To the Editor,
Serum prealbumin assessment is a highly valuable and effective strategy for predicting disease progression in critically ill patients, as well as in those affected by chronic disorders and malnutrition. 1 Reliable evidence has also been published that serum prealbumin values are decreased in patients with coronavirus disease 2019 (COVID‐19), and that its measurement may hence be clinically meaningful for early triage of these patients, 2 so that its role in predicting critical illness and unfavorable outcomes deserves deep scrutiny. We, hence, carried out a literature search, for identifying clinical studies that measured serum prealbumin in COVID‐19 patients and correlated the values of this nutritional biomarker with disease severity.
We accessed the three most widely used scientific databases (PubMed, Scopus, and Web of Science), 3 using the keywords “coronavirus disease 2019” OR “COVID‐19” AND “prealbumin” in all fields, with no date or language restrictions. The title, abstract, and full text of all documents identified with these search criteria were carefully analyzed, and those describing serum prealbumin values in COVID‐19 patients with or without severe illness were selected. The reference list was also hand‐searched, with the purpose of identifying other potentially eligible studies. A meta‐analysis was finally performed, with an estimation of weighted mean difference (WMD), along with a 95% confidence interval (95% CI), of prealbumin values in COVID‐19 patients with or without severe disease. When the mean value and SD were not evidently reported, these measures were extrapolated using sample size, median, and range, as proposed by Hozo et al. 4 A random‐effect model was applied for adjusting the possible heterogeneity arising across the different studies. Heterogeneity was assessed using χ 2 test and I 2 statistics. The statistical analysis was performed using MetaXL, software Version 5.3 (EpiGear International Pty Ltd, Sunrise Beach, QLD, Australia). The study was carried out in accordance with the declaration of Helsinki and within the terms of the local legislation.
The initial electronic search generated a total number of 14 documents after elimination of replicates, 10 of which were immediately excluded because they did not clearly report serum prealbumin values (n = 5), did not stratify serum prealbumin values in COVID‐19 patients with different illness severity (n = 3), and the endpoint was not clearly defined (n = 1), while the remaining document ought to be excluded as it could not be found in the journal website. Another eligible study was identified from the reference list, so that our final analysis included five studies, 5 , 6 , 7 , 8 , 9 all cross‐sectional, totaling 1813 COVID‐19 patients, 269 (14.8%) with severe disease (Table 1). All studies were carried out in China, while severe COVID‐19 illness was defined as a respiratory failure in three studies, and prolonged hospitalization or death in the remaining two investigations.
Table 1.
Summary of clinical studies that investigated prealbumin values in coronavirus disease 2019 (COVID‐19) patients with or with severe illness
| Study name | Setting | Study design | Sample size | Age | Females | Endpoint |
|---|---|---|---|---|---|---|
| An et al 5 | China | Cross‐sectional | 47 | 47 ± 5 vs 39 ± 7 | 49% | Prolonged hospitalization |
| Duan et al 6 | China | Cross‐sectional | 348 | 58 ± 15 vs 44 ± 15 | 47% | Respiratory failure |
| Ji et al 7 | China | Cross‐sectional | 102 | N/A | 52% | Respiratory failure |
| Luo et al 8 | China | Cross‐sectional | 1115 | 70 ± 12 vs 59 ± 15 | 49% | Death |
| Wu et al 9 | China | Cross‐sectional | 201 | 47 ± 4 vs 59 ± 5 | 36% | Respiratory failure |
The outcome of single studies and their pooled analysis are shown in Figure 1. In 4 of 5 (80%) studies, serum prealbumin levels were significantly lower in COVID‐19 patients with severe illness, while in the remaining investigation, the concentration did not vary significantly in patients with or without severe disease, defined as prolonged hospitalization (ie, >12 days). In the pooled analysis, the serum prealbumin value in COVID‐19 patients with severe illness appeared significantly lower (WMD, −61.80 mg/L; 95% CI, −98.63 to −24.96 mg/L; I 2, 99%) compared with those with milder disease. The elimination of the study of An et al, 5 which used prolonged hospitalization as an endpoint, amplified this difference (WMD, −77.48 mg/L; 95% CI, −118.17 to −36.78 mg/L; I 2, 99%).
