Abstract
Background
Many hospitals have implemented visitor restriction policies in response to the coronavirus disease 2019 pandemic. Because caregivers serve an important role in postoperative recovery, the purpose of this study was to evaluate the impact of visitor restrictions on the postoperative experience of coronavirus disease 2019-negative patients undergoing surgery.
Methods
Patients who underwent surgery immediately before or after the implementation of a visitor restriction policy were enrolled. Patients were surveyed on their inpatient experience and preparedness for discharge using items adapted from validated questionnaires.
Results
Among 128 eligible patients, 117 agreed to participate (91.4% response rate): 58 (49.6%) in the Visitor Cohort and 59 (50.4%) in the No-Visitor Cohort. Mean age was 57.5 years (standard deviation 13.9) and 66 (56.4%) were female. Among all patients, 47.8% underwent oncologic surgery, 31.6% transplant, and 20.5% general or other. Patients in the No-Visitor Cohort were less likely to report complete satisfaction with the hospital experience (80.7% vs 66.0%, P = .044), timely receipt of medications (84.5% vs 69.0%, P = .048), and assistance getting out of bed (70.7% vs 51.7%, P = .036). No-Visitor Cohort patients were less likely to feel that their discharge preferences were adequately considered (79.3% vs 54.2%, P = .004). Qualitative analysis of patient responses highlighted the consistent psychosocial support provided by visitors after surgery (84.5%), and patients in the No-Visitor Cohort reported social isolation due to lack of psychosocial support (50.8%).
Conclusion
The implementation of hospital visitor restriction policies may adversely impact the postoperative experience of coronavirus disease 2019-negative patients undergoing surgery. These findings highlight the urgent need for novel patient-centered strategies to improve the postoperative experience of patients during ongoing or future disruptions to routine hospital practice.
Introduction
The novel coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, has significantly and rapidly changed health care delivery in the United States and around the world.1 To prevent the spread of COVID-19, protect patients and health care workers, preserve personal protective equipment, and prioritize resources for treating potential or actual surges in COVID-19 patients, routine surgery at most hospitals throughout the United States was abruptly halted.2 Although elective surgery was largely postponed, semiurgent operations (eg, cancer surgery) continued to be performed when delaying surgery was not deemed safe or feasible. In addition, many hospitals instituted significant changes to hospital visitor policies to limit the potential spread of COVID-19 among patients and hospital staff.3
Surgery is an anxiety-provoking experience for patients.4 After surgery, patients must not only manage the symptoms of the surgery itself, but also disruptions in their normal daily routine, loss of independence, and nonfamiliarity with the hospital environment. Family members, friends, and caregivers serve an important role in the recovery process of patients in the hospital and are thought to be important mediators for ensuring patient-centered care and preparing for transitions to the postdischarge setting.5, 6, 7 However, the impact of visitor restriction rules, made in the wake of the COVD-19 pandemic, on the postoperative experience of COVID-19-negative patients undergoing surgery is unknown. Therefore, the purpose of this study was to better understand the impact of visitor restriction rules on the postoperative experience of patients undergoing surgery. We hypothesized that visitor restrictions policies put in place due to the COVID-19 pandemic adversely impacted patients’ hospital experience. These data will not only elucidate the importance of caregiver involvement in the postoperative period, but also identify opportunities for improving the patient experience during ongoing or future disruptive changes to routine hospital practices.
Methods
Study design and population
On March 17, 2020, Ohio Governor Mike DeWine issued an order canceling all elective surgery throughout the state.8 Exceptions were allowed for those operations deemed essential, particularly if the procedure met certain criteria: threat to the patient’s life if surgery was not performed; threat of permanent dysfunction of an extremity or organ system; risk of metastasis or progression of staging; or risk of rapidly worsening to severe symptoms. Therefore, emergency and semiurgent operations continued to be performed at the Ohio State University Wexner Medical Center (OSUWMC) and throughout the state of Ohio. To further combat the threat of COVID-19, new visitor restriction rules were implemented at the OSUWMC on March 20, 2020, mandating that, with few exceptions, no visitors would be allowed in the hospital beyond the first postoperative day.9
A pre- and post-retrospective cohort study was designed to evaluate the experience of patients undergoing surgery before and after the implementation of visitor restriction rules. All patients who underwent surgery on the general, gastrointestinal, hepatopancreatobiliary, colorectal, noncardiac thoracic, or transplant surgery services at the OSUWMC between February 2, 2020 to March 19, 2020 (Visitors cohort) and from March 20, 2002 to April 16, 2020 (No-Visitors cohort) and who had neither confirmed nor suspected COVID-19 disease were eligible for participation. All interviews were conducted and completed in 4-week period immediately after the end of the eligibility dates. The study was approved by both the Ohio State institutional review and ad-hoc COVID-19 research review board.
