Abstract
Background
Physicians play a crucial frontline role in the COVID‐19 pandemic, which may involve high levels of anxiety. We aimed to investigate the association between pandemic‐related stress factors (PRSF) and anxiety and to evaluate the potential effect of resilience on anxiety among physicians.
Methods
A self‐report digital survey was completed by 1106 Israeli physicians (564 males and 542 females) during the COVID‐19 outbreak. Anxiety was measured by the 8‐item version of the Patient‐Reported Outcomes Measurement Information System. Resilience was evaluated by the 10‐item Connor–Davidson Resilience Scale. Stress was assessed using a PRSF inventory.
Results
Physicians reported high levels of anxiety with a mean score of 59.20 ± 7.95. We found an inverse association between resilience and anxiety. Four salient PRSF (mental exhaustion, anxiety about being infected, anxiety infecting family members, and sleep difficulties) positively associated with anxiety scores.
Conclusions
Our study identified specific PRSF including workload burden and fear of infection that are associated with increased anxiety and resilience that is associated with reduced anxiety among physicians.
Keywords: anxiety, COVID‐19, mental health, resilience, stress
1. INTRODUCTION
In December 2019, a novel coronavirus outbreak (COVID‐19) emerged in Wuhan, China (Q. Li et al., 2020) and spread to many countries, including Israel, where the first case was diagnosed on February 20, 2020. The pandemic generated widespread anxiety in the general population and among healthcare workers. Physicians and other healthcare workers play a crucial frontline role in the management of the pandemic, and based on both research (Lai et al., 2020) and media reports (Gold, 2020; NHS under pressure: voices from the frontline of the coronavirus crisis, n.d.), are facing increasing emotional burdens and levels of anxiety. Anxiety may interfere with physicians' functioning under stress, their decision‐making abilities, and may have long‐term effects on their well‐being (Fahrenkopf et al., 2008; Gong et al., 2014). A better understanding of modifiable factors associated with anxiety related to the COVID‐19 outbreak among physicians has become a matter of urgency.
A recent cross‐sectional study examined mental health outcomes among healthcare workers treating patients with COVID‐19 in China and reported a high prevalence of depression (50.4%), anxiety (44.6%), insomnia (34.0%), and distress (71.5%; Lai et al., 2020). Nurses, women, workers in Wuhan, and frontline workers reported more symptoms on all measurements (Lai et al., 2020). Only 39.2% of the study participants were physicians, however, and the authors did not investigate modifiable factors that influence severe physicians' mental health.
Studies conducted during large‐scale worldwide health crises (the Severe Acute Respiratory Syndrome [SARS] outbreak, the H1N1 pandemic [Goulia, Mantas, Dimitroula, Mantis, & Hyphantis, 2010; Imai et al., 2010], and Ebola [L. Li et al., 2015]) have shown that several factors are associated with increased psychological distress among healthcare workers. These included concerns of fear of infecting family members and friends (Goulia et al., 2010; Maunder et al., 2003), uncertainty about the health consequences of the disease (Goulia et al., 2010), perception of risk to themselves (Nickell et al., 2004; Styra et al., 2008), living with children (Nickell et al., 2004), being placed in quarantine (Bai et al., 2004), and stigmatization and social isolation (Bai et al., 2004; Can et al., 2005; Maunder et al., 2003; Nickell et al., 2004).
In addition to studying the effect of the above‐mentioned factors on physicians' anxiety during the COVID‐19 pandemic, we wished to examine the effect on the anxiety of another key factor, resilience. Resilience, defined as the act of coping, adapting, or thriving from adversity, is a protective factor against adversity, and it has been inversely associated with the experience of workplace stress and anxiety among physicians (Fletcher & Sarkar, 2013; Haddadi & Ali Besharat, 2010).
The present exploratory study aims to measure the level of anxiety among physicians during the COVID‐19 outbreak and to identify potential anxiety associated with modifiable risk and protective factors.
