Abstract
Background and purpose
Ischaemic stroke has been described in association with COVID‐19. Several pathophysiological mechanisms have been suggested, i.e. prothrombotic state, cardiac injury etc. It was sought to assess the potential association between ischaemic stroke associated with SARS‐CoV‐2 infection and underlying atherosclerotic lesions.
Methods
A retrospective analysis of stroke related to large vessel occlusion was conducted amongst patients with SARS‐CoV‐2 infection and underlying mild atherosclerotic disease, between 19 March and 19 April 2020 in six different stroke centers in the Île‐de France area, France.
Results
The median age was 52 years, median body mass index was 29.5 kg/m2. All patients displayed previous vascular risk factors such as high blood pressure, diabetes, dyslipidemia or body mass index > 25. The delay between the first respiratory symptoms of COVID‐19 and stroke was 11.5 days. At baseline, all had tandem occlusions, i.e. intracerebral and extracerebral thrombus assessed with computed tomography or magnetic resonance imaging. Cases displayed a large thrombus in the cervical carotid artery with underlying mild non‐stenosing atheroma, after an etiological workup based on angio‐computed tomography or magnetic resonance imaging and/or cervical echography.
Conclusion
Our study should alert clinicians to scrutinize any new onset of ischaemic stroke during COVID‐19 infection, mainly in patients with vascular risk factors or underlying atherosclerotic lesions.
Keywords: atherosclerotic disease, cardiovascular disease, COVID, intravascular clotting, ischaemic stroke, large vessel occlusion
Introduction
The pandemic outbreak of coronavirus disease 19 (COVID‐19) was first described as a flu‐like syndrome with respiratory symptoms [1]. However, neurological symptoms have been reported in 31% of cases, with 6% of cerebrovascular disease [2]. A limited number of strokes associated with COVID‐19 have been described, either occurring in young patients (n = 5) or associated with antiphospholipid antibodies or hypercoagulability (n = 9) [3, 4, 5]. The cause of stroke was suggested to be related to the coagulopathy induced by COVID‐19 infection and the associated inflammation [6].
Here, healthcare providers are warned about the catastrophic association of stable atherosclerotic disease and COVID‐19 infection which may precipitate acute stroke.
Accordingly, six cases of patients with SARS‐CoV‐2 infection who developed large vessel ischaemic stroke, all with large intraluminal thrombus and mildly, stable, underlying atherosclerotic lesions are reported here. The demographic, clinical, radiological and laboratory characteristics of six consecutive patients admitted for ischaemic stroke associated with SARS‐CoV‐2 infection are described.
The study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the Research Ethics Committee of Foch Hospital. Oral consent was obtained from patients or next of kin.
Results
A retrospective analysis of stroke related to large vessel occlusion was conducted amongst patients with SARS‐CoV‐2 infection and underlying mild atherosclerotic disease.
Six cases of large vessel occlusion on mild atherosclerotic lesions were admitted during the study period between 19 March and 19 April 2020 in six different stroke centers in the Île‐de‐France area, France.
The median age was 52 years, median body mass index (BMI) was 29.5 kg/m2. All patients displayed previous vascular risk factors such as high blood pressure, diabetes, dyslipidemia or BMI > 25.
The delay between the first respiratory symptoms of COVID‐19 and stroke was 11.5 days. The diagnosis of SARS‐CoV‐2 infection was asserted by polymerase chain reaction or thoracic computed tomography (CT) scan for all patients. Four of the six reported cases displayed no/mild respiratory symptoms. All the patients showed an increase in inflammatory markers and a hypercoagulability state (elevation of D‐dimer or C‐reactive protein).
At baseline, all had tandem occlusions, i.e. intracerebral and extracerebral thrombi assessed by CT or magnetic resonance imaging. All cases except one (patient 1) displayed a large thrombus in the cervical carotid artery with underlying mild non‐stenosing atheroma, after an etiological workup based on angio‐CT or magnetic resonance imaging and/or cervical echography. They were classified as stroke of undetermined etiology according to the TOAST classification. Although no underlying atherosclerotic lesion was found, patient 1 displayed BMI = 33, high blood pressure and diabetes in his medical history. The rest of the etiological workup was negative for these patients (Fig. 1, Table 1).
Figure 1.
