Abstract
Background
Health care workers (HCWs) are at risk of getting infected while at work, for example, operating room (OR), hence it is pertinent that they don all the appropriate personal protective equipment (PPE) to minimize the chance of getting infected.
Methods
A COVID‐19 specific briefing and debriefing form was created and used in the OR along with the World Health Organization surgical safety checklist to reinforce the use of appropriate PPE. An audit was subsequently done to understand the compliance to PPE use, followed by a survey based on the findings of the audit to understand the issues related to noncompliance.
Results
The form was used in 183 out of the 238 (77%) surgeries performed during a months' time. The overall compliance for PPE usage was 96.3%. Noncompliance was seen most often for eye protection (45/567) (P = .01). The survey revealed that this was mostly among surgeons mainly due to discomfort, poor visibility, and frequent fogging.
Conclusions
Our HCW were adapting well to the new normal of donning appropriate PPE in the OR, except for the eye protection due to discomfort and visibility related issues. This is important to know so that necessary changes could be introduced to better the compliance.
Keywords: cancer surgery, checklist, COVID‐19 negative, elective, pandemic, PPE
1. INTRODUCTION
The year 2020 began with news about a novel coronavirus originating from the city of Wuhan in China and spreading progressively to different continents across the globe. 1 The World Health Organization (WHO) declared this rapidly evolving event as a pandemic in March 2020, and the causative organism was termed severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). 2 Health care centers around the world had various challenges to face at the same time. At one end, there was a multiplication of symptomatic patients and health care workers (HCW) infected by this virus. 3 , 4 On the other hand, there was a concern about patients with non‐COVID‐19 ailments, such as cancer, risking a delay in treatment. The judicious use of hospitals and human resources became critical. The selection of surgeries that should be performed during this pandemic was based on recommendations from various international guidelines. 5 Cancer surgery being categorized as semiemergency had to continue.
With no effective treatment or vaccines available for the COVID‐19 till date, the best way to minimize the risk of getting infected is by taking adequate protection. WHO had issued guidelines for personal protective equipment (PPE) use in February 2020 which includes gloves, medical masks, goggles or a face shield, and gown, as well as N95/FFP2 or equivalent respirators, for those performing aerosol‐generating procedures. 6 The level of exposure varies among HCW depending on their specific role in inpatient care. The HCW in the operating room (OR) is at higher risk because of the close contact with the patients while intubation or during surgery with the inherent danger of contact with the patient's body fluids and during aerosol‐generating procedures. 7 During the SARS epidemic studies showed that HCW who wore adequate personal protection had a lesser chance of getting infected. 8 , 9
Despite the proven benefits, compliance with the usage of PPE is fraught with issues like availability, discomfort, and individual perception. The model of the WHO surgical safety checklist (SSC) in ensuring patient safety is well established and has been in use at our center. 10 Similar to the concept of SSC, the surgical briefing and debriefings are essentially communication and teamwork tools, that help to identify issues at the start and the end of an operating session and involves all members of the team. 11 It helps to identify errors (such as not donning appropriate PPE in our case), excessive OR traffic and also aims at improving communication among the staff members. 12 We adopted this established concept of team briefing and debriefing to reinforce among our HCWs the use of appropriate PPE at the beginning of the case itself and confirm the same at the end of the case so that we could identify multiple recurring errors to avoid them. We created a COVID‐19 specific briefing and debriefing form and used it in addition to the SSC at the beginning and the end of the case (Supporting Information Appendix‐I). The forms were used for a month and subsequently audited. Based on the findings of the audit, a survey was done to understand the perception among HCW about various components of PPE and reasons for noncompliance if any. We also looked at common reasons for poor compliance to take suitable actions.