2. METHODS
2.1. Participants
The first patient COVID‐19 lab‐confirmed patient in Israel was identified on February 20, 2020. The first COVID‐19‐related death in Israel was reported on March 20. We conducted a national cross‐sectional survey of a nonprobability sample of physicians in Israel. The analytic sample for the current study included respondents who consented to participate in the survey between March 19 to March 22, 2020. During that time, the number of COVID‐19‐related cases in Israel grew from 153 (on March 19) to 264 (on March 22). We used a mixed‐modes survey design in which separate or overlapping samples are approached with a combination of different modes. The primary mode was an internet survey of specifically named physicians, for which we used a list‐based sampling frame of working email addresses of the Israel Medical Association (IMA). The other mode was posting the survey in physicians' forums on Facebook. While the mean age of the IMA membership and responders was similar (48.7 ± 16.9 vs. 46.1 ± 13.2, respectively), the proportion of female physicians among responders was somewhat higher compared with the study's source population (49.0% vs. 40.3%, respectively). Representation of medical specialties among responders was generally similar to that of the IMA membership (Table S1). We followed the standards and ethics of the American Association for Public Opinion Research reporting guidelines (The American Association for Public Opinion Research, 2016). The study protocol was approved by the Institutional Review Board of the Sheba Medical Center.
2.2. Assessment
Self‐administered anonymous questionnaires were answered digitally through a secured digital platform (Qualtrics). Responses were saved on a secured server at the Sheba Medical Center. The questionnaires consisted of four modules: (a) Sociodemographic characteristics included age, sex, living with children at home (yes/no), working at a hospital (yes/no), medical specialty, level of exposure to COVID‐19 patients (direct contact with the confirmed patient, direct contact with nonconfirmed patients, no contact with patients), workload (more than usual, as usual, less than usual), being quarantined (yes/no); (b) Anxiety was assessed using the 8‐item Hebrew version of the Patient‐Reported Outcomes Measurement Information System (PROMIS) Anxiety Module (Cronbach's α coefficient .92, p < .0001), a well‐accepted self‐report tool developed by the National Institute of Health for measuring symptoms of anxiety (Schalet et al., 2016). Each item is rated from 1—“never” to 5—“always.” Following the World Health Organization guidelines for the process of translation and adaptation of instruments, we adopted the well‐established method of forward‐translation and back‐translation by bilingual mental health professionals, with the latter being blinded to the original English version of the PROMIS (Yardeni et al., 2020). (c) Stress was assessed using an inventory of pandemic‐related stress factors (PRSF; Cronbach's α coefficient .73, p < .0001), compiled from questions that proved to be pertinent in previous research on the SARS and N1H1 pandemics (Imai et al., 2010). A 4‐point Likert‐type scale was used for item scoring (0—“never” to 3—“always”); (d) Resilience was assessed using the well‐validated 10‐item Connor–Davidson Resilience Scale (CD‐RISC‐; Cronbach's α coefficient .88, p < .0001), in which items are rated from 0 (not true at all) to 4 (true nearly all the time) (Campbell‐Sills & Stein, 2007). We computed Cronbach's α coefficients to verify the internal consistency of the study's instruments as a measure of their internal reliability.
2.3. Statistical analysis
We used descriptive statistics to present the sociodemographic characteristics, anxiety, resilience, and PRSF. We conducted multivariable linear regression with the PROMIS Anxiety score as a dependent variable to evaluate the crude association between anxiety, PRSF, and resilience and assessed its robustness when adjusted for age and sex. PRSF were chosen to be included in the model based on the knowledge accrued through research of previous pandemics (Imai et al., 2010), nonnegligible crude correlation coefficient with anxiety, and low probability of random error. Several PRSF were not entered into the model due to multicollinearity with predictors of a similar construct (e.g., physical exhaustion, lack of knowledge about infectiveness, and virulence, etc.).
To assess the likelihood of type I error we tested for statistical significance with α set at .05. All tests were two‐tailed. Statistical analysis was conducted with the IBM Statistical Package for the Social Sciences v.25 for Windows (IBM Inc., Chicago, IL).
