Objectives:
To determine the nationwide demographics and hospital mortality of patients with severe acute respiratory syndrome coronavirus 2 infection requiring admission to the ICU for coronavirus disease 2019 in Iceland.
Design:
Prospective observational study.
Setting:
All ICUs in Iceland (Landspitali University Hospital and Akureyri Regional Hospital).
Patients:
All patients admitted to the ICU for management of coronavirus disease 2019 between March 14, 2020, and April 13, 2020, with follow-up through May 5, 2020.
Interventions:
None.
Measurements and Main Results:
A total of 27 patients were admitted to the ICU for coronavirus disease 2019 out of 1,788 severe acute respiratory syndrome coronavirus 2 positive cases, rendering an overall admission ratio of 1.5% (95% CI, 1.0–2.2%). The population rate of ICU admission for coronavirus disease 2019 was 7.4 (95% CI, 4.9–10.8) admissions per 100,000 individuals. The hospital mortality of patients admitted to the ICU was 15% (95% CI, 4–34%), and the mortality of patients receiving mechanical ventilation was 19% (95% CI, 4–46%).
Conclusions:
We report a lower overall ratio of ICU admissions for coronavirus disease 2019 among severe acute respiratory syndrome coronavirus 2 positive patients and a lower hospital mortality for patients treated in the ICU for coronavirus disease 2019 compared with initial reports from Italy and China. Our results could be explained by the early adoption of widespread testing and a successful national response to the pandemic.
Keywords: coronavirus disease 2019, incidence, intensive care unit, mortality, severe acute respiratory syndrome coronavirus 2
With the onset of coronavirus disease 2019 (COVID-19) epidemic, there was a global concern that the number of patients requiring ICU treatment would greatly surpass the ICU capacity. This was based on initial reports suggesting that up to 5–12% of patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection required intensive care (1, 2). It is very likely that this ratio was heavily influenced by the availability of clinical testing for SARS-CoV-2. Additionally, the reported outcomes of patients admitted to the ICU for management for COVID-19 have varied substantially, with reports of up to 50–78% mortality among those admitted to the ICU (3–5). However, a substantial number of patients had not completed their ICU course at the time of reporting.
The population of Iceland was 364,134 on January 1, 2020. The first SARS-CoV-2 infection was confirmed on February 28, 2020, resulting in the launch of extensive population health measures. This included quarantine of infected patients and identified contacts, social distancing, and a gathering ban. Additionally, targeted testing among symptomatic individuals and extensive population screening of individuals from society with no or mild symptoms was initiated (6). Landspitali University Hospital established a specialized outpatient clinic to oversee the follow-up of all SARS-CoV-2 positive patients in Iceland, with frequent follow-up phone-calls to patients and immediate access outpatient visits for those deteriorating at home. Patients were subsequently referred for inpatient management as needed, including intensive care.
During normal conditions, the ICU capacity in Iceland is 16 beds (4.3 beds/100,000 population), compared with an average of 9.5 beds/100,000 population in Europe (7). Plans were developed for a scaled increase in the ICU capacity up to a maximum of 45 ICU beds. This was done by postponing all elective surgeries and converting postoperative recovery rooms into ICU wards staffed by nurses with prior ICU experience transferred from other wards. All patients were treated by critical care physicians and nurses in ICU environment specified for SARS-CoV-2-positive patients, in collaboration with consultants from infectious diseases and pulmonology.
Here we describe the nationwide incidence of ICU admissions for COVID-19 in a nation with an early adoption of widespread targeted testing and population screening. In addition, we describe the initial outcomes of patients with COVID-19 that required ICU admission during the initial peak of the pandemic.
MATERIALS AND METHODS
This prospective cohort study included all patients with confirmed SARS-CoV-2 managed in the ICUs of Landspitali University Hospital and Akureyri Hospital, the only two hospitals offering ICU care in Iceland. In general, all patients with a progressive hypoxic respiratory failure secondary to COVID-19 were evaluated for a potential ICU admission by the on-call critical care physician following consultation with internal or emergency medicine physicians. Patients considered at high risk of requiring mechanical ventilation were admitted to the ICU, after weighing the benefits of ICU admission with underlying comorbidities and frailty.
Clinical data were prospectively collected using Research electronic data capture (REDCap), a secure, web-based data capture platform. The primary outcomes were the incidence of ICU admission for COVID-19 following SARS-CoV-2 diagnosis and the incidence of all-cause hospital mortality among those patients admitted to the ICU for COVID-19. In addition to descriptive statistics, incidence and survival ratios are reported with 95% CI using the Clopper-Pearson exact method with the “binom” package. All statistics and image processing were performed in R, Version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria), using RStudio, Version 1.1.423 (RStudio, Boston, MA). The study was approved by the National Bioethics Committee (VSN-20-071), waiving individual consent.
