Dear Sir,
Hidradenitis suppurativa (HS) is a chronic, debilitating disease where even surgery, which is considered the ‘gold standard’ treatment, often has poor outcomes. With the current COVID-19 pandemic, the authors believe it important to make patients aware of the likely surgical outcomes of non-essential surgery. The authors’ aim is to present the complication rates, healing times and risk of recurrence of HS surgery from a London hospital in order to better consent HS patients accurately and offer some comparison with similar studies from other countries.
A retrospective analysis was conducted of the 53 HS patients treated by the Plastic Surgery department in a London teaching hospital over a 24-month period from January 2017 to December 2018. The average age of patients at the time of the study was 36 years old (range 15–69 years old) with 36 of the patients being female and 17 male. The number of sites affected by HS ranged from 1 to 9, with the mean number of sites affected being 3.4. The average number of operations per patient was 2.7.
The most common type of initial operation was excision and primary closure, as seen in 57% (30/53) of the patients. Other types of operation used for the first surgery for HS were excision and local flap (26%; 14/53), excision and VAC (8%; 4/53), excision and skin graft (6%; 3/53), and incision and drainage (4%; 2/53).
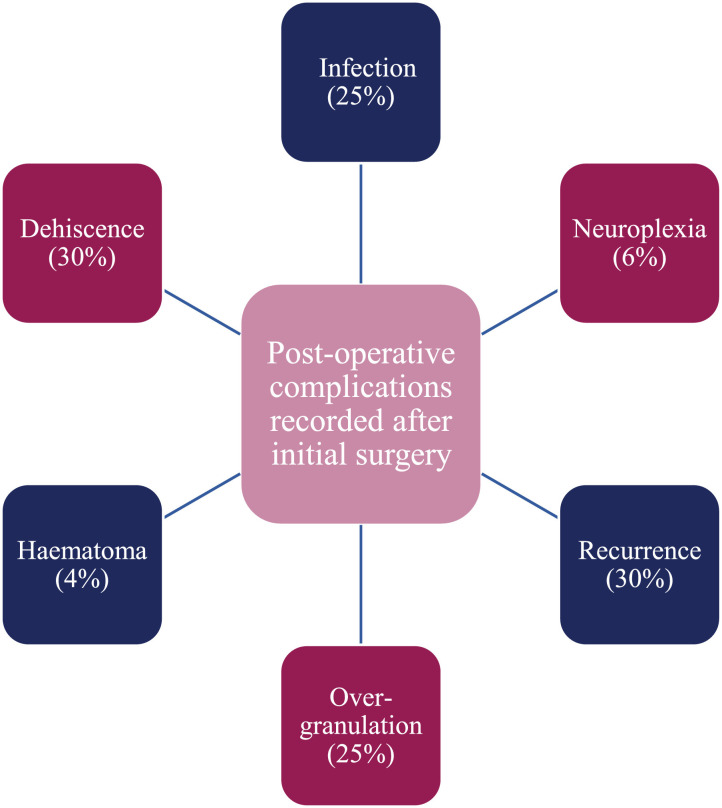
Following surgery, only 24 (45%) of the patients proceeded to primary wound healing without complications. The overall average time to wound healing, including time for complications that healed without further surgery, was 8 weeks, with the longest healing time taking up to 4 months. Post-operative complications recorded after initial surgery included wound dehiscence (30%), recurrence (30%), over-granulation (25%), infection (25%), neuropraxia (6%), and haematoma (4%) [Figure 1 ].
Figure 1.
Post-operative outcomes after initial surgery.
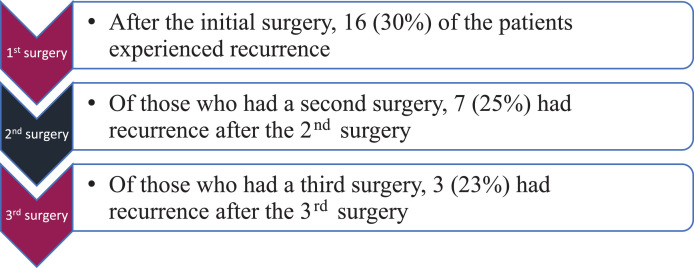
After initial surgery, 28 patients proceeded to have a second operation. Twenty of these second operations were at the same site as the initial procedure. Indications for a second operation at the same site included debridement (8/20), haematoma (2/20), revision (4/20), and recurrence (6/20). After the second operation, 16 (57%) of the patients progressed to wound healing without complications, and the average time for healing was 10 weeks for all who healed without needing an additional surgery at the same site. The recurrence rate was 25% (7/28) after a second operation. Of the 13 patients who had three or more surgeries for HS, 3 (23%) experienced recurrence after their third operation [Figure 2 ].
