The RECOVERY (Randomised Evaluation of COVid‐19 thERapY) trial found that dexamethasone 6 mg once per day for 10 days reduced deaths by one‐third in ventilated patients and by one‐fifth in other patients, receiving oxygen therapy. 1 This equates to the prevention of one death in around eight ventilated patients, or one in around 25 patients requiring oxygen. This welcome news has been considered such an important therapeutic advance that the regimen has been fast‐tracked in the UK even though the study has yet to attain peer review publication.
Although described by the investigators as ‘low dose dexamethasone therapy’ the dose is in effect five‐ to six fold greater than the therapeutic glucocorticoid replacement dose. High doses of glucocorticoids exacerbate hyperglycaemia in people with diabetes, may unmask undiagnosed diabetes and, in those at risk of diabetes, may precipitate hyperglycaemia and new‐onset diabetes (commonly termed ‘steroid‐induced diabetes’). Furthermore, glucocorticoids are the commonest cause of people with diabetes developing potentially life‐threating hyperglycaemic hyperosmolar state (HHS) in hospital. To prevent these harms, the Joint British Diabetes Societies (JBDS) published guidelines on the management of inpatients with and without diabetes receiving steroid therapy. 2 However, these guidelines, which have been adopted in most UK hospitals, may not be appropriate for those with severe COVID‐19 infection receiving dexamethasone, given the additional impact of the disease on glucose metabolism. The ‘cytokine storm’ resulting from severe COVID‐19 infection is associated with significant insulin resistance and reduced insulin production from the pancreatic β cells. This dual pathology can precipitate severe hyperglycaemia, life‐threatening ketoacidosis and HHS in people with diabetes, and even in people without, diabetes. 3 To prevent these harms, the UK National Diabetes COVID‐19 response group published in this journal guidance on the management of COVID‐19‐related hyperglycaemia. 4 However, given the ‘triple insult’ of dexamethasone‐induced impaired glucose metabolism, COVID‐19‐induced insulin resistance and COVID‐19 impaired insulin production, we now provide new guidance specifically for use in people with severe COVID‐19 infection commencing dexamethasone (Figure 1). The aim is to ensure that all patients commenced on dexamethasone, whether or not they have diabetes, receive appropriate glucose surveillance and management of hyperglycaemia should it occur. The guidance informs the clinician of the key facts pertaining to this clinical situation and the reasons why these recommendations differ from the JBDS guidelines. It describes the frequency at which capillary blood glucose monitoring should be undertaken in those with and without diabetes and gives the target ranges of capillary blood glucose levels to aim for.
The guidance recommends giving correction doses of rapid‐acting analogue insulin when capillary blood glucose > 12.0 mmol/l, with the dose calculated according to the patient’s weight or in those already treated with insulin, on their total daily insulin dose. The correction doses recommended are notably higher than those used in our previous hyperglycaemia guideline given the inevitable increase in insulin resistance. Unlike the previous guidance, we do not recommend using the insulin correction ratios that some people with type 1 diabetes usually use as these may not be appropriate given the significant disturbance of glucose metabolism.
To maintain glycaemic control we recommend using NPH insulin which has an intermediate duration of action in preference to longer‐acting insulin even though the metabolic effects of dexamethasone can persist for up to 36 h. NPH insulin given twice daily allows more flexibility in dose adjustment. The starting doses based on weight are slightly greater than those given in our previous guidance but as before, a reduced dose should be used in the frail, elderly and those with an eGFR of < 30 ml/min. If the patient is already on a long‐acting insulin or twice daily pre‐mix insulin then it is recommended this be increased by 20%, but it is noted that this may actually require rapid escalation by 40% or more. 5 Insulin resistance will fall when dexamethasone is stopped and so capillary blood glucose and insulin dose adjustment need careful monitoring to avoid hypoglycaemia. The guidance table for the NPH and long‐acting insulin assists in dose escalation and down titration of these insulins.
Finally, close initial follow‐up is advised for those with known diabetes and a yearly HbA1c measurement is recommended for those with steroid‐induced hyperglycaemia because this group have been shown to be at increased risk of developing diabetes at a later date.
