Abstract
Background
Stroke is a leading cause of morbidity and mortality worldwide. Antiplatelet agents are considered to be the cornerstone for secondary prevention of stroke, but the role of using multiple antiplatelet agents early after stroke or transient ischaemic attack (TIA) to improve outcomes has not been established.
Objectives
To determine the effectiveness and safety of initiating, within 72 hours after an ischaemic stroke or TIA, multiple antiplatelet agents versus fewer antiplatelet agents to prevent stroke recurrence. The analysis explores the evidence for different drug combinations.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched 6 July 2020), the Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 7 of 12, 2020) (last searched 6 July 2020), MEDLINE Ovid (from 1946 to 6 July 2020), Embase (1980 to 6 July 2020), ClinicalTrials.gov, and the WHO ICTRP. We also searched the reference lists of identified studies and reviews and used the Science Citation Index Cited Reference search for forward tracking of included studies.
Selection criteria
We selected all randomised controlled trials (RCTs) that compared the use of multiple versus fewer antiplatelet agents initiated within 72 hours after stroke or TIA.
Data collection and analysis
We extracted data from eligible studies for the primary outcomes of stroke recurrence and vascular death, and secondary outcomes of myocardial infarction; composite outcome of stroke, myocardial infarction, and vascular death; intracranial haemorrhage; extracranial haemorrhage; ischaemic stroke; death from all causes; and haemorrhagic stroke. We computed an estimate of treatment effect and performed a test for heterogeneity between trials. We analysed data on an intention‐to‐treat basis and assessed bias for all studies. We rated the certainty of the evidence using the GRADE approach.
Main results
We included 15 RCTs with a total of 17,091 participants. Compared with fewer antiplatelet agents, multiple antiplatelet agents were associated with a significantly lower risk of stroke recurrence (5.78% versus 7.84%, risk ratio (RR) 0.73, 95% confidence interval (CI) 0.66 to 0.82; P < 0.001; moderate‐certainty evidence) with no significant difference in vascular death (0.60% versus 0.66%, RR 0.98, 95% CI 0.66 to 1.45; P = 0.94; moderate‐certainty evidence). There was a higher risk of intracranial haemorrhage (0.42% versus 0.21%, RR 1.92, 95% CI 1.05 to 3.50; P = 0.03; low‐certainty evidence) and extracranial haemorrhage (6.38% versus 2.81%, RR 2.25, 95% CI 1.88 to 2.70; P < 0.001; high‐certainty evidence) with multiple antiplatelet agents. On secondary analysis of dual versus single antiplatelet agent therapy, benefit for stroke recurrence (5.73% versus 8.06%, RR 0.71, 95% CI 0.62 to 0.80; P < 0.001; moderate‐certainty evidence) was maintained as well as risk of extracranial haemorrhage (1.24% versus 0.40%, RR 3.08, 95% CI 1.74 to 5.46; P < 0.001; high‐certainty evidence). The composite outcome of stroke, myocardial infarction, and vascular death (6.37% versus 8.77%, RR 0.72, 95% CI 0.64 to 0.82; P < 0.001; moderate‐certainty evidence) and ischaemic stroke (6.30% versus 8.94%, RR 0.70, 95% CI 0.61 to 0.81; P < 0.001; high‐certainty evidence) were significantly in favour of dual antiplatelet therapy, whilst the risk of intracranial haemorrhage became less significant (0.34% versus 0.21%, RR 1.53, 95% CI 0.76 to 3.06; P = 0.23; low‐certainty evidence).
Authors' conclusions
Multiple antiplatelet agents are more effective in reducing stroke recurrence but increase the risk of haemorrhage compared to one antiplatelet agent. The benefit in reduction of stroke recurrence seems to outweigh the harm for dual antiplatelet agents initiated in the acute setting and continued for one month. Further studies are required in different populations to establish comprehensive safety profiles and long‐term outcomes to establish duration of therapy.
Plain language summary
Use of multiple versus fewer antiplatelet drugs for preventing early recurrence after stroke or transient ischaemic attack
Review question
Are multiple antiplatelet drugs better than fewer antiplatelet drugs for preventing early recurrence after stroke?
Background
Stroke is the second most common non‐communicable disease in the world, and carries a high risk of recurrence. Most recurrences occur early after stroke, and effective treatments are needed to prevent recurrence. Current guidelines recommend the use of an antiplatelet drug like aspirin after a stroke or transient ischaemic attack (mini‐stroke). However, the safety and benefit of using more than one antiplatelet drug early after stroke has not been clearly established.
Study characteristics
We compared the use of multiple versus fewer antiplatelet drugs early after stroke. The evidence is current to 6 July 2020. We included 15 clinical trials with a total of 17,091 participants from a range of Asian, European and North American populations. The most common antiplatelet combinations tested were aspirin and dipyridamole, and aspirin and clopidogrel.
Key results
We found that multiple antiplatelet drugs reduced the risk of stroke recurrence but increased the risk of bleeding compared with fewer antiplatelet drugs. Two antiplatelet drugs appear to be more effective in preventing early stroke recurrence than a single antiplatelet drug, but there is an increased risk of side effects, especially bleeding. The benefits of dual antiplatelet drugs started immediately after a stroke seems to outweigh the risks for the first month.
Certainty of the evidence
The certainty of evidence was generally moderate or high.
Summary of findings
Summary of findings 1. Multiple compared to fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Multiple compared to fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or TIA | |||||
| Patient or population: preventing early recurrence after ischaemic stroke or TIA Setting: inpatient and outpatient Intervention: multiple antiplatelet agents Comparison: fewer antiplatelet agents | |||||
| Outcomes at ≥ 3 months | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or TIA | Risk difference with multiple agents | ||||
| Stroke | Study population | RR 0.73 (0.66 to 0.82) | 16,707 (14 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 78 per 1000 | 21 fewer per 1000 (27 fewer to 14 fewer) | ||||
| Vascular death | Study population | RR 0.98 (0.67 to 1.45) | 15,901 (11 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 7 per 1000 | 0 fewer per 1000 (2 fewer to 3 more) | ||||
| Myocardial infarction | Study population | RR 1.38 (0.63 to 2.99) | 11,411 (3 RCTs) | ⊕⊕⊕⊕ High | |
| 2 per 1000 | 1 more per 1000 (1 fewer to 4 more) | ||||
| Stroke, myocardial infarction, or vascular death | Study population | RR 0.72 (0.64 to 0.82) | 12,932 (7 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 88 per 1000 | 25 fewer per 1000 (32 fewer to 16 fewer) | ||||
| Intracranial haemorrhage | Study population | RR 1.92 (1.05 to 3.50) | 14,287 (6 RCTs) | ⊕⊕⊝⊝ Lowa,b,c,d,e | |
| 2 per 1000 | 2 more per 1000 (0 fewer to 5 more) | ||||
| Extracranial haemorrhage | Study population | RR 2.14 (1.79 to 2.57) | 10,658 (7 RCTs) | ⊕⊕⊕⊕ High | |
| 29 per 1000 | 36 more per 1000 (25 more to 48 more) | ||||
| Ischaemic stroke | Study population | RR 0.73 (0.64 to 0.83) | 13,121 (3 RCTs) | ⊕⊕⊕⊕ High | |
| 76 per 1000 | 21 fewer per 1000 (27 fewer to 13 fewer) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio; TIA: transient ischaemic attack | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aWe found overall risk to be high in De Martiis and Petrovska‐Cvetkovska 2008, in which information regarding controlling for bias was mostly not available. The most common source of bias was performance bias, which was not controlled for in 6 of the 14 included studies (Chairangsarit 2005; EARLY‐trial; ESPIRIT; De Martiis; Nakamura 2010; Petrovska‐Cvetkovska 2008). This was due to unblinding of participants when they did not receive placebos for the additional antiplatelet agent that the intervention group received. bPerformance bias was the most frequently encountered bias due to unblinding of study participants. However, detection bias was often controlled for even when participants were not blinded. cOnly Chairangsarit 2005 was at high risk of attrition bias. This study reported 11 of 38 participants (28.9%) lost to follow‐up. It was unclear in Petrovska‐Cvetkovska 2008, which did not report participants lost to follow‐up. Both of these were two of only five studies that reported intracranial haemorrhage. dOnly Petrovska‐Cvetkovska 2008 was at unclear risk of reporting bias, as information regarding all expected outcomes was not available. eWe found two studies (De Martiis and Petrovska‐Cvetkovska 2008) where no information was available regarding sequence generation as at unclear risk of selection bias.
Summary of findings 2. Dual compared to one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Dual compared to one antiplatelet agent for preventing early recurrence after ischaemic stroke or TIA | |||||
| Patient or population: preventing early recurrence after ischaemic stroke or TIA Setting: inpatient and outpatient Intervention: dual antiplatelet agents Comparison: one antiplatelet agent | |||||
| Outcomes at ≥ 3 months | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with 1 antiplatelet agent for preventing early recurrence after ischaemic stroke or TIA | Risk difference with dual agents | ||||
| Stroke | Study population | RR 0.71 (0.62 to 0.80) | 13,637 (13 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 81 per 1000 | 23 fewer per 1000 (31 fewer to 16 fewer) | ||||
| Vascular death | Study population | RR 0.84 (0.54 to 1.30) | 12,831 (10 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 7 per 1000 | 1 fewer per 1000 (3 fewer to 2 more) | ||||
| Myocardial infarction | Study population | RR 1.38 (0.63 to 2.99) | 11,411 (3 RCTs) | ⊕⊕⊕⊕ High | |
| 2 per 1000 | 1 more per 1000 (1 fewer to 4 more) | ||||
| Stroke, myocardial infarction, or vascular death | Study population | RR 0.72 (0.64 to 0.82) | 12,932 (7 RCTs) | ⊕⊕⊕⊝ Moderatea,b,c,d,e | |
| 88 per 1000 | 25 fewer per 1000 (32 fewer to 16 fewer) | ||||
| Intracranial haemorrhage | Study population | RR 1.53 (0.76 to 3.06) | 11,217 (5 RCTs) | ⊕⊕⊝⊝ Lowa,b,c,d,e | |
| 1 per 1000 | 1 more per 1000 (0 fewer to 3 more) | ||||
| Extracranial haemorrhage | Study population | RR 3.08 (1.74 to 5.46) | 7586 (6 RCTs) | ⊕⊕⊕⊕ High | |
| 456 per 1000 | 948 more per 1000 (337 more to 2032 more) | ||||
| Ischaemic stroke | Study population | RR 0.70 (0.61 to 0.81) | 10,051 (2 RCTs) | ⊕⊕⊕⊕ High | |
| 89 per 1000 | 27 fewer per 1000 (35 fewer to 17 fewer) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio; TIA: transient ischaemic attack | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aWe found overall risk to be high in De Martiis and Petrovska‐Cvetkovska 2008, in which information regarding controlling for bias was not available. The most common source of bias was performance bias, which was not controlled for in 6 of the 14 included studies (Chairangsarit 2005; EARLY‐trial; ESPIRIT; De Martiis; Nakamura 2010; Petrovska‐Cvetkovska 2008). This was due to unblinding of participants when they did not receive placebos for the additional antiplatelet agent that the intervention group received. bPerformance bias was the most frequently encountered bias due to unblinding of study participants. However, detection bias was often controlled even when participants were not blinded. cOnly Chairangsarit 2005 was at high risk of attrition bias. This study reported 11 of 38 participants (28.9%) lost to follow‐up. It was unclear in Petrovska‐Cvetkovska 2008, which did not report participants lost to follow‐up. Both of these were two of only five studies that reported intracranial haemorrhage. dOnly Petrovska‐Cvetkovska 2008 was at unclear risk of reporting bias, as complete information regarding all expected outcomes was not available. eWe found two studies (De Martiis and Petrovska‐Cvetkovska 2008) where no information was available regarding sequence generation as at unclear risk of selection bias.
Background
Description of the condition
Over one million new strokes are reported each year in high‐income countries (Bamford 1990), whilst the low‐income countries sustain twice that incidence (Lopez 2006). About 30% of these strokes are recurrent events (Goldstein 2006). Transient ischaemic attacks (TIAs) and minor ischaemic strokes are often precursors to serious vascular events including recurrent strokes, the risk being at its maximum within the first 48 hours of the onset (Coull 2004).
Antiplatelet agents, especially aspirin as a single agent, have been shown to reduce the risk of early recurrent ischaemic stroke by 7 per 1000 people treated and improve the long‐term functional outcome, with 13 more people alive and independent per 1000 people treated. However, this is accompanied by a minimal increase in the risk of haemorrhage (2 per 1000 people). The International Stroke Trial and the Chinese Acute Stroke Trial both document the effective role of aspirin in acute stroke treatment as early as within 48 hours of onset (Chen 2000).
Recent studies have used multiple antiplatelet agents in addition to aspirin in the acute phase of stroke, based on the assumption that the additional platelet blockade will translate into superior clinical outcomes compared with a single antiplatelet agent or less intensive antiplatelet therapy for a typical duration of at least three months, or occasionally less (CHANCE; COMPRESS; FASTER PILOT; POINT; TARDIS).
Use of multiple antiplatelet therapy may be effective in the setting of acute ischaemic stroke or TIA, by minimising clinical disability associated with tissue injury along with reducing the risk of recurrence of serious vascular events. In terms of the safety profile, long‐term multiple therapy may be harmful compared with single antiplatelet therapy. A meta‐analysis is needed to determine whether multiple antiplatelet agents are indeed more effective than fewer antiplatelet agents in preventing early recurrence of stroke or TIA and, if so, to determine its safety profile as well as duration of treatment.
Description of the intervention
The included antiplatelet agents are given alone or in combination with other antiplatelet agents, and work via different mechanisms to prevent platelet aggregation (Born 2006).
At antiplatelet doses of 75 to 325 mg/day, aspirin irreversibly inhibits the platelet cyclooxygenase (COX)‐1 dependent thromboxane A2 formation that is responsible for platelet aggregation (Patrono 1994).
Dipyrimadole inhibits the activity of adenosine deaminase and phosphodiesterase, which leads to an accumulation of adenosine, adenine nucleotide, and cyclic adenosine monophosphate (cAMP). These mediators inhibit platelet aggregation and may cause vasodilatation via release of prostacyclin or prostaglandin D2 (PGD2) (d'Esterre 2010).
A combination drug consisting of two antiplatelet agents (aspirin and extended‐release dipyridamole) has been found to be more effective than aspirin alone. Like aspirin it increases plasma endothelial nitric acid oxidase (eNOS), thus preventing platelet aggregation, and also reduces oxidised low‐density lipoproteins (oxLDLs), but for a longer duration than with aspirin alone (Serebruany 2010).
Clopidogrel, a new thienopyridine derivative similar to ticlopidine, requires in vivo biotransformation to an unidentified active metabolite. This active metabolite irreversibly blocks the P2Y12 component of adenosine diphosphate (ADP) receptors, thus preventing activation of the glycoprotein (GP) IIb/IIIa receptor complex and reducing platelet aggregation. Platelets blocked by clopidogrel are affected for the remainder of their life span (D'Sa 1999).
Cilostazol increases the cAMP levels in platelets via inhibition of cyclic AMP phosphodiesterase 3 (PGE3) (Minami 1997). It also inhibits the uptake of adenosine. This leads to its dual action of reversible inhibition of platelet aggregation along with vasodilatation and inhibition of vascular smooth muscle cell proliferation.
How the intervention might work
Antiplatelet combination therapy may work better than using a single antiplatelet agent. Given together, different agents with different modes of action and variable onset of action may work synergistically, thus inhibiting platelets more effectively and with a faster onset of action. There has been growing evidence that combination antiplatelet therapy also reduces the micro‐emboli in the brain in acute ischaemic stroke. The Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial found a relative risk reduction of 39.8% (95% confidence interval (CI) 13.8 to 58.0, P = 0.0046) in micro‐embolic signals on transcranial Doppler ultrasound (TCD) amongst participants on dual therapy compared with aspirin monotherapy (Markus 2005). Another study showed similar results, with a relative risk reduction of 42.4% (95% CI 4.6 to 65.2, P = 0.025), on combination therapy with aspirin and clopidogrel (Wong 2010).
Why it is important to do this review
The early management of people with an acute cerebral ischaemic event (stroke or TIA) may have a substantial impact on clinical outcomes. The non‐randomised EXPRESS study compared multifaceted and very early intervention with standard care and suggested this was associated with an 80% reduction in the 90‐day risk of stroke recurrence. However, it was not possible to adjust fully for confounding factors, and it was not clear which components of the intervention accounted for the effects observed.
Objectives
To determine the effectiveness and safety of initiating, within 72 hours after an ischaemic stroke or TIA, multiple antiplatelet agents versus fewer antiplatelet agents to prevent stroke recurrence. The analysis explores the evidence for different drug combinations.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) where participants took any combination of antiplatelet agents, starting within 72 hours of an acute ischaemic stroke or TIA, versus fewer agents, and who were systematically followed up for development of stroke or TIA for a minimum of one month on the treatment.
Types of participants
We included participants with clinical manifestations of an acute ischaemic stroke or TIA who were given the intervention within 72 hours of onset and continued therapy for at least one month after diagnosis. We excluded any trials that included participants previously administered anticoagulants, including heparin, heparinoids, or direct thrombin inhibitors, for any duration.
