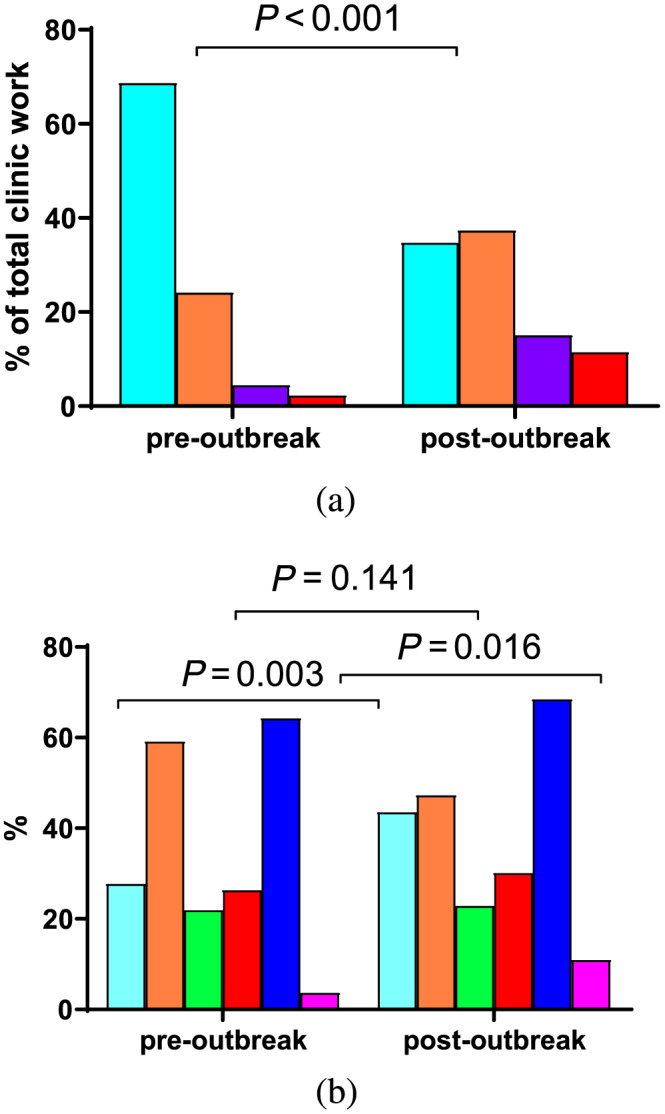
The change in (a) the percentage of telemedicine and (b) mode of telemedicine used by gastrointestinal physicians during pre‐outbreak and post‐outbreak periods according to survey ( , hospital online clinic;
, hospital online clinic;  , third‐party online clinic;
, third‐party online clinic;  , smartphone message;
, smartphone message;  , telephone;
, telephone;  , WeChat;
, WeChat;  , video). The percentage of telemedicine used among all provided patient care in each gastrointestinal physician (standard visit and telemedicine) was graded as (
, video). The percentage of telemedicine used among all provided patient care in each gastrointestinal physician (standard visit and telemedicine) was graded as ( ) < 10%, (
) < 10%, ( ) 10–30%, (
) 10–30%, ( ) 30–50%, and (
) 30–50%, and ( ) > 50%. [Color figure can be viewed at wileyonlinelibrary.com]
) > 50%. [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 5.