3. RESULTS
The survey responses to the sociodemographic characteristics, anxiety and resilience scores, and PRSF are presented in Table 1. The sample included physicians from a broad array of medical specialties (Table 1). A total of 1,106 physicians (mean age 46.07 ± 13.20 years, range 25–88; 542 females, 49.0%) completed the study questionnaire during the first four days of the survey and were included in the analyses. Notably, among all the PRSF, only a small minority of the study sample felt protected by the national and local government (n = 154, 13.9%) and by hospital and healthcare systems (n = 166, 15.0%) during the pandemic. Moreover, the majority of physicians reported coming to work because they feel mission‐driven to do so (n = 701, 63.4%). A higher rate of physicians reported anxiety about infecting family members rather than about being infected themselves (52.8% vs. 20.9%, respectively, χ 2(1) = 169.6, p < .0001). The mean PROMIS Anxiety score of the entire sample was 59.20 ± 7.95, and the mean CD‐RISC score was 29.05 ± 6.28.
Table 1.
Sociodemographic characteristics, anxiety and resilience scores, and pandemic‐related stress factors of the study sample (N = 1,106)
| Characteristic | Mean ± SD (range) | Sample, n (%) |
|---|---|---|
| Age, years | 46.07 ± 13.20 (25–88) | |
| 25–30 | 98 (8.9) | |
| 30–40 | 394 (35.6) | |
| 41–50 | 229 (20.7) | |
| 51–60 | 176 (15.9) | |
| 61–70 | 162 (14.6) | |
| ≥71 | 47 (4.2) | |
| Female | 542 (49.0) | |
| Home quarantined | 54 (4.9) | |
| Living with children at home | 704 (63.6) | |
| Hospital employee | 737 (66.6) | |
| Physical contact with nonconfirmed cases | 737 (66.6) | |
| Exposed to confirmed COVID‐19 cases | 70 (6.3) | |
| Medical specialty | ||
| Medicine | 323 (29.2) | |
| Primary care and emergency medicine | 286 (25.9) | |
| Surgery | 281 (25.4) | |
| Pediatrics | 133 (12.0) | |
| Psychiatry and child and adolescent psychiatry | 83 (7.5) | |
| Outcome measures | Score mean ± SD | |
|---|---|---|
| PROMIS Anxiety | 59.20 ± 7.95 | |
| CD‐RISC | 29.05 ± 6.28 |
| Pandemic‐related stress factors | Score mean ± SD | Often or always n (%) |
|---|---|---|
| Feeling mission‐driven to work | 2.85 ± 0.92 | 701 (63.4) |
| Anxiety about infecting family members | 2.65 ± 0.90 | 584 (52.8) |
| Childcare burden | 2.24 ± 1.21 | 422 (38.1) |
| Mental exhaustion | 2.16 ± 0.94 | 393 (35.5) |
| Financial concerns | 2.26 ± 0.92 | 391 (35.3) |
| Physical exhaustion | 1.97 ± 0.88 | 282 (25.5) |
| Feeling of being isolated and shunned by others | 1.92 ± 0.94 | 274 (24.8) |
| Increased workload | 1.91 ± 0.89 | 255 (23.0) |
| Sleep difficulties | 1.81 ± 0.88 | 245 (22.1) |
| Anxiety about being infected | 2.00 ± 0.78 | 232 (20.9) |
| Lack of knowledge about infectiveness and virulence | 1.82 ± 0.85 | 229 (20.7) |
| Lack of knowledge about prevention and protection | 1.81 ± 0.83 | 221 (19.9) |
| Feeling of being protected by hospital or healthcare systems | 1.81 ± 0.78 | 166 (15.0) |
| Feeling obligated to go to work | 1.62 ± 0.81 | 156 (14.1) |
| Feeling of being protected by national and local government | 1.70 ± 0.78 | 154 (13.9) |
Abbreviations: CD‐RISC, Connor–Davidson Resilience Scale; CI, confidence interval; OR, odds ratio; PROMIS, Patient‐Reported Outcomes Measurement Information System; SD, standard deviation.
The factors that were most strongly associated with anxiety in the multivariable linear regression were mental exhaustion, anxiety about being infected, anxiety about infecting family members, and sleep difficulties. Those variables alone explained nearly half of the variance in PROMIS Anxiety scores (adjusted R 2 = .43). The model also showed that resilience was negatively associated with anxiety (β coefficient = −0.18; 95% confidence interval: −0.23 to −0.14; p < .0001; Table 2). The mean PROMIS Anxiety scores across PRSF (low vs. high levels) are presented in Figure 1.
Table 2.