Survey instrument
We developed a novel survey instrument for the present study that included domains from other validated questionnaires that are publicly available. The hospital experience was measured using questions adapted from Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. Anxiety and preparedness for discharge were measured using the validated Patient-Reported Outcomes Measurement Information System (PROMIS)10 and short-form Care Transitions Measure,11 respectively. We also assessed data on presence of visitors and mode of communication during hospitalization. In addition, 2 open-ended questions were asked and directly transcribed: (1) “How did (not) being able to have visitors make you feel following surgery?” and (2) “How did (not) being able to have visitors impact the discharge process?”
Study procedure
Patients were identified through screening of daily operating room schedules during the study period. Inclusion criteria included age ≥18 years old, primary English-speaking, and access to telephone, while exclusion criteria consisted of impaired mental capacity, prisoner status, known or suspected COVID positivity, and length of hospital stay <2 days. Patients undergoing emergency surgery (eg, acute care surgery, trauma) were not included. Eligible patients were contacted by telephone (5 phone calls maximum before exclusion) to assess interest in the study and provide verbal informed consent. No incentives were provided to participants.
Data analysis
Patients were divided into 2 cohorts (Visitors and No-Visitors) based on whether the hospital stay was before or after implementation of visitor restriction rules. Anxiety PROMIS scores were totaled for each patient. Hospital experience and preparedness for discharge questions were scored on a 4-point Likert scale. Qualitative data was reviewed for consistent themes, which were then grouped and subcategorized. Subjective response themes were allowed to span multiple subcategories.
Mean and standard deviation were used to describe continuous variables, whereas sample size and percentages were used to describe categorical variables. In instances where normality assumptions were not met, median and interquartile range were used. To compare Visitor and No-Visitor cohort demographic, clinical and psychosocial variables, independent t test was used for continuous variables and χ2 t test of independence was used for categorical variables. Fisher exact test was used where appropriate. SAS version 9.4 was used for data analysis and alpha was set at a 2-tailed P < .05.
Results
Patient cohort
Of the 128 eligible patients who were contacted, 117 completed the survey (91.4% response rate), including 58 (49.6%) in the Visitor Cohort and 59 (50.4%) in the No-Visitor Cohort. Table I reports the clinical and demographic characteristics of patients in each cohort. Mean age was 57.5 years old and 66 (56.4%) were female. Among all patients, 47.8% underwent oncologic surgery, 31.6% received a transplant, and 20.5% underwent general or other surgery with a greater percentage undergoing transplant in the No-Visitor Cohort (P = .041). There were no other differences between the 2 groups in demographic, clinical, or postoperative characteristics including postdischarge disposition and length of stay (median, [interquartile range]: 4.5 [3] vs 5.0 [3], P = .288).
Table I.
Demographic and clinical characteristics of patients undergoing surgery before and after implementation of visitor restriction rules
| Visitor N = 58 |
No-Visitor N = 59 |
P value | |
|---|---|---|---|
| Demographic characteristics | |||
| Age, mean (SD) | 57.5 (15.4%) | 57.6 (12.6%) | .960 |
| Sex | |||
| Male | 25 (43.1%) | 21 (38.9%) | .651 |
| Female | 33 (56.9%) | 33 (61.1%) | |
| Level of education | |||
| Junior high | 0 (0.0%) | 2 (3.4%) | .087 |
| High school | 23 (40.4%) | 12 (20.3%) | |
| Some college | 17 (29.8%) | 24 (40.7%) | |
| Undergraduate | 11 (19.3%) | 10 (16.9%) | |
| Graduate | 6 (10.5%) | 11 (18.6%) | |
| Race | |||
| Black | 8 (13.8%) | 10 (17.2%) | .876 |
| White | 49 (84.5%) | 47 (81.0%) | |
| Other | 1 (1.7%) | 1 (1.7%) | |
| Marital status | |||
| Single | 9 (15.5%) | 15 (25.4%) | .337 |
| Married/partner | 35 (60.3%) | 37 (62.7%) | |
| Divorce/separated | 6 (10.3%) | 4 (6.8%) | |
| Widowed | 7 (12.1%) | 3 (5.1%) | |
| Other | 1 (1.7%) | 0 (0.0%) | |
| Clinical characteristics | |||
| Type of surgery | |||
| Cancer | 32 (55.2%) | 24 (40.7%) | .041 |
| Transplant | 12 (20.7%) | 25 (42.4%) | |
| General/other | 14 (24.1%) | 10 (16.9%) | |
| Disposition | |||
| Home | 53 (91.4%) | 58 (98.3%) | .221 |
| Skilled nursing facility | 4 (6.9%) | 1 (1.7%) | |
| Long-term nursing facility | 1 (1.7%) | 0 | |
| Length of stay, median [IQR] | 4.5 [3] | 5 [3] | .288 |
IQR, interquartile range.