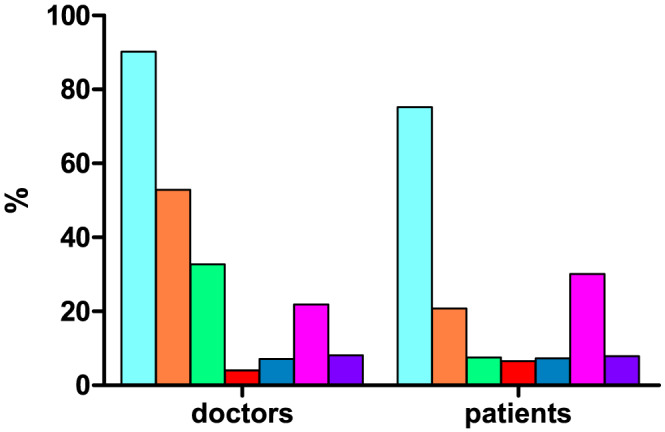
The preferred mode of health care during post‐outbreak reported by gastrointestinal physicians and inflammatory bowel disease patients according to survey ( , physical clinic visits;
, physical clinic visits;  , hospital online clinic;
, hospital online clinic;  , third‐party online clinic;
, third‐party online clinic;  , smartphone message;
, smartphone message;  , telephone;
, telephone;  , WeChat;
, WeChat;  , video). [Color figure can be viewed at wileyonlinelibrary.com]
, video). [Color figure can be viewed at wileyonlinelibrary.com]
Regarding the expected improvement in telemedicine in the future, 163 (54.88%) surveyed physicians voted for the removal of technology barrier, 203 (68.35%) voted for the flexibility of clinician's working mode, and 225 (75.76%) expected that telemedicine should be more covered by medical insurance.
Attitudes of inflammatory bowel disease patients towards telemedicine
Among the 505 IBD patients (354 Crohn's disease patients, 126 UC patients, and 25 IBD unclassified) who completed the online questionnaire, 380 patients (75.25%) prefer the standard face‐to‐face visit to telemedicine, while 125/505 (24.8%) patients prefer the telemedicine (Fig. 5); 331 (65.54%) patients supported that the use of telemedicine should be increased in future health care. There is a significant difference between older patients (≥ 40 years) and younger patients (< 40 years) (257/361, 71.2% vs 74/144, 51.4%, P < 0.001).
Regarding the expected improvement in future telemedicine, 301 (59.6%) patients hoped that more doctors will be available to provide telemedicine, while 214 (42.38%) patients thought that current telemedicine should be improved including insurance coverage and convenient drug delivery.
Discussion
Studies about the impact of COVID‐19 outbreak on management of IBD patients based on direct evidence are scarce. The IBD Unit in Milan firstly reported the strategy to deal with IBD during the pandemic including reorganization of IBD structure and patient education. 5 An early questionnaire study in Beijing, China, proposed that mobile communication applications, such as WeChat, is an effective method of information exchange. 6 Recently, the International Organization for the Study of Inflammatory Bowel Diseases issued practical statements about the management of patients with IBD during a pandemic, which emphasized that IBD patients should maintain remission to reduce the risk of recurrence and in‐depth medical treatment or hospitalization. 7 Our study investigated the impact of COVID‐19 outbreak on health care of IBD patients based on real‐setting data before and after the COVID‐19 outbreak, also incorporating a comparator data from the previous year.
Disasters and pandemics pose unique challenges to health‐care system, and telemedicine may be a virtually perfect solution to counteract the challenges in such a situation. 8 The landmark randomized clinical trial showed that telemedicine was safe and reduced outpatient visits and hospital admissions compared with standard care in patients with IBD. 9 Our study confirmed that patients tended to transit from standard care to telemedicine during the outbreak of COVID‐19. This was supported by our survey result in the physicians reporting an increase in the use of telemedicine during post‐outbreak compared with pre‐outbreak period.
The modes of telemedicine are variable among different countries. WeChat is the most widely used mobile social media in China and has profoundly integrated into the daily life of many Chinese people including health care. Our study showed that WeChat was the preferred method over the smartphone message and online consultant. In our center, a WeChat official account is operated by a full‐time nurse who is also responsible for IBD patients' daily follow‐up and consultation record management. Thanks to strict information security process and multiple patient information verification mechanisms, patients' personal information is stored securely. However, in our survey, video clinic was used during post‐outbreak period and pre‐outbreak period by only 10.88% (21/193) and 3.65% (5/137) of GI physicians. The optimal mode of telemedicine and the burden associated with the use of telemedicine for patients and providers need to be assessed in future studies. In addition, our study showed that both the majority of physicians and IBD patients prefer the standard face‐to‐face visit to telemedicine even after the pandemic outbreak, which implies that some barriers in the current telemedicine need to be overcome. Our survey provided some important insights to improve telemedicine such as more available physicians providing telemedicine, insurance for online health care, and further optimization of drug delivery system.
