Abstract
Purpose
The severe acute respiratory syndrome coronavirus-2 and its associated infection known as COVID-19 have resulted in a global pandemic. Ocular manifestations of COVID-19 are nonspecific and include hyperemia, chemosis, epiphora, secretions, and eyelid edema. There is a paucity in the literature regarding COVID-19 related inflammatory syndromes which may also include ocular manifestations.
Observations
In pediatric patients, conjunctivitis has been recently reported in association with a multisystem inflammatory condition related to COVID-19 that shares features with Kawasaki disease and toxic shock syndrome. We describe the clinical course of an adult patient with symptoms and signs consistent with a Kawasaki-like syndrome.
Conclusions and Importance
To our knowledge, this report may be the first case of a Kawasaki-like syndrome in an adult with COVID-19 infection.
Keywords: COVID-19, Conjunctivitis, Kawasaki disease, Ocular manifestations of Kawasaki disease
1. Introduction
The severe acute respiratory syndrome coronavirus-2 (Sars-Cov-2) and its associated infection known as COVID-19 have resulted in a global pandemic, accounting for over 4 million cases and more than 300,000 deaths worldwide as of the writing of this article.1 New York City was one of the epicenters of the pandemic, with nearly 200,000 confirmed cases as of May 16, 2020 and thus it has been an ideal location to study the clinical course associated with the viral infection.2
Several studies have described the clinical manifestations associated with COVID-19 infections. The ocular manifestations are nonspecific and can include signs related to conjunctivitis such as hyperemia, chemosis, epiphora, secretions, and eyelid edema.3, 4, 5 Still, some of these signs may relate to other factors such as immunological responses, external trauma, or exposure keratopathy especially in the intensive care unit (ICU) setting. A recent meta-analysis of 1167 patients found that 1.1% of patients had conjunctivitis at the time of admission, with 3% in patients showing severe systemic manifestations, and 0.7% in those with non-severe cases.3 The authors found a statistically significant difference between these two categories, where patients with severe infections were 3.4 times more likely to have conjunctivitis.6 In fact, in some cases conjunctivitis may be the only presenting sign of COVID-19.7 Still, authors using RT-PCR testing found that only 5.2% of patients were positive for SARS-CoV-2 when using conjunctival samples.3 Similarly, a meta-analysis demonstrated that 4% of conjunctival PCR samples were positive for infection.6 Other ophthalmic symptoms of COVID-19 infection include dry eye, blurry vision, and foreign body sensation.8
In pediatric patients, conjunctivitis has been reported in association with a COVID-19 related multisystem inflammatory condition with features similar to Kawasaki disease and toxic shock syndrome.9, 10, 11, 12 On April 27, 2020 the Pediatric Intensive Care Society alerted clinicians about this type of severe COVID-19 infection in children, citing a case report of a 6-month-old-infant.12 The patient was admitted and diagnosed with classic Kawasaki disease and tested positive for COVID-19, treated per guidelines with intravenous immunoglobulin (IVIG) and high-dose aspirin, and subsequently recovered.12
In New York City, the Health Department identified 15 patients aged 2–15 years hospitalized in pediatric ICUs from April 17 to May 1, 2020 with illnesses compatible with typical Kawasaki disease, incomplete Kawasaki disease, and/or shock.13 More recently on May 15, 2020 the World Health Organization (WHO) published a scientific brief summarizing the current knowledge related to these pediatric patients and a preliminary case definition. The WHO definition for this COVID-19 Kawasaki-like syndrome differs slightly from the commonly used criteria for Kawasaki disease related to children with other viral infections and can be found in Table 1, along with a comparison of the classic criteria. The definition includes children and adolescents below the age of 19 with several symptoms and signs and a positive COVID-19 test or likely contact with COVID-19 positive individuals.10
Table 1.