2. METHODOLOGY
The COVID‐19 specific briefing and debriefing forms were created and finalized after consensus among participating colleagues from the Department of Surgery and Anaesthesiology of our institute. The authors confirm that all the procedures contributing to this study complied with ethical standards. The COVID‐19 briefing and debriefing form has three parts (Supporting Information Appendix‐I). Part‐I captured the patient details including the COVID‐19 status. Part‐II is the briefing section which has two steps within. Step‐1 captures the details regarding the different PPE's (surgical cap, N95 mask, three‐ply mask, double gloves, plastic apron, face shield or goggles, and disposable gowns) being used by the HCW in the OR as the patient is wheeled into the OR and affirming the same at the time of incision. Step‐2 specifically identifies if an aerosol‐generating procedure was anticipated during surgery (surgeries involving the use of saw for cutting bone, eg, marginal mandibulectomy). Part‐III is the debriefing section to be done at the end of the surgery before the patient is wheeled out of the OR to confirm the use of the PPE till the end of the surgery. It also captures the precautions taken while the powered instrument was in use and details of any new team member that might have joined the surgery along with any concerns the team might have at the end. This COVID‐19 specific briefing and debriefing form was used in tandem with the WHO SSC for a period of 1 month (4th May 2020 to 3rd June 2020). A standard operating procedure regarding the sequence of using the forms was also circulated with the aforementioned (Supporting Information Appendix‐II). Usage of Surgical cap, N95 and a three‐ply mask (to increase the duration of use of the N95 mask), double gloves and gowns were deemed mandatory for use by all members present in the OR. Compliance related to eye protection was considered breached for surgeons if they were not wearing either of these for any part of the surgery (Figure 1). For anesthesiologists nonusage of eye protection after intubation and not using the plastic disposable apron was not considered as noncompliance. For both anesthesiologists and operation theater (OT) technicians usage of plastic apron was not considered mandatory. Based on the results of the analysis of the data obtained from the COVID‐19 team briefing and debriefing form, an electronic questionnaire‐based survey (http://www.surveymonkey.com/r/NS9GJS5) using SurveyMonkey platform (SurveyMonkey Inc, San Mateo, CA) was conducted among the OR personnel, ie, surgeons, residents, and consultants), anesthesiologist (residents and consultants) and scrub nurses. The survey included 10 questions (Supporting Information Appendix III), all questions were mandatory, regarding the usage of PPE in the OR during the surgical procedure and reasons for noncompliance. The questionnaire‐based survey was sent by email and mobile‐based application (WhatsApp) to the HCW. Two reminders were sent one on day 7 and another on day 13 before closing the survey on day 14. Statistical analysis was done with SPSS version 22, descriptive analysis and qualitative analysis was done. Also, the χ 2 test was done to understand the significance of the noncompliance among the members of the various specialties.
Figure 1.

The sequence of different PPE's donned for surgery. PPE, personal protective equipment [Color figure can be viewed at wileyonlinelibrary.com]
3. RESULTS
3.1. Audit
A total of 238 routine (elective) surgeries were performed between 4th May 2020, and 3rd June 2020. The COVID‐19 briefing and debriefing forms were used in 183 surgeries (77%). All of these patients were COVID‐19 negative. The utilization of OR among the various oncosurgical specialties is shown in Table 1. In general, for one surgery three surgeons, two anesthetists, one scrub nurse, and one technician would be involved at a given time. Typically, at our institute (and many others) scrub nurses and technicians would have an 8‐hour shift. Occasionally due to human resource logistics, a technician would be shared between adjoining OTs. In these 183 surgeries, 567 surgeons (including consultants and residents), 413 anesthesiologists (including consultants and residents), 291 scrub nurses, and 164 OT technicians were involved. The overall compliance for PPE usage was 96.3%. Noncompliance was seen most often for face shields and this was largely among surgeons (45/567) (P < .001). Surgical cap, N95/3‐ply mask, and double gloves were worn by all as part of PPE (Table 2). Nearly 10% of the OT technicians were not wearing the gowns. This could be attributed to the fact that the OT technicians do not routinely use gowns and probably are yet to get accustomed to using gowns in the COVID‐19 era on a regular basis. The scrub nurses were the most compliant to donning all the prescribed PPE (99.5%).
Table 1.
Details of surgeries performed in different surgical oncology subspecialties
| Numbers (183) | Percentage | |
|---|---|---|
| Head and neck oncology/plastic and reconstruction | 45 | 24.5 |
| Bone and soft tissue oncology | 19 | 10.4 |
| Gastrointestinal oncology | 40 | 21.8 |
| Thoracic oncology | 15 | 8.2 |
| Uro oncology | 10 | 5.6 |
| Breast oncology | 24 | 13.2 |
| Gynae oncology | 15 | 8.2 |
| Neuro oncology | 3 | 1.6 |
| Pediatric oncology | 12 | 6.5 |
Table 2.
