Abstract
Objectives
To determine the well‐being of urologists worldwide during the coronavirus disease 2019 pandemic, and whether they have adequate personal protective equipment knowledge and supplies appropriate to their clinical setting.
Methods
Urologists worldwide completed a Société Internationale d’Urologie online survey from 16 April 2020 until 1 May 2020. Analysis was carried out to evaluate their knowledge about protecting themselves and others in the workplace, including their confidence in their ability to remain safe at work, and any regional differences.
Results
There were 3488 respondents from 109 countries. Urologists who stated they were moderately comfortable that their work environment offers good protection against coronavirus disease 2019 showed a total mean satisfaction level of 5.99 (on a “0 = not at all” to “10 = very” scale). A large majority (86.33%) were confident about protecting themselves from coronavirus disease 2019 at work. However, only about one‐third reported their institution provided the required personal protective equipment (35.78%), and nearly half indicated their hospital has or had limited personal protective equipment availability (48.08%). Worldwide, a large majority of respondents answered affirmatively for testing the healthcare team (83.09%). Approximately half of the respondents (52.85%) across all regions indicated that all surgical team members face an equal risk of contracting coronavirus disease 2019 (52.85%). Nearly one‐third of respondents reported that they had experienced social avoidance (28.97%).
Conclusions
Our results show that urologists lack up‐to‐date knowledge of preferred protocols for personal protective equipment selection and use, social distancing, and coronavirus disease 2019 testing. These data can provide insights into functional domains from which other specialties could also benefit.
Keywords: COVID‐19, pandemic, personal protective equipment, protective measures, urology
Abbreviations & Acronyms
- COVID‐19
coronavirus disease 2019
- PPE
personal protective equipment
- SIU
Société Internationale d’Urologie
Introduction
Much of what we know about how clinicians are coping with and reacting to the novel COVID‐19 pandemic comes from research gleaned from the front‐line specialties of critical care medicine, anesthesiology, emergency medicine and nursing. 1 , 2 , 3 , 4
However, as the pandemic wears on, it has become clear that all clinical specialties have experienced dramatic effects in terms of how they practice, how they protect themselves in the workplace and how secure they feel in that protection, particularly when it comes to worries about infecting themselves and others.
As a surgical specialty, urologists typically divide their time between patient consultations and carrying out surgery. Due to increased staffing needs during the pandemic, physicians in second‐line specialties, including urology, have been redeployed to the emergency department or COVID‐19 tents to assist with triage of presumed COVID‐19 patients, and to the intensive care unit to manage critically ill patients.
Additionally, much of the emerging literature on the effects of COVID‐19 on the healthcare workforce has focused on a single specialty in a single country or region of the world. 5 , 6 , 7 In contrast, the SIU has taken full advantage of its global membership to create a worldwide dataset. The present study is an analysis of a survey carried out by the SIU of its membership to determine the well‐being of urologists worldwide during the COVID‐19 pandemic, and whether they have adequate PPE knowledge and supplies appropriate to their clinical setting. These data have significance beyond the specialty itself, and can provide insights into functional domains from which many non‐urology clinicians could also benefit.
Methods
The survey, the second in a series, was developed by members of the SIU Executive Board. It included multiple choice questions about respondent demographics and general practice changes in response to COVID‐19, as well as questions about educational needs and concerns about contracting COVID‐19. This analysis specifically addresses responses to questions about clinicians’ approach to and prioritization of PPE use and supplies, and staff and patient testing for COVID‐19. The full survey is available in Appendix S1.
The survey was opened on 16 April 2020, and closed on 1 May 2020. It was administered online using the Aventri platform (Norwalk, CT, USA). Distribution of the survey took place via email, using names on the SIU eNews mailing distribution list. The survey included reasons why it was being carried out and the importance of participation. No compensation was offered for its completion. All responses were anonymous.
To facilitate analysis of the impact of COVID‐19 on healthcare settings as it spread from East to West, respondents were grouped into regions. The list of countries included in each region is provided in Appendix S2.
Statistical analysis
The data were analyzed in two different ways. Categorical data were explored through a series of omnibus χ2‐tests (using a standard α threshold of P = 0.05). The χ2‐tests were followed up by calculating an adjusted standardized residual for each cell in each contingency table.