Figure 2.
Recurrence rates following first, second and third surgery.
Despite the current recurrence rate seeming high at 30% after the initial surgery and 25% after the second surgery, these results are in keeping with similar studies from other countries. A retrospective cohort study in France by Fertitta et al.1, of 75 patients, found a recurrence rate of 35% across a total of 115 surgeries for HS. A study by Ovadja et al.2 in The Netherlands, of 107 surgical interventions for HS for 54 patients, found a 32% recurrence rate after a median 30-month follow-up period. The 8 week healing time of the current study is also comparable to the 6 weeks that Ovadja et al.2 reported and the 3.3 months reported by Fertitta et al.1 A systematic review by Bouazzi et al.3 found that, of 54 relevant articles on post-operative HS complications and recurrences, there was an overall mean complication rate of 24% and a mean recurrence rate of 20%. Due to the high rates of post-surgical recurrence for HS in the literature, a retrospective review of surgical treatment of HS4 concluded that recurrence of HS should be viewed as a feature of the disease that can be anticipated and managed rather than a failure of surgical treatment.
Significant comorbidities have been associated with non-curative surgery for HS5. In the current study, of the 19 patients with 3 or more comorbidities, 10 (53%) had more than one surgery, which was equivalent to the overall cohort (where 53% of the patients had more than one surgery). However, of the 19 patients with 3 or more comorbidities, 63% (12/19) experienced complications after their initial surgery, compared to just 55% (29/53) of the overall cohort. The complications experienced by the patients with 3 or more comorbidities after initial surgery included infection (7/19), recurrence (6/19), overgranulation (1/19), haematoma (1/19) and wound dehiscence (1/19). The addition of the data from the current study to these other studies should therefore hopefully allow clinicians to feel more confident in sharing the necessary information for consenting patients for HS surgery.
The authors conclude that more conservative treatment options for HS should be maximised prior to considering surgery and that patients should only consider surgery once non-operative medical treatment options, including antibiotic courses and lifestyle modification, have been exhausted.
Declaration of Competing Interest
None to declare.
Acknowledgements
N/A.
References
- 1.Fertitta L., Hotz C., Wolkenstein P., Meningaud J.P, Sawan D., Hersant B., Sbidian E. Efficacy and satisfaction of surgical treatment for hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2020;34:839–845. doi: 10.1111/jdv.16135. [DOI] [PubMed] [Google Scholar]
- 2.Ovadja Z., Bartelink S., van de Kar A., van der Horst C., Lapid O. A multicenter comparison of reconstruction strategies after wide excision for severe axillary hidradenitis suppurativa. Plas Reconstr Surg Glob Open. 2019;7:e2361. doi: 10.1097/GOX.0000000000002361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouazzi D., Chafranska L., Saunte D.M.L., Jemec G.B.E. Systematic review of complications and recurrences after surgical interventions in hidradenitis suppurativa. Dermatol Surg. 2020;46:914–921. doi: 10.1097/DSS.0000000000002323. [DOI] [PubMed] [Google Scholar]
- 4.Burney R.E. 35-year experience with surgical treatment of hidradenitis suppurativa. World J Surg. 2017;41:2723–2730. doi: 10.1007/s00268-017-4091-7. [DOI] [PubMed] [Google Scholar]
- 5.Jemec G.B., Guérin A., Kaminsky M., Okun M., Sundaram M. What happens after a single surgical intervention for hidradenitis suppurativa? A retrospective claims-based analysis. J Med Econ. 2016;19:710–717. doi: 10.3111/13696998.2016.1161636. [DOI] [PubMed] [Google Scholar]