Abstract
Objective
To evaluate the impact of COVID‐19 pandemic migitation measures on of ST‐elevation myocardial infarction (STEMI) care.
Background
We previously reported a 38% decline in cardiac catheterization activations during the early phase of the COVID‐19 pandemic mitigation measures. This study extends our early observations using a larger sample of STEMI programs representative of different US regions with the inclusion of more contemporary data.
Methods
Data from 18 hospitals or healthcare systems in the US from January 2019 to April 2020 were collecting including number activations for STEMI, the number of activations leading to angiography and primary percutaneous coronary intervention (PPCI), and average door to balloon (D2B) times. Two periods, January 2019–February 2020 and March–April 2020, were defined to represent periods before (BC) and after (AC) initiation of pandemic mitigation measures, respectively. A generalized estimating equations approach was used to estimate the change in response variables at AC from BC.
Results
Compared to BC, the AC period was characterized by a marked reduction in the number of activations for STEMI (29%, 95% CI:18–38, p < .001), number of activations leading to angiography (34%, 95% CI: 12–50, p = .005) and number of activations leading to PPCI (20%, 95% CI: 11–27, p < .001). A decline in STEMI activations drove the reductions in angiography and PPCI volumes. Relative to BC, the D2B times in the AC period increased on average by 20%, 95%CI (−0.2 to 44, p = .05).
Conclusions
The COVID‐19 Pandemic has adversely affected many aspects of STEMI care, including timely access to the cardiac catheterization laboratory for PPCI.
Keywords: COVID‐19, ST‐elevation myocardial infarction, STEMI
1. INTRODUCTION
The coronavirus 2019 (COVID‐19) pandemic has significantly impacted healthcare delivery around the globe. 1 , 2 To preserve hospital beds and intensive care unit capacity, elective cardiovascular procedures have been canceled or postponed, and access to in‐person outpatient clinics have been severely restricted. 3
An unexpected and troublesome decline in the number of patients seeking medical care for cardiovascular emergencies has been reported during the early phase of the pandemic. 4 , 5 Concomitantly, the number of patients suffering cardiac arrest at home has significantly increased in areas most affected by COVID‐19. 6 , 7 Taken together, these observations suggest that many patients with acute cardiovascular conditions may be circumventing needed medical care. We previously reported a 38% decline in cardiac catheterization laboratory activations for ST‐segment elevation myocardial infarction (STEMI) in 9 high‐volume STEMI centers in the early phase of the Pandemic. 8 The purpose of this investigation is to extend and expand on our early observations by (a) including 18 hospitals or healthcare systems representative of different regions of the US with varying COVID‐19 incidence rates, (2) analyzing other metrics relevant to STEMI care including the number of cardiac catheterization laboratory activations leading to angiography and primary percutaneous coronary intervention (PPCI), and door to balloon (D2B) times, and (3) continuation of our analysis of STEMI decline into April 2020, including a comparison with March 2020 to assess novel trends.
2. METHODS
A total of 18 sites representing PPCI hospitals and healthcare systems across the US were included in the study (Table S1 and Figure S1). In this study, March 1, 2020, was identified as the date when US medical operations were significantly affected. It was also the day that New York City, the current epicenter of the US pandemic, reported its first COVID‐19 case through social distancing was not recommended by the federal government until March 15th. Therefore, we identified two periods before and after March 1, 2020, and label them as BC and AC, accordingly. The BC period encompasses the 14 months from January 1, 2019, to February 29, 2020. The AC period includes March and April of 2020.
Data on monthly volumes of cardiac catheterization laboratory activations for STEMI, cardiac catheterization laboratory activations leading to angiography, and PPCI were collected. In addition, monthly mean door‐to‐balloon (D2B) times (in minutes) were collected for each study site. Since COVID‐19 cases in the US initially clustered in the Tri‐state area in the Northeast of the US, we grouped STEMI programs into four geographic regions (Northeast, South, West, and Midwest) to account for potential differential effects according to COVID‐19 disease burden and testing (Table S2).
