To the Editor,
The new coronavirus (coronavirus disease 2019 [COVID‐19]) pandemic has been causing, among other devastating consequences, a significant decrease on the access and search for diagnosis and treatment of other diseases that also have historically major impact on public health, such as cardiovascular diseases and cancer. This decrease can be justified by the fear of people in getting infected inside health services, and also by the worry from health providers in increasing the number of people circulating inside their facilities. The concern is also justified, among oncologic patients, after several reports pointing worst outcomes for COVID‐19 disease in patients during cancer treatment. 1 However, delay in diagnosis and treatment of cancer have negative impact in prognosis. A model for predicting the effect of COVID‐19 on cancer screening and treatment in the United States estimates almost 10 000 excess deaths to the next decade, just for breast and colorectal cancer. 2 In our institution, we observed a 55% decrease on surgical volume, and 70% on new cancer cases, comparing April 2020 to April 2019. In this setting, actions for protecting the access to health services have been proposed and are under practice during the pandemic. Despite the weakness of evidence, preoperative testing for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has been proposed for elective surgeries, as consensus statements, and questioned by others. 3 , 4 The aim of our study is to report the results of a strategy of preoperative screening based on reverse transcription‐polymerase chain reaction (RT‐PCR) test, among asymptomatic patients, in a cancer center, during the peak of pandemic in Brazil.
This is an observational, cross‐sectional, non‐comparative study. The inclusion criteria were: patients scheduled for elective surgery from 1st May to 31st May at AC Camargo Cancer Center, Sao Paulo, Brazil. Moreover, we excluded: urgent/emergent surgeries; day‐hospital surgeries; symptomatic patients for COVID‐related symptoms within 10 days before surgery. Our main outcomes were: positivity rate for COVID‐19 preoperative test and adhesion rate to the screening protocol. The screening protocol included: (a) all patients with elective surgery scheduled should be contacted and called for performing COVID‐19 test, 3 to 2 days before admission; (b) patients were tested with RT‐PCR for SARS‐CoV‐2 from nasopharyngeal swabs; (c) before surgery, all patients were oriented to remain in social isolation; (d) patients with positive results have the admission canceled, a new test is performed after 14 days, and surgery is re‐scheduled only after a negative test. Additionally, there were no additional costs to the patients, with respect to screening.
Among 707 surgeries scheduled between 1st May and 31st May 540 met the inclusion criteria. The median age was 54 years (range, 1‐93 years), and 318 (59%) patients were women. The great majority of patients (96.3%) lives in the State of Sao Paulo, and among them, 450 (83.3%) live in the City of Sao Paulo and surrounding metropolitan area. With regard to treatment costs coverage, 82 (15.2%) patients have costs covered by the Public Health System (Unified Health System‐SUS); and 458 (84.8%) were covered by health insurance companies or fully private. The distribution of primary cancer types, in treatment or in follow up, were: 166 patients with genitourinary cancer (30.7%); gastrointestinal, 96 (17.8%); breast cancer, 88 (16.3%); head and neck, 82 (15.2%); skin cancer, 59 (10.9%); others, 49 (9.1%). We stratified type of surgeries in three categories: 290 (53.7%) were oncologic resections; 135 (25.0%) were surgeries related to treatment, but without organ resection (eg implantable venous access device insertions; urinary stents; stoma reversal); 115 (21.3%) surgeries were indicated for benign conditions (eg cholecystectomy, proctological procedures), among cancer patients already treated and in follow‐up. The distribution of surgical departments, responsible for the current surgical procedure, was: gynecology: 84 (15.6%) patients; urology: 82 (15.2%); breast cancer: 81 (15.0%); head and neck: 68 (12.6%); skin cancer: 62 (11.5%); vascular surgery: 44 (8.1%); colorectal: 32 (5.9%); upper gastrointestinal cancer: 29 (5.4%); and others: 58 (10.7%). One hundred and forty four (27%) patients have received other type of cancer treatment during 3 months before surgery: 110 have received only chemotherapy; 13 received radiation therapy, and 21 were submitted to preoperative concomitant chemoradiation.
Forty one (7.6%) patients showed positive test for COVID‐19 before surgery and had the surgery postponed (Table 1). In only one (0.2%) case, the surgery was incorrectly performed without test. Twenty five (4.6%) patients have, themselves, opted to postpone surgery, reporting worry about COVID‐19 infection during admission. Another 20 (3.7%) patients had surgery canceled due to another reasons (Figure 1). Among the 454 patients (84.1%) operated after negative test, no COVID‐related symptoms or complications were observed during the in‐hospital postoperative period. We have not identified any readmission due to COVID‐19 in the postoperative period.