Association between resilience, pandemic‐related stress factors, and anxiety among physicians, in multivariable linear regression analysis with anxiety as dependent variable (N = 1,006)
| Variable | B (95% CI)* | β (95% CI)* | p Value |
|---|---|---|---|
| Resilience | −0.24 (−0.30 to −0.18) | −0.18 (−0.23 to −0.14) | <.0001 |
| Mental exhaustion | 3.36 (2.50–4.23) | 0.20 (0.15–0.26) | <.0001 |
| Anxiety about being infected | 3.69 (2.75–4.63) | 0.19 (0.14–0.24) | <.0001 |
| Anxiety about infecting family | 2.98 (2.17–3.79) | 0.18 (0.13–0.24) | <.0001 |
| Sleep difficulties | 2.35 (1.43–3.27) | 0.12 (0.07–0.17) | <.0001 |
| Feeling obligated to go to work | 1.67 (0.62–2.71) | 0.07 (0.02–0.12) | <.001 |
| Lack of knowledge about prevention and protection | 1.30 (0.40–2.21) | 0.06 (0.02–0.11) | .005 |
| Living with children | 0.70 (−0.04 to 1.44) | 0.04 (−0.00 to 0.09) | .063 |
| Feeling mission‐driven to work | 0.68 (−0.07 to 1.43) | 0.04 (−0.00 to 0.08) | .076 |
| Financial concerns | 0.44 (−0.29 to 1.17) | 0.02 (−0.02 to 0.07) | .330 |
| Feeling of being protected by hospital or healthcare systems | −0.62 (−1.57 to 0.33) | −0.02 (−0.07 to 0.02) | .200 |
Note: R = .721, Adjusted R 2 = .513.
Abbreviations: B, unstandardized B coefficient; CI, confidence interval; β, standardized β coefficient.
Adjusted for age and sex.
Figure 1.
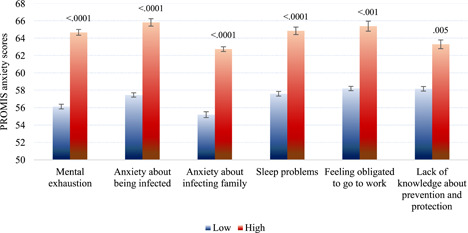
Distribution of mean Patient‐Reported Outcomes Measurement Information System (PROMIS) Anxiety scores across pandemic‐related stress factors (low vs. high levels). Error bars represent standard errors
4. DISCUSSION
Physicians and other healthcare workers have a major role at times of large‐scale public health crises, such as the current COVID‐19 pandemic. We investigated the role of resilience and PRSF associated with physicians' anxiety during the pandemic. Understanding these factors has a heuristic value for public planning and interventions aiming to reduce physicians' anxiety and improving their ability to cope with the enormous challenges of treating patients during the COVID‐19 pandemic.
Our findings of physicians reporting high levels of anxiety are in line with a recently published report on mental health outcomes among healthcare workers exposed to the COVID‐19 pandemic in China (Lai et al., 2020), as well as to reports about the 2003 SARS epidemic (Bai et al., 2004; Chong et al., 2004).
We revealed an inverse association between anxiety and prepandemic resilience. Resilience refers to the act of coping, adapting, or thriving from adversity, and reflects a complex and dynamic interplay between individual, environmental, and sociocultural domain (Venegas, Nkangu, Duffy, Fergusson, & Spilg, 2019). Resilience has been shown to be a promotable protective factor against anxiety and work‐related stress among physicians (Cleary, Kornhaber, Thapa, West, & Visentin, 2018).
We explored the effect of potentially salient PRSF on anxiety based on factors identified in previous research on pandemics (Bai et al., 2004; Goulia et al., 2010; Maunder et al., 2003; Nickell et al., 2004; Styra et al., 2008; Tam, Pang, Lam, & Chiu, 2004). Consistent with prior studies (Maunder et al., 2003; Tam et al., 2004), we found higher rates of anxiety among physicians about infecting family members than about becoming infected themselves (Chen et al., 2020). We believe that the unpredictable course of COVID‐19 infection and uncertainty about the effectiveness of currently available treatment could provoke anxiety among healthcare workers caring for these patients. In addition, it is presumable that physicians may avoid close contact with their loved ones in an attempt to reduce the risk of infecting, which in turn might further increase mental burden and anxiety.