Continuous study variables were summarized using median and interquartile ranges (median Q1, Q3). For each response variable, the change in volumes at AC from BC were estimated using a generalized estimating equations approach to account for within‐site dependencies. Poisson models were used for variables reflecting procedural volumes (STEMI, angiography, and PCI), and a Gaussian distribution was used to estimate changes in the door to balloon times (log scale). The covariates in each model included a natural cubic spline to adjust for seasonal trends, an indicator variable for the year, categorical variable for the region, and an indicator variable for influenza epidemics (October–April). The COVID pandemic period was either coded as an indicator for BC/AC or a three‐level categorical variable (BC, March 2020, April 2020). The estimates are reported either as percent change from baseline or incidence rate ratios (IRR) together with the 95% confidence intervals (CI) and p‐values. The analysis was conducted using R v4.0 in the Rstudio environment (Rstudio Inc.). No Institutional review board (IRB) approval was required to conduct this survey of the cardiac catheterization laboratory during the COVID‐19 Pandemic.
3. RESULTS
Summary statistics in Table 1 indicate a reduction in cardiac catheterization laboratory activations and procedural volumes for STEMI in the AC period relative to baseline BC period. The overall median number of monthly cardiac catheterization laboratory activations decreased from 22 procedures in BC to 13 and 17 in March and April 2020, respectively (Table 1, Figures 1 and S2). The reduction in STEMI activation volumes from BC was observed in all four regions (Figure 1). Nearly all participating sites experienced reductions in STEMI activation volumes in March 2020 relative to BC (Figure 1). The data also indicate sizeable variations in STEMI activations from March to April 2020, even within the same geographic region, with some STEMI programs returning to prepandemic levels (e.g., Iowa Heart, Christ Hospital, Northwell, Swedish), some remaining suppressed (e.g., MHI, NY Presbyterian, MGH) and others having volumes decline even further (e.g., BHC, UPenn, NYU Langone, Delray, San Diego; Figure 2).
TABLE 1.
Median (Q1, Q3) for response variables by time period for participating STEMI programs (n)
| Variable | Before COVID | March 20 | April 20 |
|---|---|---|---|
| STEMI activations, n = 18 | 22 (14, 28) | 13 (7, 26) | 17 (6, 24) |
| STEMI angiography, n = 12 | 12 (7, 17) | 8 (4, 11) | 8 (1, 14) |
| Primary PCI, n = 13 | 8 (9, 15) | 6 (4, 10) | 7 (4, 11) |
