Lombardy was the first and most severely affected Italian region to experience the COVID‐19 pandemic. 1 A strict lockdown was enforced between 8 March and 3 May 2020, during which time public health authorities advised the population to limit their use of hospitals and emergency rooms (ER). Although previous evidence is lacking, patients with mental disorders may be less prone to comply with social distancing and preventive measures enforced during such a lockdown. Unlike the majority of other clinical services, mental health departments were required to continue their activity throughout the outbreak and to limit patients' access to hospitals through alternative outpatient interventions. 2
We used a register‐based, pre/post approach to examine the effectiveness of such efforts, as well as the compliance of patients with mental disorders to the instructions received. We chose the 8 March lockdown as our index event (T0) and compared emergency department visits for mental‐health‐related conditions at the San Paolo University Hospital in Milan, Italy during the lockdown (9 March–3 May 2020) and in the previous 2 months (13 January–8 March; i.e., 8 weeks before and after T0). We determined the percentage variation in the total number of ER visits and across subgroups, based on demographics, main diagnosis at discharge (clustered according to the DSM‐5), and discharge destination (e.g., home, admission to the psychiatry ward). Finally, we used the number of psychiatric emergency visits during the same 16 weeks of the previous year (13 January–3 May 2019) as comparison. This was done to exclude the presence of habitual variations in ER visits during this time of the year that would in case be considered independent from the lockdown. Having clustered ages in three groups (18–29, 30–59, and 60+ years), all variables under study were compared using Pearson's χ2‐test with statistical significance set at P < 0.05. Approval for the purpose of this study was obtained from the hospital management.
Our data revealed a sharp reduction in psychiatric ER visits during lockdown compared to the previous 8 weeks. The total number of visits fell by 43%, from n = 398 pre‐T0 to n = 227 post‐T0 (P < 0.001). In the same period of the previous year, no difference could be observed in the number of ER visits before and after 8 March 2019 (n = 393 between 13 January and 8 March 2019, n = 426 between 9 March and 3 May 2019). This suggests that patients with mental health issues did comply with the request to limit ER use. As shown in Figure 1, however, the most notable drop in ER visits occurred 2 weeks prior to the lockdown, when the Ministry of Health issued recommendations to spontaneously restrict hospital access after the first Italian COVID‐19 cases in Lombardy. A substantial reduction in ER use was maintained throughout the lockdown, although the number of visits increased approximately halfway towards pre‐pandemic levels during the second month. This may reflect several possibilities, including a gradual loosening in patients' tendency to avoid hospitals and the emergence of COVID‐19‐related mental health issues.
Fig. 1.
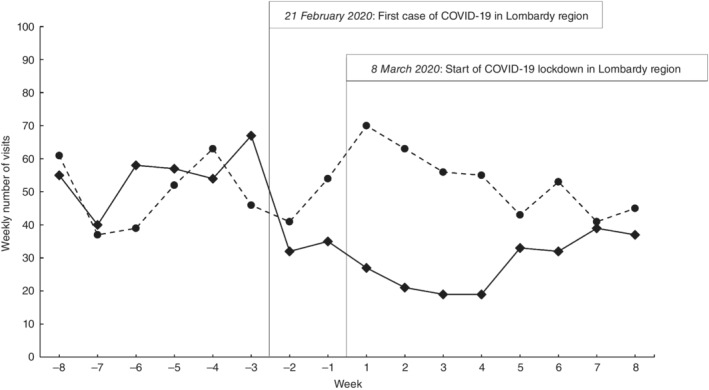
Weekly number of visits to the San Paolo Hospital emergency room (ER) due to a psychiatric condition between 13 January 2020 and 5 March 2020 (from 8 weeks before to 8 weeks after the COVID‐19 lockdown start in Lombardy on 8 March 2020) and in the same time frame of 2019 (13 January–5 March 2019). Before 8 March, the weekly number of visits is comparable in the 2 years of observation (n = 393 in 2019, n = 398 in 2020); after 8 March, the number of ER visits is significantly lower in 2020 compared to 2019 (n = 426 in 2019, n = 227 in 2020; P < 0.001). ( ) 2019. (
) 2019. ( ) 2020.
