Abstract
Influenza and coronavirus disease 2019 (COVID-19) are both contagious respiratory illnesses, but they are caused by different viruses. COVID-19 pandemic is caused by a novel virus - severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Influenza is an infectious respiratory disease, caused by influenza A and influenza B viruses. We describe the three cases of influenza and COVID-19 co-infection.
Keywords: coronavirus, covid-19, influenza, severe acute respiratory syndrome coronavirus 2, sars-cov-2, co-infection, flu, influenza virus type a, influenza virus type b, influenza-like illness
Introduction
Coronavirus disease 2019 (COVID-19) originated in the Huanan South China Seafood Market in Wuhan. It has posed a global health threat. COVID-19 can present with a spectrum of clinical manifestations including fever, myalgia, cough, dyspnea, and less frequently headache, diarrhea, nausea, and vomiting. Although respiratory symptoms predominate, multiple organ dysfunction may also occur with COVID-19. Coagulopathy has been found as a prominent feature of COVID-19 and severe coagulation dysfunction may be associated with poor prognosis [1-3]. Neurological and cardiovascular complications are also common in COVID-19 patients. No effective treatment has yet been established.
Case presentation
The mean age was 59.6 years (range 47-71 years) and 2/3 were female. Two were Hispanic and one was Pilipino. Comorbidities included hypertension and diabetes mellitus. COVID-19 was diagnosed by nasopharyngeal swab reverse-transcription polymerase chain reaction (RT-PCR) and influenza by rapid antigen assay. Two patients had influenza type B and one had influenza type A. The presenting sign and symptoms were cough, fever, shortness of breath and myalgia. Chest X-ray (CXR) and computed tomography (CT) of the case 1 and case 2 are shown in Figure 1A-1D.
Figure 1. (A) CXR of case 1 showing bilateral patchy infiltrates. (B) CT chest of case 1 showing diffuse scattered areas of ground-glass and mixed attenuating opacities. (C) CXR of case 2 showing multi-lobar infiltrates. (D) CT chest of case 2 showing diffuse bilateral ground-glass infiltrates.
CXR: Chest X-ray
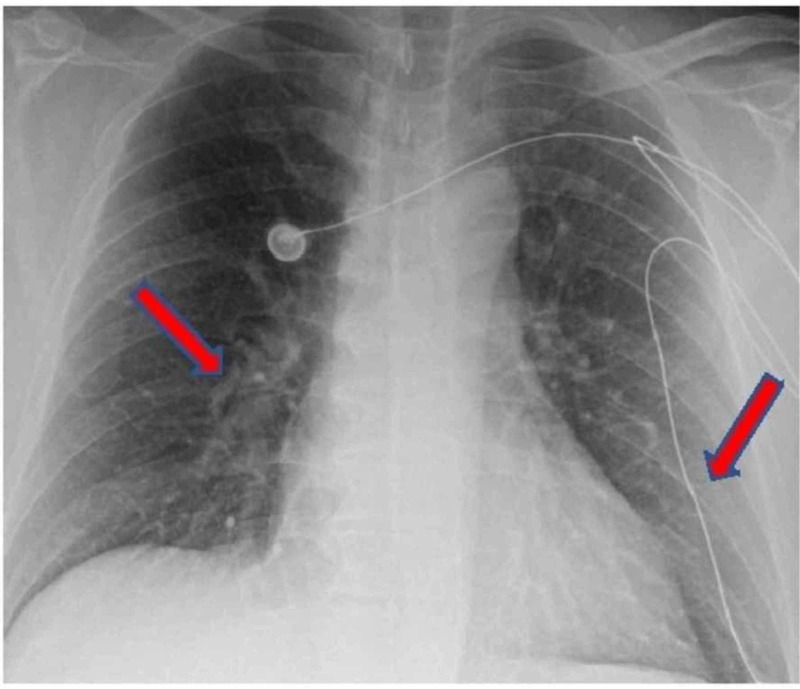
CXR of the case 3 is shown in Figure 2.
Figure 2. CXR of case 3 showing bilateral patchy infiltrates.
CXR: Chest X-ray
One patient (case 2) had positive blood culture for Enterococcus faecium. Two patients required intubation during their hospital course. Inflammatory markers (ESR, CRP, IL-6) were elevated in the patients. All three patients were treated with hydroxychloroquine, azithromycin, ceftriaxone for COVID-19 and Oseltamivir for influenza. All were discharged in stable condition. Table 1 summarizes the clinical characteristics of the three patients.
Table 1. Summarizes the clinical characteristics and outcome of the three patients.