Quantitative results
Social support and methods of communication
In both the Visitor and No-Visitor Cohorts, most patients indicated that they relied on their spouse for social support (63.8% vs 67.8%, P = .648). More patients in the Visitor Cohort said they relied upon friends (24.1% vs 10.2%, P = .045) and adult children (46.6% vs 20.3%, P = .003) compared with the No-Visitor Cohort (Table II ). In both cohorts, the most commonly used modes of communication were voice phone call and text messaging. A greater proportion of No-Visitor Cohort patients used video chat as a method of communication (30.5% vs 15.5%, P = .054).
Table II.
Survey results of patients undergoing surgery before and after implementation of visitor restriction rules
| Visitor N = 58 |
No-Visitor N = 59 |
P value | |
|---|---|---|---|
| Social support | |||
| Spouse | 37 (63.8%) | 40 (67.8%) | .648 |
| Friends | 14 (24.1%) | 6 (10.2%) | .045 |
| Adult children | 27 (46.6%) | 12 (20.3%) | .003 |
| Pastor/religious | 3 (5.2%) | 3 (5.1%) | .983 |
| Other | 22 (37.9%) | 16 (27.1%) | .212 |
| Communication | |||
| Text messaging | 44 (75.9%) | 40 (67.8%) | .332 |
| 4 (6.9%) | 4 (6.8%) | .980 | |
| 11 (19.0%) | 7 (11.9%) | .287 | |
| My chart | 1 (1.7%) | 2 (3.4%) | .569 |
| Video chat | 9 (15.5%) | 18 (30.5%) | .054 |
| Voice phone call | 47 (81.0%) | 49 (83.1%) | .776 |
| 0 (0.08%) | 3 (5.1%) | .082 | |
| Other | 4 (6.9%) | 2 (3.4%) | .390 |
| Communication used most | |||
| Text messaging | 25 (46.3%) | 20 (33.9%) | .085 |
| - | - | ||
| 2 (3.7%) | 0 (0.0%) | ||
| My chart | - | - | |
| Video chat | 0 (0.0%) | 5 (8.5%) | |
| Voice phone call | 26 (48.1%) | 33 (55.9%) | |
| - | - | ||
| Other | 1 (1.9%) | 1 (1.7%) | |
| Total anxiety score | |||
| Anxiety, mean (SD) | 12.7 (4.3) | 13.4 (4.9) | .471 |
| Hospital satisfaction: How satisfied were you with your overall hospital experience? n (%) | |||
| Completely satisfied | 46 (80.7%) | 35 (66.0%) | .044 |
| Otherwise | 11 (19.0%) | 21 (35.6%) | |
| Hospital satisfaction: How satisfied are you with your decision to proceed with surgery when you had it? n (%) | |||
| Completely satisfied | 40 (86.2%) | 47 (82.5%) | .580 |
| Otherwise | 8 (13.8%) | 10 (17.5%) | |
| Hospital experience: I had a good understanding of my condition and the plan for each day | |||
| Strongly agree | 43 (74.1%) | 35 (59.3%) | .089 |
| Otherwise | 15 (25.9%) | 24 (40.7%) | |
| Hospital experience: I was able to communicate with my care team and have my questions answered | |||
| Strongly agree | 40 (69.0%) | 34 (58.6%) | .246 |
| Otherwise | 18 (31.0%) | 24 (41.4%) | |
| Hospital experience: I was able to receive pain, nausea, or other medicines when I needed them | |||
| Strongly agree | 49 (84.5%) | 40 (69.0%) | .048 |
| Otherwise | 9 (15.5%) | 18 (31.0%) | |
| Hospital experience: Help was always available when I wanted to get out of bed | |||
| Strongly agree | 41 (70.7%) | 30 (51.7%) | .036 |
| Otherwise | 17 (29.3%) | 28 (48.3%) | |
| Care transition: The hospital staff took my preferences and those of my family or caregiver into account in deciding what my health care needs would be when I left the hospital | |||
| Strongly agree | 46 (79.3%) | 32 (54.2%) | .004 |
| Otherwise | 12 (20.7%) | 27 (45.8%) | |
| Care transition: When I left the hospital, I had a good understanding of the things I was responsible for in managing my health | |||
| Strongly agree | 44 (75.9%) | 40 (67.8%) | .332 |
| Otherwise | 14 (24.1%) | 19 (32.2%) | |
| Care transition: When I left the hospital, I clearly understood the purpose of taking each of my medications | |||
| Strongly agree | 45 (77.6%) | 41 (69.5%) | .321 |
| Otherwise | 13 (22.4%) | 18 (30.5%) | |
All data are n (%) unless otherwise specified.