Conceptually, these are the Z‐transformed differences between the expected and observed value for that cell. The larger the adjusted standardized residual, the larger this expected versus observed difference, with adjusted standardized residuals that exceed a critical threshold identifying cells with an observed value that is higher or lower than expected, given the null hypothesis. The critical threshold was Bonferroni corrected for multiple comparisons within each contingency table.
Continuous data were explored through one‐way ANOVA and follow‐up pairwise comparisons. The pairwise comparisons within each one‐way anova were Bonferroni corrected for multiple comparisons.
Results
A total of 3529 urologists from 109 countries responded to the survey. Of these, 41 started the survey but did not complete it, leaving a final sample size of 3488 completed surveys. Table 1 presents the age distribution, region of origin and practice setting of the urologists.
Table 1.
Background demographics
| Variable | n (%) |
|---|---|
| Total | 3488 (100) |
| Age (years) | |
| <40 | 1214 (38.40) |
| 40–50 | 1046 (30.00) |
| 51‐60 | 736 (20.10) |
| >60 | 492 (14.10) |
| Region of origin | |
| Europe | 1130 (32.40) |
| East/South‐East Asia | 868 (24.90) |
| West/South‐West Asia | 589 (16.90) |
| Africa | 195 (5.60) |
| South America | 310 (8.90) |
| North America | 396 (11.40) |
| Practice setting | |
| Academic/university hospital | 1869 (53.60) |
| Private practice (office/hospital) | 848 (24.30) |
| Public non‐academic/Military/Veterans’ hospital | 771 (22.10) |
In general, urologists gave a moderate score to their work environment offering good protection against COVID‐19 (Fig. 1). On a regional basis, respondents in North America and East/South‐East Asia awarded the highest scores to their workplace protections, whereas those in Africa gave the lowest scores to their workplaces (Fig. 2). In terms of practice setting, a separate analysis of the responses from questions 12 and 15 of the survey did not show any differences in outcomes between academic and non‐academic institutions.
Fig. 1.
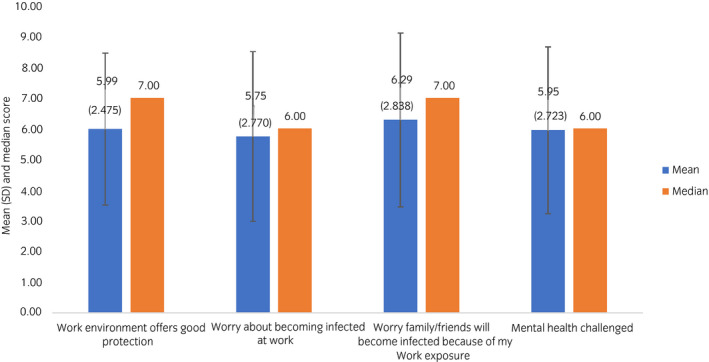
Mean (SD) and median ratings of level of concern about COVID‐19 infection. Rating scale: 0–10, where 0 is “not at all” and 10 is “very”.
Fig. 2.
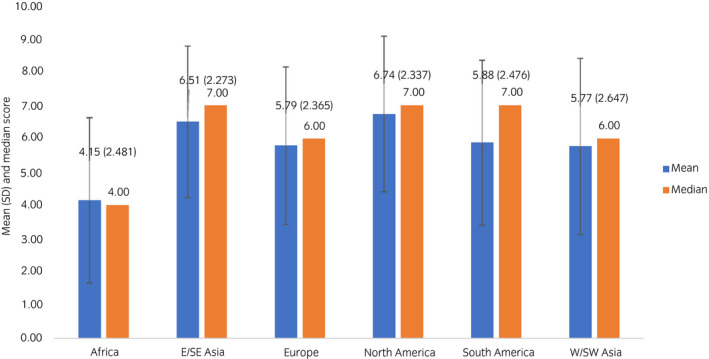
Mean (SD) and median ratings of degree to which work environment offers good protection, by region. Rating scale: 0–10, where 0 is “not at all” and 10 is “very”.
When asked whether they know how to protect themselves from becoming infected with COVID‐19 at work, a large majority of respondents answered affirmatively (86.33%), with North American respondents more likely than expected to report they have sufficient knowledge (91.09%; adjusted standardized residual 2.92; Fig. 3).