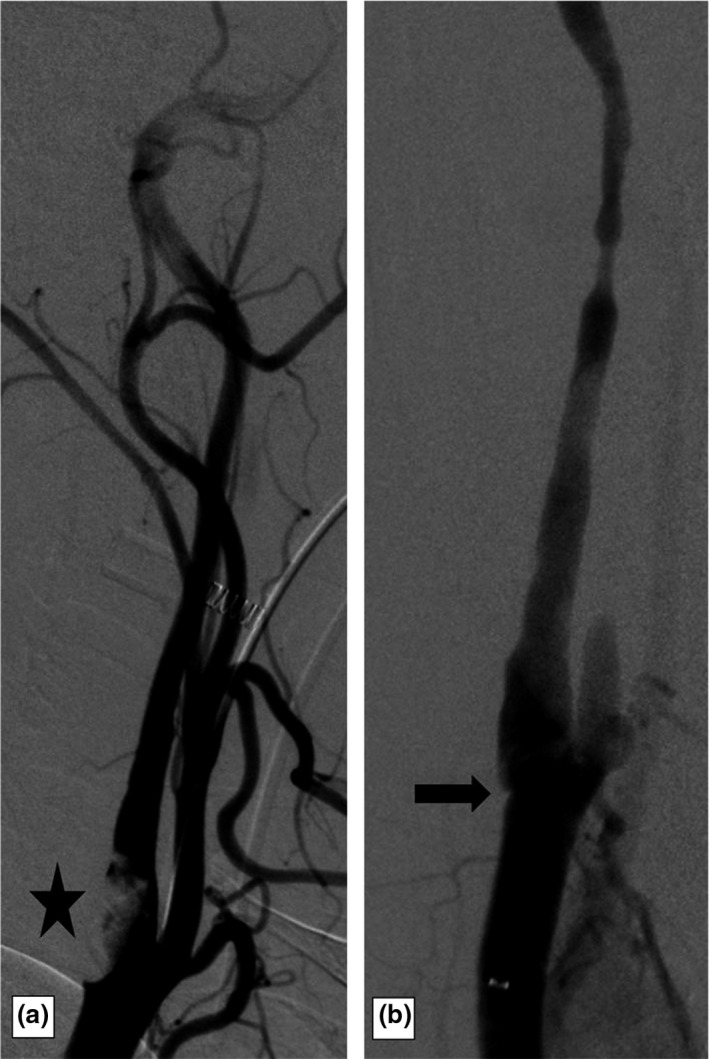
Ischaemic stroke, 50‐year‐old patient (case 3). Large intraluminal carotid artery thrombus on the carotid artery angiogram (star, a). Recanalization of the carotid after the endovascular procedure with an underlying mild atherosclerotic lesion (arrow, b).
Table 1.
Demographic, clinical, paraclinical and outcome findings
| Case number | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Age (years) | 42 | 60 | 50 | 45 | 60 | 54 |
| Sex | Male | Female | Male | Female | Male | Male |
| Medical history | HBP, diabetes | Dyslipidemia | Dyslipidemia | No | None | HBP, diabetes |
| Symptoms at disease onset | Aphasia and right hemiplegia | Right hemiplegia confusion | Hemiplegia limb ischaemia | Aphasia and right hemiplegia | Fever and mild dyspnea | Right weakness aphasia |
| Days from disease onset to ischaemic stroke | 11 | 11 | 13 | 4 | 12 | 13 |
| BMI | 33 | 35 | 33 | 26 | 26 | 22 |
| NIHSS at stroke onset | 20 | 22 | 14 | 26 | 4 | 20 |
| Site of occlusion | Common and external and internal carotid artery and MCA | Tandem occlusion with terminus carotid artery and MCA | Tandem occlusion with terminus carotid artery and MCA | Tandem occlusion with terminus carotid artery and MCA | Tandem occlusion with terminus carotid artery and MCA | Tandem occlusion with terminus carotid artery and MCA |
| Stroke topography | Anterior | Anterior | Anterior | Anterior | Anterior | Anterior |
| Side of stroke | Left | Left | Right | Right | Left | Left |
| Symptoms of COVOD‐19 severity | Mild (cough) | Severe | Severe (pulmonary embolism) | No | Severe (ARDS) | Cough |
| COVID diagnosis | Thorax CT scanner | Thorax CT scanner | PCR + | Thorax CT scan + PCR+ | PCR+ | Thorax CT scan |
| D‐dimers (µg/ml) | 19461 | 5315 | 13010 | 11970 | >4000 | 1580 |
| High‐sensitivity C‐reactive protein (mg/ml) | 30 | 158 | 32 | 137.9 | 288 | 4 |
| Platelet count | 279 000 | 253 000 | 211 000 | 371 000 | 325 000 | 424 000 |
| Antiphospholipid antibodies/anti B2‐glycoprotein 1 | Negative/negative | IgM 15/B2GP1 = 23 | Not done | Negative/negative | Negative/negative | Not done |
| Lupus anticoagulant | Negative | Negative | Not done | Positive | Positive | Not done |
| Acute stroke treatment | IVT and EVT | Heparin IV | EVT | EVT | Antiplatelet | Antiplatelet |
| Etiology work‐up | Cryptogenetic | Normal, except a thin atheromatous plaque | Normal, except a thin atheromatous plaque | Normal, except a thin atheromatous plaque | Normal, except a thin atheromatous plaque | Normal, except a thin atheromatous plaque |
| Etiology classification (TOAST) | Stroke of undetermined etiology | Stroke of undetermined etiology | Stroke of undetermined etiology | Stroke of undetermined etiology | Stroke of undetermined etiology | Stroke of undetermined etiology |
| Clinical follow‐up | Death | Death | Death | Discharge to rehabilitation center | Discharge to rehabilitation center | Discharge to rehabilitation center |
ARDS, acute respiratory distress syndrome; B2GP1, beta‐2 glycoprotein 1; BMI, body mass index; CT, computed tomography; EVT, endovascular treatment; HBP, high blood pressure; IgM, immunoglobulin M; IVT, intravenous thrombolysis; MCA, middle cerebral artery; NIHSS, National Institutes of Health Stroke Scale; PCR, polymerase chain reaction.