We hope that these guidelines will be helpful for those managing patients with COVID‐19 treated with dexamethasone in the ward setting. Although not intended for critical care units where policies around blood glucose monitoring may differ and where insulin is likely to be given by intravenous infusion, the guidelines may be adapted for use in this setting.
1.
Figure 1.
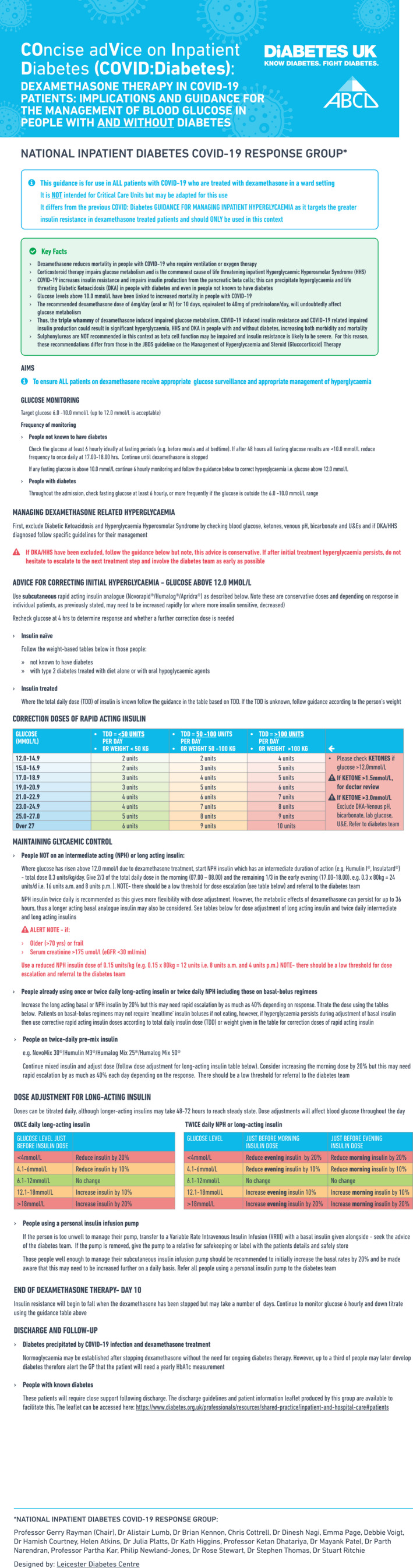
Guidance on glycaemic management for those with COVID‐19 receiving dexamethasone
REFERENCES
- 1. Low‐Cost Dexamethasone Reduces Death by up to One Third in Hospitalised Patients With Severe Respiratory Complications of COVID‐19. Available at https://www.recoverytrial.net/news/low‐cost‐dexamethasone‐reduces‐death‐by‐up‐to‐one‐third‐in‐hospitalised‐patients‐with‐severe‐respiratory‐complications‐of‐covid‐19 Last accessed 6 July 2020. [Google Scholar]
- 2. Roberts A, James J, Dhatariya J. Joint British Diabetes Societies (JBDS) for Inpatient Care. Management of hyperglycaemia and steroid (glucocorticoid) therapy: a guideline from the Joint British Diabetes Societies (JBDS) for Inpatient Care group. Diabet Med. 2018;35:1011‐1017. [DOI] [PubMed] [Google Scholar]
- 3. Bornstein SR, Rubino F, Khunti K et al. Practical recommendations for the management of diabetes in patients with COVID‐19. Lancet Diabetes Endocrinol. 2020;8:546‐550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rayman G, Lumb A, Kennon B et al. New guidance on managing inpatient hyperglycaemia during the COVID‐19 pandemic. Diabet Med. 2020;37:1214‐1216. [DOI] [PubMed] [Google Scholar]
- 5. Dashora UK, Taylor R. Maintaining glycaemic control during high‐dose prednisolone administration for hyperemesis gravidarum in type 1 diabetes. Diabet Med. 2003;21:297‐301. [DOI] [PubMed] [Google Scholar]