Types of interventions
We included trials of combinations of orally administered antiplatelet agents, which may include but were not limited to aspirin, thienopyridine derivatives, dipyridamole, cilostazol, triflusal, buflomedil, and sarpogrelate. We excluded data from any treatment arm in which the intervention was aspirin at a dose of less than 30 mg daily.
We addressed multiple versus fewer agent combinations. The comparisons based on the intervention versus control arms in the included trials were as follows.
A + B versus A or B (multiple versus single agent)
A + B + C versus C or A + B (multiple versus fewer agents)
Types of outcome measures
Primary outcomes
The primary outcome measure was stroke (of any type including fatal stroke) or vascular death during follow‐up of at least three months after initiation of therapy.
Secondary outcomes
We assessed the secondary outcomes at the final scheduled follow‐up of at least 90 days after initiation of therapy. These included components of the composite outcome (stroke, myocardial infarction (MI), or vascular death) as well as the composite outcome of stroke, MI or vascular death.
MI (non‐fatal or fatal)
Stroke, MI, or vascular death during the follow‐up period
Intracranial haemorrhage (fatal or non‐fatal)
Extracranial haemorrhage (fatal or non‐fatal)
Stroke (ischaemic or haemorrhagic, fatal or non‐fatal)
Death from any cause
For studies where there was more than one follow‐up period, we included outcome data according to follow‐up at one week, one month, three months, and six months, as available. Otherwise, we included the longest period recorded to extract outcome data (at least 90 days).
Search methods for identification of studies
See the 'Specialized register' information at the Cochrane Stroke Group's website. We searched for relevant trials in all languages and arranged translation of trial reports where necessary.
Electronic searches
We searched the Cochrane Stroke Group Trials Register (last searched 6 July 2020), the Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 7 of 12, July 2020) (last searched 6 July 2020) (Appendix 1), MEDLINE Ovid (1946 to 6 July 2020) (Appendix 2), and Embase Ovid (1980 to 6 July 2020) (Appendix 3).
We developed the MEDLINE search strategy with the help of the Cochrane Stroke Group Trials Information Specialist and adapted it for the other databases.
In an effort to identify further published, unpublished, and ongoing trials, we searched the ongoing trials registers.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 6 July 2020) (Appendix 4)
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch; searched 6 July 2020) (Appendix 5)
Searching other resources
We also searched the reference lists of identified studies and reviews, and used the Science Citation Index Cited Reference search for forward tracking of included studies.
Data collection and analysis
We reviewed all studies that met our inclusion criteria. These included:
adult men and women, 18 years of age or older;
acute stroke or TIA (onset defined by last seen normal);
given antiplatelet therapy within 72 hours of onset, with control arm participants receiving one or more antiplatelet agents (aspirin at least 30 mg daily if used as the antiplatelet agent);
on antiplatelet therapy for at least one month;
clinical trials with random allocation of participants into two or more treatment groups, including a control group;
information on vascular outcomes (fatal and non‐fatal) during the follow‐up period.
We extracted data from each study on participants enrolled, inclusive of criteria for enrolment; the process of treatment allocation, concealment, and blinding; total number of participants enrolled in the study and assigned to each treatment arm; number of participants lost to follow‐up in each treatment arm; reasons for loss to follow‐up in either treatment arm; method and duration of follow‐up; outcome events measured during follow‐up; and any adverse effects secondary to treatment that were encountered during follow‐up.
We analysed all data using intention‐to‐treat analyses. We rated the certainty of evidence using the GRADE system.
Selection of studies
Three review authors (IAN, AKK, HR) independently screened the titles and abstracts of all reports identified by the searches of electronic bibliographic databases, excluding obviously irrelevant records. We obtained the full texts of the remaining studies and selected trials for inclusion in the review. The review authors were not blinded to the names of authors, institutions, journals, and results when they made the eligibility decision. The senior review author (AKK) acted as arbiter if there was no consensus.
Data extraction and management
We designed a specific questionnaire for data extraction that included information to identify the source of data, eligibility, methods (including sequence generation and allocation), details of participants (e.g. number, age, gender), interventions (i.e. dose and type of antiplatelet agent used), outcomes, and results. Two review authors independently extracted data from each study, resolving any differences through discussion.
Assessment of risk of bias in included studies
We assessed the risk of bias of each included study using Cochrane's 'Risk of bias' tool as described in Chaper 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This tool addresses seven specific domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias. We assigned each domain as at low, high, or an unclear risk of bias based on the information available.
Measures of treatment effect
We used risk ratio (RR) with 95% confidence interval (CI) to measure treatment effects for dichotomous data. We extracted data for randomised participants in each trial as well as outcome event data to calculate pooled RRs.
Unit of analysis issues
For studies where there was more than one follow‐up period, we included outcome data according to follow‐up at one week, one month, three months, and six months, as available, to measure any difference in outcome events over time. Otherwise, we included the longest period recorded to extract outcome data, at least three months. For non‐fatal events, we only recorded the first event for each participant.
Dealing with missing data
We recorded the amount of missing data for outcome variables during data extraction. If this was substantial (i.e. 20% or more), we assumed the missing data showed no benefit from the antiplatelet agent given and performed sensitivity analyses to assess the effect of this assumption on the summary risk ratios.
Assessment of heterogeneity
We assessed the presence of heterogeneity using the I2 statistic, with a value above 50% indicating heterogeneity.
Assessment of reporting biases
We used funnel plots to assess the presence of publication bias.
Data synthesis
We assessed the effect of treatment amongst trials comparing the same combination antiplatelet therapy with one or more antiplatelet agents.
In the absence of significant heterogeneity, we used a fixed‐effect meta‐analysis model for combining data. If we found heterogeneity, we explored it by sensitivity analysis followed by the use of a random‐effects model, if required.
For dichotomous data, we presented results as a summary of RRs with 95% CIs.
Subgroup analysis and investigation of heterogeneity
We assessed the I2 statistic for heterogeneity, which showed less than 50% heterogeneity. We did not perform subgroup analysis as many of our studies were subanalyses of secondary prevention studies, and data regarding subsets were not clearly reported. However, we identified one large trial of one‐month duration. The inclusion of this trial into an exploratory analysis at one month was a change from the protocol of this review.
Sensitivity analysis
We performed sensitivity analyses for studies with substantial missing data of more than 20%. If we included studies with substantial missing data, we analysed data without these studies to assess the robustness of the pooled RRs.
Summary of findings and assessment of the certainty of the evidence
We assessed the certainty of the evidence using the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias), as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), for the following main outcomes of analysis.
Stroke
Vascular death
MI
Stroke, MI, or vascular death
Intracranial haemorrhage
Extracranial haemorrhage
Ischaemic stroke
We created a 'Summary of findings' table in which we presented the key findings of the review, including a summary of the quantity of data, the magnitude of effect size, and the overall certainty of evidence. We also created a second 'Summary of findings' table to compare dual versus single antiplatelet agents, as most of the available trials compared two versus one antiplatelet, and this is a clinically important comparison.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
Our searches identified a total of 287 potentially relevant studies. After duplicates were removed, 226 records were screened using title and abstract after which 161 records were excluded. The remaining 65 records underwent full‐text screening and 50 were excluded. Fifteen trials were included in the review (Figure 1).
1.

Study flow diagram.
Included studies
See Characteristics of included studies.
Fifteen studies met our inclusion criteria and are included in the review (Chairangsarit 2005; CHANCE; CHARISMA; COMPRESS; De Martiis; EARLY‐trial; ESPIRIT; ESPS 2; FASTER PILOT; MATCH 2001; Nakamura 2010; Petrovska‐Cvetkovska 2008; POINT; PRoFESS; TARDIS). The trials enrolled a total of 17,091 participants. In all, 8493 participants were randomised to the intervention group receiving multiple antiplatelets and 8598 participants to the control group. Whilst nine of the 15 studies were conducted in Europe or North America (De Martiis; EARLY‐trial; ESPIRIT; ESPS 2; MATCH 2001; Petrovska‐Cvetkovska 2008; PRoFESS), CHANCE, which accounted for 46% of all participants, was conducted in China.
The most common antiplatelet combinations tested were aspirin and dipyridamole (6 studies: Chairangsarit 2005; De Martiis; EARLY‐trial; ESPIRIT; ESPS 2; PRoFESS) and aspirin and clopidogrel (7 studies: CHANCE; CHARISMA; COMPRESS; FASTER PILOT; MATCH 2001; Petrovska‐Cvetkovska 2008; POINT). One study including three antiplatelet combinations versus aspirin and dipyridamole or clopidogrel met our inclusion criteria (TARDIS). Only Nakamura 2010 tested a combination that included cilostazol (aspirin and cilostazol). Aspirin was usually employed as the control antiplatelet agent (11 studies: Chairangsarit 2005; CHANCE; CHARISMA; COMPRESS; EARLY‐trial; ESPIRIT; ESPS 2; FASTER PILOT; Nakamura 2010; Petrovska‐Cvetkovska 2008; POINT). Other controls included clopidogrel, MATCH 2001; PRoFESS; TARDIS, and dipyridamole, De Martiis; ESPS 2. As per study protocol, all these medications were given orally. Most studies did report a loading dose employed for aspirin, clopidogrel, and dipyridamole, and doses varied slightly in different studies but were within therapeutic range.
The range of follow‐up varied from 30 days to 3.5 years.
All 15 trials reported stroke as an outcome, whilst 11 studies also reported vascular death (Chairangsarit 2005; CHANCE; COMPRESS; EARLY‐trial; ESPIRIT; ESPS 2; FASTER PILOT; Nakamura 2010; Petrovska‐Cvetkovska 2008; POINT; PRoFESS). Secondary outcomes reported included the composite outcome of stroke, MI, and death (8 studies: CHANCE; COMPRESS; EARLY‐trial; ESPIRIT; FASTER PILOT; MATCH 2001; POINT; PRoFESS), intracranial haemorrhage (6 studies: Chairangsarit 2005; CHANCE; COMPRESS; Petrovska‐Cvetkovska 2008; PRoFESS; TARDIS), and extracranial haemorrhage (8 studies: CHARISMA; COMPRESS; EARLY‐trial; ESPIRIT; MATCH 2001; POINT; PRoFESS; TARDIS), being reported most frequently. One study, COMPRESS, followed participants for one month only and could not be included in the analysis of participants followed for at least three months.
Excluded studies
See Characteristics of excluded studies.
We excluded 50 trials after full‐text screening that failed to meet the eligibility criteria. Common reasons for exclusion included comparison of single antiplatelet agents, use of anticoagulants, and failure to randomise within 72 hours of the ischaemic event.
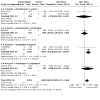
Risk of bias in included studies
See Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Risk of bias was low in most studies. Risk was found to be high in De Martiis and Petrovska‐Cvetkovska 2008, where information regarding controlling for bias was not available. At least nine studies were high‐quality studies where the study design controlled for all possible biases (CHANCE; CHARISMA; COMPRESS; ESPS 2; FASTER PILOT; MATCH 2001; POINT; PRoFESS; TARDIS). The most common source of bias was performance bias, which was not controlled for in six of the 15 included studies (Chairangsarit 2005; De Martiis; EARLY‐trial; ESPIRIT; Nakamura 2010; Petrovska‐Cvetkovska 2008). This was due to unblinding of participants when they did not receive placebos for the additional antiplatelet agent that the intervention group received.
Allocation
Most studies were at low risk of selection bias. Two studies (De Martiis and Petrovska‐Cvetkovska 2008) where no information was available regarding sequence generation were assessed as at unclear risk of bias.
Blinding
Performance bias was the most frequently encountered bias due to the unblinding of study participants. However, detection bias was often controlled even when participants were not blinded.
Incomplete outcome data
Only Chairangsarit 2005 was assessed as at high risk of attrition bias. This study reported 11 of 38 (28.9%) of participants lost to follow‐up. We assessed Petrovska‐Cvetkovska 2008 as at unclear risk of bias, as information regarding all participants was not available, and participants lost to follow‐up were not reported.
Selective reporting
Reporting bias was not obvious, with outcomes reported as planned in the included studies.
Other potential sources of bias
None.
Effects of interventions
The effects of interventions are categorised into primary and secondary outcomes. The results presented were composite numbers from all the included trials. These included a comparison of multiple versus fewer agents, with a secondary analysis of dual‐ versus single‐agent therapy, and are divided into subcategories of actual drug comparisons. There were up to six subcategories based on the included trials, as described in the table below.
|
Intervention (multiple antiplatelet agents) |
Comparison (fewer antiplatelet agents) | ||
| Aspirin | Clopidogrel | Clopidogrel alone or aspirin + dipyridamole | |
| Aspirin + dipyridamole |
Subcategory: aspirin + dipyridamole vs aspirin Chairangsarit 2005; De Martiis; EARLY‐trial; ESPIRIT; ESPS 2 |
Subcategory: aspirin + dipyridamole vs clopidogrel PRoFESS |
‐ |
| Aspirin + clopidogrel |
Subcategory: aspirin + clopidogrel vs aspirin CHANCE; CHARISMA; COMPRESS; FASTER PILOT; Petrovska‐Cvetkovska 2008; POINT |
Subcategory: aspirin + clopidogrel vs clopidogrel MATCH 2001 |
‐ |
| Aspirin + cilostazol |
Subcategory: aspirin + cilostazol vs aspirin Nakamura 2010 |
‐ | ‐ |
| Aspirin + clopidogrel + dipyridamole | ‐ | ‐ |
Subcategory: aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole TARDIS |
Primary outcomes
Stroke
See Analysis 1.1; Figure 3.
1.1. Analysis.

Comparison 1: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Stroke
3.

Funnel plot of comparison: 1 Primary outcomes, outcome: 1.1 Stroke.
Stroke was found to be lower in the multiple antiplatelet group in 10 of 14 studies at three months (CHANCE; COMPRESS; EARLY‐trial; FASTER PILOT; MATCH 2001; Nakamura 2010; Petrovska‐Cvetkovska 2008; POINT; PRoFESS; TARDIS). Two studies did not report a single case of stroke recurrence (Chairangsarit 2005; De Martiis), whilst three studies had a higher number of strokes when participants received dual agents (CHARISMA; ESPIRIT; ESPS 2). The common factor in these three studies was the small number of events in each group, since they were all subanalyses of larger studies. CHANCE, which constituted 46% of participants, followed by POINT at 24%, and TARDIS 16%, showed a significant difference in favour of the intervention group in decrementing response. Overall, 480 of the 8299 (5.78%) participants receiving multiple antiplatelets had an episode of stroke, whilst 659 of the 8408 (7.84%) participants in the control group had an event. The risk ratio was found to be significant (RR 0.73, 95% confidence interval (CI) 0.66 to 0.82; P < 0.001; moderate‐certainty evidence), with a number needed to treat for an additional beneficial outcome (NNTB) of 48 participants to prevent one episode using more than a single antiplatelet agent.
As most of the studies compared dual versus single antiplatelet therapy, we conducted a secondary analysis that compared the effectiveness of different dual combinations with single antiplatelet therapy (A + B versus A or B or C). Most dual versus single antiplatelet therapy trials studied a combination of A + B versus A. We excluded two trials from this analysis: COMPRESS because it measured outcomes at one month alone and not at three months as in the other trials, and TARDIS because it tested multiple antiplatelet therapy against dual or single agents (A + B + C versus C or A + B) and was the only study with this comparison.
In terms of the primary outcome of stroke, 387 of the 6759 (5.73%) participants receiving dual antiplatelets had an episode of stroke, whilst 554 of the 6878 (8.06%) participants in the control group had an event. The risk ratio was found to be significant (RR 0.71, 95% CI 0.62 to 0.80; P < 0.001; moderate‐certainty evidence), that is 23 fewer events per 1000 with an NNTB of 43 participants to prevent one stroke using dual antiplatelet agents instead of single antiplatelet therapy.
Moreover, the combination of aspirin‐clopidogrel independently showed a significantly lower incidence of stroke in the intervention group compared to the control group (RR 0.72, 95% CI 0.63 to 0.82; P < 0.001) (Analysis 6.1) (6 studies: CHANCE; CHARISMA; FASTER PILOT; MATCH 2001; Petrovska‐Cvetkovska 2008; POINT). Five of these studies used aspirin in the control group apart from MATCH 2001 that used clopidogrel. The aspirin‐dipyridamole combination used in six studies showed a lower incidence of stroke in the dual combination group (RR 0.62, 95% CI 0.40 to 0.95; P = 0.03) (Analysis 7.1) (6 studies: Chairangsarit 2005; De Martiis; EARLY‐trial; ESPIRIT; ESPS 2; PRoFESS). All of these used aspirin in the control group apart from PRoFESS that used clopidogrel.
6.1. Analysis.

Comparison 6: Aspirin and clopidogrel versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Stroke
7.1. Analysis.

Comparison 7: Aspirin and dipyridamole versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Stroke
Vascular death
See Analysis 1.2.
1.2. Analysis.

Comparison 1: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 2: Vascular death
Eleven studies reported vascular death (Chairangsarit 2005; CHANCE; EARLY‐trial; ESPIRIT; ESPS 2; FASTER PILOT; Nakamura 2010; Petrovska‐Cvetkovska 2008; POINT; PRoFESS; TARDIS). Of these, vascular death occurred in 47 of 7882 (0.6%) participants in the intervention group and 53 of 8019 (0.66%) in the control group. The overall association was not significant (RR 0.98, 95% CI 0.67 to 1.45; P = 0.94; moderate‐certainty evidence). This finding was related to the large sample size of CHANCE. The difference could not be estimated in five studies where the outcome was assessed but no cases were reported (Chairangsarit 2005; FASTER PILOT; Nakamura 2010; Petrovska‐Cvetkovska 2008; PRoFESS).