Figure 1.
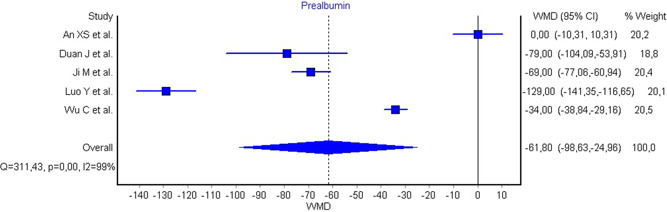
Weighted mean difference (WMD) and 95% confidence interval (95% CI) of antithrombin values in coronavirus disease 2019 (COVID‐19) patients with severe illness compared with those with milder disease
The findings of this meta‐analysis of available scientific literature attest that serum prealbumin values are significantly lower in COVID‐19 patients developing more severe illness. It is also important to report here the findings of another study, which was omitted from our analysis as the serum prealbumin values were unavailable in COVID‐19 patients with or without severe illness. Briefly, Zuo et al 10 prospectively studied 446 COVID‐19 elderly patients, followed‐up during their hospital stay. In a fully adjusted model, COVID‐19 patients in the lowest tertile of serum prealbumin displayed a nearly threefold higher risk of mechanical ventilation (odds ratio, 2.8; 95% CI, 1.2‐6.8), a 25‐fold higher risk of intensive care (odds ratio, 26.4; 95% CI, 4.0‐172.4) and a 19‐fold higher risk of death (odds ratio, 20.1; 95% CI, 3.6‐111.6) compared with those in the highest serum prealbumin tertile.
According to this evidence, we can hence conclude that the progressive decline of serum prealbumin values in COVID‐19 reflects a deteriorated clinical status, and may also be considered an additional contributing and predictive factor for enhancing the risk of developing unfavorable disease progression, up to death. 8
REFERENCES
- 1. Beck FK, Rosenthal TC. Prealbumin: a marker for nutritional evaluation. Am Fam Physician. 2002;65:1575‐1578. [PubMed] [Google Scholar]
- 2.Guo X, Zhang Y, Zeng Y, et al. Serum prealbumin deserves more significance in the early triage of COVID‐19 patients [published online ahead of print July 20, 2020]. Clin Chem Lab Med. 10.1515/cclm-2020-0663 [DOI] [PubMed]
- 3. Lippi G, Favalor EJ, Simundic AM. Biomedical research platforms and their influence on article submissions and journal rankings: an update. Biochem Med (Zagreb). 2012;22(1):7‐14. [PMC free article] [PubMed] [Google Scholar]
- 4. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. An XS, Li XY, Shang FT, et al. Clinical characteristics and blood test results in COVID‐19 patients. Ann Clin Lab Sci. 2020;50(3):299‐307. [PubMed] [Google Scholar]
- 6.Duan J, Wang X, Chi J, et al. Correlation between the variables collected at admission and progression to severe cases during hospitalization among patients with COVID‐19 in Chongqing [published online ahead of print May 29, 2020]. J Med Virol. 10.1002/jmv.26082 [DOI] [PMC free article] [PubMed]
- 7. Ji M, Yuan L, Shen W, et al. Characteristics of disease progress in patients with coronavirus disease 2019 in Wuhan, China. Epidemiol Infect. 2020;148:e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Luo Y, Xue Y, Mao L, et al. Prealbumin as a predictor of prognosis in patients with coronavirus disease 2019. Front Med (Lausanne). 2020;7:374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuo P, Tong S, Yan Q, et al. Decreased prealbumin level is associated with increased risk of mortality in hospitalized elderly patients with COVID‐19 [published online ahead of print 2020]. Nutrition. 10.1016/j.nut.2020.110930 [DOI] [PMC free article] [PubMed]