Diagnostic criteria. Comparison of the WHO definition for COVID-19 Kawasaki-like syndrome to the classic diagnostic criteria used for Kawasaki disease related to other viral infections.
| World Health Organization (WHO) Preliminary Case Definition of COVID-19 Kawasaki Syndrome in Children and Adolescents14 | Classic Criteria for Kawasaki Disease Associated with Other Viral Infections24 | |
|---|---|---|
| Symptoms |
|
|
| Signs | At least 2 of the following:
|
At least 4 of the following clinical signs, not explained by another disease process:
|
2. Case report
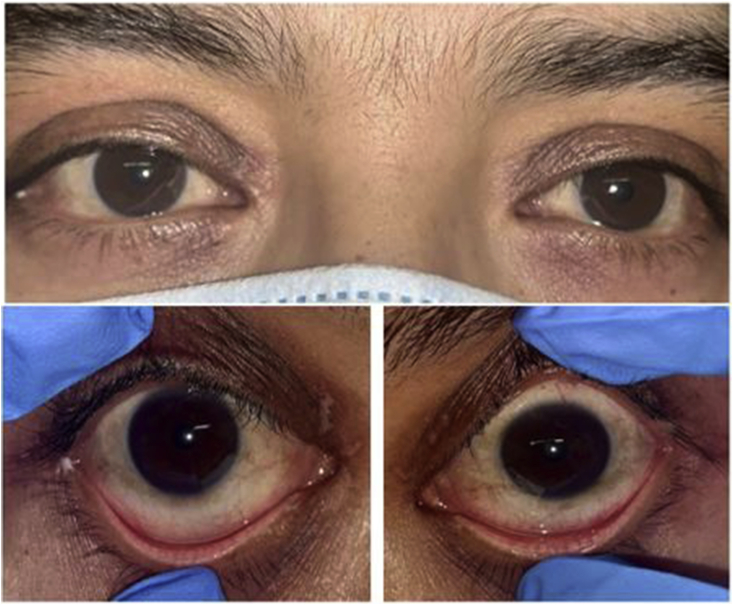
Herein, we describe the clinical course of an adult patient with COVID-19 and symptoms and signs consistent with a Kawasaki-like syndrome similar to that recently reported in pediatric patients. To our knowledge this report may be the first published case of a COVID-19 related Kawasaki-like syndrome in an adult patient. On May 5, 2020, a forty-five-year-old otherwise healthy male without past ocular history presented with five days of fever, sore throat, diarrhea, eye redness, eyelid swelling, and a diffuse rash including bilateral upper and lower eyelids. On admission he was found to be COVID-19 positive on PCR testing with lymphopenia, severely elevated inflammatory markers including ferritin, CRP, ESR, and D-dimer, and elevated troponin. A transthoracic echocardiogram demonstrated global hypokinesis and a reduced ejection fraction of 40% and CT imaging showed unilateral cervical lymphadenopathy with a lymph node measuring 1.8 cm. In addition, he reported photophobia and swollen eyelids that began at the same time as the aforementioned symptoms. He denied other vision changes including blurry vision and eye pain. External photos exhibiting his periorbital rash involving the upper and lower eyelids, bilateral diffuse conjunctival hyperemia and trace chemosis consistent with non-exudative conjunctivitis, and perioral mucosal involvement are shown in Fig. 1. On exam, uncorrected near visual acuity was 20/20 bilaterally with bilateral superficial punctate keratitis, symmetric anterior chamber (AC) inflammation with 10–15 cells per high power field, and normal intraocular pressure. Dilated fundus exam was notable only for one small peripheral cotton wool spot in each eye. Given the patient's clinical status including the inpatient setting and symptomatic COVID-19 positive status, additional imaging including fundus photos or OCT could not be obtained. The lack of additional ophthalmic testing could be a limitation of this case report.
Fig. 1.
Initial presentation.
External photos exhibiting the patient's periorbital rash involving the upper and lower eyelids, bilateral diffuse conjunctival hyperemia consistent with non-exudative conjunctivitis, and perioral mucosal changes.
