Abstract
Background
Severe respiratory failure patients with coronavirus disease (COVID‐19) sometimes do not receive post‐intensive care syndrome prevention bundles. No detailed report has been published on the practical observations of mental impairments in these patients.
Case presentation
A 33‐year‐old man was admitted with COVID‐19 pneumonia. On day 6, he was admitted to the intensive care unit (ICU). Considering the risk of nosocomial infection, as per the hospital policy, early rehabilitation could not be initiated for COVID‐19 patients at that time and family visits were not allowed. Thereafter, his respiratory condition gradually improved; he was discharged on day 19. When the ICU nurse called to assess his medical condition, the patient complained of insomnia after ICU discharge. Therefore, we called him for an outpatient visit 28 days after discharge and scored his mental health status.
Conclusion
Careful follow‐up is required to treat mental impairment in patients with COVID‐19.
Keywords: COVID‐19, post‐intensive care syndrome, post‐traumatic stress disorder
Patients with COVID‐19 generally do not receive post‐intensive care syndrome prevention bundle. Careful follow‐up is required to treat post‐intensive care syndrome in patients with COVID‐19.

INTRODUCTION
Patients with coronavirus disease (COVID‐19)‐related severe respiratory failure are frequently treated with deep sedation, as well as using neuromuscular blockades (NMBs) and steroids. 1 These approaches can cause post‐intensive care syndrome (PICS). 2 Moreover, family visits are strictly restricted when patients are still at a high risk of causing contagion. 3 Early rehabilitation sometimes cannot be initiated due to the risk of nosocomial infections. Thus, severe respiratory failure patients with COVID‐19 sometimes do not receive the PICS prevention bundle, which is commonly applied in standard intensive care unit (ICU) practice. 4
Several action/management plans for PICS prevention in patients with COVID‐19 are proposed; 5 , 6 however, details of mental impairment in practically observed cases have remained unreported.
Here, we report a COVID‐19 case that developed an impaired mental health status following ICU care. We also emphasize the significance of follow‐up in these patients.
CASE REPORT
A 33‐year‐old male magazine editor was admitted because of COVID‐19 pneumonia. He had no medical history, such as alcohol dependence or mental disorders, and he lives with his wife and a 1‐year‐old son. Oxygen demand was not observed on the admission day, but the oxygen saturation level eventually dropped. On day 6, he had prominent tachypnea despite having a reservoir mask delivering 8 L/min of oxygen. Hence, he underwent emergency tracheal intubation and was admitted to the ICU. Weak sedation was maintained during ICU management. No steroids or NMB was given. Considering the concern about nosocomial infection in the hospital policy, early rehabilitation in patients with COVID‐19 could not be initiated at that time. Family visits were also prohibited for the same reason. Subsequently, his respiratory condition gradually improved, and he was extubated on day 8, left the ICU on day 9, and was finally discharged on day 19. Before discharge, he was slightly worried about infecting his family. When the ICU nurse examined his medical condition, the patient said, “When I try to sleep, I can’t sleep because I remember the ICU stay,” “The news that a popular comedian died from coronavirus made me feel anxious and scared,” and “It’s hard to see people die while playing games.” Therefore, in his outpatient visit 28 days after discharge, we assessed his mental status. In the Post‐traumatic Stress Diagnostic Scale, the patient met the post‐traumatic stress disorder (PTSD) criteria (Fig. 1A). Thereafter, under psychiatric consultation, we evaluated his mental status by using the Hospital Anxiety and Depression Scale and the Impact of Event Scale – Revised. On the same day, the psychiatrist prescribed etizolam. Although the psychiatric symptoms gradually improved, he was still diagnosed with PTSD because the symptoms, based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, continued for more than 1 month. Then, 46 days after discharge, the scoring improved compared with the scoring 28 days after discharge (Fig. 1B). He continues to be an outpatient of our hospital.
Fig. 1.
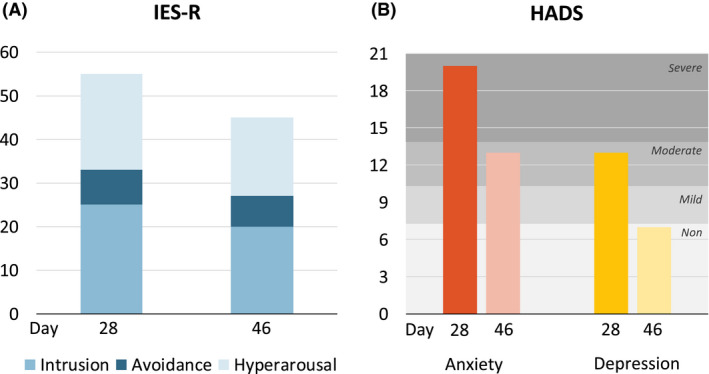
Changes in (A) Impact of Event Scale – Revised (IES‐R) and (B) Hospital Anxiety and Depression Scale (HADS) over time in a 33‐year‐old man following treatment for COVID‐19 in an intensive care unit.