Details of the use of different PPE by OT personnel
| Surgical cap, % | N95/3‐ply mask, % | Face shields, % | Plastic apron, % | Double gloves, % | Gowns, % | Overall compliance, % | |
|---|---|---|---|---|---|---|---|
| Surgeons, n = 567 | 567 (100) | 567 (100) | 522 (92) | 563 (99.2) | 567 (100) | 567 (100) | 98.5 |
| Anesthetists, n = 413 | 413 (100) | 412 (99.7) | 406 (98.3) | 235 (57)a | 411 (99.5) | 413 (100) | 92.5 |
| Scrub nurses, n = 291 | 291 (100) | 291 (100) | 285 (98) | 289 (99.3) | 291 (100) | 291 (100) | 99.5 |
| OT technicians, n = 164 | 164 (100) | 164 (100) | 157 (95.7) | 136 (83)a | 164 (100) | 148 (90.2) | 94.8 |
Abbreviations: OT, operation theater; PPE, personal protective equipment.
Anesthetist and OT technicians not wearing the Plastic Apron (in the colored box) was not considered a breach in protocol.
3.2. Survey
As noted in the audit, surgeons were not using the face shields provided most often. The circulated survey questionnaire was an effort to understand the reasons for this and in general the perception of PPE usage by all stakeholders. The survey questions were sent out to 351 individuals (surgeons—44 consultants, 125 residents; anesthetists—28 consultants, 110 residents, and 44 nursing staff). A total of 122 responses (35%) were obtained of which 77 (63%) were from surgeons, 31 (25%) from anesthesiologists, and 14 (12%) from the nursing staff. The surgeons were from different subspecialties within the department of surgical oncology. This included head and neck surgery, gastrointestinal surgery, gynecology, urology, bone and soft tissue, plastic surgery, breast surgery, pediatric surgery, neurosurgery, and thoracic surgery. The majority of the survey participants (94%) were aware of the PPE checklist being used in the OR and 70% of them thought that the implementation of the checklist had improved the compliance to PPE in the OR.
Among the PPE, that is, N95, 3‐ply mask, double gloves, eye protection (face shield, and/or goggles; Figure 1), only 43 of the 122 (35%) wore all of the above at the times that it was considered mandatory in the OR among the respondents. Thirty‐six out of the 122 (29.5%) people surveyed wore neither goggles nor face shields. Only 40% of the respondents felt either goggles or face shields or both needed to be worn in the OT in the current situation. Among the surgeons, uro‐oncologists (100%) followed by head and neck surgeons (81%) perceived that face shields and goggles are not required once the patient has been tested negative for SARS‐CoV‐2.
Since face shields had been repeatedly found to be least worn in the OR, the questionnaire specifically included further questions directed towards finding the usage pattern, preference, and reasons for nonusage. One of the questions in the survey had pictorial options of the different varieties of face shields available for usage. Among the four commonly used face shield types (Figure 2), that is, hard visor shield, the M foam shield, OHP face shield, and shield mask, the M foam shield was the most commonly used (70% usage).
Figure 2.
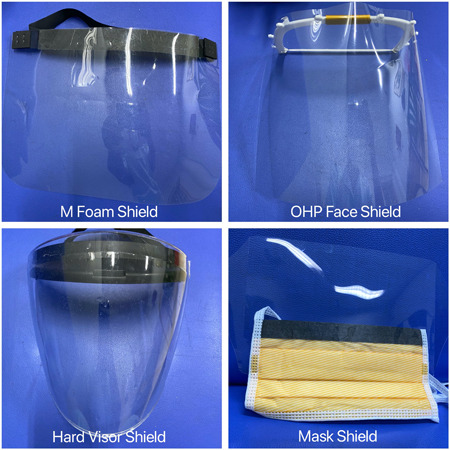
Different types of face shields used [Color figure can be viewed at wileyonlinelibrary.com]
The reasons for poor compliance with the usage of face shield included discomfort (33%), poor visibility due to thickness (36%), and repeated fogging (33%). A total of 42 of the 122 (34%) did not have any issues with using face shields (Figure 3). Based on the survey, the hard visor shield was the most preferred and the shielding mask was the least preferred one among the four face shields currently available.
Figure 3.
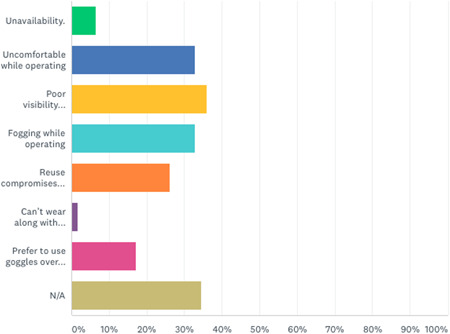
Different issues attributed for not using the face mask [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
The audit showed that the overall compliance with the use of PPE in the OR by HCWs was high at 96.3%. Face shield was one of the components among the PPE that was not always donned while in the OR, especially by the surgeons, citing poor visibility, fogging, and discomfort as the common reasons.