Limited data are available about the impact of medications including steroids, immunomodulators, and biologics on risk of COVID‐19 and outcomes in patients with IBD. However, it is agreed by the expert panel of International Organization for the Study of Inflammatory Bowel Diseases that it is safe to continue the current therapy except reducing dose of steroids as a preventive strategy in IBD patients without symptoms suggestive of COVID‐19. 7 Mazza et al. recently reported the first case of a COVID‐19 pneumonia in an elderly patient with severe acute UC treated with corticosteroids, and the patient died after 14 days of hospitalization. 10 The authors suggested to test for the virus before systemic steroid initiation in highly pandemic areas. Much attention and concern was focused on biologics infusion visit during the pandemic. The European Crohn's and Colitis Organisation (ECCO) taskforce group suggested that infusion could be delayed depending on the drug and the local conditions. For asymptomatic patients with normal fecal calprotectin and/or other biomarkers, IFX can be postponed to every 10 weeks. 11 The GEMINI trial shows that patients randomized from vedolizumab to placebo can maintain remission up to week 24; therefore, postponing vedolizumab to 4–8 weeks more than scheduled may be reasonable, according to local situations. 11 Our study showed that 39 (39/56, 69.6%) patients had their IFX infusion delayed during the 1 month after outbreak of COVID‐19, with the mean delayed time of 3 weeks. The symptoms of five patients with disease relapse were resolved after reinfusion of IFX. This is consistent with IFX withdrawal study in which response to retreatment with the same anti‐tumor necrosis factor agent was favorable. 12 However, in the five relapsed patients in our study, the trough level of four patients was subtherapeutic (< 3.5 μg/mL), and one patient had detectable antibody to IFX. Caution should be taken as a further dosing after delay may worsen immunogenicity in patients with biologic drug levels declining to undetectable level.
Our study has certain limitations. Firstly, this is a retrospective single‐center study performed in South China rather than Wuhan City, the epicenter of COVID‐19 outbreak in China. Future multicenter studies with comparison of IBD centers in Wuhan are warranted. Secondly, no patients with IBD have been reported to be infected with SARS‐CoV‐2 in the IBD Elite Union and the three largest tertiary IBD centers in Wuhan (Tongji Hospital, Union Hospital, and Zhongnan Hospital). Studies from Europe and USA with increasing number of IBD patients infected with SARS‐CoV‐2 (SECURE‐IBD registry) are important to evaluate the impact of COVID‐19 outbreak on patients with IBD in such regions. Last but not the least, IFX is the only biologics approved in China until December 2019. The availability of other biologics and its impact on health care in patients with IBD in the background of COVID‐19 remain to be clarified.
In conclusion, COVID‐19 resulted in a great change to health care in patients with IBD including decrease in standard face‐to‐face visit and delay of biologics use and surgery. There was an increased use and need of telemedicine after COVID‐19 outbreak. However, the telemedicine needs to be optimized towards a wider acceptance by IBD physicians and patients in China. Future post‐outbreak studies are important and needed to investigate the long‐term consequences of change in health care of patients with IBD due to outbreak of COVID‐19 and report whether some of these changes continue in the longer term.
Supporting information
Table S1. Summary of patients presented with respiratory symptoms during outbreak of COVID‐19.
Acknowledgment
None.
Appendix I. Impact of COVID‐19 on attitudes of physician and inflammatory bowel disease patient towards telemedicine
Questionnaire for doctors
【Before the COVID‐19 epidemic】
1. Before the outbreak of COVID‐19 (before 2020.1.23), did you ever diagnose or treat IBD patients through any online platforms?