Hospital experience
Patients in the No-Visitor Cohort were less likely to report that they were completely satisfied with their overall hospital experience (80.7% vs 66.0%, P = .044), but were similarly satisfied with their decision to proceed with surgery (86.2% vs 82.5%, P = .580). There was no statistical difference between the groups in reporting a strong understanding of their condition and daily plan (74.1% vs 59.3%, P = .089). Patients in the No-Visitor Cohort were also less likely to report timely access to pain, nausea, and other medications (84.5% vs 69.0%, P = .048) and help getting out of bed (70.7% vs 51.7%, P = .036). There was no difference in mean PROMIS anxiety scores (13.4 vs 12.7, P = .471; Table II).
Preparedness for discharge
Although there was no difference in the proportion of patients who reported a good understanding of their condition at discharge (75.9% vs 67.8%, P = .332) or purpose of their discharge medications (77.6% vs 69.5%, P = .321), patients in the No-Visitor Cohort were less likely to strongly agree that their preferences and their family members’ preferences were adequately considered upon discharge (79.3% vs 54.2%, P = .004; Table II).
Qualitative results
Hospital experience
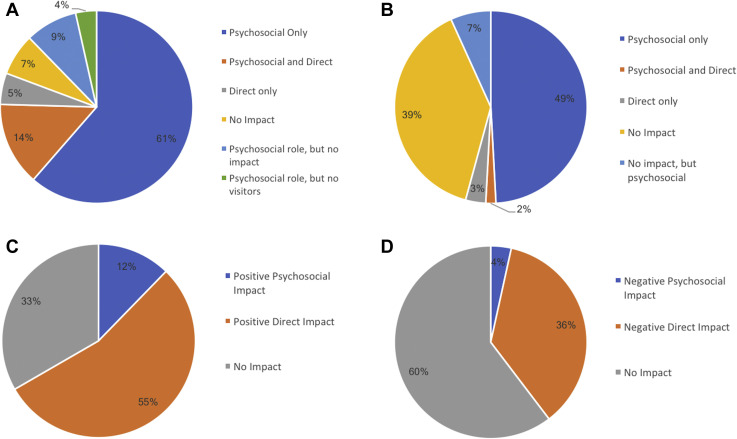
Most patients in the Visitor Cohort (84.5%) reported that visitors provided psychosocial support after surgery, whereas lack of psychosocial support from visitors was commonly cited in the No-Visitor Cohort (50.8%). Specifically, feelings of isolation and loneliness were common among those without visitors. A minority of patients in both cohorts (18.9% vs 5.1%) felt that visitors served important direct support roles. More patients in the No-Visitor Cohort reported that visitors did not impact their hospital experience compared with the Visitor cohort (42.3% vs 17.2%; Table III , Fig 1 , A and B).
Table III.