| Median D2B, min, n = 12 | 70 (61, 75) | 70 (66, 95) | 87 (57, 99) |
Abbreviations: D2B, door to balloon time; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction.
FIGURE 1.
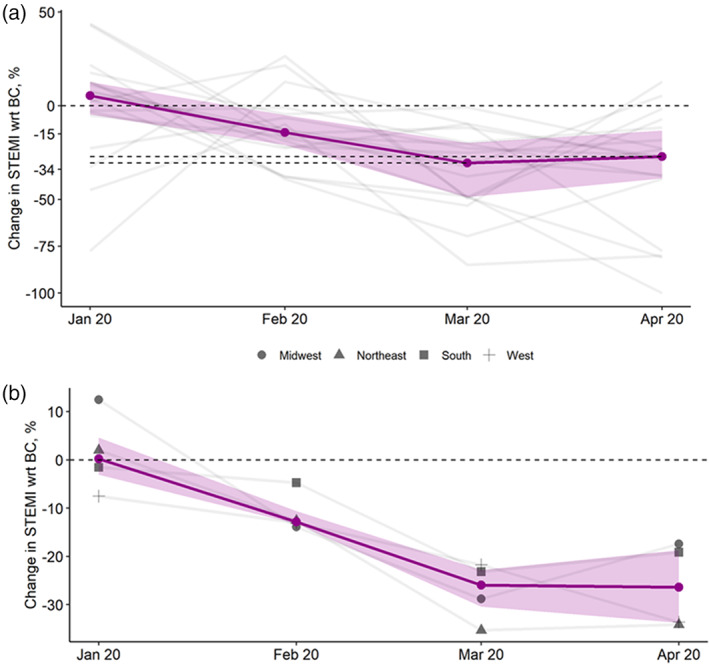
Changes in cardiac catheterization laboratory ST‐elevation myocardial infarction activations for each program (gray lines) relative to their respective mean BC volumes (Panel A) and Changes in cardiac catheterization laboratory ST‐elevation myocardial infarction activations according to geographic regions (gray lines) relative to their respective BC volumes (Panel B). The purple line represents the overall median. The band represents interquartile ranges [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
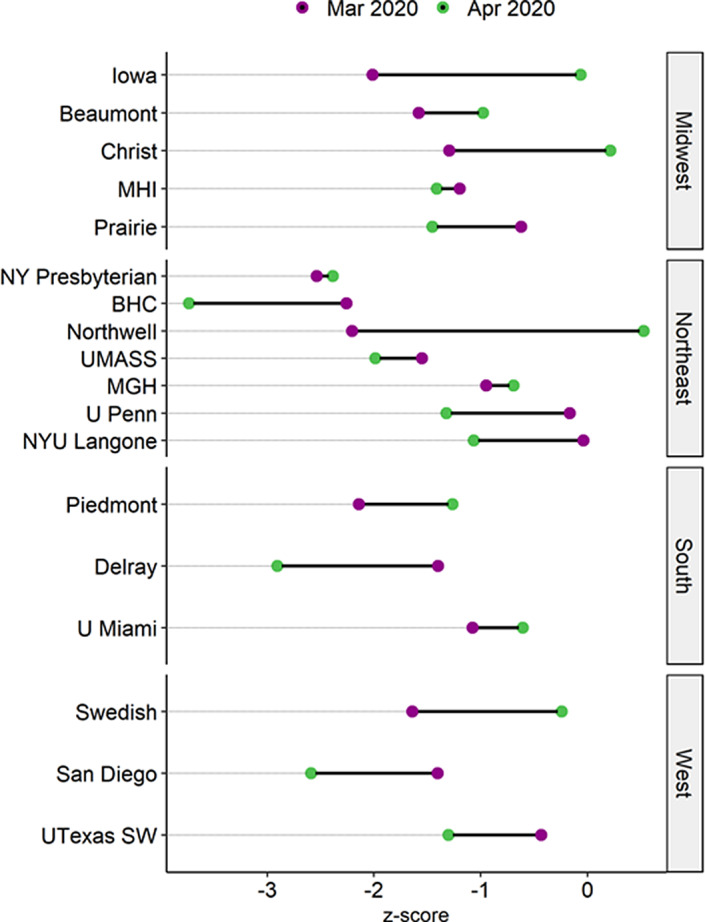
A dumbbell plot of Z‐scores showing changes in cardiac catheterization laboratory ST‐elevation myocardial infarction activations for each program. Units are standard deviations from their BC means, for example, Z‐score = 0 indicates that the volume at a given month in 2020 is identical to the mean BC volume. A negative Z‐score indicates a decline in units of standard deviations from their mean BC volumes. All programs saw a decline in March 2020 (Z‐scores marked by purple dots are all negative) with some recovering in April to nearly 2019 volumes (e.g., Iowa, Christ Hospital, Northwell, Swedish) and others either nearly unchanged (e.g., NY Presbyterian, MHI, MGH) or worsening (Prairie, Delray, BHC, U Penn, San Diego). BC, before COVID‐19 [Color figure can be viewed at wileyonlinelibrary.com]
Relative to the BC period, the estimated average reduction in cardiac catheterization laboratory activations in the AC period was 29%, 95% CI: (18, 38), p < .001. There was no apparent change in STEMI activation volumes in April 2020 relative to March 2020: IRR = 0.96, 95% CI: (0.81, 1.14), p = .67.
Information on cardiac catheterization laboratory STEMI activations leading to coronary angiography was available from 12 sites. The median monthly volumes of angiographies for STEMI decreased from 12 in the BC period to 8 in both March and April 2020 (Table 1 and Figure 3). The estimated reduction in AC volumes relative to BC was 34%, 95% CI: (12, 50), p = .005. The March 2020 volumes fell on average 20%, 95% CI: (0, 36), p = .053 from the BC period and the April volumes fell further by 30%, 95% CI: (5, 48), p = .022 relative to March. The reduction in angiography volumes appeared to be driven by a decline in STEMI activations; when adjusted for the latter, the estimated IRR = 0.07, 95%CI (−0.28, 0.41), p = .693.