) 2020.
After dividing ER visits into subgroups based on diagnosis at discharge, some differences may be observed among diagnostic categories. Overall, a significant decrease in ER visits after lockdown was observed for psychotic disorders (−46%, P < 0.001), mood disorders (−58%, P < 0.001), anxiety disorders (−49%, P = 0.011), and ‘other’ conditions (e.g., obsessive–compulsive disorder, neurocognitive disorders; −57%, P < 0.001). In particular, psychotic disorders comprised 21.4% of total ER visits pre‐T0 and 20.3% post‐T0; mood disorders, 16.3% and 11.9%, respectively; and anxiety disorders, 10.3% and 9.3%, respectively. For personality disorders, a statistical trend of decline was observed (−29%, P = 0.066), unlike that for alcohol‐ and substance‐abuse disorders (−27%, P = 0.297) and, most notably, for trauma‐ and stressor‐related disorders (−7%, P = 0.785). Indeed, the relative frequency of these three categories grew from 17.3% to 21.6% for personality disorders, from 6.5% to 8.4% for alcohol‐ and substance‐abuse disorders, and from 7.0% to 11.5% for stressor‐related disorders. Stress‐related disorders reduced by only two cases after lockdown (28 to 26), despite total cases falling by 43%. We interpret this finding as preliminary evidence of an increase in these mental health emergencies related to the COVID‐19 pandemic and lockdown. Personality disorders appear to represent the only group with limited compliance to restrictive measures. This might reflect a lower propensity to observe social norms and low frustration tolerance in the so‐called Cluster B group of patients. Furthermore, the stability of substance‐use disorder diagnoses might be explained by their frequent comorbidity with personality disorders on the one hand, and the possibility of self‐medication attempts to cope with acute stress on the other. No significant differences in the reduction were found between subgroups based on sex (P = 0.102), age group (P = 0.594), or destination upon discharge from ER (P = 0.742).
Our findings should be considered preliminary and interpreted with caution due to the following limitations. First, data were collected in a single ER, so they might reflect characteristics of the catchment area rather than a general regional trend. However, our findings are in line with the reduction of hospital admission rates for psychiatric diagnoses reported by another four mental health departments in Lombardy. 3 Second, no information was available on patients with mental health issues who had reached the hospital with an overarching COVID‐19‐related medical problem. Third, the short period of observation might have masked substantial epidemiological phenomena that will be clarified in upcoming months. Indeed, further studies over longer time periods will be necessary to assess the effects of the COVID‐19 pandemic and lockdown on mental health and mental health service use more extensively.
In conclusion, this study shows that: (i) ER visits for mental‐health‐related conditions were successfully reduced during lockdown by almost 50%; (ii) ER visits fell 2 weeks before lockdown, just as the Italian pandemic broke out, and began to rise again during the second month of lockdown; (iii) these variations in the number of ER visits are not observed in the corresponding period of 2019; and (iv) the decrease in ER use involved all diagnostic categories except for personality disorders, alcohol‐ and substance‐abuse disorders, and particularly trauma‐ and stressor‐related disorders.
Disclosure statement
The authors declare that there is no conflict of interest.
References
- 1. De Girolamo G, Cerveri G, Clerici M et al. Mental health in the coronavirus disease 2019 emergency–The Italian response. JAMA Psychiatry 2020. 10.1001/jamapsychiatry.2020.1276 [DOI] [PubMed] [Google Scholar]
- 2. D'Agostino A, Demartini B, Cavallotti S, Gambini O. Mental health services in Italy during the COVID‐19 outbreak. Lancet Psychiatry 2020; 7: 385–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clerici M, Durbano F, Spinogatti F et al. Psychiatric hospitalization rates in Italy before and during COVID‐19: Did they change? An analysis of register data. Ir. J. Psychol. Med. 2020. 10.1017/ipm.2020.29 [DOI] [PMC free article] [PubMed] [Google Scholar]