Qualitative answers regarding impact of visitors on postoperative experience before and after implementation of visitor restriction rules
| Theme | Frequency | Representative comment |
|---|---|---|
| How did being able to have visitors make you feel after surgery? | ||
| Visitor (n = 58) | ||
| Psychosocial | 49 (84.5%) | “It lifted my spirits. When people close to you come, your spirits are lifted. Communication and talking to loved ones is the best help.” |
| General positive reaction | 24 (41.4%) | |
| Reassurance, comfort | 15 (25.9%) | |
| Morale boosting | 5 (8.6%) | |
| Pain and stress relief | 5(8.6%) | |
| Company/communication | 8 (13.8%) | |
| Direct | 11 (18.9%) | “[It made me feel] safer. Coming out of surgery and not being able to listen or grasp what was going on, it was good to have someone to hear, listen, and gather information.” |
| Instructions/comprehension | 11 (18.9%) | |
| Patient safety | 1 (1.7%) | |
| Patient advocacy | 1 (1.7%) | |
| No impact | 10 (17.2%) | [It] “did not impact me at all, I'm the type of person who hates when people come to the hospital and just sit there and watch you when you can't do anything.” |
| More opportunity to rest/less distractions | 5 (8.6%) | |
| Support from hospital resources | 3 (5.2%) | |
| Indifference toward visitation | 4 (6.9%) | |
| Other | 4 (6.9%) | “I did not have any visitors in the hospital, but felt good knowing they could come.” |
| No visitors | 3 (5.2%) | |
| No comment | 1 (1.7%) | |
| No-Visitor (n = 59) | ||
| How did the lack of visitors make you feel after surgery? | ||
| Psychosocial | 30 (50.8%) | “It was really hard…I just wanted to see my daughter. She cried on facetime every day and I really just wanted to see her and my wife.” |
| Isolation, decreased communication | 29 (49.2%) | |
| General sadness, anxiety | 11 (18.6%) | |
| Other | 3 (5.1%) | |
| Direct | 3 (5.1%) | “…it was really hard. He has been taking care of me through all of this and I depend upon him.” |
| Other | 3 (5.1%) | |
| No impact | 25 (42.3%) | |
| More opportunity to rest/less distractions | 6 (10.2%) | “[It was] no problem, it let me rest more…I felt relieved that others would not be exposed to virus.” |
| Adequate preparation/expectations | 4 (6.7%) | |
| Other | 16 (32.2%) | |
Fig 1.
Impact of visitors on the postoperative experience of patients before (A) and after (B) visitor restriction rules; impact of visitors on discharge process of patients before (C) and after (D) visitor restriction rules.
Preparedness for discharge
In the Visitor Cohort, 53.4% patients indicated that the presence of visitors had a direct effect on the discharge process whereas 35.5% in the No-Visitor Cohort reported their discharge was affected in a direct way due to the lack of visitors. Fewer patients in both cohorts (12.0% vs 3.3%) felt that visitors affected the discharge process due to psychosocial support. Although 34.5% of Visitor Cohort patients felt that the presence of visitors had no impact on the discharge process, 61.0% of No-Visitor Cohort patients felt that the lack of visitors had no impact. Among the No-Visitor Cohort patients, early discharge coordination, comfort level with their health condition, and increased staff support were the main reasons that the restrictions did not have an effect on discharge (Table IV , Fig 1, C and D).
Table IV.
Qualitative answers regarding impact of visitors on discharge process before and after implementation of visitor restriction rules
| Theme | Frequency | Representative comment |
|---|---|---|
| Visitor (n = 58) | ||
| How did being able to have visitors impact the discharge process? | ||
| Psychosocial | 7 (12.0%) | [It] “made me more comfortable and ready to be discharged. I was more certain of continued progress outside the hospital. It made me feel reassured and stronger leaving, and more connected having a continuation of the social support that I had inside the hospital.” |
| Direct | 31 (53.4%) | “They showed my fiancé everything he needed to know to take care of me. He was able to learn everything necessary for care so that he could take care of me and so we would not need to have home health…” |
| Discharge instruction | 18 (31.0%) | |
| Ambulation/physical help | 8 (13.8%) | |
| Facilitation | 6 (10.3%) | |
| Other | 2 (3.4%) | |
| No impact | 20 (34.5%) | [It] “honestly didn't really matter with the discharge, other than transportation, but everything else was communicated clearly ahead of time so [discharge] wasn't affected a whole lot.” |
| Prior coordination | 8 (13.8%) | |
| Other or unspecified | 14 (24.1%) | |
| No-Visitor (n = 59) | ||
| How did the lack of visitors impact the discharge process? | ||
| Psychosocial | 2 (3.3%) | “I was just happy that I could …. be with my husband and daughter.” |
| Direct | 21 (35.5%) | “My wife was going to be the one responsible for taking care of me… so it would have been nice if she could have been there. It would have helped us understand together.” |
| Discharge Instructions | 13 (22.0%) | |
| Ambulation/physical help | 6 (10.2%) | |
| Other | 6 (10.2%) | |
| No impact | 36 (61.0%) | “It didn’t really affect it. I had a coordinator talking to my wife about expectations, pick up, medication refills, and transportation. So, it was great; we knew what to expect about discharge.” |
| Not specified | 18 (30.5%) | |
| Prior instruction/coordination | 8 (13.6%) | |
| Health literacy | 4 (6.8%) | |
| Staff support | 4 (6.8%) | |
| No comment | 1 (1.7%) | |
Discussion
The abrupt implementation of strict visitor restriction rules in the face of the COVID-19 pandemic allowed a social experiment on the influence of caregivers on the hospital experience and discharge preparedness of patients recovering from surgery. Our results suggest that visitor restriction policies may directly impact the postoperative experience of patients in several ways. First, patients lacking visitors were more likely to be dissatisfied with their overall hospital experience. Second, a lack of visitors adversely affected patients’ psychosocial well-being. Finally, patients without visitors were less likely to have their preferences adequately addressed upon discharge. These findings highlight the urgent need for novel strategies to improve the postoperative experience of hospitalized patients during the COVID-19 pandemic.