RESULTS
Out of 51,622 individuals tested on May 5, 2020, 18,357 (35.6%) were tested for symptoms suggestive of SARS-CoV-2 and the remainder were tested as a part of population screening. Of all tested, 1,799 (3.5%; 95% CI, 3.3–3.6%) were positive for SARS-CoV-2, and of those, 118 (6.7%, 95% CI 5.5–7.8%) were admitted to the hospital. The first patient was admitted to the ICU on March 14, 2020, and the last patient was admitted on April 13, 2020. In total, 27 out of 1,799 (1.5%; 95% CI, 1.0–2.2%) SARS-CoV-2 positive individuals were admitted to the ICU due to COVID-19. Two patients admitted to the ICU for other indications (hemorrhagic shock and urosepsis) were positive for SARS-CoV-2 but were excluded from further analysis as they were minimally symptomatic or had recovered from COVID-19. The population incidence of an ICU admission for COVID-19 was, therefore, 7.4 (95% CI, 4.9–10.8) admissions per 100,000 individuals.
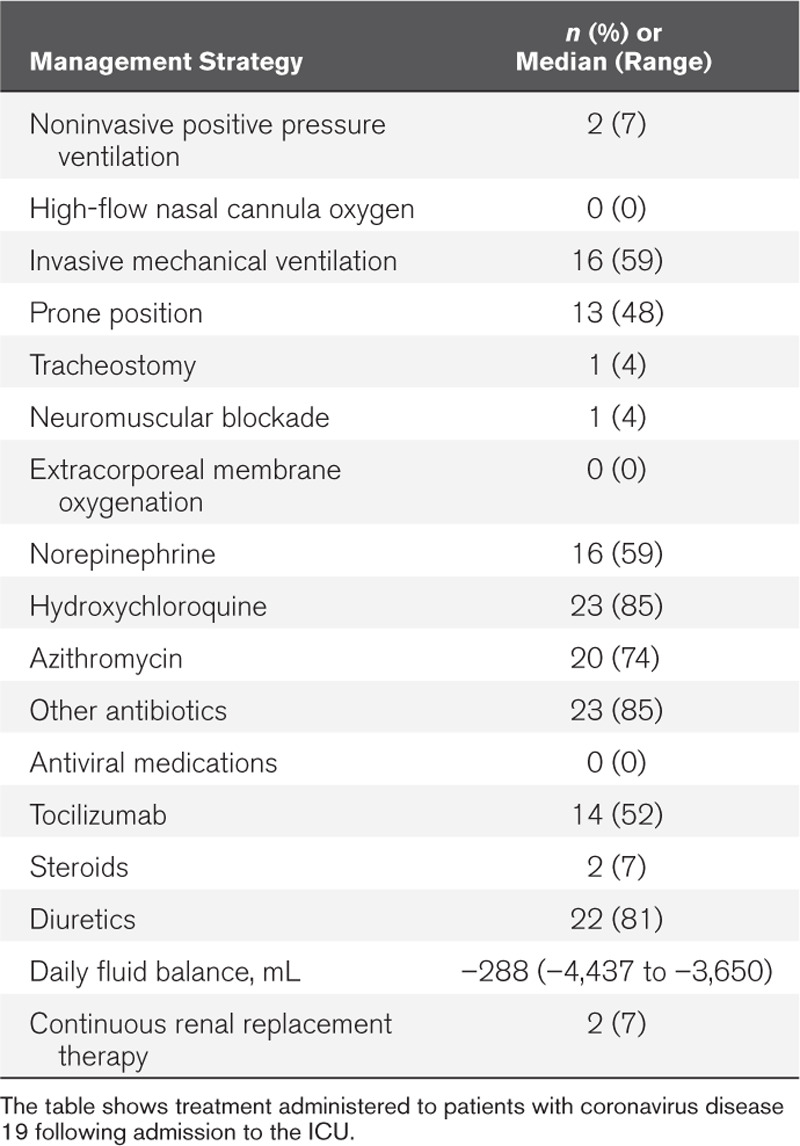
The clinical course for all 27 patients is shown in Figure 1, and patient characteristics, laboratory profile, and ward management prior to admission are described in Table 1. Most patients were admitted to the ICU due to hypoxic respiratory failure after clinical deterioration on the general ward. Of the 27 patients admitted to the ICU, 16 required mechanical ventilation, and prone positioning and diuretics were frequently used (Table 2).
Figure 1.