Reference ranges are as follows: white blood cells 4.5-11 K/mm3, hemoglobin 12-16 g/dl, platelets 140-440 K/mm3, creatine kinase 30-223 unit/L, troponin less than 0.03 ng/ml, sodium 135-145 meq/L, potassium 3.5-5 meq/L, chloride 98-107 meq/L, HCO3 21-31 meq/L, BUN 7-23 mg/dl, creatinine 0.6-1.30 mg/dl, aspartate transaminase 13-39 U/L, alanine transaminase 7-52 U/L, ESR 0-32 mm/hr, CRP less than 10 mg/L, IL-6 0-15.5 pg/ml, fibrinogen 183-503 mg/dl, ferritin 12-300 ng/ml.
DM: diabetes mellitus; HTN: hypertension; SOB: shortness of breath; RT-PCR: reverse-transcription polymerase chain reaction; ND: not done; HCO3: bicarbonate; BUN: blood urea nitrogen; CK: creatine kinase; AST: aspartate transaminase; ALT: alanine transaminase; ESR: erythrocyte sedimentation rate; CRP: c-reactive protein; IL-6: Interleukin-6.
| Variables | Case 1 | Case 2 | Case 3 |
| Age | 47 | 71 | 61 |
| Sex | Male | Female | Female |
| Race | Pilipino | Hispanic | Hispanic |
| Medical history | DM | None | DM, HTN |
| Smoking history | Unknown | Negative | Former |
| Presenting complaints | Cough, fever | Fever, cough, SOB | SOB, myalgia |
| Vital signs on presentation: Blood pressure mm Hg / heart rate per minute / temperature degree Celsius / respiratory rate per minute / saturation percent on room air | 109-65/88/38/18/98% | 196-97/105/35.8 24/83% | 175-106/131 37.1/18/94 |
| COVID-19 diagnostic test | RT-PCR | RT-PCR | RT-PCR |
| Influenza diagnostic test / type | Antigen detection assay/ B | Antigen detection assay/ B | Antigen detection assay/ A |
| Chest X-ray | Bilateral patchy infiltrates | Multi-lobar infiltrates | Bilateral patchy infiltrates |
| Chest computed tomography | Diffuse scattered areas of ground-glass and mixed attenuating opacities | Diffuse bilateral ground-glass infiltrates | ND |
| Blood culture / organism | Negative | Enterococcus faecium | Negative |
| White blood cells on presentation- K/mm3 | 4.4 | 15.5 | 11.5 |
| Hemoglobin- g/dl | 15.1 | 14.4 | 13.7 |
| Platelets- K/mm3 | 199 | 246 | 266 |
| Creatine Kinase total- unit/L | ND | 58 | 343 |
| Troponin- ng/ml | ND | 0.04 | 0.01 |
| Sodium- meq/L | 135 | 141 | 136 |
| Potassium- meq/L | 3.9 | 3.6 | 3.9 |
| Chloride- meq/L | 102 | 103 | 103 |
| HCO3- meq/L | 23 | 24 | 22 |
| BUN- mg/dl | 11 | 21 | 11 |
| Creatine- mg/dl | 1.23 | 0.65 | 0.75 |
| AST/ALT-U/L | 31/30 | 20/15 | 81/55 |
| ESR- mm/hr | 43 | 38 | 67 |
| CRP- mg/L | 45.8 | 144.5 | 203.2 |
| IL-6- pg/ml | 62.1 | 155.2 | 51 |
| Fibrinogen- mg/dl | ND | 546 | ND |
| Ferritin- ng/ml | ND | 270 | 76 |
| Treatment for COVID-19 | Hydroxychloroquine, azithromycin and ceftriaxone | Hydroxychloroquine, azithromycin, ceftriaxone, tocilizumab convalescent plasma | Hydroxychloroquine, azithromycin ceftriaxone |
| Treatment for influenza | Oseltamivir | Oseltamivir | Oseltamivir |
| Intubation | Yes | Yes | No |
| Outcome | Discharged | Discharged | Discharged |
Discussion
In a metanalysis study, 3% of patients hospitalized with COVID-19 were also co-infected with another respiratory virus; respiratory syncytial virus (RSV) and influenza A being the most common viral pathogens identified [4]. Table 2 summarizes salient differences between the two viruses [4-7].