Objective measures of patient satisfaction and the patient experience after inpatient surgery have been an increasingly important quality metric since the Centers for Medicare and Medicaid Services partnered with the Agency for Healthcare Research and Quality to implement the Hospital CAHPS survey program nearly 20 years ago.12 The use of the CAHPS survey also reflects a shift in recognizing the importance of patient-centered outcomes among patients, physicians, payers, and hospitals.13 It is therefore relevant that a significantly lower proportion of patients were highly satisfied with their inpatient experience after the implementation of a visitor restriction policy. Although patient satisfaction may reflect a number of perceptions regarding care, especially during a tumultuous time of change, the observation that perceptions of timely access to medications and assistance getting out of bed were affected (both issues where a bedside caregiver’s advocacy and direct assistance may play a role), suggests that the decrease in hospital satisfaction was at least partially related to the absence of permitted visitors. Previous research among Medicare beneficiaries has suggested a close link between the presence of visitors and patient satisfaction scores, potentially mediated via improved patient-physician engagement and communication.14 Similarly, obtaining information from the care team might be easier with a companion present, which may explain the slight difference in patient-reported understanding of their daily condition noted in our study (P = .09).15
Surgery is understood to be a stressful experience no matter the circumstances.4 Psychosocial stress occurs in a number of domains including anxiety and loneliness. Although we had hypothesized that patients without visitors would experience higher rates of anxiety, we found that feelings of loneliness and isolation were much more prominent. Most patients in both cohorts commented on the importance of visitors for psychosocial support, which is consistent with previous research.16 , 17 Prior studies have specifically documented the importance of psychosocial support among patients recovering from transplant and cancer surgery, which comprised a majority of the patients in our study.18, 19, 20 Given that social isolation and loneliness are common among hospitalized patients after surgery, it is not surprising that lack of visitors had a detrimental effect. Our study found greater use of video messaging during the no visitor time period; additional research is warranted to promote such interactions as a means to ameliorate the deleterious feelings of isolation that may occur as a result of no-visitor policies. Alternatives to strict “no-visitor” policies, such as permitting limited visitors, allocation of personal protective equipment, or expanded COVID testing could also be considered by various stakeholders and hospital leaders. For example, hospitals could consider permitting a limited number of visitors for non-COVID patients provided they pass temperature and symptom screening, ensure no recent travel to hotspots or contact with COVID-positive individuals, and agree to appropriate mask wearing and hand hygiene. These policies could also be dynamic responding to current trends in local infection rates.
Despite their importance on COVID-negative patients’ in-hospital experience, the visitor restrictions appeared to have less of an influence on preparedness for discharge. Patients still reported a good understanding of their condition and the purpose of their medications at the time of discharge but were less likely to perceive that their preferences were adequately being considered in discharge planning. Some patient comments noted caregivers’ value in assisting with discharge, but more patients (61%) reported little to no impact on their discharge process. These results were reassuring since miscommunication and misunderstandings are a common cause of hospital readmission.21 Based on patient responses, it is likely that greater differences in preparedness for discharge were mitigated by early discharge planning by hospital staff and the allowance of some caregiver education at the time of patient transport. As caregiver engagement is an integral component of care transitions, a limitation of the current study is the absence of data on the caregiver’s experience and their preparedness for discharge.