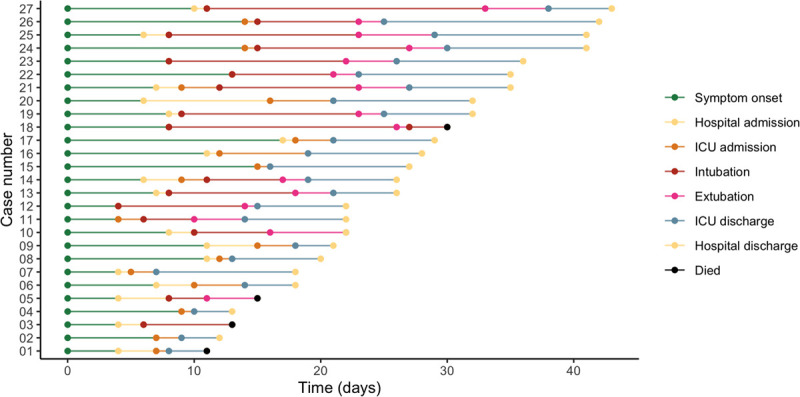
The clinical course of all patients admitted to the ICU in Iceland for coronavirus disease 2019. Shown is the timeline for each patient from symptom onset to date of death or discharge from the hospital. The case number reflects the duration of disease from shortest to longest.
Table 1.
Patient Characteristics

Table 2.
ICU Management
The last patient was discharged from the ICU on April 28, 2020, and on final follow-up, May 6, 2020, four patients had died, but the other 23 patients were all discharged from both the ICU and the hospital. Out of 16 patients receiving invasive mechanical ventilation, three died, but the other 13 had been successfully liberated from mechanical ventilation. The hospital mortality of all patients who required ICU admission due to COVID-19 was, therefore, four of 27 (15%, 95% CI, 4–34%), and the mortality of all patients who required mechanical ventilation was three of 16 (19%; 95% CI, 4–46%).
DISCUSSION
When determining the ratio of ICU admissions among COVID-19 patients, it is of paramount importance to eliminate bias due to tertiary care referrals or restricted ability to screen for SARS-CoV-2. We found that in our cohort, 1.5% of all patients with a confirmed SARS-CoV-2 required ICU for COVID-19. This estimate is substantially lower than initial published estimates from Italy and China, predicting that around 5–7% of positive patients would require ICU (1, 2). The population screening performed in Iceland indicated a low prevalence among asymptomatic individuals at the peak of the pandemic, with only 0.6% of randomly screened individuals positive for SARS-CoV-2 compared with 13.3% of patients with symptoms suggestive of COVID-19 (6). It is, therefore, likely that our reported rate differs from prior reports due to extensive testing of individuals that likely captures more cases, including patients with milder symptoms.
Our mortality ratio of 15% compares favorably to initial population reports describing up to 50–78% mortality among patients treated for COVID-19 in the ICU (3–5). There could be several explanations for this, including better overall health of the admitted patients as well as nationwide approval and participation in population health measures resulting reduced incidence of COVID-19. This contributed to a pandemic that was managed within the capacity of the entire healthcare system, including the ICU. The centralized follow-up of all SARS-CoV-2 positive patients provided frequent contact with patients at home and an early evaluation of patients deteriorating at home, including an evaluation for ICU admission. This strategy can potentially both decrease the chance of an ICU admission as well as improve the ICU outcomes. Additionally, a careful multidisciplinary assessment weighing the benefit of ICU care of each individual against disease status and the overall burden of comorbidity and frailty was performed, and this can result in fewer ICU admissions and better outcomes. Among limitations is the small size of the Icelandic population that is genetically homogenous and geographically isolated. This might render our findings less applicable to other populations.
We hope that in addition to assisting with surge planning for COVID-19, our findings will encourage other nationwide reports of ICU outcomes. This would allow a dialogue on how different response strategies to COVID-19 are associated with ICU outcomes, with the hope that the response to future pandemics could be improved.
Footnotes
Drs. Kristinsson, Blondal, Thormar, Kristjansson, Karason, Sigvaldason, and Sigurdsson participated in study design. Drs. Kristinsson, Kristinsdottir, Blondal, and Sigurdsson participated in data acquisition. Drs. Kristinsson, Kristinsdottir, and Sigurdsson participated in analysis of data and drafting of article. Dr. Sigurdsson takes responsibility for the integrity of the work as a whole. All authors participated in critical revision of article.
Dr. Kristjansson disclosed off-label product use of tocilizumab in cytokine storm. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA 2020; 323:1545–1546 [DOI] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323:1239–1242 [DOI] [PubMed] [Google Scholar]
- 3.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med 2020; 382:2012–2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med 2020; 8:475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395:1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med 2020; 382:2302–2315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhodes A, Ferdinande P, Flaatten H, et al. The variability of critical care bed numbers in Europe. Intensive Care Med 2012; 38:1647–1653 [DOI] [PubMed] [Google Scholar]


