The coronavirus disease 2019 (COVID‐19) pandemic has significantly affected health care utilization in the United States. Although reductions in routine outpatient visits and elective procedures were intentional in preparation for increases in COVID‐19–related volume, 1 National Syndromic Surveillance Program data indicate that weekly emergency department (ED) visits decreased 42% during the early stages of the pandemic. 2 This reduction may have been driven by a public fear of seeking care, 3 , 4 ultimately delaying interventions for time‐sensitive serious conditions. A group of U.S. hospitals recently reported a 38% reduction in ST‐elevation myocardial infarction (STEMI) activations, 5 and a national neuroimaging database indicated a 39% reduction in patients undergoing stroke imaging. 6 To yield a more complete picture of the COVID‐19 pandemic's effect on emergency care, we sought to describe ED visit trends for other serious diagnoses requiring acute intervention or hospitalization.
We conducted a cross‐sectional study of adult visits to seven EDs in a large health system located in greater Chicago, Illinois, with a combined 2019 visit volume of 308,000. These seven EDs include one urban academic hospital, five suburban community hospitals, and one free‐standing ED. Additional hospital characteristics are included in Data Supplement S1, Appendix S1 (, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14099/full) We measured ED visit frequencies for serious diagnoses during the early stages of the COVID‐19 pandemic (March 8 to May 2, 2020), a period of time encompassing the World Health Organization pandemic declaration on March 11, 2020, up to the date of data collection. We then compared this early pandemic period to a prepandemic period (December 31, 2019, to March 7, 2020) and a historical control period from the prior year (March 10, 2019, to April 27, 2019). Thus, the total study duration spanned from March 10, 2019, to May 2, 2020. This study was approved by the Northwestern University Institutional Review Board.
We selected a limited set of serious diagnoses associated with the need for emergency care by multiple rounds of consensus‐driven discussion. This process was guided by the priority selection of conditions requiring time‐sensitive intervention (e.g., acute myocardial infarction) or the need for timely therapy to prevent clinical deterioration (e.g., gastrointestinal hemorrhage). We were additionally guided by the need to limit the overall number of diagnoses to preserve meaningful data visualization and to minimize the risk of achieving statistical significance through multiple comparisons alone. We did not include symptom‐based diagnoses (e.g., chest pain) given that these are nonspecific by definition.
We identified International Classification of Diseases, Tenth Revision (ICD‐10), codes corresponding to selected diagnoses using the Agency for Healthcare Research and Quality Clinical Classifications Software Refined (AHRQ CCSR) system, and we grouped similar diagnoses into the following major diagnosis classes: cardiac (acute myocardial infarction, dysrhythmias, conduction disorders, coronary atherosclerosis), surgical (appendicitis, biliary tract disease, intestinal obstruction), orthopedic (dislocations, fractures), neurologic (hemorrhagic and ischemic stroke, seizure), gastrointestinal (diverticulitis, gastritis/duodenitis and ulcers, hemorrhage, pancreatitis, enteritis and colitis, hepatitis, hepatic failure), chronic respiratory (asthma, chronic obstructive pulmonary disease, heart failure), and COVID‐19 for comparison. Because the AHRQ CCSR system was created prior to the COVID‐19 pandemic, we identified these ICD‐10 codes based on Centers for Disease Control and Prevention guidance. 7 A full list of ICD‐10 codes is included as Data Supplement S1, Appendix S2.
We searched ICD‐10 codes of interest during the study period via structured query language of the health system's electronic data warehouse. We restricted our search criteria to the primary ICD‐10 code associated with the ED visit in order to avoid double counting ED visits (e.g., a single visit with both appendicitis and atrial fibrillation with rapid ventricular response).
We compared the rate of ED visits for each major diagnosis class in the early pandemic period to the prepandemic period using incidence rate ratios (IRRs) with corresponding 95% confidence intervals estimated by Poisson regression with robust standard errors in Stata v14.2. We used a two‐sided significance threshold of p < 0.05.