In line with recent studies conducted with healthcare workers in China during the COVID‐19 pandemic (Wang et al., 2020; Wu & Wei, 2020; Zhang et al., 2020), we found a positive association between sleep difficulties and higher levels of anxiety among physicians. Of note, during the pandemic physicians were working long hours and were doing more night shifts which may have disrupted their circadian rhythm and led to insomnia and sleep difficulties. Addressing physician's sleep problems during the COVID‐19 pandemic is important because of their negative effect on cognition, performance, and relations among workers (Goel, Basner, Rao, & Dinges, 2013; Swanson et al., 2011; Wada et al., 2008). It is also plausible that reported insomnia and sleeping problems were in fact secondary to anxiety (Oh, Kim, Na, Cho, & Chu, 2019; Soehner & Harvey, 2012).
The main strengths of our study include a sizable sample of physicians, real‐time reporting which reduces the likelihood of recall bias, use of acceptable and well‐validated tools for assessing anxiety and resilience, and low proportion of missing data. Another advantage of our study stems from the fact that Israel is a geographically small country, whereupon the adversities of the current COVID‐19 pandemic are experienced simultaneously nationwide, making the sample representative of the average exposure of the physicians' population.
This study also has several limitations that bear mention. First, its cross‐sectional design limits the arrival at conclusions about directionality. Another limitation is the response rate. It is possible, that the physicians who participated in our study are different from nonresponders in terms of the outcome measures, which might introduce a selection bias that could potentially affect the internal validity of our results as well as limit their generalizability. Even if our findings are generalizable to Israeli physicians, they might not be fully applicable to physicians in other countries. Finally, there might be a potential reporting bias, since physicians might underreport their levels of anxiety at times of global crisis.
To the best of our knowledge, our study is the first to assess modifiable PRSF and resilience and their association with anxiety among physicians during a major global health crisis. Our findings offer an additional dimension of how physicians are facing such excruciating challenges.
Future research should focus on developing better measures of resilience that would capture constructs that are unique to pandemics, and study the differential effect of protective processes on diverse populations at different levels of risk exposure (Ungar & Theron, 2019). Controlled trials of potential anxiety‐reducing strategies such as focused resilience training, optimal workload management, and risk communication are also recommended (Goulia et al., 2010; Maunder et al., 2003; Ranney, Griffeth, & Jha, 2020). Finally, the effect of increasing the visibility of team leaders on strengthening team endurance during missions should also be tested (Hershkovich, Gilad, Zimlichman, & Kreiss, 2016; Shanafelt, Ripp, & Trockel, 2020).
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
All authors contributed, reviewed, and approved the final manuscript. M. M., N. H. P., I. M. P., A. A., A. Z., Y. K., D. G., and R. G. were responsible for conceiving and designing the study. M. M., N. M., and N. H. P. collected the data. N. H.P. conducted statistical analyses. M. M., N. H. P., S. D. I., R. G., and D. G. interpreted the data. M. M., N. H. P., S. D. I., R. G., and D. G. wrote the final manuscript.
Supporting information
Supporting information
ACKNOWLEDGMENT
This study was supported by a grant from Foundation Dora and by the Binational Science Foundation (Grant No. 2017369).
Mosheva M, Hertz‐Palmor N, Dorman Ilan S, et al. Anxiety, pandemic‐related stress and resilience among physicians during the COVID‐19 pandemic. Depression and Anxiety. 2020;37:965–971. 10.1002/da.23085
Raz Gross and Doron Gothelf are senior authors with equal contribution.
Mariela Mosheva and Nimrod Hertz‐Palmor contributed equally as first author.
Contributor Information
Raz Gross, Email: raz.gross@sheba.health.gov.il.
Doron Gothelf, Email: gothelf@tauex.tau.ac.il.