Fig. 3.
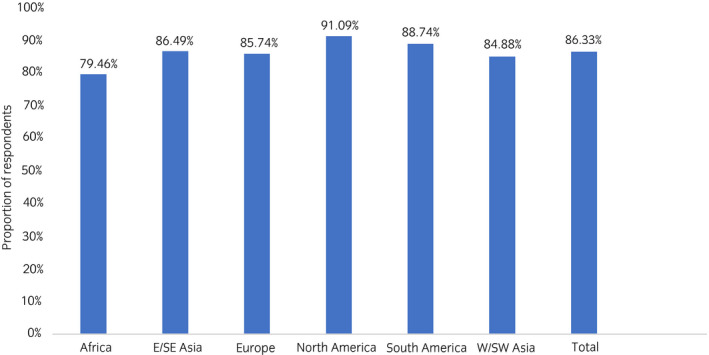
Proportion of respondents reporting they know how to protect themselves from becoming infected at work, by region.
Access to and use of PPE
Respondents were asked to indicate whether their institution provides adequate quantities of the appropriate PPE or limited quantities of the appropriate PPE (Fig. 4). Slightly more than one‐third of urologists reported that their institution provides all required PPE for any type of medical or surgical setting (35.78%). North American respondents were more likely than expected to report access to all needed PPE (45.95%; adjusted standardized residual 4.04), whereas just 11.28% of African urologists reported good access (adjusted standardized residual −7.34). Nearly half of respondents indicated that their hospital has or had limited availability of the full range of PPE (48.08%). Here, respondents from Africa were more likely than expected to report limited access to PPE (64.62%; adjusted standardized residual 4.76).
Fig. 4.
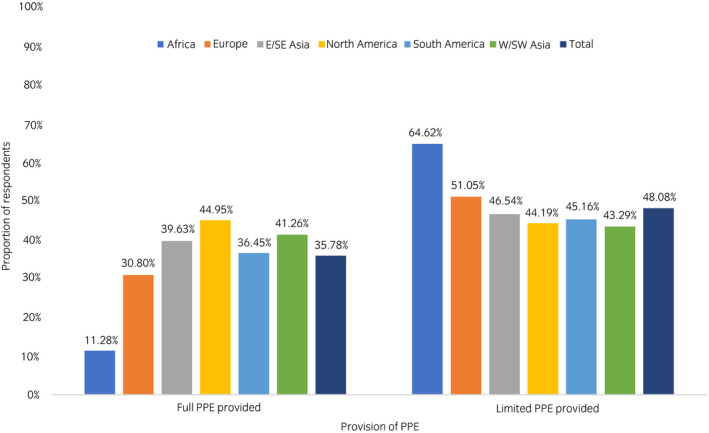
Proportion of respondents reporting full or limited access to PPE in all work settings, by region.
The survey also inquired about the PPE urologists typically choose for surgery (Fig. 5). More than two‐thirds of respondents across all regions indicated that they would wear a surgical mask (68.41%). Slightly more than one‐third of respondents (38.45%) indicated that an N95/FFP3 mask is the required surgical PPE. Eye protection, such as glasses or goggles, was the next most popular response, chosen by 52.47% of respondents. Similarly, one‐third of urologists (33.40%) from all regions indicated that they would choose a face shield to wear as PPE when operating on an untested patient. There were regional differences observed for the PPE used.
Fig. 5.
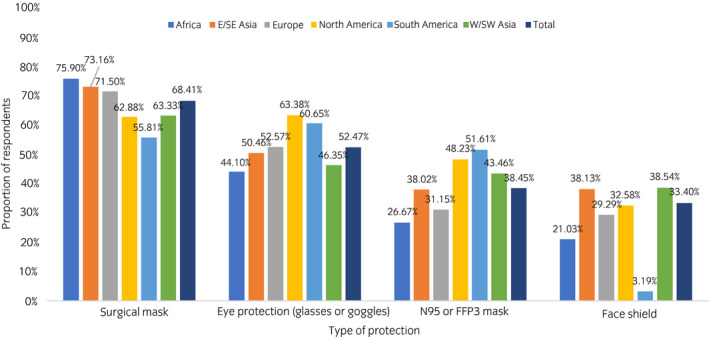
PPE used for surgery on patients with no symptoms and not tested for COVID‐19, by region.