There were a total of 283,187 visits across the seven EDs during the study period. Mean ED volumes were 3,709 visits per week in the early pandemic period compared to 4,854 visits per week in the prepandemic period and 4,839 visits per week in the historical control period. Figure 1 shows the number of weekly ED visits for each major diagnosis class over the early pandemic and prepandemic periods. A longer time series including the historical control period is included as Data Supplement S1, Appendix S3. The first diagnosis of COVID‐19 in the health system occurred on March 4, 2020, with COVID‐19 diagnoses increasing weekly thereafter until reaching 325 ED visits in the last week of the study period. In contrast, ED visits for all major diagnosis classes decreased in the early pandemic period compared to the prepandemic period (all p ≤ 0.001): cardiac (41.0 vs. 78.3 weekly visits, IRR = 0.52 [95% CI = 0.44 to 0.62]), surgical (53.6 vs. 80.9 weekly visits, IRR = 0.66 [95% CI = 0.57‐0.77]), neurologic (40.0 vs 57.9 weekly visits, IRR = 0.69 [95% CI = 0.56 to 0.86]), orthopedic (51.5 vs 96.9 weekly visits, IRR = 0.53 [95% CI = 0.41 to 0.69]), gastrointestinal (91.3 vs 131.1 weekly visits, IRR = 0.70 [95% CI = 0.56 to 0.86]), and chronic respiratory (79.4 vs 120.6 weekly visits, IRR = 0.66 [95% CI = 0.52‐0.84]). IRRs for the early pandemic period compared to the historical control period were similarly decreased (Data Supplement S1, Appendix S4).
Figure 1.
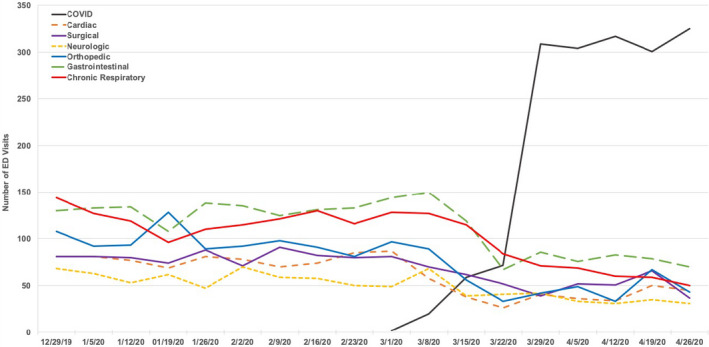
Weekly ED visits for serious diagnoses in the prepandemic and early pandemic periods, by major class.
In summary, we noted significant reductions in ED visits for all major diagnosis classes during the early stages of the COVID‐19 pandemic, including a 48% reduction in cardiac diagnoses and a 31% reduction in neurologic diagnoses. These findings support previous reports of decreased health care utilization during COVID‐19, particularly for STEMI activations and stroke neuroimaging. 5 , 6 We extend these previous reports using ED visit data and additionally report reductions in care for other serious surgical and medical diagnoses, including a 34% reduction in surgical diagnoses and a 47% reduction in orthopedic diagnoses.
The state of Illinois and the city of Chicago instituted a number of social distancing measures (e.g., statewide stay‐at‐home order, closure of city parks) in the early pandemic period to delay community transmission of COVID‐19. While these measures might be expected to reduce orthopedic injuries frequently associated with outdoor activities and motor vehicle use, they would not be expected to decrease the incidence of other major diagnoses, such as acute myocardial infarction or acute appendicitis. These diagnoses would be expected to occur at a similar rate in the early pandemic and prepandemic periods, given the random probability of any event (e.g., appendicitis) occurring in any member of the population at a given time. Our study findings therefore support ongoing concerns that the public may be refraining from seeking care for a wide breadth of serious conditions due to fears of COVID‐19 exposure in the health care setting.
It is possible that many serious diagnoses, such as acute myocardial infarction or stroke, could be directly related to primary COVID‐19 infections given the heterogeneity of disease findings reported 8 and our relative lack of knowledge regarding the pathophysiology of this novel disease. However, this possible association would be expected to increase the incidence of ED visits for these serious diagnoses (i.e., in the direction of the null hypothesis), rather than reduce the number of ED visits observed in the early pandemic period.