FIGURE 3.
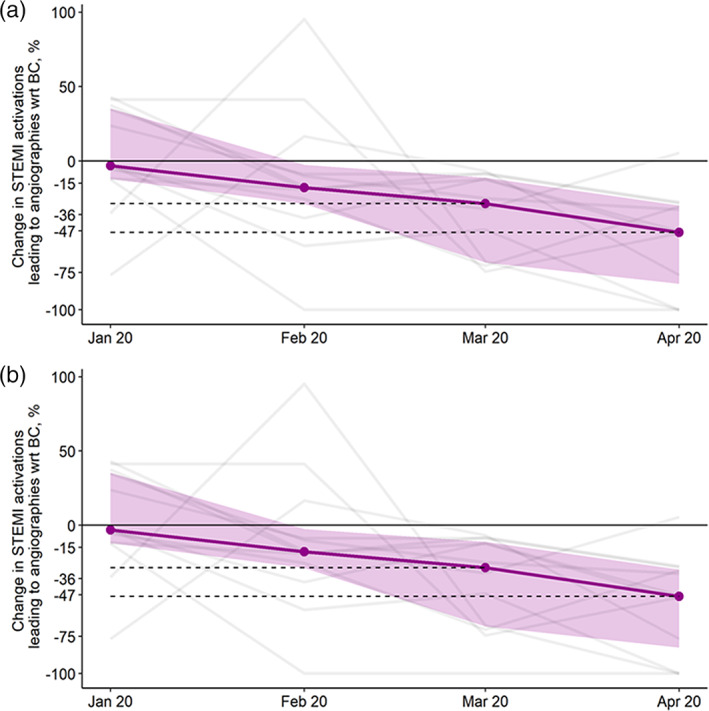
Changes in cardiac catheterization laboratory ST‐elevation myocardial infarction activations leading to angiographies for each program (gray lines) (Panel A) and leading to percutaneous coronary intervention (Panel B) relative to their respective average BC volumes. The purple line represents the overall median. The band represents interquartile ranges. BC, before COVID‐19 [Color figure can be viewed at wileyonlinelibrary.com]
Information on cardiac catheterization laboratory STEMI activations leading to PPCI was available from 12 sites. The median volume of PPCI fell from 8 procedures in the BC period to 6 and 7 in March and April 2020, respectively (Table 1 and Figure 3). The estimated reduction in PPCI volumes in the AC period from BC was 20%, 95% CI: (11, 27), p < .001. When controlled for STEMI activations, the estimated incidence ratio relative to the BC period was IRR = 0.21(−0.06, 0.48), p = .123.
Information on D2B times was available from 12 sites. The data indicated an increase in D2B (Table 1, Figure 4). The increase in D2B times in AC relative to BC was 20%, 95% CI: (−0.2, 44), p = .052. On average, D2B times in March 2020 relative to BC increased by 27%, 95% CI: (6, 52), p = .011 with no apparent change in D2B in April 2020; −11%, 95% CI: (−31, 13), p = .314.
FIGURE 4.
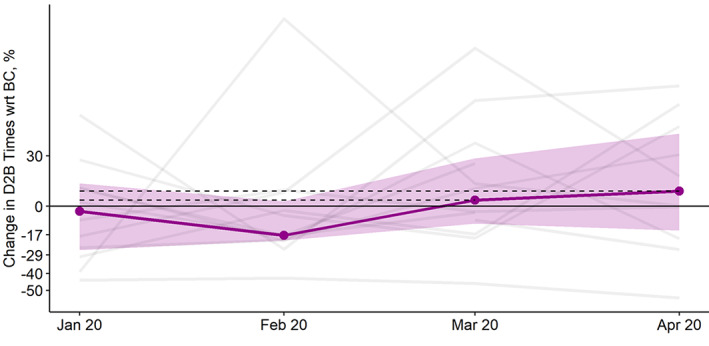
Changes in median door to balloon times for each program (gray lines) relative to their respective average BC volumes. The purple line represents the overall median. The band represents interquartile ranges. BC, before COVID‐19 [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
Our expanded analysis of the impact of COVID‐19 Pandemic on STEMI care has several key findings. First, the decline in cardiac catheterization laboratory activations for STEMI has persisted into April 2020, with some programs showing signs of recovery while others remain significantly below their 2019 averages. Second, the number of cardiac catheterization laboratory activations leading to coronary angiography and PPCI has also declined during the Pandemic by 31% and 18%, respectively. Third, the decline in STEMI metrics was seen in all geographic areas included in our analysis, irrespective of COVID‐19 incidence, implementation of lockdown orders, and levels of testing. Finally, among patients who received PPCI, delays in reperfusion were noted in March 2020 with improvements in April 2020.