When we removed TARDIS from the analysis to assess this primary outcome in terms of dual versus single antiplatelet therapy, the results were similar with vascular death in 34 out of 6342 participants in the intervention group and 46 out of 6489 in the control group (RR 0.84, 95% Cl 0.54 to 1.30; P = 0.43; moderate‐certainty evidence).
Secondary outcomes
2.1 Myocardial infarction
See Analysis 2.1.
2.1. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Myocardial infarction
Myocardial infarctions were reported in only three of the 15 included studies at three or more months (CHANCE; POINT; PRoFESS). All three of these studies examined dual versus single antiplatelet therapy, and the proportion was higher in the intervention group compared to the control group. There were 15 episodes in 5688 participants (0.26%) in the dual antiplatelet group and 11 episodes in 5723 participants (0.19%) in the control group. This association was not significant (RR 1.38, 95% CI 0.63 to 2.99; P = 0.42).
2.2 Stroke, myocardial infarction, or vascular death
See Analysis 2.2.
2.2. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 2: Stroke, myocardial infarction, or vascular death
Composite results from stroke, MI, and vascular death were reported in seven included studies that compared dual to single antiplatelet agent therapy (CHANCE; EARLY‐trial; ESPIRIT; FASTER PILOT; MATCH 2001; POINT; PRoFESS). A total of 412 cases from 6468 participants (6.37%) were reported in the intervention group compared to 567 cases from 6464 participants (8.77%) in the control group. The association was found to be significant (RR 0.72, 95% CI 0.64 to 0.82; P < 0.001; moderate‐certainty evidence), with 25 fewer events per 1000 in the intervention group. This finding suggests that to prevent one death from either stroke, MI, and vascular death, 42 participants needed to be treated with dual antiplatelet agents.
Three studies, COMPRESS, POINT, and PRoFESS subgroup, reported follow‐up outcome data at an earlier time point, that is one month from treatment (Analysis 5.1). A total of 114 cases from 3271 participants (3.49%) were reported in the intervention group compared to 158 cases from 3303 participants (4.78%) in the control group. The association was found to be significant (RR 0.73, 95% Cl 0.57 to 0.92; P = 0.008).
5.1. Analysis.

Comparison 5: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack at one month, Outcome 1: Stroke, myocardial infarction, or vascular death
2.3 Intracranial haemorrhage
See Analysis 2.3.
2.3. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 3: Intracranial haemorrhage
Six studies reported intracranial haemorrhage at three or more months (Chairangsarit 2005; CHANCE; Petrovska‐Cvetkovska 2008; POINT; PRoFESS; TARDIS). The incidence was found to be higher in the multiple antiplatelet therapy group compared to the control group, with a total of 30 cases of 7156 participants (0.42%) in the intervention group and 15 cases of 7131 participants (0.21%) in the control group. The association was found to be significant (RR 1.92, 95% CI 1.05 to 3.50; P = 0.03; low‐certainty evidence), with two more haemorrhages per 1000 in the intervention group.
On secondary analysis for dual versus single antiplatelet agent therapy, once TARDIS was excluded, a total of 19 cases of 5616 participants (0.34%) were reported in the intervention group compared to 12 cases of 5601 participants (0.21%) in the control group (Analysis 4.3). The association was not significant in this scenario (RR 1.53, 95% CI 0.76 to 3.06; P = 0.23), with one more haemorrhage per 1000 in the intervention group.
4.3. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 3: Intracranial haemorrhage
2.4 Extracranial haemorrhage
See Analysis 2.4.
2.4. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 4: Extracranial haemorrhage
Seven studies reported extracranial haemorrhage (CHARISMA; EARLY‐trial; ESPIRIT; MATCH 2001; POINT; PRoFESS; TARDIS). The incidence was found to be higher in the intervention group compared to the control group: extracranial haemorrhage was reported in 340 of 5325 participants (6.38%) in the intervention group and 150 of 5333 participants (2.81%) in the control group. TARDIS contributed 88.6% of the data to this analysis with a large effect. The association was found to be significant (RR 2.25, 95% CI 1.88 to 2.70; P < 0.001).
This result was maintained on secondary analysis for dual versus single antiplatelet agent therapy (RR 3.08, 95% CI 1.74 to 5.46; P < 0.001) (Analysis 4.4).
4.4. Analysis.
Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 4: Extracranial haemorrhage
2.5 Ischaemic stroke
See Analysis 2.5.
2.5. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 5: Ischaemic stroke
Ischaemic and haemorrhagic stroke were differentiated in CHANCE, POINT, and TARDIS. Ischaemic stroke occurred in 362 participants in the intervention group (5.52%) and 500 participants in the control group (7.62%). This association was found to be significant (RR 0.73, 95% CI 0.64 to 0.82, P < 0.001; high‐certainty evidence). There were 21 fewer events per 1000 in the intervention group, with an NNTB of 48 to prevent one ischaemic stroke.
For studies that reported dual versus antiplatelet agent therapy, the association was again significant in favour of dual antiplatelet therapy, with 27 fewer ischaemic strokes per 1000 in the intervention group (RR 0.70, 95% CI 0.61 to 0.81; P < 0.001) (Analysis 4.5).
4.5. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 5: Ischaemic stroke
2.6 Haemorrhagic stroke
See Analysis 2.6.
2.6. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 6: Haemorrhagic stroke
Three studies reported ischaemic and haemorrhagic strokes separately (CHANCE; POINT; TARDIS). Of these, 27 of the 6556 participants (0.41%) receiving dual antiplatelet, CHANCE; POINT, and triple antiplatelet therapy, TARDIS, developed haemorrhagic stroke, whilst 16 of the 6565 participants (0.24%) receiving single agents (or dual agents as in TARDIS) developed haemorrhagic stroke. The association was not significant (RR 1.69, 95% CI 0.91 to 3.13; P = 0.10; high‐certainty evidence).
This result was maintained on secondary analysis for dual versus single antiplatelet agent therapy once TARDIS was excluded (RR 1.19, 95% CI 0.53 to 2.64; P = 0.86) (Analysis 4.6).
4.6. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 6: Haemorrhagic stroke
2.7 Death from any cause
See Analysis 2.7.
2.7. Analysis.

Comparison 2: Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 7: Death from any cause
Four studies reported death from any cause (CHANCE; POINT; PRoFESS; TARDIS). Overall, 59 participants in the intervention group (0.82%) and 56 participants in the control group (0.77%) died from all causes. There was no significant difference between groups (RR 1.05, 95% CI 0.73 to 1.51; P = 0.79).
This result was maintained on secondary analysis for dual versus single antiplatelet agent therapy (RR 1.19, 95% CI 0.72 to 1.96; P = 0.50) (Analysis 4.7).
4.7. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 7: Death from any cause
Discussion
Summary of main results
We undertook this review to compare the use of multiple versus fewer antiplatelet agents to prevent recurrence after stroke or transient ischaemic attack (TIA). We analysed data from 15 studies. All combination therapies utilised aspirin as one of the drugs; the other drugs were either clopidogrel (7 studies), dipyridamole (6 studies), or cilostazol (1 study). The control group was typically a single agent and most frequently aspirin, with clopidogrel and dipyridamole used as controls infrequently. One study tested all three agents against aspirin and dipyridamole or clopidogrel alone.
The CHANCE trial consisted of 46.3% of the total number of participants included in the review. This was a multicentre study based in China that compared the effects of dual antiplatelets against a single antiplatelet agent after acute stroke. It reported efficacy outcomes and safety profile in detail. This was in contrast to four other secondary prevention studies which had different primary objectives, but as their subsets met our study criteria they were included in the analysis. Studies that were conducted prior to the 1990s tended not to report the study design and the safety profiles in detail.
Analysis revealed that multiple antiplatelet agents were associated with significantly lower incidence of stroke compared to fewer antiplatelet agents in people with a history of stroke or TIA. There was a relative reduction of 27% (95% CI 18% to 34%) corresponding to 21 strokes, ranging between 14 and 27 strokes (95% CI), avoided for every 1000 people treated with multiple antiplatelets compared to treatment with fewer (typically single) agents. Thus to avoid one stroke after an episode of stroke or TIA, 48 people need to be treated with multiple antiplatelets for a period of at least 30 days to avoid an event (Table 1). On secondary analysis, dual versus single antiplatelet therapy held this benefit, with a relative reduction of 29% (95% CI 20% to 38%), that is 23 strokes avoided for every 1000 people treated with dual antiplatelet therapy (Table 2).
Vascular death was the other primary outcome analysed in our review. Unlike stroke, however, this was not reported in all the included studies. In the 11 studies that did report vascular death, there was a slightly lower incidence in the intervention group compared to the control group. Multiple antiplatelets reduced the risk of vascular death by 0.06% compared to fewer antiplatelet agents. The association was not significant (95% CI 0.67 to 1.45; P = 0.94). This was perhaps because five of the eleven studies that reported vascular death did not report a single event in either arm. This would in turn suggest that a follow‐up period of three months is not sufficient to evaluate this outcome. Analysis of trials comparing only dual versus single antiplatelet therapy yielded similar results (RR 0.84, 95% CI 0.54 to 1.30; P = 0.43).
The composite outcome of stroke, myocardial infarction, or vascular death was associated with a reduction of 28%, which corresponds to 25 fewer strokes per 1000, with an NNTB of 42 people for participants who received dual antiplatelet therapy versus a single agent. On subgroup analysis of three studies that addressed follow‐up at one month, this outcome was again associated with a relative reduction of 27%.
The most commonly reported adverse events were intracranial haemorrhage (6 studies) and extracranial haemorrhage (7 studies). As expected, the proportion of intracranial and extracranial haemorrhage reported in the intervention group of multiple antiplatelets was higher compared to the control group. Intracranial haemorrhage was significantly higher in this comparison (RR 1.92, 95% CI 1.05 to 3.50; P = 0.03), with two more events per 1000. The association was found to be significant for extracranial haemorrhage as well, with 36 more events per 1000. Of note, the data in this group were largely affected by TARDIS, which contributed 88.6% of the total data included, and compared multiple antiplatelet therapy versus single or dual antiplatelet therapy with a significantly higher proportion of events in the intervention arm, raising concern over the safety of triple antiplatelet therapy. However, when dual antiplatelet therapy was compared to single antiplatelet therapy, the risk of intracranial haemorrhage was found to be statistically insignificant (RR 1.53, 95% CI 0.76 to 3.06; P = 0.23) with one more event per 1000. Nonetheless, the risk of extracranial haemorrhage remained significant (RR 3.08, 95% CI 1.74 to 5.46; P < 0.001).
When considering duration of treatment, subgroup analysis revealed benefit at one month of dual antiplatelet therapy initiated with 72 hours of symptom onset. The POINT study indicated the benefit from dual antiplatelet therapy to be more than the risk of major haemorrhage (including intracranial haemorrhage) at one‐week (2.9% composite outcome of ischaemic stroke, myocardial infarction, or ischaemic vascular death versus 0.3% major haemorrhage risk, P = 0.04) and one‐month follow‐up (3.9% composite outcome and 0.5% major haemorrhage risk, P = 0.02). Furthermore, secondary analysis to assess the time course for benefit and risk revealed an optimal duration of 21 days for dual therapy. However, this significance was lost at three‐month follow‐up with an increased risk of bleeding. In CHANCE, where early dual antiplatelet therapy was found to be effective and safe, participants in the intervention arm were administered dual antiplatelet therapy for 21 days, followed by monotherapy alone. Although these two studies differed not only in ethnicity but also in stroke mechanisms involved, the results were consistent for the first month. These data suggest that dual antiplatelet therapy for the duration of one month, or arguably 21 days, confers benefit in terms of secondary prevention of stroke, without a significantly increased risk of bleeding.
Almost half of the participants contributing data were from one study alone (CHANCE), based in China, which would seem to significantly affect the results. However, even on exclusion of the CHANCE study, the primary results did not change. There was a statistically lower incidence of stroke, more specifically ischaemic stroke, in the group receiving multiple antiplatelets or dual agents versus those receiving a single agent. Similarly, adverse outcomes such as intracranial haemorrhage also remained unchanged.
Adverse outcomes other than haemorrhage that were included in the protocol, such as myocardial infarction, were only reported in a few studies. It was therefore difficult to reach a conclusion regarding these adverse events.
Overall completeness and applicability of evidence
Our review analysed 15 trials, mostly of which were of good quality. However, trials pre‐1990 were not clearly reported in terms of design and safety profiles. One finding, although accounted for, is that almost half the data were contributed by CHANCE alone. However, it is important to note that the primary and secondary outcomes did not change drastically even after CHANCE was excluded from the analyses, and so the greater benefit to risk is maintained. It may be argued that this was observed most when dual antiplatelet therapy was continued for the first month of therapy.
This review applies to atherothrombotic strokes and not cardioembolic strokes, which puts into perspective the population to whom these findings can be applied. The participants included in the analysis received at least one month of therapy, and the range of follow‐up, although for 3.5 years in some cases, was limited to three months in most cases.
Perhaps the biggest limitation of this analysis stems from the inclusion of studies whose subset analyses were used since they often failed to report safety profiles as measures of interest. We thus lacked information on outcomes such as myocardial infarction and overall mortality, and so no conclusions can be made regarding these outcomes. Estimations can be made, however, for safety in terms of haemorrhage, which was more frequently reported with the combination of multiple versus fewer antiplatelet agents than of dual versus single antiplatelet use.
The trials included in this review mostly used clopidogrel (usual dose 75 mg) or dipyridamole (usual dose 400 mg) in combination with aspirin (dose 75 mg to 81 mg), and loading doses were often used. CHANCE used a loading dose of 300 mg of clopidogrel, whilst POINT used 600 mg.
It appears that, at least in the short term after an atherothrombotic stroke, a dual antiplatelet agent approach with loading doses may prevent 23 strokes per 1000 people, as well as 25 strokes, myocardial infarctions, and vascular deaths per 1000 people against one intracranial haemorrhage per 1000 people administered therapy for one month.
Quality of the evidence
The evidence for this review came from well‐designed trials; however, study designs were not well reported for studies that were conducted prior to 1990. Subset analyses often limit the outcomes of interest. The certainty of evidence was based on the GRADE approach, and the evidence for the primary outcomes was downgraded for risk of bias in the included trials. Another domain rated was the magnitude of effect, where a large effect was noted in the secondary outcomes of intracranial and extracranial haemorrhage.
We performed sensitivity analyses as Chairangsarit 2005 reported more than 20% missing data at 28.9%. We analysed data without this study and found the robustness of the pooled RRs adequate for the primary outcomes of stroke (RR 0.73 95% CI 0.66 to 0.82; P < 0.001) and vascular death (RR 0.98, 95% CI 0.67 to 1.45; P = 0.94).
Potential biases in the review process
We do not report any conflicts of interest. The protocol was designed and registered to study this topic prior to collection of data and analysis, and at a time when some of the included trials were still ongoing and unpublished. We excluded non‐randomised studies due to their high susceptibility of error and bias. We reviewed data independently and then cross‐checked them centrally to avoid biases in observations and conclusions. Variation in frequency and dose of drugs in the included trials were within limits of those used in clinical practice and would not have made a difference to the review outcome.
Agreements and disagreements with other studies or reviews
The conclusions presented in our study are in agreement with a previous systematic review by Geeganage 2012, which concurred that dual antiplatelets are effective and may be safe in preventing recurrence of stroke when compared to monotherapy.
Authors' conclusions
Implications for practice.
The results of our review indicate that, in the high‐risk phase after stroke, multiple antiplatelet agents are more effective than single agents at preventing stroke recurrence. The evidence is strongest for secondary stroke prevention in people with ischaemic stroke. Most of the evidence comes from trials comparing two antiplatelet agents versus a single agent and, in those trials, the risk of adverse events was less than the benefit in terms of preventing stroke. There was a lack of evidence regarding multiple versus multiple antiplatelet agents. Further refinement of the benefit and risk of two antiplatelet agents and the optimal duration of treatment will depend on future research.
Implications for research.
Our analysis highlights the lack of data regarding the use of dual antiplatelets. As mentioned previously, one study from Asia contributed a large portion of the participants, and so future studies need to be undertaken in other populations to establish the effectiveness of dual antiplatelets. Studies should focus on the efficacy and safety profile of using dual antiplatelets, in shorter follow‐up periods. Additional trials that address variation in underlying aetiologies as well as disease severity may provide more insight.
What's new
| Date | Event | Description |
|---|---|---|
| 24 September 2020 | Amended | An amendment has been made to the 'Authors conclusions' section of the Abstract |
History
Protocol first published: Issue 3, 2012 Review first published: Issue 8, 2020
Acknowledgements
We acknowledge the assistance of Hina Tejani, Musa Khan, and Khawaja Mustafa for local assistance in the preparation of this review. We thank Peter Sandercock, Peter Langhorne, Hazel Fraser, Joshua Cheyne, and our reviewers for their extensive input and assistance in the shaping of this review.