We did not evaluate ambulatory minor conditions (e.g., lacerations) given the focus of this study on serious time‐sensitive diagnoses, nor did we evaluate symptom‐based diagnoses, such as chest pain or headache, which may ultimately have been caused by more serious conditions undiagnosed during the ED evaluation. However, we anticipate that ED visits for both nonemergent and symptom‐based diagnoses might have similarly declined, given that others have reported that encounters for routine preventive care, such as pediatric vaccinations, have decreased during the COVID‐19 pandemic. 9
This study is limited by its focus on a single health system in the greater Chicago area. Although we compiled data from seven EDs with diverse care settings, our findings may not be generalizable to other settings with different patient population characteristics and/or local government responses to the COVID‐19 pandemic. Additionally, this study is limited by its reliance on ICD‐10 coding data, which are dependent on the impression of the treating ED physician. We attempted to minimize this limitation by excluding symptom‐based diagnoses and including diagnoses that typically require objective findings available during the ED evaluation (e.g., appendicitis). Finally, ICD‐10 codes are fundamentally a billing mechanism rather than a clinical organization system. Although we matched ICD‐10 codes to clinical diagnoses using a validated, publicly available system, it is possible that not all relevant ICD‐10 codes for serious diagnoses were captured. However, this limitation would not be expected to differentially impact our comparison of the early pandemic period to the prepandemic period.
In summary, we found significant reductions in ED visits for many emergent and time‐sensitive diagnoses during the early COVID‐19 pandemic. These findings raise concern that the public may be delaying or avoiding necessary emergency care, which may ultimately increase the burden of morbidity and mortality associated with COVID‐19, especially in light of concomitant reports that out‐of‐hospital cardiac arrests have significantly increased compared to the prior year. 10 Future efforts should focus on public health messaging regarding the necessity of seeking care for serious conditions and ensuring the safety of patients presenting to EDs during the COVID‐19 pandemic.
Supporting information
Data Supplement S1. Supplemental material.
Academic Emergency Medicine 2020;27:910–913.
The authors have no relevant financial information or potential conflicts of interest to disclose.
Supervising Editor: Arjun K. Venkatesh, MD, MBA, MHS.
Address for correspondence and reprints: Howard S. Kim, MD, MS; e‐mail: howard.kim@northwestern.edu.
References
- 1. Centers for Medicare and Medicaid Services . Non‐Emergent, Elective Medical Services, and Treatment Recommendations. 2020. Available online at: https://www.cms.gov/files/document/cms‐non‐emergent‐elective‐medical‐recommendations.pdf. Accessed May 12, 2020.
- 2. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 pandemic on emergency department visits – United States, January 1, 2019‐May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kolata G. Amid the coronavirus crisis, heart and stroke patients go missing. New York Times 2020;25:2020. [Google Scholar]
- 4. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of Covid‐19 in the young. N Engl J Med 2020;382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol 2020;75:2871–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid‐19 on stroke evaluation in the United States. N Engl J Med 2020;383:400–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention . ICD‐10‐CM Official Coding and Reporting Guidelines, April 1, 2020 through September 30, 2020. 2020. Available online at: https://www.cdc.gov/nchs/data/icd/COVID‐19‐guidelines‐final.pdf. Accessed May 12, 2020.
- 8. Chen T, Hanna J, Walsh EE, Falsey AR, Laguio‐Vila M, Lesho E. Syncope, near‐syncope, or non‐mechanical fallas as a presenting feature of COVID‐19. Ann Emerg Med 2020;76:P115–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID‐19 pandemic on routine pediatric vaccine ordering and administration – United States, 2020. MMWR Morb Mortal Wkly Rep 2020;69:591–3. [DOI] [PubMed] [Google Scholar]
- 10. Lai PH, Lancet EA, Weiden MD, et al. Characteristics associated with out‐of‐hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol 2020;e202488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Supplemental material.