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
REFERENCES
- Bai, Y. M. , Lin, C. C. , Lin, C. Y. , Chen, J. Y. , Chue, C. M. , & Chou, P. (2004). Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatric Services, 55(9), 1055–1057. 10.1176/appi.ps.55.9.1055 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L. , & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20, 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Can, W. , Learn, W. , Koh, D. , Lim, M. K. , Chia, S. E. , & Ko, S. M. (2005). Risk perception and impact of Severe Acute Respiratory Syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Medical Care, 43(7), 676–682. [DOI] [PubMed] [Google Scholar]
- Chen, Q. , Liang, M. , Li, Y. , Guo, J. , Fei, D. , Wang, L. , … Zhang, Z. (2020). Mental health care for medical staff in China during the COVID‐19 outbreak. The Lancet Psychiatry, 7(4), e15–e16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong, M. Y. , Wang, W. C. , Hsieh, W. C. , Lee, C. Y. , Chiu, N. M. , Yeh, W. C. , … Chen, C. L. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry, 185, 127–133. 10.1192/bjp.185.2.127 [DOI] [PubMed] [Google Scholar]
- Cleary, M. , Kornhaber, R. , Thapa, D. K. , West, S. , & Visentin, D. (2018). The effectiveness of interventions to improve resilience among health professionals: A systematic review. Nurse Education Today, 71, 247–263. 10.1016/j.nedt.2018.10.002 [DOI] [PubMed] [Google Scholar]
- Fahrenkopf, A. M. , Sectish, T. C. , Barger, L. K. , Sharek, P. J. , Lewin, D. , Chiang, V. W. , … Landrigan, C. P. (2008). Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ, 336(7642), 488–491. 10.1136/bmj.39469.763218.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher, D. , & Sarkar, M. (2013). Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist, 18(1), 12–23. 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- Goel, N. , Basner, M. , Rao, H. , & Dinges, D. F. (2013). Circadian rhythms, sleep deprivation, and human performance. Progress in Molecular Biology and Translational Science, 119, 155–190. 10.1016/B978-0-12-396971-2.00007-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, J. (2020). The Covid‐19 crisis too few are talking about: health care workers’ mental healthitle. Retrieved from https://www.statnews.com/2020/04/03/the-covid-19-crisis-too-few-are-talking-about-health-care-workers-mental-health/
- Gong, Y. , Han, T. , Chen, W. , Dib, H. H. , Yang, G. , Zhuang, R. , … Lu, Z. (2014). Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: A cross‐sectional study. PLoS One, 9(7), 1–7. 10.1371/journal.pone.0103242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulia, P. , Mantas, C. , Dimitroula, D. , Mantis, D. , & Hyphantis, T. (2010). General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infectious Diseases, 10(1), 322. 10.1186/1471-2334-10-322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddadi, P. , & Ali Besharat, M. (2010). Resilience, vulnerability and mental health. Procedia—Social and Behavioral Sciences, 5, 639–642. 10.1016/j.sbspro.2010.07.157 [DOI] [Google Scholar]
- Hershkovich, O. , Gilad, D. , Zimlichman, E. , & Kreiss, Y. (2016). Effective medical leadership in times of emergency: A perspective. Disaster and Military Medicine, 2, 4. 10.1186/s40696-016-0013-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, H. , Matsuishi, K. , Ito, A. , Mouri, K. , Kitamura, N. , Akimoto, K. , … Mita, T. (2010). Factors associated with motivation and hesitation to work among health professionals during a public crisis: A cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health, 10, 672. 10.1186/1471-2458-10-672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. , Cai, Z. , Hu, J. , Wei, N. , … Hu, S. (2020). Factors associated With mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open, 3(3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Q. , Guan, X. , Wu, P. , Wang, X. , Zhou, L. , Tong, Y. , … Feng, Z. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New England Journal of Medicine, 382, 1199–1207. 10.1056/nejmoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, L. , Wan, C. , Ding, R. , Liu, Y. , Chen, J. , Wu, Z. , … Li, C. (2015). Mental distress among Liberian medical staff working at the China Ebola Treatment Unit: A cross sectional study. Health and Quality of Life Outcomes, 13(1), 156. 10.1186/s12955-015-0341-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R. , Hunter, J. , Vincent, L. , Bennett, J. , Peladeau, N. , Leszcz, M. , … Mazzulli, T. (2003). The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Canadian Medical Association Journal, 168(10), 1245–1251. [PMC free article] [PubMed] [Google Scholar]