A. Yes B. No
2. Before the outbreak of COVID‐19 (before 2020.1.23), which online platform did you use? (Multiple choices are available)
A. Internet platform built by hospital (e.g. cloud clinic)
B. Other internet platforms (e.g.)
C. Smartphone message consultation
D. Phone call consultation
E. Consultation on WeChat
F. Video consultation
G. Others _________ (describe please)
3. Before the outbreak of COVID‐19 (before 2020.1.23), how much did the online consultation compose of your total consultation (both online and offline)?
A. ≤ 10%
B. 10–30% (> 10%, ≤ 30%)
C. 30–50% (> 30%, ≤ 50%)
D. > 50%
[After the outbreak of COVID‐19]
4. Since the outbreak of COVID‐19 (since 2020.1.24), have you ever used an online internet platform to diagnose and treat IBD patients?
A. Yes B. No
5. Since the outbreak of COVID‐19 (since 2020.1.24), which online platform have you used? (Multiple choices are available)
A. Internet platform built by hospital (e.g. cloud clinic)
B. Other internet platforms (e.g.)
C. Smartphone message consultation
D. Phone call consultation
E. Consultation on WeChat
F. Video consultation
G. Others _________ (describe please)
6. After the outbreak of COVID‐19 (after 2020.1.24), how much did the online consultation compose of your total consultation (both online and offline)?
A. ≤ 10%
B. 10–30% (> 10%, ≤ 30%)
C. 30–50% (> 30%, ≤ 50%)
D. > 50%
7. During the COVID‐19 epidemic, did you have any IBD patients diagnosed with COVID‐19?
A. Yes (The number of cases __) B. No
【Expectations after the epidemic】
8. Has this epidemic changed your way of consultation?
A. Yes B. No
9. Which way of consultation would you prefer in the future? (Multiple choices are available)
A. Face‐to‐face consultation in hospital outpatient clinics
B. Internet platform built by hospital (e.g. cloud clinic)
C. Other internet platforms (e.g.)
D. Smartphone message consultation
E. Phone call consultation
F. Consultation on WeChat
G. Video consultation
H. Others _________ (describe please)
10. Do you want the online Internet platform to replace the offline hospital clinic?
A. Yes.
B. No.
C. Partial replacement is OK.
11. In your opinion, how much proportion of your online consultation accounted for your total consultation (online + offline) would be appropriate?
A. ≤ 10%
B.10–30% (> 10%, ≤ 30%)
C. 30–50% (> 30%, ≤ 50%)
D. > 50%
12. In your opinion, which aspects of the existing online internet platform need to be improved most to meet future needs?
A. Technical level
B. Patient acceptance
C. Increasing flexibility of the doctor's work mode
D. Subsequent medical‐insurance‐related measures for online medical treatment
E. Others _________ (describe please)
【General information】
13. What is your profession?
A. General digestive physician
B. IBD‐specialized physician (mainly serving for IBD patients)
C. IBD‐specialized surgeon (specializing in surgical treatment of IBD patients)
D. IBD‐specialized nurse
14. What is your current title?
A. No title B. Junior C. Intermediate D. Deputy Senior E. Senior
15. How many years of your experience in diagnosing and treating IBD patients?
A. ≤ 3 years
B. 3–5 years (> 3, ≤ 5)
C. 5–10 years (> 3, ≤ 10)
D. > 10 years
16. How many IBD patients in your IBD center?
A. ≤ 100
B. 100–500 (> 100, ≤ 500)
C. 500–1000 (> 500, ≤ 1000)
D. 1000–3000 (> 1000, ≤ 3000)
E. > 3000
Questionnaire for patients with inflammatory bowel disease
[General information]