The findings of this study highlight the need for patient-centered interventions designed to improve the experience of patients during ongoing visitor restrictions due to the COVID-19 pandemic. First, although patient satisfaction is a complex measure that differs among respondents, a critical component is establishing clear patient expectations regarding their care. An improved understanding of hospital policies before surgery may set realistic expectations for patients and allow them time to prepare accordingly. Previous studies have emphasized the important benefits of patient and caregiver preparatory education on postoperative recovery after surgery.22 Care teams may also consider including a discussion of visitor restriction policies and how they might impact patient recovery in the informed consent process before surgery.23 Second, strategies aimed at decreasing social isolation and loneliness and improving psychosocial support should be implemented. Although the use of technology may overcome some of these barriers, these methods may be limited by access and familiarity to newer devices especially in vulnerable populations.24 , 25 At the OSUWMC, patients are now offered tablets with built-in video chat capabilities; many hospitals have created similar “virtual visitor” programs. Third, because patients perceived that timely access to medications and walking assistance was affected by the lack of visitors, hospitals should make changes to adjust for this deficiency. Increasing the number of medical assistants, adjusting medication or walking schedules, and clarifying patient expectations regularly may be helpful. Collectively, these findings have important implications for hospitals, payers, and local government leaders. Given the importance of hospital satisfaction as a quality measure for accreditation and reimbursement, continued attention to patient experience scores in a rapidly changing medical environment will be imperative. These data may also be helpful as hospital and government leaders adjust local policies aimed at combating the COVID-19 pandemic.
Despite the novelty and importance of the present study’s findings, several limitations should be acknowledged. First, there was an implicit risk of recall bias since the No-Visitor cohort patients were interviewed more closely to their time of surgery and discharge. Second, this was a single-institution study of a relatively homogenous patient population and while our survey was adapted from several validated instruments, it was designed for this study and had not been previously validated in this patient population. Third, given the nonrandomized before or after design of the study, our results may have been influenced by other clinical or hospital-related factors such as other formal or informal hospital changes in wake of COVID-19 (eg, reduced staff availability, structural barriers to patient contact, resource reallocation, etc). Fourth, differences in the indications for surgery may have existed which could have influenced our results. Indeed, the No-Visitor cohort was comprised of a greater proportion of patients undergoing transplant surgery. On the other hand, only 3.4% of operations in the Visitor cohort would not have met criteria to have been performed during the No-Visitor time period, which may minimize the impact of this limitation. Finally, this study only examined patients undergoing essential surgery that could not be postponed and therefore the findings do not necessarily apply to patients undergoing emergency or nonessential surgery.
In conclusion, compared with patients undergoing surgery immediately before the implementation of a hospital visitor restriction policy, COVID-negative patients without hospital visitors were less likely to report complete satisfaction with their hospital experience, less timely access to necessary medications and assistance getting out of bed, and that their preferences were adequately considered at the time of discharge. Patients in both cohorts consistently reported the importance of visitors in providing psychosocial support during the hospital stay. These findings highlight the urgent need for novel strategies to improve the postoperative experience of hospitalized patients during the COVID-19 pandemic.
Funding/Support
The authors did not receive funding or financial support for this project.
Conflict of interest/Disclosure
The authors have no conflicts of interest to declare.
Acknowledgments
The authors extend their sincere appreciation to the patients who participated in this study and shared their experience with us. We thank Victor Heh, MS, for assistance with statistical analysis.
References
- 1.Del Rio C., Malani P.N. COVID-19-new insights on a rapidly changing epidemic. JAMA. 2020;323:1339–1340. doi: 10.1001/jama.2020.3072. [DOI] [PubMed] [Google Scholar]
- 2.Weise K. The coronavirus is forcing hospitals to cancel surgeries. New York Times. 2020;35:1630–1636. [Google Scholar]
- 3.Anand P. The pandemic is changing how we die—and not just for COVID-19 patients. TIME. 2020 [Google Scholar]
- 4.Badner N.H., Nielson W.R., Munk S., Kwiatkowska C., Gelb A.W. Preoperative anxiety: detection and contributing factors. Can J Anaesth. 1990;37:444–447. doi: 10.1007/BF03005624. [DOI] [PubMed] [Google Scholar]
- 5.Gillick M.R. The critical role of caregivers in achieving patient-centered care. JAMA. 2013;310:575–576. doi: 10.1001/jama.2013.7310. [DOI] [PubMed] [Google Scholar]
- 6.Kulik J.A., Mahler H.I. Social support and recovery from surgery. Health Psychol. 1989;8:221–238. doi: 10.1037//0278-6133.8.2.221. [DOI] [PubMed] [Google Scholar]
- 7.Weinberg D.B., Lusenhop R.W., Gittell J.H., Kautz C.M. Coordination between formal providers and informal caregivers. Health Care Manage Rev. 2007;32:140–149. doi: 10.1097/01.HMR.0000267790.24933.4c. [DOI] [PubMed] [Google Scholar]
- 8.Elective Surgeries Postponed in Ohio Hospitals 3/17/2020, 2020. Available at: https://governor.ohio.gov/wps/portal/gov/governor/media/news-and-media/elective%2Bsurgeries-postponed-in-ohio-hospitals. Accessed March 27, 2020.