Table 1.
Characteristics of the 41 patients tested positive for COVID‐19 on preoperative screening, whom have surgery postponed
| Variable | N (%) |
|---|---|
| Age, y (median) | 56 (13‐76) |
| Gender | |
| Male | 18 (44) |
| Female | 23 (56) |
| City of address | |
| Sao Paulo metropolitan area | 36 (87.8) |
| Sao Paulo countryside or other state | 5 (12.2) |
| Costs coverage | |
| Public health system (SUS) | 8 (19.5) |
| Insurance/private | 33 (80.5) |
| Primary cancer | |
| Genitourinary | 15 36.6) |
| Gastrointestinal | 10 (24.4) |
| Breast | 5 (12.2) |
| Head and neck | 5 (12.2) |
| Skin | 3 (7.3) |
| Others | 3 (7.3) |
| Surgical departmenta | |
| Urology | 8 (19.5) |
| Gynecology | 7 (17.1) |
| Vascular surgery | 7 (17.1) |
| Breast | 5 (12.2) |
| Head and neck | 4 (9.8) |
| Skin cancer | 4 (9.8) |
| Others | 6 (14.6) |
Abbreviation: COVID‐19, coronavirus disease 2019.
Department responsible for the current surgical procedure.
Figure 1.
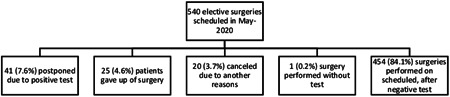
Results of the preoperative test‐based screening for coronavirus disease 2019 (COVID‐19), applied to 540 asymptomatic patients, scheduled to be operated in May 2020
According to the World Health Organization reports, Brazil is the second country in the number of cases and deaths by COVID‐19 disease, behind United States. 5 In Brazil, the State of Sao Paulo is the epicenter of the pandemic, with the majority of cases from the City of Sao Paulo and metropolitan area. By the end of May, the State of Sao Paulo reached 109 698 confirmed cases, with peaks of 6,382 new cases per day, and 324 confirmed deaths per day. 6 Unfortunately, the numbers in Brazil continued to rise during June. Despite these numbers, we decided not to stop elective surgeries, considering the implications in delaying oncologic care, and the availability of ward and intensive care unit (ICU) beds. The strategy for safety maintenance was mainly based on universal preoperative testing. A study from Seattle reported only 0.4% of positive tests among 840 asymptomatic patients tested for preoperative screening. 7 In our preliminary experience, the positivity rate was 7.6% among asymptomatic preoperative patients, with almost 100% of adhesion to the screening protocol, allowing us to perform 84.1% of the surgeries electively scheduled. Our higher positivity rate, compared with the other cited study, is certainly due to the higher contagious rate in Sao Paulo. According to recently published data by the CovidSurg group, postoperative mortality rates among COVID‐positive patients was 19.1% for elective surgeries, but it can reach 27.1% for the oncologic subgroup. 8 Extrapolating this rate to our results, we can estimate that up to seven to nine deaths have been potentially avoided by applying the preoperative test. In conclusion, if ward and ICU beds are available, elective oncologic surgeries can be scheduled safely with preoperative screening for COVID‐19 based on systematic RT‐PCR testing, even in high incidence areas of COVID‐19.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
REFERENCES
- 1. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sharpless NE. COVID‐19 and cancer. Science. 2020;368(6497):1290. [DOI] [PubMed] [Google Scholar]
- 3. Lu AC, Schmiesing CA, Mahoney M, et al. COVID‐19 preoperative assessment and testing: from surge to recovery. Ann Surg. 2020;10:1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bogani G, Signorelli M, Ditto A, Raspagliesi F. Surgical oncology at the time of COVID‐19 outbreak. J Surg Oncol. 2020;122:115‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Coronavirus Disease (COVID-19) Dashboard. Situation by country, territory or area. Retrieved July 20, 2020 from https://covid19.who.int
- 6.SP contra o novo coronavirus. Boletim completo. Retrieved July 20, 2020 from https://www.seade.gov.br/coronavirus
- 7. Ferenczi BA, Baliga C, Akl P, et al. Pre‐procedural COVID‐19 screeningof asymptomatic patients: a model for protecting patients, community and staff during expansion of surgical care. NEJM Catal. 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0261 [Google Scholar]
- 8. COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS‐CoV‐2 infection: an International Cohort Study. Lancet. 2020;S0140‐6736(20):31182‐3118. [DOI] [PMC free article] [PubMed] [Google Scholar]