1. What is your current diagnosis?
A. Crohn's disease B. Ulcerative colitis C. Others__________(describe please)
2. What is your gender?
A. Male B. Female
3. How old are you?
A. ≤ 16 years old
B. 16–40 years old (> 16 years old, ≤ 40 years old)
C. 40–65 years old (> 40 years old, ≤ 65 years old)
D. >65 years old
4. What is your residential address?
_______ Province _________City__________________.
5. How long have you been diagnosed with inflammatory bowel disease?
A. ≤ 2 years
B. 2–5 years (> 2 years, ≤ 5 years)
C. 5–10 years (> 5 years, ≤ 10 years)
D. > 10 years
6. How long has it been since your last visit to hospital? (until 2020.04)
A. ≤ 3 months
B. 3–6 months (> 3 months, ≤ 6 months)
C. 6–12 months (> 6 months, ≤ 12 months)
D. > 12 months
[Before the outbreak of COVID‐19]
7. How did you get medical treatment one month before the outbreak of COVID‐19 epidemic (2019.12.25‐2020.1.23)? (Multiple choices are available)
A. Outpatient clinics in hospital
B. Emergency clinics in hospital
C. Internet platform built by hospital (e.g. cloud clinic)
D. Other Internet platforms (e.g.)
E. Smartphone message consultation
F. Phone call consultation
G. Consultation on WeChat
H. Video consultation
I. None
J. Others_________ (describe please)
[After the outbreak of COVID‐19]
8. Could you purchase medicine in time one month after the outbreak of the COVID‐19 epidemic? (2020.1.24‐2020.2.29)?
A. Yes B. No C. Not purchased due to enough medicine
9. How did you get drugs one month after the outbreak of the COVID‐19 epidemic in 2020 (2020.1.24–2020.2.29)? (Multiple choices are available)
A. Prescribed from outpatient clinics in hospital
B. Prescribed from emergency clinics in hospital
C. Purchased in pharmacies
D. Purchased on the Internet platform (Taobao, Jianke, etc.)
E. Purchased by relatives
F. Not purchased due to sufficient amount of medicine
G. Others_________ (describe please)
10. How did you get medical treatment one month after the outbreak of COVID‐19 epidemic in 2020 (2020.1.24‐2020.2.29)? (Multiple choices are available)
A. Outpatient clinics in hospital
B. Emergency clinics in hospital
C. Internet platform built by hospital (e.g. cloud clinic)
D. Other Internet platforms (e.g.)
E. Smartphone message consultation
F. Phone call consultation
G. Consultation on WeChat
H. Video consultation
I. None
J. Others_________ (describe please)
11. How many times did you use the Internet platform (WeChat, SMS, cloud clinic, etc.) for consultation one month after the outbreak of the COVID‐19 epidemic (2020.1.24‐2020.2.29)?
A. ≤ 2 times B. 2–5 times (> 2 times, ≤ 5 times) C. > 5 times
[Expectations after the COVID‐19 epidemic]
12. Which way of consultation would you prefer after the epidemic?
A. Face‐to‐face consultation in hospital outpatient clinics
B. Internet platform built by hospital (e.g. cloud clinic)
C. Other internet platforms (e.g.)
D. Smartphone message consultation
E. Phone call consultation
F. Consultation on WeChat
G. Video consultation
H. Others _________ (describe please)
13. Would you like online ways provided for diagnosis and treatment after the epidemic?
A. Yes B. No C. Not sure
14. In your opinion, which aspects of the existing online platforms need to be improved to meet future needs? (Multiple choices are available)?
A. Improvement in internet platform technology
B. More doctors providing diagnosis and treatment services on the Internet
C. Subsequent medical‐insurance‐related measures for online medical treatment
D. Improvement in relevant inspections and drug distribution system
E. _________ (describe please)
Zhang, Y.‐F. , Qiu, Y. , He, J.‐S. , Tan, J.‐Y. , Li, X.‐Z. , Zhu, L.‐R. , Chen, Y. , Liu, Z.‐J. , Iacucci, M. , Chen, B.‐L. , He, Y. , Ben‐Horin, S. , Shen, B. , Zeng, Z.‐R. , Ghosh, S. , Chen, M.‐H. , and Mao, R. (2021) Impact of COVID‐19 outbreak on the care of patients with inflammatory bowel disease: A comparison before and after the outbreak in South China. Journal of Gastroenterology and Hepatology, 36: 700–709. 10.1111/jgh.15205.