Appendices
Appendix 1. CENTRAL search strategy
#1MeSH descriptor: [Cerebrovascular Disorders] this term only1425 #2MeSH descriptor: [Basal Ganglia Cerebrovascular Disease] this term only10 #3MeSH descriptor: [Brain Ischemia] explode all trees3534 #4MeSH descriptor: [Carotid Artery Diseases] this term only471 #5MeSH descriptor: [Carotid Artery Thrombosis] this term only18 #6MeSH descriptor: [Intracranial Arterial Diseases] this term only10 #7MeSH descriptor: [Cerebral Arterial Diseases] this term only26 #8MeSH descriptor: [Intracranial Embolism and Thrombosis] explode all trees308 #9MeSH descriptor: [Stroke] explode all trees9502 #10(isch?emi* near/6 (stroke* or apoplex* or cerebral vasc* or cerebrovasc* or cva or attack*)):ti,ab,kw15375 #11((brain or cerebr* or cerebell* or vertebrobasil* or hemispher* or intracran* or intracerebral or infratentorial or supratentorial or middle cerebr* or mca* or anterior circulation) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus* or hypoxi*)):ti,ab,kw16412 #12tia*10578 #13{or #1‐#12}39827 #14MeSH descriptor: [Platelet Aggregation Inhibitors] explode all trees3834 #15(antiplatelet& or anti‐platelet* or antiaggreg* or anti‐aggreg* or (platelet* near/5 inhibit*) or (thrombocyt* near/5 inhibit*)):ti,ab,kw10918 #16(alprostadil* or aspirin* or dipyridamol* or disintegrin* or epoprostenol* or iloprost* or ketanserin* or ketorolac tromethamine* or milrinone* or mopidamol* or pentoxifyllin* or ticlopidine* or thiophen* or trapidil* or prasugrel or terutroban):ti,ab,kw22091 #17(acetyl salicylic acid* or acetyl?salicylic acid or clopidogrel* or picotamide* or ligustrazine* or levamisol$ or suloctidil* or ozagrel* or oky046 or oky‐046 or defibrotide$ or cilostazol or satigrel or sarpolgrelate or kbt3022 or kbt‐3022 or isbogrel or cv4151 or cv‐4151 or triflusal):ti,ab,kw10586 #18(Dispril or Albyl* or Ticlid* or Persantin* or Plavix or Aggrenox or Pletal):ti,ab,kw393 #19MeSH descriptor: [Platelet Glycoprotein GPIIb‐IIIa Complex] explode all trees and with qualifier(s): [antagonists & inhibitors ‐ AI, drug effects ‐ DE]492 #20(((glycoprotein iib* or gp iib*) near/5 (antagonist* or inhibitor*)) or GR144053 or GR‐144053 or abciximab* or tirofiban* or eftifibatid*):ti,ab,kw2378 #21ReoPro or Integrilin* or Aggrastat271 #22MeSH descriptor: [Platelet Activation] explode all trees and with qualifier(s): [drug effects ‐ DE]1833 #23MeSH descriptor: [Blood Platelets] explode all trees and with qualifier(s): [drug effects ‐ DE]1101 #24(sulphinpyrazone or sulfinpyrazone or indobufen):ti,ab,kw236 #25{or #14‐#24}32587 #26#13 and #254527
Appendix 2. MEDLINE search strategy
1. cerebrovascular disorders/ or basal ganglia cerebrovascular disease/ or exp brain ischemia/ or carotid artery diseases/ or carotid artery thrombosis/ or intracranial arterial diseases/ or cerebral arterial diseases/ or exp "intracranial embolism and thrombosis"/ or exp stroke/ 2. (isch?emi$ adj6 (stroke$ or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva or attack$)).tw. 3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebr$ or mca$ or anterior circulation) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw. 4. tia$1.tw. 5. or/1‐4 6. exp platelet aggregation inhibitors/ 7. (antiplatelet$ or anti‐platelet$ or antiaggreg$ or anti‐aggreg$ or (platelet$ adj5 inhibit$) or (thrombocyt$ adj5 inhibit$)).tw. 8. (alprostadil$ or aspirin$ or dipyridamol$ or disintegrin$ or epoprostenol$ or iloprost$ or ketanserin$ or ketorolac tromethamine$ or milrinone$ or mopidamol$ or pentoxifyllin$ or ticlopidine$ or thiophen$ or trapidil$ or prasugrel or terutroban).tw. 9. (acetyl salicylic acid$ or acetyl?salicylic acid or clopidogrel$ or picotamide$ or ligustrazine$ or levamisol$ or suloctidil$ or ozagrel$ or oky046 or oky‐046 or defibrotide$ or cilostazol or satigrel or sarpolgrelate or kbt3022 or kbt‐3022 or isbogrel or cv4151 or cv‐4151 or triflusal).tw. 10. (Dispril or Albyl$ or Ticlid$ or Persantin$ or Plavix or Aggrenox or Pletal).tw. 11. Platelet Glycoprotein GPIIb‐IIIa Complex/ai, de [Antagonists & Inhibitors, Drug Effects] 12. (((glycoprotein iib$ or gp iib$) adj5 (antagonist$ or inhibitor$)) or GR144053 or GR‐44053 or abciximab$ or tirofiban$ or eftifibatid$).tw. 13. (ReoPro or Integrilin$ or Aggrastat).tw. 14. exp Platelet Activation/de [Drug Effects] 15. exp Blood Platelets/de [Drug Effects] 16. (sulphinpyrazone or sulfinpyrazone or indobufen).tw. 17. or/6‐16 18. randomized controlled trial.pt. 19. controlled clinical trial.pt. 20. randomized.ab. 21. placebo.ab. 22. clinical trials as topic.sh. 23. random$.ab. 24. trial.ti. 25. or/18‐24 26. exp animals/ not humans.sh. 27. 25 not 26 28. 5 and 17 and 27
Appendix 3. Embase search strategy
1. cerebrovascular disease/ or cerebral artery disease/ or cerebrovascular accident/ or stroke/ or vertebrobasilar insufficiency/ or carotid artery disease/ or exp carotid artery obstruction/ or exp brain infarction/ or exp brain ischemia/ or exp occlusive cerebrovascular disease/ 2. (isch?emi$ adj6 (stroke$ or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva or attack$)).tw. 3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebr$ or mca$ or anterior circulation) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw. 4. tia$1.tw. 5. or/1‐4 6. exp antithrombocytic agent/ 7. (antiplatelet$ or anti‐platelet$ or antiaggreg$ or anti‐aggreg$ or (platelet$ adj5 inhibit$) or (thrombocyt$ adj5 inhibit$)).tw. 8. (alprostadil$ or aspirin$ or dipyridamol$ or disintegrin$ or epoprostenol$ or iloprost$ or ketanserin$ or ketorolac tromethamine$ or milrinone$ or mopidamol$ or pentoxifyllin$ or ticlopidine$ or thiophen$ or trapidil$ or prasugrel or terutroban).tw,tn. 9. (acetyl salicylic acid$ or acetyl?salicylic acid or clopidogrel$ or picotamide$ or ligustrazine$ or levamisol$ or suloctidil$ or ozagrel$ or oky046 or oky‐046 or defibrotide$ or cilostazol or satigrel or sarpolgrelate or kbt3022 or kbt‐3022 or isbogrel or cv4151 or cv‐4151 or triflusal).tw,tn. 10. (Dispril or Albyl$ or Ticlid$ or Persantin$ or Plavix or Aggrenox or Pletal).tw,tn. 11. exp fibrinogen receptor/ 12. (((glycoprotein iib$ or gp iib$) adj5 (antagonist$ or inhibitor$)) or GR144053 or GR‐144053 or abciximab$ or tirofiban$ or eftifibatid$).tw. 13. (ReoPro or Integrilin$ or Aggrastat).tw,tn. 14. exp thrombocyte activation/ 15. exp thrombocyte/ 16. (sulphinpyrazone or sulfinpyrazone or indobufen).tw. 17. or/6‐16 18. 5 and 17 19. Randomized Controlled Trial/ or "randomized controlled trial (topic)"/ 20. Randomization/ 21. Controlled clinical trial/ or "controlled clinical trial (topic)"/ 22. control group/ or controlled study/ 23. clinical trial/ or "clinical trial (topic)"/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/ 24. Crossover Procedure/ 25. Double Blind Procedure/ 26. Single Blind Procedure/ or triple blind procedure/ 27. placebo/ or placebo effect/ 28. (random$ or RCT or RCTs).tw. 29. (controlled adj5 (trial$ or stud$)).tw. 30. (clinical$ adj5 trial$).tw. 31. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 32. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 33. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 34. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 35. (cross‐over or cross over or crossover).tw. 36. (placebo$ or sham).tw. 37. trial.ti. 38. (assign$ or allocat$).tw. 39. controls.tw. 40. or/19‐39 41. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 42. 18 and 40 43. 42 not 41
Appendix 4. ClinicalTrials.gov search strategy
(antiplatelet agents OR platelet aggregation inhibitors ) AND ( ischaemic stroke OR brain ischaemia OR cerebral infarction OR ischaemic attack ) [DISEASE]
Appendix 5. WHO ICTRP search strategy
Condition: stroke OR ischaemic attack Intervention: antiplatelet OR alprostadil OR aspirin OR dipyridamol OR disintegrin OR epoprostenol OR iloprost OR ketanserin OR ketorolac OR tromethamine OR milrinone OR mopidamol OR pentoxifylline OR ticlopidine OR thiophene OR trapidil OR prasugrel OR terutroban Recruitment status is: ALL Phases are: ALL Display synonyms: ‐ ischemic attack ‐ ACCIDENT CEREBROVASCULAR, ACCIDENT; CEREBRAL, ACCIDENT; CEREBROVASCULAR, APOPLEXY, APOPLEXY, CEREBROVASCULAR, APOPLEXY; CEREBRAL, BRAIN ATTACK, BRAIN VASCULAR ACCIDENT, BRAIN VASCULAR ACCIDENTS, CEREBRAL VASCULAR ACCIDENT, CEREBRAL VASCULAR EVENTS, CEREBRAL; ACCIDENT, CEREBRAL; APOPLEXY, CEREBROVASCULAR ACCIDENT, CEREBROVASCULAR ACCIDENT (DISORDER), CEREBROVASCULAR ACCIDENT NOS, CEREBROVASCULAR ACCIDENT, NOS, CEREBROVASCULAR ACCIDENTS, CEREBROVASCULAR APOPLEXY, CEREBROVASCULAR; ACCIDENT, CVA, CVA (CEREBRAL VASCULAR ACCIDENT), CVA (CEREBROVASCULAR ACCIDENT), CVA NOS, CVAS (CEREBROVASCULAR ACCIDENT), NEURO: CEREBROVASCULAR ACCIDENT, VASCULAR ACCIDENT, BRAIN, VASCULAR ACCIDENTS, BRAIN, stroke ‐ OXPENTIFYLLINE, PENTOXYFYLLINE, PENTOXYPHYLLINE, PTX, pentoxifylline ‐ ABBOTT BRAND OF TROMETAMOL, THAM, TRI(HYDROXYMETHYL)AMINOMETHANE, TRIS BUFFER, TRIS(HYDROXYMETHYL)AMINOMETHANE, TRIS‐(HYDROXYMETHYL) AMINOMETHANE, TRISAMINE, TROMETAMOL, TROMETAMOL ABBOTT BRAND, tromethamine ‐ EPOPROSTANOL, PGI2, PGX, PROSTACYCLIN, PROSTAGLANDIN I 02, PROSTAGLANDIN I(2), PROSTAGLANDIN I2, PROSTAGLANDIN PGI2, PROSTAGLANDIN PGI>2<, PROSTAGLANDIN PGI2, PROSTAGLANDIN X, epoprostenol ‐ antiplatelet ‐ ticlopidine ‐ disintegrin ‐ DIPYRAMIDOLE, dipyridamol ‐ (11ALPHA,13E,15S)‐11,15‐DIHYDROXY‐9‐OXOPROST‐13‐EN‐1‐OIC ACID, LIPO PGE1, LIPO‐PGE1, PGE 01, PGE1, PGE1ALPHA, PROSTAGLANDIN E 01, PROSTAGLANDIN E1, PROSTAGLANDIN E1, PROSTAGLANDIN E1ALPHA, PROSTAGLANDIN PGE1, PROSTAGLANDIN PGE>1<, PROSTAGLANDIN PGE1, PROSTAGLANDIN PGE1 (SUBSTANCE), alprostadil ‐ 3‐((6‐AMINO‐(4‐CHLOROBENZENESULFONYL)‐2‐METHYL‐5,6,7,8‐TETRAHYDRONAPHT)‐1‐YL)PROPIONIC ACID, terutroban ‐ 3‐(2‐(4‐(4‐FLUOROBENZOYL)PIPERIDINOL)ETHYL)‐2,4(1H,3H)‐QUINAZOLINEDIONE, ketanserin ‐ THIOFURAN, THIOLE, thiophene ‐ prasugrel ‐ mopidamol ‐ milrinone ‐ ketorolac ‐ TRAPYMIN, trapidil ‐ iloprost ‐ 2‐(ACETYLOXY)BENZOIC ACID, ACETYLSALICYCLIC ACID, ACETYLSALICYLIC ACID, ACID, ACETYLSALICYLIC, AMPICILLIN, ASA, aspirin
Data and analyses
Comparison 1. Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Stroke | 14 | 16707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.66, 0.82] |
| 1.1.1 Aspirin + dipyridamole vs aspirin | 5 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.38, 1.11] |
| 1.1.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.27, 1.17] |
| 1.1.3 Aspirin + clopidogrel vs aspirin | 5 | 10739 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.63, 0.82] |
| 1.1.4 Aspirin + clopidogrel vs clopidogrel | 1 | 485 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.97] |
| 1.1.5 Aspirin + cilostazol vs aspirin | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.13] |
| 1.1.6 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3070 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.67, 1.15] |
| 1.2 Vascular death | 11 | 15901 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.67, 1.45] |
| 1.2.1 Aspirin + dipyridamole vs aspirin | 4 | 868 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.38, 1.11] |
| 1.2.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.2.3 Aspirin + clopidogrel vs aspirin | 4 | 10527 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.63, 2.98] |
| 1.2.4 Aspirin + cilostazol vs aspirin | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.2.5 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3070 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [0.74, 4.61] |
Comparison 2. Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Myocardial infarction | 3 | 11411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.63, 2.99] |
| 2.1.1 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.14, 7.25] |
| 2.1.2 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.62, 3.39] |
| 2.2 Stroke, myocardial infarction, or vascular death | 7 | 12932 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.82] |
| 2.2.1 Aspirin + dipyridamole vs aspirin | 2 | 638 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.42, 1.07] |
| 2.2.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.38, 1.34] |
| 2.2.3 Aspirin + clopidogrel vs aspirin | 3 | 10443 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.82] |
| 2.2.4 Aspirin + clopidogrel vs clopidogrel | 1 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.41, 1.59] |
| 2.3 Intracranial haemorrhage | 6 | 14287 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [1.05, 3.50] |
| 2.3.1 Aspirin + dipyridamole vs aspirin | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [0.12, 62.70] |
| 2.3.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 2.3.3 Aspirin + clopidogrel vs aspirin | 3 | 9819 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.57, 2.86] |
| 2.3.4 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3070 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.18 [1.17, 8.66] |
| 2.4 Extracranial haemorrhage | 7 | 10658 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.25 [1.88, 2.70] |
| 2.4.1 Aspirin + dipyridamole vs aspirin | 2 | 638 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.06, 14.61] |
| 2.4.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.40, 3.54] |
| 2.4.3 Aspirin + clopidogrel vs aspirin | 2 | 5097 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.81 [2.19, 10.57] |
| 2.4.4 Aspirin + clopidogrel vs clopidogrel | 1 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.67 [0.41, 32.62] |
| 2.4.5 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3072 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.16 [1.78, 2.61] |
| 2.5 Ischaemic stroke | 3 | 13121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.64, 0.83] |
| 2.5.1 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.61, 0.81] |
| 2.5.2 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3070 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.62, 1.36] |
| 2.6 Haemorrhagic stroke | 3 | 13121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.91, 3.13] |
| 2.6.1 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.53, 2.64] |
| 2.6.2 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3070 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.78 [1.00, 7.70] |
| 2.7 Death from any cause | 4 | 14502 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.73, 1.51] |
| 2.7.1 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.26, 2.78] |
| 2.7.2 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.73, 2.23] |
| 2.7.3 Aspirin + clopidogrel + dipyridamole vs clopidogrel or aspirin + dipyridamole | 1 | 3091 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.54, 1.55] |
Comparison 3. Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Stroke | 13 | 13637 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.62, 0.80] |
| 3.1.1 Aspirin + dipyridamole vs aspirin | 5 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.38, 1.11] |
| 3.1.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.27, 1.17] |
| 3.1.3 Aspirin + clopidogrel vs aspirin | 5 | 10739 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.63, 0.82] |
| 3.1.4 Aspirin + clopidogrel vs clopidogrel | 1 | 485 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.97] |
| 3.1.5 Aspirin + cilostazol vs aspirin | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.13] |
| 3.2 Vascular death | 10 | 12831 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 3.2.1 Aspirin + dipyridamole vs aspirin | 4 | 868 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.38, 1.11] |
| 3.2.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.2.3 Aspirin + clopidogrel vs aspirin | 4 | 10527 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.63, 2.98] |
| 3.2.4 Aspirin + cilostazol vs aspirin | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