Another question addressed typical outpatient consultation PPE (Fig. 6). Approximately two‐thirds of respondents (65.88%) across all regions indicated that a surgical mask is sufficient PPE outside of the operating room. Slightly more than one‐quarter of respondents (27.92%) indicated that N95/FFP3 masks should be worn during patient consultations. Similarly, slightly less than one‐quarter of respondents (24.03%) chose face shields as appropriate clinical examination PPE. Responses by region were as expected, with the exception of respondents from East/South‐East Asia, who were more likely to select face shields (29.26%; adjusted standardized residual 4.17). Only a small percentage (5.96%) of all respondents indicated that no mask is required during patient consultations.
Fig. 6.
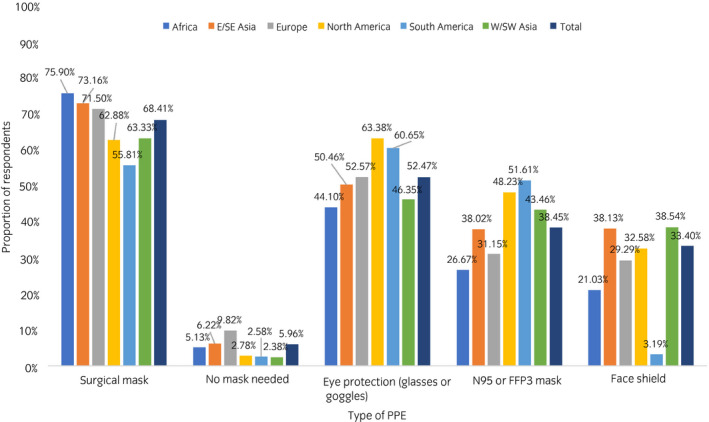
PPE used for outpatient consultations with patients with no symptoms and not tested for COVID‐19, by region.
Testing for COVID‐19 and perception of risk
Just 19 respondents (0.54%) responded that they tested positive for COVID‐19, with no regional variation among responses. The replies to testing for COVID‐19 are presented in Figure 7. Nearly two‐thirds of respondents favored testing either all patients or only those undergoing surgery. Worldwide, a large majority of respondents answered affirmatively for testing the healthcare team (83.09%). For all the different domains on testing, some difference was observed for the different regions.
Fig. 7.
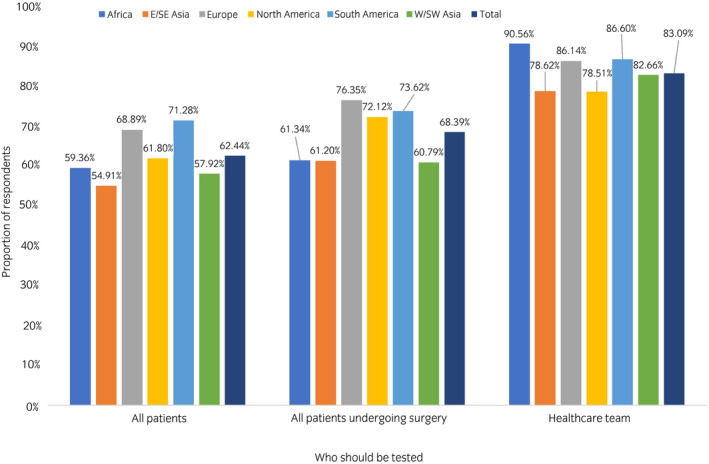
Those who should be tested for COVID‐19, by region.
Slightly more than half of respondents across all regions indicated that all surgical team members face an equal risk of contracting COVID‐19 (52.85%), followed by the anesthetist, the surgical nurse and the surgeon (Fig. 8). No significant regional differences were reported for perception of risk among surgical team members.
Fig. 8.