COVID‐19 has significantly impacted healthcare delivery in the US and around the world. As hospital systems prepared to receive COVID‐19 patients, several measures were implemented that restricted access to outpatient care, emergency room evaluations, and diagnostic and therapeutic cardiac procedures deemed elective. Unintended consequences of these directives have been documented. 4 , 5 , 6 , 9 , 10 We have previously reported a 38% decline in cardiac catheterization laboratory activations for STEMI during the early phase of the COVID‐19 Pandemic and highlighted the importance of continuous monitoring of this trend and need to investigate its causes as the pandemic effects are likely to be felt for most of 2020. To that end, we expanded our initial analysis from 9–18 STEMI programs (or healthcare systems) representative of the US, added more granular information regarding important metrics of STEMI care including utilization of coronary angiography, PPCI and D2B times, performed a detailed geographic analysis in areas with different levels of COVID testing and disease burden, and conducted a hospital‐or healthcare system‐level analysis of trends during the Pandemic. Taken together, these observations suggest a negative, widespread, and persistent impact on STEMI care during the COVID 19 pandemic in the US.
The reduction in utilization of coronary angiography, PPCI, and delays in mechanical reperfusion suggest that even for patients who present to the healthcare system, processes of care might have changed during the Pandemic. Although some have advocated for increased use of pharmacological (thrombolytic) reperfusion or pharmacoinvasive strategies, 11 the American College of Cardiology (ACC) and Society for Cardiovascular Angiography and Interventions (SCAI) continue to recommend PPCI for STEMI patients. 12 In fact, of the programs surveyed for this analysis, only three reported using fibrinolytic therapy with very few patients treated (<5 per year). None of them reported using them preferentially during the COVID‐19 Pandemic. The reasons for these reductions and treatment delays remain speculative and may include (a) overwhelmed emergency medical systems (EMS), (b) changes in STEMI pathways to facilitate testing in the emergency department with cancellations of direct transfers to the cardiac catheterization laboratory, (c) increased used of imaging, including cardiac CT and echocardiography, to triage STEMI patients suspected of having COVID, 13 (d) late presentations, outside the therapeutic window for mechanical reperfusion, and (e) insufficient access to personnel protective equipment.
The finding of similar reductions in STEMI activations in various geographic areas within the US with different COVID‐19 disease burden suggests that overwhelmed EMS systems alone are unlikely to explain these declines. Avoidance of the medical system due to fear of contracting COVID‐19, restricted access to primary care physicians and emergency departments, and STEMI misdiagnosis are likely to play a role. 14 Of note, some healthcare systems seem to be rebounding from their March 2020 declines faster than others and may provide some clues as to what is needed to revert these trends. For example, Christ Hospital in Cincinnati, OH, conducted an extensive media and public relations campaign in late March to alert patients about the importance of timely medical care. In April 2020, their number of STEMI activations was back to 2019 levels. More information is needed to understand the drivers of and potential solutions to these negative trends in STEMI care.
4.1. Limitations
Our study has important strengths, including 16 months of continuous STEMI metrics in 18 large hospitals or healthcare systems representative of diverse areas of the US, but also important limitations. First, given the observational study design, our results are hypothesis‐generating regarding the potential mechanisms leading to a reduction in STEMI metrics. Second, we were unable to provide individual‐patient data, including demographic, angiographic, and treatment data. Third, we included STEMI hospitals and healthcare systems that may have different configurations (spoke and hub), transfer, and time to treatment protocols. We provided aggregate data for some STEMI metrics but lack granular information on transfer times and other aspects of STEMI care.