3.1. Analysis.

Comparison 3: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Stroke
3.2. Analysis.

Comparison 3: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 2: Vascular death
Comparison 4. Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Myocardial infarction | 3 | 11411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.63, 2.99] |
| 4.1.1 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.14, 7.25] |
| 4.1.2 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.62, 3.39] |
| 4.2 Stroke, myocardial infarction, or vascular death | 7 | 12932 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.82] |
| 4.2.1 Aspirin + dipyridamole vs aspirin | 2 | 638 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.42, 1.07] |
| 4.2.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.38, 1.34] |
| 4.2.3 Aspirin + clopidogrel vs aspirin | 3 | 10443 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.82] |
| 4.2.4 Aspirin + clopidogrel vs clopidogrel | 1 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.41, 1.59] |
| 4.3 Intracranial haemorrhage | 5 | 11217 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [0.76, 3.06] |
| 4.3.1 Aspirin + dipyridamole vs aspirin | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [0.12, 62.70] |
| 4.3.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.3.3 Aspirin + clopidogrel vs aspirin | 3 | 9819 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.72, 3.02] |
| 4.4 Extracranial haemorrhage | 6 | 7586 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [1.74, 5.46] |
| 4.4.1 Aspirin + dipyridamole vs aspirin | 2 | 638 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.06, 14.61] |
| 4.4.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.40, 3.54] |
| 4.4.3 Aspirin + clopidogrel vs aspirin | 2 | 5097 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.81 [2.19, 10.57] |
| 4.4.4 Aspirin + clopidogrel vs clopidogrel | 1 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.67 [0.41, 32.62] |
| 4.5 Ischaemic stroke | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.61, 0.81] |
| 4.5.1 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.61, 0.81] |
| 4.6 Haemorrhagic stroke | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.53, 2.64] |
| 4.6.1 Aspirin + dipyridamole vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.53, 2.64] |
| 4.7 Death from any cause | 3 | 11411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.72, 1.96] |
| 4.7.1 Aspirin + clopidogrel vs aspirin | 2 | 10051 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.73, 2.23] |
| 4.7.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.26, 2.78] |
4.1. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 1: Myocardial infarction
4.2. Analysis.

Comparison 4: Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack, Outcome 2: Stroke, myocardial infarction, or vascular death
Comparison 5. Dual versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack at one month.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Stroke, myocardial infarction, or vascular death | 3 | 6574 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.57, 0.92] |
| 5.1.1 Aspirin + clopidogrel vs aspirin | 2 | 5214 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.53, 0.87] |
| 5.1.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.65, 3.02] |
Comparison 6. Aspirin and clopidogrel versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Stroke | 6 | 11224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.63, 0.82] |
| 6.1.1 Aspirin + clopidogrel vs aspirin | 5 | 10739 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.63, 0.82] |
| 6.1.2 Aspirin + clopidogrel vs clopidogrel | 1 | 485 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.97] |
Comparison 7. Aspirin and dipyridamole versus one antiplatelet agent for preventing early recurrence after ischaemic stroke or transient ischaemic attack.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Stroke | 6 | 2337 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.40, 0.95] |
| 7.1.1 Aspirin + dipyridamole vs aspirin | 5 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.38, 1.11] |
| 7.1.2 Aspirin + dipyridamole vs clopidogrel | 1 | 1360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.27, 1.17] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chairangsarit 2005.
| Study characteristics | ||
| Methods | Randomised, open‐label, blind assessment | |
| Participants | Participants with acute ischaemic stroke enrolled within 48 hours after clinical onset. Age should be more than 45 years. CT or MRI of the brain confirmed cerebral infarction and excluded haemorrhagic stroke or brain tumour. 38 participants were enrolled in the study (20 men, 18 women). Participants were followed up through clinic visits at 1 month, 3 months, and 6 months. |
|
| Interventions | Aspirin 300 mg once daily vs aspirin 300 mg once daily plus dipyridamole 75 mg 3 times a day | |
| Outcomes | Primary outcome: recurrent ischaemic stroke and TIA Secondary outcome: vascular death due to MI or any type of stroke |
|
| Notes | During the 9‐month screening period, 39 of 60 eligible participants were recruited and followed up for 6 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blinded randomisation |
| Allocation concealment (selection bias) | Low risk | Methods described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participant is aware of treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 11 of 38 (28.9%) participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
CHANCE.
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled trial | |
| Participants | 5170 participants (3350 men, 1750 women) of Chinese ethnicity took part in the study. Participants had a history of stroke or TIA. Age of participants was greater than 40 years. Participants with acute non‐disabling ischaemic stroke (NIHSS ≤ 3 at the time of randomisation) that can be treated with study drug within 24 hours of symptoms onset; or TIA (neurological deficit attributed to focal brain ischaemia, with resolution of the deficit within 24 hours of symptom onset), that can be treated with study drug within 24 hours of symptoms onset and with moderate‐to‐high risk of stroke recurrence (ABCD2 score ≥ 4 at the time of randomisation) | |
| Interventions | Clopidogrel 75 mg once daily (loading dose 300 mg first day) and aspirin 75 mg vs placebo and aspirin 75 mg. On the first day all participants received open‐label aspirin at a clinician‐determined dose of 75 to 300 mg per day. 165 participants in the combination group and 146 participants in the aspirin‐only group had stopped taking their medicine at the time of follow‐up. |
|
| Outcomes | Primary outcome: any stroke (ischaemic or haemorrhage) at 90 days follow‐up Secondary outcome: participants with the 3‐month new clinical vascular events (ischaemic stroke/haemorrhagic stroke/TIA/MI/vascular death) as a cluster and evaluated individually. Modified Rankin Scale score changes (continuous) and dichotomised at percentage with score 0 to 2 vs 3 to 6 at 3‐month follow‐up. Further efficacy exploratory analysis: impairment (changes in NIHSS scores at 3‐month follow‐up) and quality of life (EuroQol EQ‐5D scale) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centralised, automated system random assignment |
| Allocation concealment (selection bias) | Low risk | Site randomisation different from primary team |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐dummy, double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20 of 2584 participants (0.8%) in the combination group (clopidogrel + aspirin) and 16 of 2586 participants (0.6%) in the aspirin‐alone group were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
CHARISMA.
| Study characteristics | ||
| Methods | Randomised, multicentre, parallel‐group, double‐blind, placebo‐controlled trial | |
| Participants | Individuals with symptomatic cerebrovascular disease within the previous 5 years | |
| Interventions | Aspirin 75 to 162 mg once daily plus clopidogrel 75 mg once daily vs aspirin 75 to 162 mg daily + placebo | |
| Outcomes | Primary outcome: stroke Secondary outcome: MI, vascular death, or the composite of stroke, MI, vascular death |
|
| Notes | Subanalysis of a larger CHARISMA trial of participants with recent event | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Methods described |
| Allocation concealment (selection bias) | Low risk | Methods described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo given |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
COMPRESS.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants with cerebral ischaemic stroke identified on DWI within 48 hours from symptom onset, relevant cerebral atherosclerosis on MRA, study drug administration within 48 hours from symptom onset, and mRS is 0 to 2 before the stroke | |
| Interventions | Clopidogrel plus aspirin (75 mg/d without loading dose plus 300 mg loading dose followed by 100 mg/d) vs aspirin alone (300 mg loading dose followed by 100 mg/d) for 30 days + placebo | |
| Outcomes | Primary outcome: number of participants with new lesions after the onset of acute atherothrombotic stroke (7 or 30 day, or both, on DWI) Secondary outcomes: distribution of mRS scores (time frame: 30 days after the onset of stroke throughout the study period), non‐fatal stroke, MI and vascular death (composite, first‐ever), all types of stroke, number of participants with bleeding episode (major and minor) during the follow‐up period, number of participants with symptomatic ICH at 1 month |
|
| Notes | Conducted in 10 Korean centres; 2 participants crossed over from intervention to control arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 1:1 ratio stratified random assignment performed centrally by a computer‐generated randomisation sequence |
| Allocation concealment (selection bias) | Low risk | Independent adjudication committee |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo (matched to clopidogrel for taste, colour, and size) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
De Martiis.
| Study characteristics | ||
| Methods | Prospective, controlled study | |
| Participants | Individuals under age 65 who had experienced at least 1 transient atherothrombotic cerebral event according to Joint Committee for Stroke facilities | |
| Interventions | Dipyridamole 400 mg per day vs aspirin 100 mg + dipyridamole 300 mg per day | |
| Outcomes | Ischaemic events (stroke, TIA), deaths (stroke, cardiovascular, all‐cause mortality) | |
| Notes | Subanalysis of participants recruited early in a secondary prevention trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information regarding randomisation |
| Allocation concealment (selection bias) | Unclear risk | No method described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description of placebo pills provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No method described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 11 of 197 (5.6%) participants enrolled lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Outcomes reported |
EARLY‐trial.
| Study characteristics | ||
| Methods | Prospective, randomised, open‐label, blinded, endpoint trial in 46 stroke units in Germany | |
| Participants | Individuals aged > 18 years presenting with symptoms of an acute ischaemic stroke causing measurable neurological defect (NIHSS 5 to 20). Randomised and treated within 24 hours | |
| Interventions | Aspirin 25 mg and extended‐release dipyridamole 200 mg twice daily vs 100 mg aspirin once daily | |
| Outcomes | mRS score and vascular adverse events (non‐fatal stroke, TIA, non‐fatal MI, and bleeding complications) | |
| Notes | Subset | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using a pseudorandom number generator |
| Allocation concealment (selection bias) | Low risk | Through telephone interview |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20% discontinued treatment due to various causes |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
ESPIRIT.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants referred to the hospital within 6 months of reporting a TIA or minor ischaemic stroke (grade < 3 on mRS) | |
| Interventions | Aspirin 325 mg vs aspirin 325 mg + dipyridamole 200 mg twice daily | |
| Outcomes | Fatal and non‐fatal ischaemic strokes and cardiac events (fatal and non‐fatal MI, sudden death, and death from cardiovascular causes) | |
| Notes | Subanalysis of a larger study on anticoagulation, focus on antiplatelet intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used centralised randomisation via phone, fax, email |
| Allocation concealment (selection bias) | Low risk | Computer‐generated allocation concealment by clinical epidemiologist not involved in clinical trial |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study design for pragmatic outcome assessment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study design for pragmatic outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 106 (3.8%) lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes accounted for |
ESPS 2.
| Study characteristics | ||
| Methods | Randomised, placebo‐controlled, double‐blinded study | |
| Participants | Individuals older than 18 years with TIA or stroke within the preceding 3 months | |
| Interventions | Aspirin 50 mg daily alone vs aspirin 50 mg once daily plus modified release dipyridamole 400 mg daily vs modified‐release dipyridamole 400 mg alone vs placebo | |
| Outcomes | Stroke, death, and stroke or death | |
| Notes | Subset analysis of those treated early | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done through minimisation technique |
| Allocation concealment (selection bias) | Low risk | Sequence generated centrally |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Medicine cessation in 479 of 1650 participants (29%) in intervention group and 851 of 3303 participants (25.7%) in control group. Although the dropout rates are significant, the sample size is large enough to justify attrition. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
FASTER PILOT.
| Study characteristics | ||
| Methods | Double‐blinded RCT | |
| Participants | 185 women and 187 men recruited in the trial. Participants had a history of stroke or TIA. Age of participants had to be greater than 40 years and should not have been eligible for thrombolysis or acute intervention. Symptoms present for at least 5 minutes and included weakness or language disturbance. Enrolment must be done within 24 hours of symptom onset. Exclusion criteria included pure sensory symptoms, presumed cardiac source of emboli, and stroke/TIA mimics. 194 participants assigned to groups without clopidogrel (control) and 198 participants assigned to clopidogrel group. Participants were followed up in clinic at 10 days and 90 days. 1 participant was lost to follow‐up in each group. |
|
| Interventions | Aspirin 81 mg (day 1: aspirin 162 mg) once daily plus clopidogrel 75 mg (300 mg loading dose) once daily vs aspirin only 81 mg (day 1: aspirin 162 mg) To ensure follow‐ups, telephone calls were made at 2, 30, 60, and 90 days. |
|
| Outcomes | Primary outcome: any stroke at 90 days Secondary outcome: composite of any stroke, MI, and vascular death |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Low risk | Pharmacist provided predetermined kits. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 7 (1.8%) participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported |
MATCH 2001.
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo controlled | |
| Participants | Individuals > 40 years with TIA or ischaemic stroke in last 3 months and at least 1 risk factor | |
| Interventions | Aspirin 75 mg per day + clopidogrel 75 mg per day vs clopidogrel 75 mg per day | |
| Outcomes | First occurrence of an event | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Methods described |
| Allocation concealment (selection bias) | Low risk | Used interactive voice response system (telephone) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13 of 7599 participants (0.1%) lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported |
Nakamura 2010.
| Study characteristics | ||
| Methods | Randomised. Unclear allocation and blinding | |
| Participants | 76 participants (56 men and 20 women) of Japanese ethnicity with a history of non‐cardioembolic stroke Mean age of participants was between 66 and 67 years. There were 38 participants in each group, with 4 participants lost to follow‐up in each group. Participants in the combination treatment group (aspirin + cilostazol) complained of drug eruption (1 participant) and palpitations (3 participants). Participants in the aspirin‐only group reported drug eruption (2 participants), gastrointestinal bleeding (1 participant), and acute coronary event (1 participant). Participants were followed at 14 days and then at 6 months. |
|
| Interventions | Cilostazol 100 mg twice daily plus aspirin 300 mg once daily for 4 days and a lower dose of aspirin from day 5 until 6 months The other group received only aspirin 300 mg once daily for 4 days and a lower dose of aspirin from day 5 until 6 months. |
|
| Outcomes | Primary outcome: neurological deterioration or stroke recurrence within 14 days Secondary outcome: neurological deterioration or stroke recurrence within 6 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation |
| Allocation concealment (selection bias) | Low risk | Random allocation concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 of 76 participants (10.5%) lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
Petrovska‐Cvetkovska 2008.
| Study characteristics | ||
| Methods | Randomised, open‐label. Unclear outcome assessment blinding and allocation concealment | |
| Participants | Participants had a history of TIA, were randomised within the first 24 hours. 40 participants received aspirin 75 mg + clopidogrel 75 mg and 44 received aspirin (100 mg to 325 mg) alone. | |
| Interventions | 1 group received oral aspirin 75 mg and oral clopidogrel 75 mg once daily while the other group received oral aspirin 100 mg to 325 mg alone. Participants were followed up for 1 year. | |
| Outcomes | Primary outcome: recurrent TIA or stroke Secondary: intracranial or systemic adverse effects |
|
| Notes | 2 other groups received statins | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label trial |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label trial |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clearly described |
| Selective reporting (reporting bias) | Unclear risk | Not clearly described |
POINT.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Individuals with high‐risk TIA (defined as an ABCD2 score > 4) or minor ischaemic stroke (with NIHSS < 3) and study drug administered within 12 hours of time last known free of new ischaemic symptoms | |
| Interventions | Clopidogrel plus aspirin versus aspirin alone | |
| Outcomes | Primary outcome: new ischaemic vascular events (ischaemic stroke, MI, and ischaemic vascular death) Secondary outcomes: risk of ischaemic stroke, intracranial haemorrhage, and major haemorrhage, and composite of the primary outcome and major haemorrhage |
|
| Notes | Subgroup analysis at 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random selection by computer software |
| Allocation concealment (selection bias) | Low risk | Allocation concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment by independent study group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for as lost to follow‐up or ceased treatment |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
PRoFESS.