- 9.Visitor Policy: COVID-19 | Ohio State Medical Center. Available at: wexnermedical.osu.edu. https://wexnermedical.osu.edu/features/coronavirus/patient-care/visitor-policy. Accessed March 27, 2020.
- 10.Hays R.D., Spritzer K.L., Schalet B.D., Cella D. PROMIS-29 v2.0 profile physical and mental health summary scores. Qual Life Res. 2018;27:1885–1891. doi: 10.1007/s11136-018-1842-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flink M., Tessma M., Cvancarova Smastuen M., Lindblad M., Coleman E.A., Ekstedt M. Measuring care transitions in Sweden: validation of the care transitions measure. Int J Qual Health Care. 2018;30:291–297. doi: 10.1093/intqhc/mzy001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldstein E., Fyock J. Reporting of CAHPS quality information to medicare beneficiaries. Health Serv Res. 2001;36:477–488. [PMC free article] [PubMed] [Google Scholar]
- 13.Selby J.V., Beal A.C., Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307:1583–1584. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 14.Wolff J.L., Roter D.L. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. 2008;168:1409–1415. doi: 10.1001/archinte.168.13.1409. [DOI] [PubMed] [Google Scholar]
- 15.Wolff J.L., Roter D.L. Family presence in routine medical visits: a meta-analytical review. Soc Sci Med. 2011;72:823–831. doi: 10.1016/j.socscimed.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ang S.G., Chen H.C., Siah R.J., He H.G., Klainin-Yobas P. Stressors relating to patient psychological health following stoma surgery: an integrated literature review. Oncol Nurs Forum. 2013;40:587–594. doi: 10.1188/13.ONF.587-594. [DOI] [PubMed] [Google Scholar]
- 17.Leeds I.L., Meyers P.M., Enumah Z.O. Psychosocial risks are independently associated with cancer surgery outcomes in medically comorbid patients. Ann Surg Oncol. 2019;26:936–944. doi: 10.1245/s10434-018-07136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ercolano E. Psychosocial concerns in the postoperative oncology patient. Semin Oncol Nurs. 2017;33:74–79. doi: 10.1016/j.soncn.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Mavros M.N., Athanasiou S., Gkegkes I.D., Polyzos K.A., Peppas G., Falagas M.E. Do psychological variables affect early surgical recovery? PLoS One. 2011;6:e20306. doi: 10.1371/journal.pone.0020306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skotzko C.E., Stowe J.A., Wright C., Kendall K., Dew M.A. Approaching a consensus: psychosocial support services for solid organ transplantation programs. Prog Transplant. 2001;11:163–168. doi: 10.1177/152692480101100303. [DOI] [PubMed] [Google Scholar]
- 21.Solan L.G., Beck A.F., Brunswick S.A. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136:e1539–e1549. doi: 10.1542/peds.2015-2098. [DOI] [PubMed] [Google Scholar]
- 22.Ronco M., Iona L., Fabbro C., Bulfone G., Palese A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int J Evid Based Healthc. 2012;10:309–323. doi: 10.1111/j.1744-1609.2012.00286.x. [DOI] [PubMed] [Google Scholar]
- 23.Poulose B.K., Phieffer L.S., Mayerson J. Responsible return to essential and non-essential surgery during the COVID-19 pandemic. J Gastrointest Surg. 2020 doi: 10.1007/s11605-020-04673-9. [e-pub ahead of print] Accessed June 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huh J., Koola J., Contreras A. Consumer health informatics adoption among underserved populations: Thinking beyond the digital divide. Yearb Med Inform. 2018;27:146–155. doi: 10.1055/s-0038-1641217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Renault M. When Health Care Moves Online, Many Patients Are Left Behind. WIRED. https://www.wired.com/story/health-care-online-patients-left-behind/.