A multidisciplinary effort involving dermatology, rheumatology, infectious disease, cardiology, and ophthalmology teams collaborated on the patient's care. Punch biopsy of his erythema multiforme-like rash (which has been seen in pediatric Kawasaki disease14,15 and COVID-19 patients)16 showed sparse superficial perivascular infiltrate of lymphocytes with neutrophils and scattered eosinophils, suggestive of toxic shock syndrome. In this case, however, the patient did not demonstrate other shock-like signs such as hypotension. He continued to be febrile during the admission. Testing for myositis, especially given the heliotrope-appearing rash and concern for possible dermatomyositis, including anti-Jo, anti-Ro, and anti-La testing was negative. HIV testing was negative. An exhaustive rheumatologic workup including ANA, RF, anti-CCP, anti-Smith, anti-dsDNA, p-ANCA/MPO, c-ANCA/PR3 was also negative. Blood cultures were negative.
Our patient showed many symptoms and signs consistent with previously published ocular manifestations of Kawasaki disease associated with other viral infections.17, 18, 19, 20, 21 One of these studies, a review of 41 patients, found that conjunctival injection (78%) and AC reaction (19.5%) were the most common ocular features.17 Furthermore, our patient not only exhibited sufficient criteria for the aforementioned WHO definition for COVID-19 related Kawasaki syndrome, but also the common criteria for Kawasaki disease associated with other viral infections, including persistent fevers, non-exudative conjunctivitis, unilateral cervical adenopathy greater than 1.5 cm, and inflammation of the oral mucosa.22,23
Although this patient tested negative for HIV, prior literature has demonstrated a Kawasaki-like syndrome in HIV positive patients. One study showed that HIV infection can predispose a patient to this syndrome and these cases were particularly associated with severe immunosuppression and a high viral load.24
We treated our patient with ophthalmic lubricating therapy in addition to prednisolone acetate 1% eye drops four times daily for his photophobia in the setting of AC inflammation. He was treated systemically with IVIG and an IL-6 inhibitor (tocilizumab) in addition to using a topical triamcinolone ointment for his diffuse rash. His fever resolved and he clinically improved with decreasing inflammatory markers. On repeat ophthalmic examination two weeks later, his vision was stable and his periorbital rash, ocular surface disease, and conjunctival injection all improved (Fig. 2). His AC reaction had also resolved. We tapered his topical steroid and continued to monitor his exam.
Fig. 2.
Follow-up examination.
External photos exhibiting the patient's improved clinical signs including minimal bilateral periorbital rash and conjunctival hyperemia.
3. Discussion
This case highlights a new manifestation of Kawasaki-like disease in an adult with COVID-19 infection who had numerous anterior segment findings. This coronavirus represents a new clinical entity, and we are learning about its many varied presentations almost daily. The new description of Kawasaki type disease associated with COVID-19 in the pediatric population over the past several months certainly has very serious, and in rare cases, life threatening implications. To our knowledge, this report may be the first case of a Kawasaki-like syndrome in an adult with COVID-19 infection.
Patient consent
Written consent was obtained from the patient in order to publish this case report.
Funding
Supported in part by an unrestricted grant from Research to Prevent Blindness to New York University Langone Health Department of Ophthalmology.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of competing interest
The following authors have no financial disclosures: AKL, SAP, DRL.