| Study characteristics | ||
| Methods | Randomised. Allocation concealment | |
| Participants | 1360 participants (884 men and 476 women) with a history of stroke. Age of participants was greater than 55 years. Participants had to be hospitalised with stable stroke. 5 of 672 participants in the combination group (aspirin + extended‐release dipyridamole) and 7 of 688 participants in the clopidogrel‐only group were lost to follow‐up. 36 participants complained of headache in the combination group, whilst 3 participants in the clopidogrel‐only group reported adverse effects. | |
| Interventions | Aspirin 25 mg twice daily plus extended‐release dipyridamole 200 mg twice daily vs clopidogrel 75 mg alone once daily followed for 90 days | |
| Outcomes | Primary outcome: mRS at 30 days Secondary outcome: recurrent stroke, haemorrhagic transformation |
|
| Notes | Subset of participants enrolled early | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Methods described. |
| Allocation concealment (selection bias) | Low risk | Methods described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 of 1360 participants (0.8%) lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
TARDIS.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Individuals with acute non‐cardioembolic ischaemic stroke (less than 48 hours of onset) or acute TIA (less than 48 hours of onset) with 1 or more of: crescendo TIA (greater than 1 TIA within 1 week), and/or admitted on dual antiplatelet therapy (aspirin/dipyridamole, aspirin/clopidogrel, clopidogrel/dipyridamole), and/or with an ABCD2 score > 5 | |
| Interventions | Aspirin, clopidogrel, and dipyridamole vs aspirin and dipyridamole or clopidogrel | |
| Outcomes | Primary outcome: ordinal stroke severity at 90 days Secondary outcomes: binary and ordinal outcomes of stroke, TIA, MI, acute coronary syndrome, composite vascular outcome, death. Also safety (ordinal bleeding events), tolerability, and feasibility. Additional measures included transcranial Doppler for embolic events, laboratory measures (FBC and P‐Selectin), clinical efficacy (NIHSS), function (mRS, BI), cognition (TICS), quality of life (EuroQoL, EQ‐5D), mood (Zung), disposition, days at home, and economic activity | |
| Notes | Estimated study completion date: March 2017 (5 years duration from start‐up phase) 3096 participants recruited from the UK and internationally, to assess the efficacy, safety, and health economics of triple therapy, with endpoints measured at 7, 35, and 90 days. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based 1:1 ratio simple randomisation, with stratification and minimisation |
| Allocation concealment (selection bias) | Low risk | Methods described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Outcome blinded assessment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes validated and categorised by expert adjudicators masked to treatment assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All accounted for as lost to follow‐up or refused. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
BI: Barthel Index
CT: computed tomography
DWI: diffusion weighted imaging
FBC: full blood count
ICH: intracerebral haemorrhage
MI: myocardial infarction
MRA: magnetic resonance angiography
MRI: magnetic resonance imaging
mRS: modified Rankin Scale
NIHSS: National Institutes of Health Stroke Scale
RCT: randomised controlled trial
TIA: transient ischaemic attack
TICS: Telephone Interview for Cognitive Status
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| AICLA | Participants were not randomised in the first 72 hours. |
| AMBDAP | Primary endpoint was embolic signals. |
| APACHE‐AF 2014 | Anticoagulants are compared in the study; our review is restricted to antiplatelet agents alone. |
| APLAUD 2000 | Participants were not randomised in the first 72 hours. |
| Apollonio 1989 | Measure of outcome was change in stenosis. |
| ATARI | Unclear time to randomisation |
| AVERROES | Compared single antiplatelet vs anticoagulant: aspirin vs apixaban |
| Bath 2002 | Multiple antiplatelet agents were administered for long‐term secondary prevention, not for prevention of early recurrence of ischaemic stroke or TIA. |
| CADISS | Anticoagulants are compared in the study; our review is restricted to antiplatelet agents alone. |
| Caneschi 1985 | Participants were not randomised in the first 72 hours. |
| CARESS | Treatment given for only 7 days. |
| CATHARSIS | Participants were not randomised in the first 72 hours. |
| CCS 1978 | Participants were not randomised in the first 72 hours. |
| CLAIR | Follow‐up period short. Did not measure clinical outcome |
| CLOSURE | Anticoagulants compared in the study; our review is restricted to antiplatelet agents alone. |
| CSPS.com | Aspirin and cilostazol vs aspirin; however, participants were not randomised in the first 72 hours |
| Fan 2004 | Unclear treatment duration |
| Fujimoto 2010 | Treatment for less than 1 month |
| Fujimoto 2011 | Treatment for less than 1 month |
| Hashemilar 2011 | Microembolic signals used to measure outcome. |
| Herskovits 1981 | Participants were not randomised within the first 72 hours. |
| Herskovits 1985a | Participants were not randomised within the first 72 hours. |
| Herskovits 1985b | Participants were not randomised within the first 72 hours. |
| Herskovits 1989 | Participants were not randomised within the first 72 hours. |
| JASAP | Participants were not randomised in the first 72 hours. |
| Khazaei 2018 | Unclear time of enrolment from stroke onset, and primary outcome was secondary TIA |
| PATICI 1985 | Participants were not enrolled within 72 hours. |
| PERFORM | Compared single antiplatelet agents |
| PLATO 2009 | Compared single antiplatelet agents |
| PRCASA | Primary outcome measure was restenosis measured through cerebral angiography. |
| RE‐SPECT‐ESUS 2014 | Anticoagulants compared in the study; our review is restricted to antiplatelet agents alone. |
| Rizky 2015 | Unclear time of enrolment from stroke onset |
| Sancho Rieger 1984 | Compared single antiplatelet agents, ticlopidine vs dipyridamole |
| Satoh 1994 | Compared same antiplatelet doses (pyrazolopyridine) |
| SOCRATES 2014 | Compared single antiplatelet agents |
| SPS3 | Unclear time to randomisation |
| Stakhovskaya 2001 | Participants were not randomised within 72 hours. |
| TACS 2000 | Participants were not randomised in the first 72 hours. |
| Terayama 2008 | Stroke recurrence not reported, and only progression of event followed. |
| TOPALS | Participants were not randomised in the first 72 hours. |
| TOSS | Participants were not randomised in the first 72 hours. |
| Uchiyama 1989 | Unclear time to randomisation |
| Uchiyama 1991 | Unclear time to randomisation |
| Uchiyama 1992 | Unclear time to randomisation |
| UMPIRE | Compared different risk factor control medications. Combination pill vs single |
| Vaya 1988 | Studied effect on platelet reactivity |
| WASID 1998 | Anticoagulants were compared in the study; our review is restricted to antiplatelet agents alone. |
| WOEST 2013 | Anticoagulants were used at baseline. |
| Zuo 2017 | Participants were randomised in the first 7 days instead of first 72 hours. |
TIA: transient ischaemic attack
Characteristics of ongoing studies [ordered by study ID]
THALES 2018.
| Study name | THALES |
| Methods | RCT |
| Participants | Participants are ≥ 40 years of age with non‐cardioembolic ischaemic stroke of NIHSS of ≤ 5 or high‐risk TIA (defined as ABCD2 score of ≥ 6 or with ipsilateral large vessel stenosis of ≥ 50%). Participants are randomised within 24 hours of the time last known free of new ischaemic symptoms, and study drug is administered immediately afterwards. |
| Interventions | Ticagrelor and aspirin compared with aspirin |
| Outcomes | The primary efficacy outcome is time from randomisation to first subsequent stroke or death through 30 days of treatment. The primary safety outcome is time to first severe bleeding event based on the GUSTO definition. |
| Starting date | 22 January 2018 |
| Contact information | |
| Notes | Met primary endpoint as presented at International Stroke Conference, final results pending. |
GUSTO: Global Use of Strategies To Open up coronary arteries NIHSS: National Institutes of Health Stroke Scale RCT: randomised controlled trial TIA: transient ischaemic attack
Differences between protocol and review
We conducted a secondary analysis of dual versus single antiplatelets, as most of the included studies compared dual antiplatelets to a single agent.
Although we did not initially intend to do so, we explored a trial of one‐month duration as a change in the protocol (COMPRESS), and included this in analysis with trials that clearly reported relevant outcome data at one month.
Contributions of authors
IAN drafted the protocol, developed tools for data abstraction, reviewed studies, performed data analysis, and drafted the manuscript. AKK conceived the idea, assisted in reviewing studies, manuscript editing and provided oversight. HR reviewed papers, added studies for analysis, and assisted in manuscript writing.
Sources of support
Internal sources
-
The Aga Khan University Hospital, Pakistan
Library access, electronic support, and professional development
External sources
No sources of support supplied
Declarations of interest
Imama A Naqvi: none known Ayeesha K Kamal: none known Hasan Rehman: none known
Edited (no change to conclusions)
References
References to studies included in this review
Chairangsarit 2005 {published data only}
- Chairangsarit P, Sithinamsuwan P, Niyasom S, Udommongkol C, Nidhinandana S, Suwantamee J. Comparison between aspirin combined with dipyridamole versus aspirin alone within 48 hours after ischemic stroke event for prevention of recurrent stroke and improvement of neurological function: a preliminary study. Journal of the Medical Association of Thailand 2005;88(Suppl 3):S148-54. [PubMed] [Google Scholar]
CHANCE {published data only}
- NCT00979589. Clopidogrel in High-risk patients with Acute Non-disabling Cerebrovascular Events (CHANCE). www.clinicaltrials.gov/ct2/show/NCT00979589 (first received 15 February 2012).
- Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. New England Journal of Medicine 2013;369(1):11-9. [DOI: 10.1056/NEJMoa1215340] [DOI] [PubMed] [Google Scholar]
CHARISMA {published data only}
- Hankey GJ, Johnston CS, Easton JD, Hacke W, Mas J-L, Brennan D, the CHARISMA trial investigators. Effect of clopidogrel plus ASA vs ASA early after TIA and ischaemic stroke: a substudy of the CHARISMA trial. International Journal of Stroke 2001;6:3-9. [DOI] [PubMed] [Google Scholar]
COMPRESS {published data only}
- Hong KS, Lee SH, Kim EG, Cho KH, Chang DI, Rha JH, et al. Recurrent ischemic lesions after acute atherothrombotic stroke: clopidogrel plus aspirin versus aspirin alone. Stroke 2016;47(9):2323-30. [DOI] [PubMed] [Google Scholar]
- NCT00814268. COMbination of Clopidogrel and Aspirin for Prevention of Early REcurrence in Acute Atherothrombotic Stroke (COMPRESS). www.clinicaltrials.gov/ct2/show/NCT00814268 (first received 15 February 2012).
De Martiis {published data only}
- De Martiis M, Parenzi A, Barlattani A, De Martiis A. Randomized clinical study of the efficacy of buflomedil in the prevention of recurrence of cerebral ischemia in comparison with anti-platelet aggregation agents. La Clinica Terpeutica 1986;116(5):367-71. [PubMed] [Google Scholar]
EARLY‐trial {published data only}
- Adams HP. EARLY antiplatelet treatment after ischaemic stroke. Lancet Neurology 2010;9:131-3. [DOI] [PubMed]
- Dengler R, Diener HC, Grond M, Haberl R, Leonard J, Machnig T, et al. Early treatment with aspirin and extended-release dipyridamole versus low dose aspirin alone for TIA/ischaemic stroke within 24 hour of symptom onset (EARLY-trial): a randomised open-label blinded-endpoint trial. Lancet Neurology 2010;9:159-66. [DOI] [PubMed] [Google Scholar]
- Dengler R, Diener HC, Schwartz A, Grond M, Schumacher H, Machnig T, et al. Early treatment with aspirin plus extended-release dipyridamole for transient ischaemic attack or ischaemic stroke within 24 h of symptom onset (EARLY trial): a randomised, open-label, blinded-endpoint trial. European Journal of Neurology 2009;16(Suppl 3):655 (Abst.LBN101). [DOI] [PubMed]
- Dengler R, Lichtinghagen R, Schumacher H, Weissenborn K, Worthmann H. C-reactive protein and its pharmacologic reduction as predictor of outcome in the early treatment with aspirin and extended-release dipyridamole versus low dose aspirin alone for TIA/ischemic stroke within 24 hour of symptom-onset (EARLY-Trial). Stroke 2010;41(4):e261 (Abst. P27). [Google Scholar]
- Dengler R. Early administration of Aggrenox is effective and safe after acute ischaemic stroke or TIA. www.prnewswire.co.uk/cgi/news/release?id=265925 (accessed prior to 10 August 2020).
- NCT00562588. EARLY 3-months Aggrenox treatment started within 24 hrs of ischemic stroke onset vs after one week 100 mg ASA. www.clinicaltrials.gov/ct2/show/NCT00562588 (first received 15 February 2012).
- Schwartz A, Dengler R, Eschenfelder C, Eisert W, Schumacher H, Haberl R, et al. Early treatment with aspirin plus extended-release dipyridamole for TIA/ischaemic stroke within 24 hours of symptom onset (EARLY-trial): results of the MRI substudy. Cerebrovascular Diseases 2010;29 Suppl 2:12 (Abst. 4).
- Worthmann H, Lichtinghagen R, Dengler R, Schumacher H, Schwartz A, Eisert W, et al. Relationship between inflammatory biomarkers, acute treatment and clinical outcome after ischaemic stroke and TIA: a substudy of the EARLY trial. Cerebrovascular Diseases 2010;29 Suppl 2:12 (Abst. 4).
ESPIRIT {published data only}
- The ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet 2006;367:1665-73. [DOI] [PubMed] [Google Scholar]
ESPS 2 {published data only}
- Diener H, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European stroke prevention study 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. Journal of the Neurological Sciences 1996;143:1-13. [DOI] [PubMed] [Google Scholar]
FASTER PILOT {published data only}
- Geraghty OC, Kennedy J, Chandratheva A, Marquardt L, Buchan AM, Rothwell PM. Preliminary evidence of a high risk of bleeding on aspirin plus clopidogrel in aspirin-naïve patients in the acute phase after TIA or minor ischaemic stroke. Cerebrovascular Diseases 2010;29:460-7. [DOI] [PubMed] [Google Scholar]
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM. Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER):a randomised controlled pilot trial. Lancet Neurology 2007;6:961-9. [DOI] [PubMed] [Google Scholar]
MATCH 2001 {published data only}
- Amarenco P, Donnan GA. Should the MATCH results be extrapolated to all stroke patients and affect ongoing trials evaluating clopidogrel plus aspirin? Stroke 2004;35:2606-8. [DOI] [PubMed] [Google Scholar]
- Benavente O, Pearce L, Amarenco P, Streifler J, Kase C. Is there a different effect of clopidogrel plus aspirin versus clopidogrel alone on stroke patients with small vessel disease and large artery atherosclerosis? Analysis from MATCH. Stroke 2007;38(2):522. [Google Scholar]
- Bezerra DC, Bogousslavsky J. Antiplatelets in stroke prevention: the MATCH trial. Some answers, many questions and countless perspectives. Cerebrovascular Diseases 2005;20 Suppl 2:109-18. [DOI] [PubMed] [Google Scholar]
- Calvet D, Touze E, Mas J-L. Adding aspirin to clopidogrel in secondary prevention of ischemic stroke: no significant benefits - results of the Match study. Presse Medicale 2006;35(4 II):679-82. [DOI] [PubMed] [Google Scholar]
- Caplan LR. Thoughts evoked by MATCH and other trials. Stroke 2004;35:2604-5. [DOI] [PubMed] [Google Scholar]
- Carolei A. MATCH: Management of atherothrombosis with clopidogrel in high-risk patients with recent transient ischemic attack or ischemic stroke. In: Italian Stroke Forum. 2001.
- Diener H-C, Bogousslavsky J, Brass LM, Cimminiello C, Csiba L, Kaste M, et al. Management of atherothrombosis with clopidogrel in high-risk patients with recent transient ischemic attacks or ischemic stroke (MATCH): trial design and rationale. Cerebrovascular Diseases 2004;17(23):253-61. [DOI: 10.1159/000076962] [DOI] [PubMed] [Google Scholar]
- Diener H-C. Management of atherosclerosis with clopidogrel in high-risk patients with recent transient ischaemic attack or ischemic stroke (MATCH): study results. Stroke 2004;35(6):e181. [DOI] [PubMed] [Google Scholar]
- Dulli D. The MATCH trial: disappointments and surprises. Cardiology Review 2006;23(2):42-3. [Google Scholar]
- Fisher M, Davalos A. The MATCH Study results in the context of secondary stroke prevention. Stroke 2004;35:2609. [DOI] [PubMed] [Google Scholar]
- Frey JL. The results of MATCH: light or heat? Lancet Neurology 2004;3:642. [DOI] [PubMed] [Google Scholar]
- Hacke W. From CURE to MATCH: ADP receptor antagonists as the treatment of choice for high-risk atherothrombotic patients. Cerebrovascular Diseases 2002;13 Suppl 1:22-6. [DOI] [PubMed] [Google Scholar]
- Hankey G, Moneuse P, Gabriel S. Building a link between disability after an ischemic stroke and need for follow-up care. Cerebrovascular Diseases 2005;19 Suppl 2:37. [Google Scholar]
- Ling GSF, Eriksson P, Bath P, Diener H-C. Role of aspirin in MATCH. Lancet 2004;364:1661-3. [DOI] [PubMed] [Google Scholar]
- Lutsep HL. MATCH results: implications for the internist. American Journal of Medicine 2006;119:526.e1-7. [DOI] [PubMed] [Google Scholar]
- Moussouttas M. Emerging therapies: clopidogrel and aspirin. Stroke 2005;36(4):707. [DOI] [PubMed] [Google Scholar]
- Nitschmann S, Hartung HP, Siebler M. Secondary prevention of stroke - clopidogrel only or in combination with acetylsalicylic acid: the MATCH study. Internist 2005;46:1278-82. [DOI] [PubMed] [Google Scholar]
- Rothell PM. Lessons from MATCH for future randomised trials in secondary prevention of stroke. Lancet 2004;364(9431):305-7. [DOI] [PubMed] [Google Scholar]
- Skvortsova VI, Shamalov NA. The results of the MATCH study evidence for advantages of clopidogrel monotherapy as secondary prophylaxis in cerebrovascular pathology. Zhurnal Nevrologii i Psikhiatrii Imeni S.S. Korsakova 2004;Suppl 11:7-12. [PubMed] [Google Scholar]
- Spiel M, Diener HC. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Tagliche Praxis 2005;46(4):858. [DOI] [PubMed] [Google Scholar]
Nakamura 2010 {published data only}
- Nakamura T, Tsuruta S, Uchiyama S. Cilostazol combined with aspirin prevents early neurological deterioration in patients with acute ischemic stroke: a pilot study. Journal of the Neurological Sciences 2012;313(1-2):22–6. [DOI] [PubMed] [Google Scholar]
Petrovska‐Cvetkovska 2008 {published data only}
- Petrovska-Cvetkovska D, Baneva N, Trencev R, Georgievska A, Radulovic-Bekarovska S. Efficacy and tolerability of aspirin, aspirin plus clopidogrel and statins in prevention after transient ischemic attacks. International Journal of Stroke 2008;3 Suppl 1:314 (Abst.PO02-192). [Google Scholar]
POINT {published data only}
- Johnston SC, Easton JD, Farrant M, Barsan W, Battenhouse H, Conwit R, et al. Platelet-oriented inhibition in new TIA and minor ischemic stroke (POINT) trial: rationale and design. International Journal of Stroke 2013;8(6):479-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston SC, Easton JD, Farrant M, Barsan W, Conwit RA, Elm JJ, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. New England Journal of Medicine 2018;379(3):215-25. [DOI: 10.1056/NEJMoa1800410] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston SC, Elm JJ, Easton JD, Farrant M, Barsan WG, Kim AS, et al. Time course for benefit and risk of clopidogrel and aspirin after acute transient ischemic attack and minor ischemic stroke: a secondary analysis from the POINT randomized trial. Circulation 2019;140(8):658-64. [DOI: 10.1161/CIRCULATIONAHA.119.040713] [DOI] [PubMed] [Google Scholar]
- NCT00991029. Platelet-Oriented Inhibition in New TIA and minor ischemic stroke (POINT) Trial. www.clinicaltrials.gov/ct2/show/NCT00991029 (first received 25 August 2017).