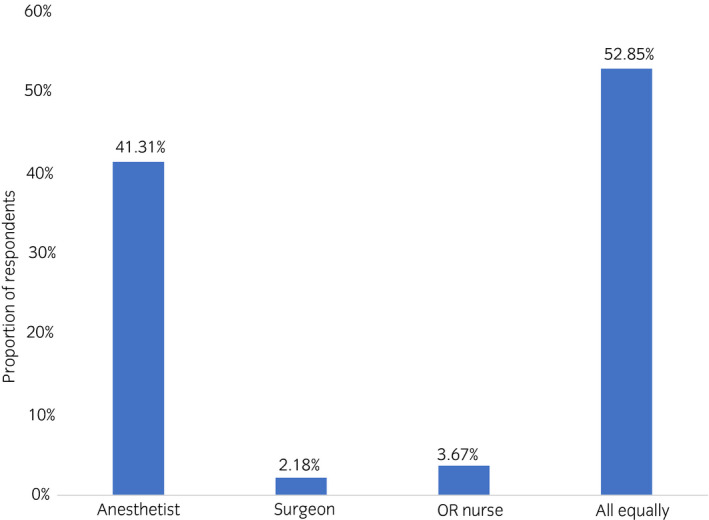
Who is perceived to be at greatest risk of contracting COVID‐19.
The survey also assessed respondents’ perceptions of how those around them react to them after being at work. Nearly one‐third of respondents reported that they had experienced social avoidance (28.97%).
Discussion
The present survey was launched under the umbrella of the SIU and distributed among all its 10 000 members. It captures the perceptions of the urological community worldwide on safety and protection in the framework of the COVID‐19 pandemic. Urologists of all ages and ethnicities, from different practice settings and from different countries, have provided a snapshot of their knowledge on a subject they were relatively unfamiliar with just weeks earlier. They also provided insights on personal attitudes and worries, and on the possible differences among different world regions.
On the subject of PPE access and use, most urologists worldwide responded that they know how to protect themselves from becoming infected with COVID‐19 at work, and that they feel moderately comfortable in their work environment. However, nearly half of the urologists responded that their hospital provides PPE of only limited types, quantities or both, and only one‐third of urologists reported that their institution provides all the required PPE for medical and surgical procedures.
These two findings – that urologists are moderately comfortable with their workplace protections, even while they might lack sufficient access to PPE – present an interesting juxtaposition. Their moderate satisfaction with the work environment might reflect either physicians’ general predisposition to self‐confidence or simply their sense of dedication. Certainly, the fact that urologists’ work environment entails fewer risks than other specialties, such as critical care or infectious disease, might also explain these seemingly contradictory responses. Furthermore, the incidence of COVID‐19 infection varied among different countries and regions. Some countries might have seen a lower incidence due to successful containment measures.
When responding to the question about the types of PPE that should be worn in the operating room and in the outpatient clinic, urologists provided a worrisome range of responses. Only one‐third of urologists were aware of the need for a specific mask as surgical PPE or would choose a face shield when operating on a non‐tested patient. Both types of protection are recommended in the specific protocols designed for surgery in times of COVID‐19. 8 , 9 , 10 , 11 There is an apparent lack of correlation between these two answers, which suggests wide variation in local or national recommendations on what PPE should be worn. When COVID‐19 emerged, the initial confusion and contradictory information meant that preliminary recommendations for worker safety and clinical care in Asia was likely outdated as new information emerged. However, the virulence of severe acute respiratory syndrome coronavirus 2 was already known by the time the pandemic spread through Europe and the Americas. 11 , 12 Understandably, respondents’ dissatisfaction with PPE shortfalls was higher in Europe, as the pandemic’s peak coincided with the survey’s distribution, and in Africa and South America, where the number of low‐ and middle‐income countries is higher than in other geographical regions. 13
Similarly, urologists gave a wide range of responses as to the relative risks of infection faced by different members of the surgical team. It was known early during the pandemic’s first weeks, and even before the World Health Organization’s pandemic declaration, that the individuals at highest risk in the operating room are those exposed to aerosols, namely, the anesthesia team. 14 This lack of uniformity in responses might be explained by the relative absence of urologists from the operating room during the pandemic. In some hospitals, only emergency or highly prioritized urological surgeries have been carried out, whereas other hospitals were converted into COVID‐19 hospitals. 13 , 15
When attitudes about testing are explored, it becomes clear that policies and beliefs regarding testing of surgical patients and of surgeons differ among urologists across the world. Two‐thirds of the respondents across all regions indicated that all patients receiving surgery should be tested; one‐quarter favored testing surgical patients only when there is clinical suspicion for COVID‐19; 6% of urologists believed only those patients awaiting elective surgery should be tested. These variations likely reflect a lack of institutional protocols, shortage of testing resources or simply the lack of consistent recommendations, as well as a combination of other unknown factors.