References
- 1.World Health Organization . 2020. Coronavirus Disease 2019 (COVID-19) Situation Report- 77. [Google Scholar]
- 2.NYC Department of Health . 2020. COVID-19: Data. [Google Scholar]
- 3.Wu P., Duan F., Luo C. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in hubei province, China. JAMA Ophthalmol. 2020 doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daruich A., Martin D., Bremond-Gignac D. Ocular manifestation as first sign of Coronavirus Disease 2019 (COVID-19): interest of telemedicine during the pandemic context. J Fr Ophtalmol. 2020;43(5):389–391. doi: 10.1016/j.jfo.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu P., Liang L., Chen C., Nie S. A child confirmed COVID-19 with only symptoms of conjunctivitis and eyelid dermatitis. Graefes Arch Clin Exp Ophthalmol. 2020:1–2. doi: 10.1007/s00417-020-04708-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loffredo L., Pacella F., Pacella E., Tiscione G., Oliva A., Violi F. Conjunctivitis and COVID-19: a meta-analysis. J Med Virol. 2020 doi: 10.1002/jmv.25938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scalinci S.Z., Trovato Battagliola E. Conjunctivitis can be the only presenting sign and symptom of COVID-19. ID Cases. 2020;20 doi: 10.1016/j.idcr.2020.e00774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen L., Deng C., Chen X. medRxiv; 2020. Ocular Manifestations and Clinical Characteristics of 534 Cases of COVID-19 in China: A Cross-Sectional Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeBiasi R.L., Song X., Delaney M. Severe COVID-19 in children and young adults in the Washington, DC metropolitan region. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . 2020. Multisystem Inflammatory Syndrome in Children and Adolescents Temporally Related to COVID-19. [Google Scholar]
- 11.Jones V.G., Mills M., Suarez D. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020;10(6):537–540. doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- 12.Pediatric Intensive Care Society . 2020. PICS Statement: Increased Number of Reported Cases of Novel Presentation of Multisystem Inflammatory Disease. [Google Scholar]
- 13.NYC Health Department . 2020. Pediatric Multi-System Inflammatory Syndrome Potentially Associated with COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jimenez-Cauhe J., Ortega-Quijano D., Carretero-Barrio I. Erythema multiforme-like eruption in patients with COVID-19 infection: clinical and histological findings. Clin Exp Dermatol. 2020 doi: 10.1111/ced.14281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shwe S., Kraus C.N., Linden K.G., Rojek N.W. Erythema multiforme in a child with Kawasaki disease. JAAD Case Rep. 2019;5(4):386–388. doi: 10.1016/j.jdcr.2019.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang Y.-H., Lee M., Jung J.W., Ahn J., Yang H.S., Kook K.H. Ocular manifestation of Kawasaki disease. J AAOPS. 2007;11(1):85–86. [Google Scholar]
- 17.Ohno S., Miyajima T., Higuchi M. Ocular manifestations of Kawasaki's disease (mucocutaneous lymph node syndrome) Am J Ophthalmol. 1982;93(6):713–717. doi: 10.1016/0002-9394(82)90465-2. [DOI] [PubMed] [Google Scholar]
- 18.Jacob J.L., Polomeno R.C., Chad Z., Lapointe N. Ocular manifestations of Kawasaki disease (mucocutaneous lymph node syndrome) Can J Ophthalmol. 1982;17(5):199–202. [PubMed] [Google Scholar]
- 19.Puglise J.V., Rao N.A., Weiss R.A., Phillips T.M., Marak G.E., Jr. Ocular features of Kawasaki's disease. Arch Opthalmol. 1982;100(7):1101–1103. doi: 10.1001/archopht.1982.01030040079014. [DOI] [PubMed] [Google Scholar]
- 20.Kim M., Kim S.Y. Anterior uveitis associated with Kawasaki disease-and the ophthalmologist's role. J Korean Ophthalmol Soc. 2016;57(2):296–301. [Google Scholar]
- 21.Wolff A.E., Hansen K.E., Zakowski L. Acute Kawasaki disease: not just for kids. J Gen Intern Med. 2007;22(5):681–684. doi: 10.1007/s11606-006-0100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rozo J.C., Jefferies J.L., Eidem B.W., Cook P.J. Kawasaki disease in the adult: a case report and review of the literature. Tex Heart Inst J. 2004;31(2):160–164. [PMC free article] [PubMed] [Google Scholar]
- 23.Son M.B., Sundel R.P. Chapter 35 - Kawasaki disease. In: Petty R.E., Laxer R.M., Lindsley C.B., Wedderburn L.R., editors. Textbook of Pediatric Rheumatology. seventh ed. W.B. Saunders; Philadelphia: 2016. pp. 467–483. e466. [Google Scholar]
- 24.Stankovic K., Miailhes P., Bessis D., Ferry T., Broussolle C., Sève P. Kawasaki-like syndromes in HIV-infected adults. J Infection. 2007;55(6):488–494. doi: 10.1016/j.jinf.2007.09.005. [DOI] [PubMed] [Google Scholar]