Our hospital is a tertiary care center, located in Mumbai, catering to the largest volume of cancer patients in India. Very early on during the pandemic, our hospital administration decided to continue cancer treatment taking all necessary precautions for the patients and HCW. 13 An integral component of being able to continue delivering health care in these circumstances is the appropriate usage of PPE. The protection offered by PPEs against transmission of SARS‐CoV‐2 has been proven beyond doubt, and there are some recommendations about the level of protection required based on the type of surgery. 14 Despite PPE equipment being in relatively short supply, our hospital administration provided all HCW with the required PPE to be used while at work. As Mumbai was the worst affected city since the COVID‐19 pandemic started in India, we were mindful from the very beginning about the need to reinforce the usage of appropriate PPE among the HCW while in the OR. This would also be the new normal which the HCW will have to get adapted to and follow for quite some time in the future. With adequate preparedness, we were able to perform close to five hundred major cancer surgeries between 23rd March 2020, and 30th April 2020 with no worsening of perioperative outcomes. 15
During the initial days of the pandemic, we did not adopt routine COVID‐19 testing before elective surgery. COVID‐19 testing was done in patients with symptoms suggestive of COVID‐19, history of travel from a hotspot, and history of high‐risk contact with a COVID‐19 positive patient. Given the subsequent increase in COVID‐19 positive cases (both in the country and especially in our city, Mumbai) and an increase in the number of asymptomatic COVID‐19 positive patients in the community, the policy was modified and we started doing preoperative COVID‐19 testing before routine cancer surgery.
Similar to some of the findings in the present study, Benitez et al reported that more than half of the respondents in their study reported that the use of PPE affected surgical performance. They also reported visibility impairment due to goggle fogging by two‐thirds of the respondents. 16 Face shields and goggles generate glare and when not used properly generate fogging leading to poor visibility. This is an important finding because if the surgeons do not wear these face shields or goggles it could be potentially harmful as there is evidence to show transmission via conjunctival contact of the body fluids. 17 Chu et al 18 in their systematic review concluded that eye protection also was associated with less infection. Benitez et al 16 also reported that apart from poor visibility there was reduced comfort and difficulty in communication with the other members in the OR. Though we could not capture these details we would concur with these findings of the problem faced by many of us in the OR. These factors would be contributing to surgical fatigue and exhaustion. Our next effort would be directed towards identifying issues that cause discomfort while donning these PPE and attempt to reduce their influence on surgeon fatigue. We believe that the checklist was probably instrumental in ensuring the compliance of PPE usage among the HCW in the OR.
Improvement in compliance for all components of PPE would depend on two factors. One, the perceived necessity for wearing a particular protective equipment and second the comfort of HCW while using these PPE. These two factors are likely to be interrelated as also reflected in our results. Hospitals should be receptive to the fact that discomfort is known and options of different types of PPE, especially like face protection equipment, should be made available. We have made an initial effort towards this by connecting with a reputed national manufacturer of motorcycle helmet visors with the feedback from our surgeons. Our current batch of hard visors supplied by this manufacturer has improved visibility, have less fogging and better comfort. There is also a need for a global collaborative effort to know which components of the PPE are required in which categories/subspecialty of surgery with suggestions to increase user comfort and reduce user fatigue.
The strengths of our study are that the COVID‐19 briefing and debriefing form can be used universally which is relevant to the present pandemic. This study helped us realize the compliance of the use of the PPE among the large majority of the HCW and also understand the possible reasons for noncompliance for corrective measures to be taken. In a way, we feel this would help our HCW get more accustomed to the new normal. The limitations of the study include that the COVID‐19 briefing and debriefing forms could not be used in all the operated cases during the mentioned period and also we did not include the OT technicians (as not all may be accustomed to answering the survey on the digital platform such as Survey Monkey) in the survey.
5. CONCLUSIONS
Most of our HCW (96.3%) were geared to adapt to the new normal of donning all the prescribed PPE. However, some surgeons had issues with visibility with the use of face shields/goggles due to discomfort and fogging which we have attempted to resolve. Furthermore, the policymakers should be cognizant of the fact that while ensuring compliance of PPE usage, perception and comfort of the HCW (which may play a crucial role) should be considered.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ETHICS STATEMENT
The authors confirm that all ethical standards were adhered to whilewhile doing this study. All the patients received the standard of care for their condition. No identifying information about participants is available in the article. However, all patients have given consent for the treatment they have received.