PRoFESS {published data only}
- Bath PMW, Cotton D, Martin RH, Palesch Y, Yusuf S, Sacco R, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke. PRoFESS Subgroup Analysis. Stroke 2010;41:732-8. [DOI] [PubMed] [Google Scholar]
TARDIS {published data only}
- Bath PM, Woodhouse LJ, Appleton JP, Beridze M, Christensen H, Dineen RA, et al. Antiplatelet therapy with aspirin, clopidogrel, and dipyridamole versus clopidogrel alone or aspirin and dipyridamole in patients with acute cerebral ischaemia (TARDIS): a randomised, open-label, phase 3 superiority trial. Lancet 2018;391(10123):850-9. [DOI: 10.1016/S0140-6736(17)32849-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01661322. Safety and tolerability of clopidogrel when added to aspirin and dipyridamole in high risk patients with recent ischaemic stroke: a randomised controlled trial. www.clinicaltrials.gov/ct2/show/NCT01661322 (first received 15 February 2012).
References to studies excluded from this review
AICLA {published data only}
- Bousser MG, Eschwege E, Hagenau M, Lefaucconnier JM, Thibult N, Touboul D, et al. 'AICLA' controlled trial of aspirin and dipyridamole in the secondary prevention of athero-thrombotic cerebral ischemia. Stroke 1983;14(1):5-14. [DOI] [PubMed] [Google Scholar]
AMBDAP {published data only}
- King A, Bath PMW, Markus HS. Clopidogrel versus dipyridamole in addition to aspirin in reducing embolization detected with ambulatory transcranial Doppler. A randomized trial. Stroke 2011;42:650-5. [DOI] [PubMed] [Google Scholar]
APACHE‐AF 2014 {published data only}
- Nieuwenhuizen KM, Worp HB, Algra A, Kappelle LJ, Rinkel GJE, Gelder IC, Schutgens REG, Klijn CJM, APACHE-AF Investigators. Apixaban versus Antiplatelet drugs or no antithrombotic drugs after anticoagulation-associated intraCerebral HaEmorrhage in patients with Atrial Fibrillation (APACHE-AF): study protocol for a randomised controlled trial. Trials 2015 Sep 4;16:393. [DOI: 10.1186/s13063-015-0898-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
APLAUD 2000 {published data only}
- Harrington RA, Graffagnino C, Armstrong PW, Joseph D, Card TL, Sigmon KN, et al. Dose-finding and tolerability of a new oral platelet glycoprotein IIb/IIIa inhibitor, SB 214857, in patients with coronary artery and cerebrovascular disease: the APLAUD results. Circulation 1998;98(17 Suppl 1). [CN-00371224]
- Harrington RA. Dose-finding and tolerability of a new oral platelet glycoprotein IIb/IIIa inhibitor, SB214857, in patients with coronary artery disease and cerebrovascular disease: the APLAUD. American Heart Journal 1999;137(3):572-3. [CN-00445649]
Apollonio 1989 {published data only}
- Apollonio A, Castignani P, Magrini L, Angeletti R. Ticlopidine-pentoxifylline combination in the treatment of atherosclerosis and the prevention of cerebrovascular accidents. Journal of International Medical Research 1989;17:28-35. [DOI] [PubMed] [Google Scholar]
ATARI {published data only}
- Hankey GJ. Ongoing and planned trials of antiplatelet therapy in the acute and long-term management of patients with ischaemic brain syndromes: setting a new standard of care. Cerebrovascular Diseases 2004;17 Suppl 3:11-6. [DOI] [PubMed] [Google Scholar]
AVERROES {published data only}
- NCT00496769. A phase III study of Apixaban in patients with atrial fibrillation (AVERROES). www.clinicaltrials.gov/ct2/show/NCT00496769 (first received 15 February 2012). [CN-00645054]
- O'Donnell, Yusuf S, Eikelboom J, Hart R, Diener HC, Diehl A. Effect of apixaban on covert cerebral infarction and microbleeds: AVERROES MRI assessment study. Cerebrovascular Diseases 2012;33 Suppl 2:47. [CN-00854733]
Bath 2002 {published data only}
- Sprigg N, Gray LJ, England T, Willmot MR, Zhao L, Sare GM, et al. A randomised controlled trial of triple antiplatelet therapy (aspirin, clopidogrel and dipyridamole) in the secondary prevention of stroke: safety, tolerability and feasibility. PLoS ONE 2008;3(8):e2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
CADISS {published data only}
- Cervical Artery Dissection in Stroke Study Trial Investigators. Antiplatelet therapy vs. anticoagulation in cervical artery dissection: rationale and design of the Cervical Artery Dissection in Stroke Study (CADISS). International Journal of Stroke 2007;2(4):292-6. [DOI: 10.1111/j.1747-4949.2007.00165.x] [CN-00687538] [DOI] [PubMed]
- Markus HS, Levi C, King A, Madigan J, Norris J, Cervical Artery Dissection in Stroke Study (CADISS) Investigators. Antiplatelet Therapy vs Anticoagulation Therapy in Cervical Artery Dissection: The Cervical Artery Dissection in Stroke Study (CADISS) Randomized Clinical Trial Final Results. JAMA Neurology 2019 Jun 1;76(6):657-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warlow CP. Comment on the CADISS trial protocol. International Journal of Stroke 2007;2:291. [CN-00644422] [DOI] [PubMed]
Caneschi 1985 {published data only}
- Caneschi S, Bonaventi C, Finzi F. Ischemic cerebrovascular disease: treatment with different platelet suppressant drugs. Clinical follow-up of 80 patients (22-34 months). Minerva Medica 1985;76:1933-43. [PubMed] [Google Scholar]
CARESS {published data only}
- Dittrich R, Ritter MA, Kaps M, Siebler M, Lees K, Larrue V, et al. The use of embolic signal detection in multicenter trials to evaluate antiplatelet efficacy. Signal analysis and quality control mechanisms in the CARESS (Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic carotid Stenosis) trial. Stroke 2006;37(4):1065-9. [DOI] [PubMed] [Google Scholar]
- Imray CHE, Higman DJ, Marshall C, Cohen SN, Markus HS, Droste DW, et al. Letter regarding article by Markus et al, "Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic cardiac stenosis evaluated using doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic carotid Stenosis (CARESS) trial". Circulation 2005;112(20):e325; author reply e325-6. [PubMed]
- Markus H, Ringelstein EB. Evaluating antiplatelet agents using asymptomatic microembolic signals as a surrogate end point: lessons from the CARESS trial. Journal of the Neurological Sciences 2005;238 Suppl 1:S42 (Abst. IS249).
- Markus HS, Droste DW, Kaps M, Larrue V, Lees KR, Siebler M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using Doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation 2005;111(17):2233-40. [DOI] [PubMed]
CATHARSIS {published data only}
- NCT00333164. Cilostazol-Aspirin Therapy Against Recurrent Stroke With Intracranial Artery Stenosis. www.clinicaltrials.gov/ct2/show/NCT00333164 (first received 15 February 2012).
- Uchiyama S, Sakai N, Takagi M, Minematsu K, Ezura M, Okada Y, et al. Analysis of baseline data on the Cilostazol-Aspirin Therapy Against Recurrent Stroke with Intracranial Artery Stenosis (CATHARSIS). Stroke 2011;42(3):e346 (Abst.Th P320). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchiyama S, Sakai N, Toi S, Ezura M, Okada Y, Takagi M, et al. Cilostazol plus aspirin versus aspirin alone in patients with symptomatic intracranial arterial stenosis: results of CATHARSIS. Journal of the Neurological Sciences 2013;333:e194. [DOI: 10.1016/j.jns.2013.07.781] [CN-01006701] [DOI]
- Uchiyama S, Sakai N, Toi S, Ezura M, Okada Y, Takagi M, et al. Final results of cilostazol-aspirin therapy against recurrent stroke with intracranial artery stenosis (CATHARSIS). Cerebrovascular Diseases Extra 2015 Jan 15;5(1):1-13. [DOI: 10.1159/000369610] [DOI] [PMC free article] [PubMed]
- Uchiyama S, Sakai N, Toi S, Ezura M, Okada Y, Takagi M, et al. Final results of cilostazol-aspirin therapy against recurrent stroke with intracranial artery stenosis (CATHARSIS). Stroke 2011;42(3):e346 (Abst.Th P320). [DOI] [PMC free article] [PubMed]
CCS 1978 {published data only}
- Barnett HJM. Aspirin and sulfinpyrazone in threatened stroke - the results of the Canadian collaborative double blind trial. In: Acetylsalicylic Acid in Cerebral Ischaemia and Coronary Heart Disease. 1st edition. Stuttgart: Schattauer Verlag, 1978:93-6. [Google Scholar]
- Barnett HJM. Canadian cooperative platelet-inhibiting drug trial in threatened stroke. Stroke 1978;9:110-1. [Google Scholar]
- Barnett HJM. The Canadian cooperative platelet-inhibition drug trial. Canadian Journal of Neurological Sciences 1978;5(3):338-9. [Google Scholar]
- Barnett JHM. A randomized trial of aspirin and sulfinpyrazone in threatened stroke. The Canadian Cooperative Study Group. New England Journal of Medicine 1978;299(2):53-9. [DOI] [PubMed] [Google Scholar]
- Gent M, Barnett HJM, Sackett DL, Taylor DW. A randomized trial of aspirin and sulfinpyrazone in patients with threatened stroke: results and methodological issues. Circulation 1980;62 (Suppl V):97-105. [PubMed] [Google Scholar]
- Gent M. The Canadian Cooperative Study of platelet suppressant therapy in threatened stroke. Thrombosis and Haemostasis 1979;41(1):163-70. [PubMed] [Google Scholar]
- Kurtzke JF. Controversy in neurology: the Canadian study on TIA and aspirin. A critique of the Canadian TIA study. Annals of Neurology 1979;5:597-602. [DOI] [PubMed] [Google Scholar]
- Lauzier S, Cote R, Ogunyami A, Hopkins M, Vandervoort MK, Barnett HJM. Predictive value of cerebral atheroma in 158 patients - a 10 year follow-up. Stroke 1986;17:127. [Google Scholar]
- Stuart RK, Barnett HJM. The effect of sulfinpyrazone and aspirin on the ivy template bleeding time. Thrombosis and Haemostasis 1977;38(1):279. [Google Scholar]
- Taylor DW, Sackett DL, Barnett HJM. A randomized trial of aspirin and sulfinpyrazone in patients with transient ischemic attacks. American Journal of Epidemiology 1978;108(3):228-9. [Google Scholar]
- The Canadian Cooperative Study Group. A randomized trial of aspirin and sulfinpyrazone in threatened stroke. New England Journal of Medicine 1978;299(2):53-9. [DOI] [PubMed] [Google Scholar]
CLAIR {published data only}
- Wong KSL, Chen C, Fu J, Chang HM, Suwanwela NC, Huang YN, et al. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. Lancet Neurology 2010;9:489-97. [DOI] [PubMed] [Google Scholar]
CLOSURE {published data only}
- Furlan AJ, Reisman M, Massaro J, Mauri L, Adams H, Albers GW, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. New England Journal of Medicine 2012;366(11):991-9. [DOI] [PubMed] [Google Scholar]
CSPS.com {published data only}
- Toyoda K, Uchiyama S, Hoshino H, Kimura K, Origasa H, Naritomi H, et al. Protocol for Cilostazol Stroke Prevention Study for Antiplatelet Combination (CSPS.com): a randomized, open-label, parallel-group trial. International Journal of Stroke 2015;10:253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fan 2004 {published data only}
- Fan Y-H, Wong K-S, Ng P-W, Tsoi TH, Yeung H-M, Wong C-K. Tolerability of clopidogrel combining with aspirin in Chinese patients with aspirin failure. Journal of Clinical Neuroscience 2004;11 Suppl 1:S48 (Abst.PP4.06). [Google Scholar]
Fujimoto 2010 {published data only}
- Fujimoto S, Jinnouchi J, Inoue T, Suzuki S, Sadoshima S. Effect of combined antithrombotic treatment with cilostazol for progressive stroke. International Journal of Stroke 2010;5 Suppl 2:87-8. [Google Scholar]
Fujimoto 2011 {published data only}
- Fujimoto S, Jinnouchi J, Matsuki T, Suzuki S, Inoue T, Amemiya T, et al. Effect of early cilostazol in the acute phase of non-cardioembolic stroke. Cerebrovascular Diseases 2011;31 Suppl 2:128-9 (Abst.310). [Google Scholar]
Hashemilar 2011 {published data only}
- Hashemilar M, Farhoudi M, Hosseini S, Moshayedi H, Savadi Oskoui D, Oghli BE, et al. Frequency of microembolic signals in patients with acute ischemic stroke in middle cerebral artery territory treated with aspirin or clopidogrel. Iranian Journal of Neurology 2011;10(1-2):16-8. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Herskovits 1981 {published data only}
- Herskovits E, Famulari A, Tamaroff L, Gonzalez AM, Vazquez A, Smud R, et al. Randomised trial of pentoxifylline versus acetylsalicylic acid plus dipyridamole in preventing transient ischaemic attacks. Lancet 1981;2:966-8. [DOI] [PubMed] [Google Scholar]
- Herskovits E, Vazquez A, Famulari A, Tamaroff L, Fraiman H, Gonzáles AM, et al. A randomized clinical trial of pentoxifylline and antiaggregants in recent transient ischemic attacks (TIA). A one year follow-up. Ricerca in Clinica e in Laboratorio 1981;11 Suppl 1:257-64. [PubMed] [Google Scholar]
Herskovits 1985a {published data only}
- Herskovits E, Famulari A, Tamaroff L, Gonzalez AM, Vazquez A, Dominguez R, et al. Preventive treatment of cerebral transient ischemia: comparative randomised trial of pentoxifylline versus conventional antiaggregants. European Neurology 1985;24:73-81. [DOI] [PubMed] [Google Scholar]
Herskovits 1985b {published data only}
- Herskovits E, Tamaroff L, Famulari A, Dominguez R, Micheli F, Pardal JF, et al. Preventive treatment of TIA. Comparative randomised trial of buflomedil. Journal of Neurology 1985;232 Suppl:237 (Abst.15.30.07). [Google Scholar]
Herskovits 1989 {published data only}
- Herskovits E, Famulari A, Tamaroff L, Dominguez R, Benjamin V, Bauso Toselli L, et al. Comparative trial of pentoxifylline and antiaggregants in patients with transient ischemic attacks (TIA). Clinical Hemorheology 1987;7(3):538 (Abst.318). [Google Scholar]
- Herskovits E, Famulari A, Tamaroff L, Gonzalez AM, Vzquez A, Dominguez R, et al. Comparative study of pentoxifylline versus antiaggregants in patients with transient ischaemic attacks. Acta Neurologica Scandinavica 1989;Suppl 127:31-5. [DOI] [PubMed] [Google Scholar]
JASAP {published data only}
- Uchiyama S, Ikeda Y, Urano Y, Horie Y, Yamaguchi T. The Japanese Aggrenox (Extended-Release Dipyridamole plus Aspirin) Stroke Prevention versus Aspirin Programme (JASAP) study: a randomized, double-blind, controlled trial. Cerebrovascular Diseases 2011;31:601-13. [DOI] [PubMed] [Google Scholar]
Khazaei 2018 {published data only}
- Khazaei M, Ghasemian F, Mazdeh M, Taheri M, Ghafouri-Fard S. Comparison of administration of clopidogrel with aspirin versus aspirin alone in prevention of secondary stroke after transient ischemic attack. Clinical and Translational Medicine 2019;8(1):6. [DOI: 10.1186/s40169-019-0223-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
PATICI 1985 {published data only}
- The American-Canadian Co-Operative Study Group. Persantine Aspirin Trial in cerebral ischemia. Part II: endpoint results. Stroke 1985;16(3):406-15. [DOI: 10.1161/01.STR.16.3.406] [DOI] [PubMed] [Google Scholar]
- The American-Canadian Co-operative Study Group. Persantine Aspirin Trial in cerebral ischemia. Stroke 1983;14(1):99-103. [DOI] [PubMed] [Google Scholar]
- The American-Canadian Co-operative Study Group. Persantine aspirin trial in cerebral ischemia. Part III: risk factors for stroke. Stroke 1986;17:12-8. [DOI] [PubMed] [Google Scholar]
PERFORM {published data only}
- Fox K, Bousser MG, Amarenco P, Chamorro A, Fisher M, Ford I, et al. Heart rate is a prognostic risk factor for myocardial infarction: a post hoc analysis in the PERFORM (Prevention of cerebrovascular and cardiovascular Events of ischemic origin with teRutroban in patients with a history oF ischemic strOke or tRansient ischeMic attack) study population. International Journal of Cardiology 2013;168(4):3500-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
PLATO 2009 {published data only}
PRCASA {published data only}
- Smith W. PRCASA. Preventing Restenosis of Cerebral Arterial Stents with Aggrenox. www.strokecenter.org/trials/clinicalstudies/preventing-restenosis-of-cerebral-arterial-stents-with-aggrenox (accessed 2 April 2009). [CN-00603362]
RE‐SPECT‐ESUS 2014 {published data only}
- Diener HC, Sacco RL, Easton JD, Granger CB, Bernstein RA, Uchiyama S et al. Dabigatran for Prevention of Stroke after Embolic Stroke of Undetermined Source. New England Journal of Medicine 2019;380:1906-1917. [DOI: 10.1056/NEJMoa1813959] [DOI] [PubMed] [Google Scholar]
Rizky 2015 {published data only}
- Rizky S. Comparison of therapeutic effect between combination of aspirin and clopidogrel, clopidogrel alone, aspirin 300 mg alone and aspirin 100 mg alone against functional outcome and recurrence in ischemic stroke patients. Neuroepidemiology 2015;45:333. [Google Scholar]
Sancho Rieger 1984 {published data only}
- Sancho Rieger J, Lopez-Trigo Picho J. Effect of ticlopidine on the prevention of relapses of cerebrovascular ischaemic disease. Medicina Clinica 1984;82:62-4. [CN-00324939] [PubMed]
Satoh 1994 {published data only}
- Satoh K, Yoshida H, Imaizumi TA, Koyama M, Hiramoto M, Takamatsu S. Pyrazolopyridine derivative acts as a novel cyclooxygenase inhibitor: antiplatelet effect in aged patients with ischemic stroke. Journal of the American Geriatrics Society 1994;42(6):639-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
SOCRATES 2014 {published data only}
- Johnston SC, Amarenco P, Albers GW, Denison H, Easton JD, Evans SR et al. Ticagrelor versus Aspirin in Acute Stroke or Transient Ischemic Attack. New England Journal of Medicine 2016 Jul 7;375(1):35-43. [DOI: 10.1056/NEJMoa1603060] [DOI] [PubMed] [Google Scholar]
- NCT01994720. SOCRATES - Acute Stroke Or Transient IsChaemic Attack TReated With Aspirin or Ticagrelor and Patient OutcomES. www.clinicaltrials.gov/ct2/show/NCT01994720 (first received 26 November 2013).