Almost one‐third of respondents experienced social avoidance because of their work – a remarkably high percentage, despite the fact that one of the social highlights of this medical crisis has been the acknowledgment of healthcare workers’ dedication and professionalism, especially when the pandemic’s future psychological consequences on healthcare workers’ mental health remain unknown. 16 , 17
When we compared responses and attitudes among different geographical regions, we saw evidence that African urologists felt under‐resourced. Compared with urologists from other regions, African urologists viewed their work environment as providing the least protection against COVID‐19.
At the other end of the spectrum, respondents from East/South‐East Asia, the first to bear the brunt of COVID‐19, showed signs of returning to normal practice. Urologists there had the highest comfort level with their workplace protective measures, and fewer than expected respondents experienced social avoidance based on their work.
These differences show that the way countries responded to the pandemic might have varied between regions and individual countries across the world; that there might be a time effect conditioned by the spread patterns and COVID‐19’s asynchronous movement across the globe; and that countries’ socioeconomic levels affect the opinions and feelings of its healthcare workers, in this case, urologists.
The current pandemic raises the main question of whether the healthcare work environment offers adequate protection against a highly transmissible and morbid disease. Severe acute respiratory syndrome coronavirus 2 transmission has an airborne component that potentially fuels and accelerates its spread. Although frontline healthcare workers are at the highest risk of exposure to the virus, no healthcare worker should be neglected and all deserve adequate protection.
Among others’ tasks, national and international centers for epidemiology and disease control and prevention serve their populations by identifying possible infection threats, isolating sources of infection, and establishing timely and effective measures to protect the public and control any infectious surge. National or federal governments depend mainly on these agencies to implement necessary measures, and to provide the safest possible environment for the general population and healthcare workers. 18
Individual healthcare providers, such as medical organizations and hospitals, should follow these recommendations in a responsible manner and fulfill the standards of care. Most hospitals maintain internal working groups or partnerships with the appropriate external organizations in order to achieve, maintain, and promote rigorous standards of care and follow crisis protocols. These efforts include the credentialing of medical and non‐medical staff, quality improvement, governance and leadership, prevention and control of infectious sources, information management, and securing the safety of patients and medical professionals. While many, if not most, healthcare organizations are reasonably successful in attaining these standards during normal times, the current unprecedented pandemic, although not unexpected, has revealed painful shortcomings in our current healthcare systems.
Ultimately, health professionals rely mainly on their upper management teams, but the last phase of the medical process is always the contact between the physician or healthcare professional and the patient. Although we did not specifically ask about trust in our survey, the COVID‐19 pandemic might have damaged both types of trust: the interaction of healthcare professionals with their management teams, and the interaction of healthcare professionals with their patients.
What we distill from our survey is this: urologists know what to do to protect themselves and they feel comfortable at work, likely as most non‐healthcare workers do in non‐pandemic times. However, many urologists do not have access to enough protective gear, a constant concern in most of the world’s regions. In some cases, they experience social avoidance due to their occupation. Even if there were enough COVID‐19 tests, there is no agreement about which patients should be tested. Hopefully, when normality returns, training in crisis management and regular updates on standard medical crisis protocols will be included in healthcare professional licensure requirements. 18
It is obvious that our survey had several limitations. There is a certain degree of respondents’ self‐selection bias, as surveys are inherently biased by the respondents’ own interests. Additionally, the necessary sample size to be representative was not calculated beforehand, in our haste to capture data from a rapidly developing situation. Also, participation from Africa and South America was lower than ideal, resulting in underrepresentation of these continents. However, the large number of participants far exceeded our expectations, and the variety of geographical representation allowed us to draw broad inferences on urologists’ perceptions and feelings. Although the findings can be extrapolated to similar medico‐surgical specialties during the COVID‐19 pandemic, we acknowledge that non‐physician healthcare providers involved in patient care during this time period were not the target population of the survey, and therefore might have different views and perceptions.