SYNOPSIS
The overall compliance to the use of PPE by our HCW's during routine cancer surgery in COVID‐19 negative patients was 96.3%. The noncompliance was mostly noticed among surgeons for eye protection for reasons such as discomfort, poor visibility and fogging.
Supporting information
Supporting information
Supporting information
Supporting information
ACKNOWLEDGMENTS
Two of the lead authors trained in the workshops (Life Box SAFE OR practice Workshop) conducted in 2019 and are presently Mentors in the Workshop.
Prakash G, Shetty P, Thiagarajan S, et al. Compliance and perception about personal protective equipment among health care workers involved in the surgery of COVID‐19 negative cancer patients during the pandemic. J Surg Oncol. 2020;122:1013–1019. 10.1002/jso.26151
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Keni R, Alexander A, Nayak PG, Mudgal J, Nandakumar K. COVID‐19: emergence, spread, possible treatments, and global burden. Front Public Health. 2020;8:216. 10.3389/fpubh.2020.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghebreyesus TA. WHO Director‐General's opening remarks at the media briefing on COVID‐19. 2020, March 11. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3. Lai X, Wang M, Qin C, et al. Coronavirus disease 2019 (COVID‐2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw Open. 2020;3(5):e209666. 10.1001/jamanetworkopen.2020.9666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cheng VC, Wong S, Yuen K. Estimating coronavirus disease 2019 infection risk in health care workers. JAMA Netw Open. 2020;3(5):e209687. 10.1001/jamanetworkopen.2020.9687 [DOI] [PubMed] [Google Scholar]
- 5. Moletta L, Pierobon ES, Capovilla G, et al. International guidelines and recommendations for surgery during COVID‐19 pandemic: A systematic review. Int J Surg. 2020;79:180‐188. 10.1016/j.ijsu.2020.05.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID‐19). Interim guidance. 2020, February 27. https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCovIPCPPE_use-2020.1-eng.pdf
- 7. Forrester JD, Nassar AK, Maggio PM, et al. Precautions for operating room team members during the COVID‐19 pandemic. J Am Coll Surg. 2020;230(6):1098‐1101. 10.1016/j.jamcollsurg.2020.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lau JT, Fung KS, Wong TW, et al. SARS transmission among hospital workers in Hong Kong. Emerg Infect Dis. 2004;10:280‐286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seto WH, Tsang D, Yung RW, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003;361:1519‐1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ambulkar R, Ranganathan P, Salunke K, Savarkar S. The World Health Organization surgical safety checklist: an audit of quality of implementation at a tertiary care high volume cancer institution. J Anaesthesiol Clin Pharmacol. 2018;34:392‐398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Civil I, Shuker C. Briefings and debriefings in one surgeon's practice. ANZ J Surg85. 2015;85:321‐323. [DOI] [PubMed] [Google Scholar]
- 12. Brennan PA, Mitchell DA, Holmes S, Plint S, Parry D. Good people who try their best can have problems: recognition of human factors and how to minimise error. Br J Oral Maxillofac Surg. 2016;54(1):3‐7. 10.1016/j.bjoms.2015.09.023 [DOI] [PubMed] [Google Scholar]
- 13. Pramesh CS, Badwe RA. Cancer management in India during COVID‐19. N Engl J Med. 2020;382:61. 10.1056/nejmc2011595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Rational use of personal protective equipment for coronavirus disease (COVID‐19) and considerations during severe shortages. Interim guidance. WHO/2019‐nCov/IPC_PPE_use/2020.3. 2020, April 6.
- 15. Shrikhande SV, Pai PS, Bhandare MS, et al. Outcomes of elective major cancer surgery during COVID 19 at Tata Memorial Centre: implications for cancer care policy. Ann Surg. 2020. 10.1097/SLA.0000000000004116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yánez Benítez C, Güemes A, International Cooperation Group on PPE and Emergency Surgery ., et al. Impact of personal protective equipment on surgical performance during the COVID‐19 pandemic. World J Surg. 2020;44:1‐6. 10.1007/s00268-020-05648-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bischoff WE, Reid T, Russell GB, Peters TR. Transocular entry of seasonal influenza–attenuated virus aerosols and the efficacy of N95 respirators, surgical masks, and eye protection in humans. J Infect Dis. 2011;204:193‐199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: a systematic review and meta‐analysis. Lancet. 2020;395(10242):1973‐1987. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Supporting information
Supporting information
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