Table 2. Summarizes salient differences between the two viruses.
| Influenza | COVID-19 | |
| Virus characteristics | Influenza viruses are negative-sense single-strand RNA viruses with a segmented genome | Coronaviruses are positive-sense single-stranded, RNA viruses with an unsegmented, genome |
| Incubation period | 1 to 4 days (average 2 days) | Generally, within 14 days following exposure, with most cases occurring approximately four to five days after exposure |
| Transmission | Respiratory droplets and contact | Respiratory droplets and contact |
| Diagnostic tests | Antigen detection assays reverse-transcription polymerase chain reaction (RT-PCR), multiplex PCR, and rapid molecular assays | Nucleic acid amplification testing (NAAT) most commonly with RT-PCR assay |
| Chest X-ray | Bilateral reticular or reticulonodular opacities with or without superimposed consolidation | Consolidation and ground glass opacities |
| Signs and symptoms | Fever, headache, myalgia, malaise, cough, sore throat, and nasal discharge. Gastrointestinal illness, such as vomiting and diarrhea, is usually not part of influenza infections in adults but can occur in 10 to 20 percent of influenza infections in children. | Fever, cough, dyspnea, nasal discharge, myalgias. However, diarrhea and smell or taste disorders, are also common. Other manifestations include conjunctivitis and dermatologic manifestations - maculopapular, urticarial, and vesicular eruptions and transient livedo reticularis |
| Laboratory abnormalities | Leukocyte counts are normal or low early in the illness but may become elevated later in the illness | Lymphopenia, elevated aminotransaminase levels, elevated lactate dehydrogenase levels, elevated inflammatory markers (e.g., ferritin, C-reactive protein, and erythrocyte sedimentation rate), and abnormalities in coagulation tests. |
| Treatment | FDA-approved antiviral drugs | Optimal approach to treatment of COVID-19 is uncertain. Preliminary evidence suggests role for antiviral agent - remdesivir and dexamethasone in the management of COVID-19 |
| Vaccine | FDA-licensed influenza vaccines produced annually | Currently there is no vaccine to prevent COVID-19, clinical trials available |
| Complications | Acute respiratory distress syndrome (ARDS), myositis, rhabdomyolysis, acute myocardial infarction, myocarditis and pericarditis, toxic-shock syndrome, Guillain–Barre syndrome, transverse myelitis, encephalopathy | Acute respiratory distress syndrome (ARDS), myocarditis, heart failure, acute coronary syndrome, arrhythmias, cardiogenic shock, thromboembolic complications (pulmonary embolism, acute limb ischemia, mesenteric thrombosis, acute stroke), multisystem inflammatory syndrome and Guillain–Barre syndrome. |
| Bacterial co-infection in intensive care unit (ICU) patients | More prevalent (19% of cases) | Less prevalent (14% of cases) |
| Most commonly detected bacterial pathogen | Streptococcus pneumoniae, Staphylococcus aureus, Streptococcus pyogenes | Mycoplasma pneumoniae, Pseudomonas aeruginosa, Hemophilus influenzae, Klebsiella pneumoniae |
Conclusions
In conclusion, we report three cases of co-infection of influenza and COVID-19. Health care providers should be aware of this unique situation as both can present with similar symptoms but vary in treatment. Clinicians should have a high index of suspicion in the appropriate clinical scenario. Further studies are needed to determine whether patients who have a concurrent viral infection have a worse prognosis than those in whom SARS-CoV-2 is the only detected pathogen.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Acute upper limb ischemia in a patient with COVID-19 (PREPRINT) Kaur P, Qaqa F, Ramahi A, et al. Hematol Oncol Stem Cell Ther. 2020 doi: 10.1016/j.hemonc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 presenting as acute limb ischaemia. Kaur P, Posimreddy S, Singh B, Qaqa F, Habib HA, Maroules M, Shamoon F. Eur J Case Rep Intern Med. 2020;7:1724. doi: 10.12890/2020_001724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covid-19 presenting as acute limb ischemia. Singh B, Kaur P, Ajdir N, Gupta S, Maroules M. Cureus. 2020;22:9344. doi: 10.7759/cureus.9344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Co-infections in people with COVID-19: a systematic review and meta-analysis. Lansbury L, Lim B, Baskaran V, Lim WS. J Infect. 2020;81:266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Influenza. Krammer F, Smith GJD, Fouchier RAM, et al. Nat Rev Dis Primers. 2018;4:3. doi: 10.1038/s41572-018-0002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neurological manifestations and complications of COVID-19: a literature review. Ahmad I, Rathore FA. J Clin Neurosci. 2020;77:8–12. doi: 10.1016/j.jocn.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. Bikdeli B, Madhavan MV, Jimenez D, et al. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]