In conclusion, this global survey shows that urologists feel relatively safe at work, but some have experienced social avoidance due to their work. Although they are confident in their knowledge of protective measures, there is a wide variation of the specific details on the PPE measures, both in the operating room and in the outpatient clinic setting. There are also variations in preferences and recommendations for COVID‐19 testing for surgical patients. Ultimately, we also emphasize that more than half the urologists have been affected by PPE shortfalls across the world.
Conflict of interest
None declared.
Supporting information
Appendix S1. The complete survey.
Appendix S2. List of respondents’ countries by region.
Acknowledgments
The authors acknowledge support from the SIU Central Office, including Merveille de Souza, Carrie Thompson, Melissa St‐Onge, Susie Petrusa and Christine Albino, the contributions of Darcy Lewis and Alison Palkhivala for medical writing and editorial support, and Michael Barlev for statistical support.
References
- 1. Givi B, Schiff BA, Chinn SB et al. Recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA Otolaryngol. Head Neck Surg. 2020; 146: 579–84. [DOI] [PubMed] [Google Scholar]
- 2. Alhazzani W, Møller MH, Arabi YM et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID‐19). Intensive Care Med. 2020; 46: 854–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID‐19. JAMA 2020; 323: 1499–500. [DOI] [PubMed] [Google Scholar]
- 4. Sanders JM, Monogue MS, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID‐19): a review. JAMA 2020; 323: 1824–36. [DOI] [PubMed] [Google Scholar]
- 5. Zhang HF, Bo L, Lin Y et al. Response of Chinese anesthesiologists to the COVID‐19 outbreak. Anesthesiology 2020; 132: 1333–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ademuyiwa AO, Bekele A, Berhea AB et al. COVID‐19 preparedness within the surgical, obstetric and anesthetic ecosystem in Sub Saharan Africa. Ann. Surg. 2020; 272: e9–e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liang H, Archarya G. Novel corona virus disease (COVID‐19) in pregnancy: What clinical recommendations to follow? Acta Obstet. Gynecol. Scand. 2020; 99: 439–42. [DOI] [PubMed] [Google Scholar]
- 8. MacIntyre CR, Seale H, Dung TC et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5: e006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. MacIntyre CR, Dung TC, Seale H, Chughtai A. COVID‐19, shortages of masks and the use of cloth masks as a last resort. 2020. [Cited 5 Jun 2020.] Available from URL: https://bmjopen.bmj.com/content/5/4/e006577.responses#covid‐19‐shortages‐of‐masks‐and‐the‐use‐of‐cloth‐masks‐as‐a‐last‐resort
- 10. Li Y, Wong T, Chung J et al. In vivo protective performance of N95 respirator and surgical facemasks. Am. J. Ind. Med. 2006; 49: 1056–65. [DOI] [PubMed] [Google Scholar]
- 11. Desai AN, Aronoff DM Masks and Coronavirus Disease 2019 (COVID‐19). JAMA 2020; 323: 2103. [DOI] [PubMed] [Google Scholar]
- 12. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; 323: 1545–6. [DOI] [PubMed] [Google Scholar]
- 13. Hopman J, Allegranzi B, Mehtar S. Managing COVID‐19 in low‐ and middle‐income countries. JAMA 2020; 323: 1549–50. [DOI] [PubMed] [Google Scholar]
- 14. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA 2020; 323: 1439–40. [DOI] [PubMed] [Google Scholar]
- 15. Gravas S, Bolton D, Gomez R et al. Impact of COVID‐19 on urology practice: A global perspective and snapshot analysis. J. Clin. Med. 2020; 96: 1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tsai C. Personal risk and societal obligation amidst COVID‐19. JAMA 2020; 323: 1555–6. [DOI] [PubMed] [Google Scholar]
- 17. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID‐19 and physical distancing. JAMA Intern. Med. 2020; 180: 817. [DOI] [PubMed] [Google Scholar]
- 18. Lamontagne F, Angus DC Toward universal deployable guidelines for the care of patients with COVID‐19. JAMA 2020; 10.1001/jama.2020.5110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. The complete survey.
Appendix S2. List of respondents’ countries by region.