SPS3 {published data only}
- Asdaghi N, Pearce L, Nakajima M, Bazan C, Cermeno F, McClure LA, et al. Clinical correlates of infarct shape and volume in lacunar strokes: the SPS3 Trial. Stroke 2014;45(10):2952-8. [DOI: 10.1161/STROKEAHA.114.005211] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benavente O, Hart R, Palacio S, Pearce L, Roldan A, Talbert R, et al. Secondary prevention of small subcortical strokes (SPS3) pilot trial: final results. Stroke 2003;34:238-322. [Google Scholar]
- Benavente OR, White CL, Pearce L, Pergola P, Roldan A, Benavente MF: SPS3 Investigators. The Secondary Prevention of Small Subcortical Strokes (SPS3) study. International Journal of Stroke 2011;6(2):164-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart RG, Pearce LA, Bakheet MF, Benavente OR, Conwit RA, McClure LA, et al. Predictors of stroke recurrence in patients with recent lacunar stroke and response to interventions according to risk status: Secondary Prevention of Small Subcortical Strokes Trial. Journal of Stroke and Cerebrovascular Diseases 201;23(4):618-24. [DOI: 10.1016/j.jstrokecerebrovasdis.2013.05.021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00059306. Secondary prevention of small subcortical strokes (SPS3). www.clinicaltrials.gov/ct2/show/NCT00059306 (first received 23 August 2017).
- Nakajima M, Pearce LA, Ohara N, Field TS, Bazan C, Anderson DC, et al. Vertebrobasilar ectasia in patients with lacunar stroke: the secondary prevention of small subcortical strokes trial. Journal of Stroke and Cerebrovascular Diseases 2015;24(5):1052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG. Cognitive impairment in lacunar stroke patients. The secondary prevention of small subcortical strokes (SPS3) trial. Lancet Neurology 2014;13(12):1177-85. [Google Scholar]
- SPS3 Investigators, Benavente OR, Hart RG, McClure LA, Szychowski JM, Coffey CS, Szychowski JM, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. New England Journal of Medicine 2012;367(9):815-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stakhovskaya 2001 {published data only}
- Stakhovskaya LV, Pryanikova NA, Kvasova OV, Guseva OI, Buvaltsev VI, Skvortsova VI. Comparative analysis of treatment with either dipyridamol or combination dipyridamol + aspirin in patients selected for secondary stroke prevention. Zhurnal Nevropatologii I Psikhiatrii Imeni S.s. Korsakova 2001;1:66-71. [CN-00421585]
TACS 2000 {published data only}
- Marini C, Rothwell P, Di Orio F, Maragliano E. Efficacy and safety of ticlopidine and aspirin versus aspirin alone in the prevention of vascular events after cerebral ischaemia (as supplied 2000). Data on file.
- The TACS Study Group. Safety and efficacy of ticlopidine and aspirin combination versus aspirin alone in the secondary prevention of stroke. Cerebrovascular Diseases 2006;21 Suppl 4:2 (Abst. 7). [CN-00603332] [Google Scholar]
Terayama 2008 {published data only}
- Terayama Y, Ishibashi Y, Suzuki M. Aspirin and cilostazol vs aspirin alone for the prevention of progressing stroke. International Journal of Stroke 2008;3 Suppl 1:315 (Abst.PO02-196). [Google Scholar]
TOPALS {published data only}
TOSS {published data only}
- Kwon SU, Cho YJ, Koo JS, Bae HJ, Lee YS, Hong KS, et al. Cilostazol prevents the progression of the symptomatic intracranial arterial stenosis: the multicenter double-blind placebo-controlled trial of cilostazol in symptomatic intracranial arterial stenosis. Stroke 2005;6(4):782-6. [DOI] [PubMed] [Google Scholar]
Uchiyama 1989 {published data only}
- Uchiyama S, Sone R, Nagayama T, Shibagaki Y, Kobayashi I, Maruyama S, et al. Combination therapy with low-dose aspirin and ticlopidine in cerebral ischemia. Stroke 1989;20(12):1643-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Uchiyama 1991 {published data only}
- Uchiyama S, Yamazaki M, Maruyama S. Role of platelet-activating factor in aggregation of leukocytes and platelets in cerebral ischemia. Lipids 1991;26(12):1247-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Uchiyama 1992 {published data only}
- Uchiyama S, Maruyama S, Shimizu T, Mannen T. Combination therapy with aspirin and dilazep in cerebral infarction. Cerebrovascular Diseases 1992;2:219. [CN-00243744]
- Uchiyama S, Maruyama S, Shimizu T, Mannen T. Secondary prevention of vascular events by combination therapy with aspirin and dilazep in patients with cerebral infarction. Thrombosis Research 1992;65 Suppl 1:S145 (Abst. P285). [CN-00243746] [Google Scholar]
UMPIRE {published data only}
- Thom S, Poulter N, Field J, Patel A, Prabhakaran D, Stanton A, et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD: the UMPIRE randomized clinical trial. JAMA 2013;310(9):918-29. [DOI: 10.1001/jama.2013.277064] [CN-00869720] [DOI] [PubMed]
Vaya 1988 {published data only}
- Santos M-T, Valles J, Aznar J, Yaya R, Perez-Requejo JL. Effects of dipyridamole, pentoxifylline or dipyridamole plus pentoxifylline on platelet reactivity in patients with ischemic cerebrovascular insufficiency. Thrombosis Research 1993;72:219-29. [CN-00273784] [DOI] [PubMed]
- Vaya A, Aznar J, Villa P, Valles J, Santos MT, Martinez-Sales V. Erthrocyte filterability in patients with cerebrovascular insufficiency. Effect of pentoxifylline and dipyridamole. Preliminary results. Clinical Hemorheology 1988;8:773-8. [Google Scholar]
WASID 1998 {published data only}
- Chimowitz M, Lynn M, Howlett-Smith H, Stern B, Hertzberg VS, Frankel M, et al. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial: final results. Stroke 2004;35(1):235. [CN-00466341] [Google Scholar]
- Famakin BM, Chimowitz MI, Lynn MJ, Stern BJ, George MG. Causes and severity of ischemic stroke in patients with symptomatic intracranial arterial stenosis. Stroke 2009;40(6):1999-2003. [DOI: 10.1161/STROKEAHA.108.546150] [CN-00700207] [DOI] [PMC free article] [PubMed]
- Famakin BM, Lynn MJ, George MG, Chimowitz MI. Causes and severity of stroke in patients with symptomatic intracranial stenosis. Stroke 2006;37(2):642-3. [CN-00603604] [Google Scholar]
- Howlett-Smith HA, Cruz-Flores S, Belden JR, Sauerbeck LR, Levine RL, Stern BJ, et al. Management of intracranial arterial stenosis in a heterogeneous population. Neurology 1998;50:A295-6. [CN-00242878] [Google Scholar]
- Kasner SE, Lynn MJ, Chimowitz MI, Frankel MR, Howlett-Smith H, Hertzberg VS, et al. Warfarin vs aspirin for symptomatic intracranial stenosis: subgroup analyses from WASID. Neurology 2006;67(7):1275-8. [DOI: 10.1212/01.wnl.0000238506.76873.2f] [CN-00568379] [DOI] [PubMed] [Google Scholar]
- Kasner SE, Lynn MJ, Jackson BP, Pullicino PM, Chimowitz MI. Echocardiography in patients with symptomatic intracranial stenosis. Journal of Stroke and Cerebrovascular Diseases 2007;16(5):216-9. [DOI: 10.1016/j.jstrokecerebrovasdis.2007.07.002] [CN-00611981] [DOI] [PMC free article] [PubMed]
- Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ, et al. Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Annals of Neurology 2011;69(6):963-74. [DOI: 10.1002/ana.22354] [CN-00801058] [DOI] [PMC free article] [PubMed]
- Ovbiagele B, Cruz-Flores S, Lynn MJ, Chimowitz MI. Early stroke risk after transient ischemic attack among individuals with symptomatic intracranial artery stenosis. Archives of Neurology 2008;65(6):733-7. [DOI: 10.1001/archneur.65.6.733] [CN-00640206] [DOI] [PubMed]
- Ovbiagele B, Lynn MJ, Saver JL, Chimowitz MI. Elevated white blood cell count and increased risk for stroke and vascular death in patients with symptomatic intracranial disease. Stroke 2006;37(2):626. [CN-00603937]
- Ovbiagele B, Lynn MJ, Saver JL, Chimowitz MI. Leukocyte count and vascular risk in symptomatic intracranial atherosclerosis. Cerebrovascular Diseases 2007;24(2-3):283-8. [DOI: 10.1159/000105681] [CN-00610782] [DOI] [PubMed]
- Waddy S, Cotsonis G, Lynn M, Frankel M, Chaturvedi S, Chimowitz M. Racial differences in risk factor management in the Warfarin vs Aspirin for Symptomatic Intracranial Disease Trial. Stroke 2006;37(2):638. [CN-00604139]
- Williams JE, Chimowitz MI, Cotsonis GA, Lynn MJ, Waddy SP. Gender differences in outcomes among patients with symptomatic intracranial arterial stenosis. Stroke 2007;38(7):2055-62. [DOI: 10.1161/STROKEAHA.107.482240] [CN-00589395] [DOI] [PubMed]
WOEST 2013 {published data only}
- Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, Smet BJ, Herrman JP, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013;381(9872):1107-15. [DOI: 10.1016/S0140-6736(12)62177-1] [CN-00853575] [DOI] [PubMed]
Zuo 2017 {published data only}
- Zuo F-T, Liu H, Wu H-J, Su N, Liu J-Q, Dong A-Q. The effectiveness and safety of dual antiplatelet therapy in ischemic cerebrovascular disease with intracranial and extracranial arteriostenosis in Chinese patients: a randomized and controlled trial. Medicine 2017;96(1):e5497. [DOI: 10.1097/MD.0000000000005497] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
THALES 2018 {published data only}
- Johnston SC, Amarenco P, Denison H, Evans SR, Himmelmann A, James S, et al. The THALES (acute stroke or transient ischaemic attack treated with ticagrelor and aspirin for prevention of stroke and death) trial design. European Stroke Journal 2018;3 Suppl 1:596. [DOI: 10.1177/2396987318773967] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03354429. Acute STroke or Transient IscHaemic Attack Treated With TicAgreLor and ASA for PrEvention of Stroke and Death. www.clinicaltrials.gov/ct2/show/NCT03354429 (first received 4 September 2018).
Additional references
Bamford 1990
- Bamford J, Dennis M, Sandercock P, Burn J, Warlow C. The frequency, causes and timing of death within 30 days of a first stroke: the Oxfordshire Community Stroke Project. Journal of Neurology, Neurosurgery and Psychiatry 1990;53(10):824-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Born 2006
- Born G, Patrono C. Antiplatelet drugs. British Journal of Pharmacology 2006;147 Suppl 1:241-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2000
- Chen ZM, Sandercock P, Pan HC, Counsell C, Collins R, Liu LS, et al. Indications for early aspirin use in acute ischemic stroke: a combined analysis of 40,000 randomized patients from the Chinese Acute Stroke Trial and the International Stroke Trial. On behalf of the CAST and IST Collaborative Groups. Stroke 2000;31(6):1240-9. [DOI] [PubMed] [Google Scholar]
Coull 2004
- Coull AJ, Lovett JK, Rothwell PM. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ 2004;328(7435):326. [DOI] [PMC free article] [PubMed] [Google Scholar]
d'Esterre 2010
- d'Esterre CD, Lee TY. Effect of dipyridamole during acute stroke: exploring antithrombosis and neuroprotective benefits. Annals of the New York Academy of Sciences 2010;1207:71-5. [DOI] [PubMed] [Google Scholar]
D'Sa 1999
- D'Sa S, Machin SJ. Clopidogrel: a novel antiplatelet agent. Hospital Medicine 1999;60(5):362-3. [DOI] [PubMed] [Google Scholar]
EXPRESS
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurology 2009;8(3):235-43. [DOI] [PubMed] [Google Scholar]
Geeganage 2012
- Geeganage CM, Diener HC, Algra A, Chen C, Topol EJ, Dengler R, et al. Dual or mono antiplatelet therapy for patients with acute ischemic stroke or transient ischemic attack: systematic review and meta-analysis of randomized controlled trials. Stroke 2012;43(4):1058-66. [PMID: ] [DOI] [PubMed] [Google Scholar]
Goldstein 2006
- Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke 2006;37(6):1583-633. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Lopez 2006
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367(9524):1747-57. [DOI] [PubMed] [Google Scholar]
Markus 2005
- Markus HS, Droste DW, Kaps M, Larrue V, Lees KR, Siebler M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation 2005;111(17):2233-40. [DOI] [PubMed] [Google Scholar]
Minami 1997
- Minami N, Suzuki Y, Yamamoto M, Kihira H, Imai E, Wada H, et al. Inhibition of shear stress-induced platelet aggregation by cilostazol, a specific inhibitor of cGMP-inhibited phosphodiesterase, in vitro and ex vivo. Life Sciences 1997;61(25):383-9. [DOI] [PubMed] [Google Scholar]
Patrono 1994
- Patrono C. Aspirin as an antiplatelet drug. New England Journal of Medicine 1994;330(18):1287-94. [DOI] [PubMed] [Google Scholar]
Serebruany 2010
- Serebruany V, Sani Y, Eisert C, Schevchuck A, Fong A, Hanley D. Effects of Aggrenox and aspirin on plasma endothelial nitric oxide synthase and oxidised low-density lipoproteins in patients after ischaemic stroke. The AGgrenox versus Aspirin Therapy Evaluation (AGATE) biomarker substudy. Thrombosis and Haemostasis 2010;105(1):81-7. [DOI] [PubMed] [Google Scholar]
Wong 2010
- Wong KS, Chen C, Fu J, Chang HM, Suwanwela NC, Huang YN, et al. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. Lancet Neurology 2010;9(5):489-97. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kamal 2012
- Kamal AK, Siddiqi SA, Naqvi I, Khan M, Majeed F, Ahmed B. Multiple versus one or more antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack. Cochrane Database of Systematic Reviews 2012, Issue 3. Art. No: CD009716. [DOI: 10.1002/14651858.CD009716] [DOI] [PMC free article] [PubMed] [Google Scholar]