Declaration of conflict of interest: All authors declared no conflict of interest.
Author contribution: R. M., S. G., and M. H. C. conceived the study. R. M. and M. H. C. supervised the overall study. R. M., Y. F. Z., and Y. Q. wrote the manuscript. R. M., Y. F. Z., Y. Q., J. S. H., J. Y. T., X. Z. L., L. R. Z., Y. C., Z. J. L., and B. S. analyzed the data. M. I., B. S., S. B.‐H., and S. G. critically revised the manuscript.
Financial support: None.
Contributor Information
Min‐Hu Chen, Email: chenminhu@mail.sysu.edu.cn.
Ren Mao, Email: maoren2023@gmail.com.
References
- 1. Brenner EJ, Ungaro RC, Colombel JF, Kappelman MD. SECURE‐IBD database public data update. Accessed on 04/20/2020.
- 2. Ng SC, Shi HY, Hamidi N et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population‐based studies. Lancet 2018; 390: 2769–2778. [DOI] [PubMed] [Google Scholar]
- 3. Hudesman DP, Chakravarty SD, Emond B et al. Healthcare resource utilization and costs associated with inflammatory bowel disease among patients with chronic inflammatory diseases: a retrospective cohort study. BMC Rheumatol. 2020. Apr 2; 4: 16. 10.1186/s41927-020-0115-2 eCollection 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mao R, Chen MH. Networked clinical study collaboration on inflammatory bowel disease in China. Am. J. Gastroenterol. 2018; 113: 1266. [DOI] [PubMed] [Google Scholar]
- 5. Fiorino G, Allocca M, Furfaro F et al. Inflammatory bowel disease care in the COVID‐19 pandemic era: the Humanitas, Milan experience. J. Crohns Colitis 2020. Mar 24. 10.1093/ecco-jcc/jjaa058 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bai X, Yang H, Qian J. COVID‐19 outbreak and inflammatory bowel disease management: a questionnaire survey from realistic practice. J. Crohns Colitis 2020. Mar 28. 10.1093/ecco-jcc/jjaa064 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rubin DT, Feuerstein JD, Wang AY, Cohen RD. AGA clinical practice update on management of inflammatory bowel disease during the COVID‐19 pandemic: expert commentary. Gastroenterology 2020. Apr 10. pii: S0016–5085: 30482–30490. 10.1053/j.gastro.2020.04.012 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid‐19. N. Engl. J. Med. 2020. [DOI] [PubMed] [Google Scholar]
- 9. de Jong MJ, van der Meulen‐de Jong AE, Romberg‐Camps MJ et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet 2017; 390: 959–968. [DOI] [PubMed] [Google Scholar]
- 10. Mazza S, Sorce A, Peyvandi F, Vecchi M, Caprioli F. A fatal case of COVID‐19 pneumonia occurring in a patient with severe acute ulcerative colitis. Gut 2020. Apr 3. pii: gutjnl‐2020‐321183. 10.1136/gutjnl-2020-321183 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11. Zhu LR, Mao R, Fiorino G, Schneider T. 2nd interview COVID‐19 ECCO taskforce, Published March 20, 2020.
- 12. Gisbert JP, Marín AC, Chaparro M. The risk of relapse after anti‐TNF discontinuation in inflammatory bowel disease: systematic review and meta‐analysis. Am. J. Gastroenterol. 2016. May; 111: 632–647. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary of patients presented with respiratory symptoms during outbreak of COVID‐19.