Concerning the outcome, three patients had died and three were discharged to a rehabilitation center.
Discussion
The mechanisms of ischaemic stroke associated with SARS‐CoV‐2 infection are poorly understood [6, 7, 8]. The prothrombotic state associated with COVID‐19 infection has been proposed to be responsible, as for pulmonary embolism [9]. Furthermore, circulating inflammatory factors (e.g. interleukin and C‐reactive protein) are responsible for early molecular events triggered by coagulation abnormalities.
Major prognostic factors of the SARS‐CoV‐2 infection encompass a medical history of vascular disease and risk factors of atherosclerotic disease (obesity, high blood pressure, diabetes). Our observations of acute ischaemic stroke in patients with SARS‐CoV‐2 infection are in accordance with the reported high‐risk profile of patients admitted with the most severe form of SARS‐CoV‐2 infection [1, 10].
Our observations illustrate large vessel occlusion associated with clotting induced by SARS‐CoV‐2 infection complicating underlying stable atherosclerotic disease. Complications of atherosclerotic disease by viral infection have previously been described [11, 12] but the heavy burden of the current COVID outbreak has permitted an infrequent complication of atheroma associated with viral infection to be described. Direct (invasion by virus) or indirect mechanisms (inflammatory/procoagulant status) have also been debated [7, 13]. Our report does not provide definitive evidence whether the clotting in the internal carotid artery is related to the underlying atherosclerosis or whether this is simply an epiphenomenon, given the high prevalence of atherosclerotic disease. However, in the reported cases, clotting was described only at the surface of the atherosclerotic plaque and in the downstream circulation. Multiple clotting in different arteries was not observed in these cases, supporting the potential causal effect of the underlying atherosclerotic lesion.
The observation of these large vessel occlusions amongst COVID patients with mild atherosclerotic disease could represent important clinical findings to warn healthcare providers about the high‐risk profile of patients with vascular risk factors. Thus, the community needs to be alerted on the risk of precipitating severe complications due to underlying atheroma.
This study has several limitations. It is a retrospective report. Whilst it may not be generalizable, our study should alert clinicians to scrutinize any new onset of ischaemic stroke during COVID‐19 infection, mainly in patients with vascular risk factors or underlying atherosclerotic lesions.
Disclosure
The authors declare no financial or other conflicts of interest.
Acknowledgement
Mary Osborne‐Pellegrin is thanked for help in editing the final draft of the manuscript.
Funding: None.
The manuscript has not been submitted elsewhere or published elsewhere in whole or in part.
Data availability statement
The data will be available to others on reasonable requests to the corresponding author.
References
- 1. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020; 77: 683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bowles L, Platton S, Yartey N, et al. Lupus anticoagulant and abnormal coagulation tests in patients with COVID‐19. N Engl J Med 2020; 383: 288–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of COVID‐19 in the young. N Engl J Med. 2020; 382: e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID‐19. J Neurol Neurosurg Psychiatry 2020; 91: 889–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID‐19. N Engl J Med 2020; 382: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Madjid M, Safavi‐Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020; 5: 831. [DOI] [PubMed] [Google Scholar]
- 8. Valderrama EV, Humbert K, Lord A, Frontera J, Yaghi S. Severe acute respiratory syndrome coronavirus 2 infection and ischemic stroke. Stroke 2020; 51:STROKEAHA120030153. [DOI] [PubMed] [Google Scholar]
- 9. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020; 18: 844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA 2020; 323: 2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boehme AK, Luna J, Kulick ER, Kamel H, Elkind MSV. Influenza‐like illness as a trigger for ischemic stroke. Ann Clin Transl Neurol 2018; 5: 456–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grau AJ, Buggle F, Becher H, et al. Recent bacterial and viral infection is a risk factor for cerebrovascular ischemia: clinical and biochemical studies. Neurology 1998; 50: 196–203. [DOI] [PubMed] [Google Scholar]
- 13. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID‐19. Lancet 2020; 395: 1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data will be available to others on reasonable requests to the corresponding author.