- NHS under pressure: voices from the frontline of the coronavirus crisis . (n.d.). Retrieved from The Guardian website: https://www.theguardian.com/world/2020/mar/25/nhs-under-pressure-voices-from-the-frontline-of-the-coronavirus-crisis
- Nickell, L. A. , Crighton, E. J. , Tracy, C. S. , Al‐Enazy, H. , Bolaji, Y. , Hanjrah, S. , … Upshur, R. E. G. (2004). Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. Canadian Medical Association Journal, 170(5), 793–798. 10.1503/cmaj.1031077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh, C.‐M. , Kim, H. Y. , Na, H. K. , Cho, K. H. , & Chu, M. K. (2019). The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: A population‐based study. Frontiers in Neurology, 10, 849. 10.3389/fneur.2019.00849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney, M. L. , Griffeth, V. , & Jha, A. K. (2020). Critical supply shortages—The need for ventilators and personal protective equipment during the Covid‐19 pandemic. New England Journal of Medicine, 382, e41. 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- Schalet, B. D. , Pilkonis, P. A. , Yu, L. , Dodds, N. , Johnston, K. L. , Yount, S. , … Cella, D. (2016). Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. Journal of Clinical Epidemiology, 10.1016/j.jclinepi.2015.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. JAMA, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Soehner, A. M. , & Harvey, A. G. (2012). Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: Results from a nationally representative sample. Sleep, 35(10), 1367–1375. 10.5665/sleep.2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Styra, R. , Hawryluck, L. , Robinson, S. , Kasapinovic, S. , Fones, C. , & Gold, W. L. (2008). Impact on health care workers employed in high‐risk areas during the Toronto SARS outbreak. Journal of Psychosomatic Research, 64(2), 177–183. 10.1016/j.jpsychores.2007.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson, L. M. , Arnedt, J. T. , Rosekind, M. R. , Belenky, G. , Balkin, T. J. , & Drake, C. (2011). Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. Journal of Sleep Research, 20(3), 487–494. 10.1111/j.1365-2869.2010.00890.x [DOI] [PubMed] [Google Scholar]
- Tam, C. W. C. , Pang, E. P. F. , Lam, L. C. W. , & Chiu, H. F. K. (2004). Severe acute respiratory syndrome (SARS) in Hongkong in 2003: Stress and psychological impact among frontline healthcare workers. Psychological Medicine, 34(7), 1197–1204. 10.1017/S0033291704002247 [DOI] [PubMed] [Google Scholar]
- The American Association for Public Opinion Research (2016). Standard definitions: Final dispositions of case codes and outcome rates for surveys.
- Ungar, M. , & Theron, L. (2019). Resilience and mental health: How multisystemic processes contribute to positive outcomes. The Lancet Psychiatry, 7(5), 441–448. 10.1016/s2215-0366(19)30434-1 [DOI] [PubMed] [Google Scholar]
- Venegas, C. L. , Nkangu, M. N. , Duffy, M. C. , Fergusson, D. A. , & Spilg, E. G. (2019). Interventions to improve resilience in physicians who have completed training: A systematic review. PLoS One, 14, e0210512. 10.1371/journal.pone.0210512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada, K. , Arimatsu, M. , Yoshikawa, T. , Oda, S. , Taniguchi, H. , Higashi, T. , & Aizawa, Y. (2008). Factors on working conditions and prolonged fatigue among physicians in Japan. International Archives of Occupational and Environmental Health, 82, 59–66. 10.1007/s00420-008-0307-3 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, K. , & Wei, X. (2020). Analysis of psychological and sleep status and exercise rehabilitation of front‐line clinical staff in the fight against COVID‐19 in China. Medical Science Monitor Basic Research, 26, e924085. 10.12659/MSMBR.924085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardeni, M. A. M. , Abebe‐Campino, G. , Bursztyn, B. A. S. , Shamir, B. A. A. , Mekori‐Domachevsky, E. , Toren, A. , & Gothelf, D. (2020). A three‐tier process for screening depression and anxiety among children and adolescents with cancer. Psycho‐Oncology. 10.1002/pon.5494 [DOI] [PubMed] [Google Scholar]
- Zhang, C. , Yang, L. , Liu, S. , Ma, S. , Wang, Y. , Cai, Z. , … Zhang, B. (2020). Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry, 11, 306. 10.3389/fpsyt.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request.