5. CONCLUSIONS
The COVID‐19 Pandemic has had a negative, widespread, and persistent impact on STEMI care in the US. Efforts to educate the public on the importance of timely care and to maintain unrestricted access to emergency medical care are needed to overcome these trends.
CONFLICT OF INTEREST
All authors have no conflict of interest related to this project.
Supporting information
FIGURE S1 Location and number of ST‐elevation myocardial infarction programs in each state. The number inside each start denotes the number of hospitals included in each state.
FIGURE S2 Number of ST‐elevation myocardial infarction cardiac catherization laboratory activations in each program (gray lines) on log10 scale.
TABLE S1 Hospitals and healthcare systems included in the analysis
Table S2. Measures of disease incidence and testing affecting STEMI programs included in the study as of April 7, 2020.
ACKNOWLEDGMENT
The regional STEMI program at Abbott Northwestern Hospital is supported by the Minneapolis Heart Institute Foundation and Allina Health.
Garcia S, Stanberry L, Schmidt C, et al. Impact of COVID‐19 pandemic on STEMI care: An expanded analysis from the United States. Catheter Cardiovasc Interv. 2021;98:217–222. 10.1002/ccd.29154
EDITORIAL COMMENT: Expert Article Analysis for: Practice patterns for patients with ST‐elevation myocardial infarction during the early phase of the COVID‐19 pandemic—Valuable lessons learned
REFERENCES
- 1. http://www.euro.who.int/__data/assets/pdf_file/0007/436354/strengthening‐health‐systems‐response‐COVID‐19‐technical‐guidance‐1.pdf. Accessed May 21, 2020.
- 2. Szerlip M, Anwaruddin S, Aronow HD, et al. Considerations for cardiac catheterization laboratory procedures during the COVID‐19 pandemic. Catheter Cardiovasc Interv. 2020;96(3):586‐597. 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 3. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/guidance‐hcf.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019‐ncov%2Fhealthcare‐facilities%2Fguidance‐hcf.html. Accessed May 21, 2020.
- 4. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid‐19 on stroke evaluation in the United States. New Engl J Med. 2020;383:400‐401. 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in Northern Italy. New Engl J Med. 2020;383:88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marijon E, Karam N, Jost D, et al. Out‐of‐hospital cardiac arrest during the COVID‐19 pandemic in Paris, France: a population‐based, observational study. Lancet Public Health. 2020;5(8):E437‐E443. 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. https://www.propublica.org/article/theres‐been‐a‐spike‐in‐people‐dying‐at‐home‐in‐several‐cities‐that‐suggests‐coronavirus‐deaths‐are‐higher‐than‐reported. Accessed May 21, 2020.
- 8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol. 2020;75:2871‐2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J. 2020;41:2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pramesh C, Badwe RA. Cancer management in India during Covid‐19. New Engl J Med. 2020;382(20):e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daniels MJ, Cohen MG, Bavry AA, Kumbhani DJ. Reperfusion of STEMI in the COVID‐19 era‐business as usual? Circulation. 2020;141:1948–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mahmud E, Dauerman HL, Welt FG, et al. Management of acute myocardial infarction during the COVID‐19 pandemic. J Am Coll Cardiol. 2020;76(11):1375‐1384. 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bangalore S, Sharma A, Slotwiner A, et al. ST‐segment elevation in patients with Covid‐19—a case series. New Engl J Med. 2020;382:2478‐2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stefanini GG, Montorfano M, Trabattoni D, et al. ST‐elevation myocardial infarction in patients with COVID‐19: clinical and angiographic outcomes. Circulation. 2020;141:2113‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1 Location and number of ST‐elevation myocardial infarction programs in each state. The number inside each start denotes the number of hospitals included in each state.
FIGURE S2 Number of ST‐elevation myocardial infarction cardiac catherization laboratory activations in each program (gray lines) on log10 scale.
TABLE S1 Hospitals and healthcare systems included in the analysis
Table S2. Measures of disease incidence and testing affecting STEMI programs included in the study as of April 7, 2020.