DISCUSSION
Our patient with COVID‐19 who received ICU care developed PTSD after discharge. Through close observation with appropriate medication and frequent medical interview, his PTSD improved.
To the best of our knowledge, mental impairment after ICU care in patients with COVID‐19 has remained unreported. A recently published a systematic review and meta‐analysis regarding psychiatric and neuropsychiatric presentations associated with severe coronavirus infections reported that the prevalence of depression, anxiety, PTSD, and fatigue might be high in these patients; however, to date, data on these diagnoses in patients with COVID‐19 are preliminary or unpublished. 7 With regard to risk factors, in a systematic review by Davydow et al., 8 it was reported that female sex is a significant predictor of PTSD after ICU care. Pre‐existing depression, anxiety, PTSD, and alcohol abuse as well as lower education level increase the risk of ICU‐acquired mental illness. 8 Although these risks were not observed our patient, he still developed severe PTSD.
Regarding the mechanism of the development of impaired mental status, no deep sedation, steroids, or NMB was used for this patient. However, neither family visits nor early rehabilitation were provided because of the concern of COVID‐19 nosocomial infection. Moreover, undesirable TV news, such as the COVID‐19‐related death of celebrities, might have contributed to his PTSD. Thus, early rehabilitation is mandatory to reduce PICS. 9
We carefully observed the mental status of our patient after discharge. After interview over the telephone, we scheduled him for outpatient appointments. In the outpatient clinic, we discussed his current mental state and evaluated the symptoms using several scales. Given that no outpatient practice is covered by any insurance in Japan to follow up on the progress of PICS, during his telephone interview we urged the patient to come to the hospital regularly for drug prescription and mental status evaluation. According to a national survey in Japan, only 7% of respondents said that a system exists for following up the long‐term outcomes of patients after ICU discharge. 10 To actually follow‐up patients’ long‐term outcomes at medical institutions, health‐care providers need to resolve various issues, such as securing costs and actual medical booths, in collaboration with other hospital departments (especially the psychiatry department, which is an important department for PICS), and secure nurses and physicians for medical care. Establishing a follow‐up system for the long‐term outcomes of patients after ICU discharge enables the evaluation of long‐term outcomes in current treatments. The limitation of the present study is that neither physical disabilities nor cognitive impairment were evaluated, and that PICS following COVID‐19 infection was not comprehensively described.
CONCLUSION
Careful follow‐up is required to treat PTSD in patients with COVID‐19. Further actual condition evaluation, prevention, treatment, and follow‐up activities for mental disorders should be systematically developed in actual clinical practice to improve the long‐term prognosis of patients with COVID‐19 who underwent ICU treatment.
DISCLOSURE
Approval of the Research Protocol: N/A.
Informed Consent: Written informed consent was obtained from the patient.
Registry and the Registration No. of the study/trial: N/A.
Animal Studies: N/A.
Conflict of Interest: None.
Funding information
No funding information provided.
References
- 1. Alhazzani W, Moller MH, Arabi YM et al Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID‐19). Intensive Care Med. 2020; 48: e440–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Needham DM, Davidson J, Cohen H et al Improving long‐term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit. Care Med. 2012; 40: 502–9. [DOI] [PubMed] [Google Scholar]
- 3. Rosa RG, Falavigna M, da Silva DB et al Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU visits randomized clinical trial. JAMA 2019; 322: 216–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Inoue S, Hatakeyama J, Kondo Y et al Post‐intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019; 6: 233–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kotfis K, Williams Roberson S, Wilson JE, Dabrowski W, Pun BT, Ely EW. COVID‐19: ICU delirium management during SARS‐CoV‐2 pandemic. Crit. Care 2020; 24: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stam HJ, Stucki G, Bickenbach J. Covid‐19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020; 52: jrm00044. [DOI] [PubMed] [Google Scholar]
- 7. Rogers JP, Chesney E, Oliver D et al Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta‐analysis with comparison to the COVID‐19 pandemic. Lancet Psychiatry 2020; 7: 611–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen. Hosp. Psychiatry 2008; 30: 421–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fuke R, Hifumi T, Kondo Y et al Early rehabilitation to prevent postintensive care syndrome in patients with critical illness: a systematic review and meta‐analysis. BMJ Open 2018; 8: e019998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The committee on PICS management and improvement of quality of life JSoICM . A questionnaire survey regarding recognition and clinical practice of post‐inten‐ sive care syndrome in Japan. J. Jpn. Soc. Intensive Care Med. 2019; 26: 467–75. [Google Scholar]


