Abstract
The many carbohydrate chains on Covid-19 coronavirus SARS-CoV-2 and its S-protein form a glycan-shield that masks antigenic peptides and decreases uptake of inactivated virus or S-protein vaccines by APC. Studies on inactivated influenza virus and recombinant gp120 of HIV vaccines indicate that glycoengineering of glycan-shields to present α-gal epitopes (Galα1-3Galβ1-4GlcNAc-R) enables harnessing of the natural anti-Gal antibody for amplifying vaccine efficacy, as evaluated in mice producing anti-Gal. The α-gal epitope is the ligand for the natural anti-Gal antibody which constitutes ~1% of immunoglobulins in humans. Upon administration of vaccines presenting α-gal epitopes, anti-Gal binds to these epitopes at the vaccination site and forms immune complexes with the vaccines. These immune complexes are targeted for extensive uptake by APC as a result of binding of the Fc portion of immunocomplexed anti-Gal to Fc receptors on APC. This anti-Gal mediated effective uptake of vaccines by APC results in 10–200-fold higher anti-viral immune response and in 8-fold higher survival rate following challenge with a lethal dose of live influenza virus, than same vaccines lacking α-gal epitopes. It is suggested that glycoengineering of carbohydrate chains on the glycan-shield of inactivated SARS-CoV-2 or on S-protein vaccines, for presenting α-gal epitopes, will have similar amplifying effects on vaccine efficacy. α-Gal epitope synthesis on coronavirus vaccines can be achieved with recombinant α1,3galactosyltransferase, replication of the virus in cells with high α1,3galactosyltransferase activity as a result of stable transfection of cells with several copies of the α1,3galactosyltransferase gene (GGTA1), or by transduction of host cells with replication defective adenovirus containing this gene. In addition, recombinant S-protein presenting multiple α-gal epitopes on the glycan-shield may be produced in glycoengineered yeast or bacteria expression systems containing the corresponding glycosyltransferases. Prospective Covid-19 vaccines presenting α-gal epitopes may provide better protection than vaccines lacking this epitope because of increased uptake by APC.
Keywords: Covid-19 vaccine, SARS-CoV-2, S-protein, Glycan shield, anti-Gal, α-gal epitopes
1. Introduction
Increasing numbers of research groups are developing prophylactic vaccines against infection by the Covid-19 coronavirus SARS-CoV-2. As of June 2020, >120 vaccines reported to be at various stages of development [1], are divided into two major groups: 1. Vaccines prepared of virus replicating in cell lines, including live attenuated viruses, inactivated viruses, split vaccines, subunit vaccines prepared of the virus or produced as a recombinant protein in various expression systems, and virus-like particles. 2. Vaccines composed of nucleic acid (DNA and RNA) and viral vectors or nanoparticles that deliver the gene or mRNA of the coronavirus spike glycoprotein (referred to as S-protein) on the envelope of SARS-CoV-2. These vaccines are delivered into tissues (usually muscle tissue) of the vaccinated individual for activation of the immune system to develop protective T cells and neutralizing antibody response against infecting SARS-CoV-2 [1], [2], [3]. The S-protein, which is the major glycoprotein on the envelope of SARS-CoV-2, mediates binding of the virus to the angiotensin converting enzyme 2 (ACE-2) that functions as the cell surface “docking” receptor for SARS-CoV-2, and further enables the fusion of the virus with the cell membrane within endosomes [4], [5], [6], [7]. Because of these activities, the S-protein is considered an important target for development of vaccines that elicit production of neutralizing antibodies which inhibit binding of the virus to cells, thereby preventing viral infections causing Covid-19 and induce activation and proliferation of T cells that lyse virus infected cells. Two recent examples of clinical trials with DNA and RNA S-protein vaccines are the ChAdOx1 nCoV-19 [8] and mRNA-1273 [9], respectively. ChAdOx1 nCoV-19 uses a replication-deficient chimpanzee adenovirus to deliver the SARS-CoV-2 S-protein gene. The mRNA-1273 vaccine consists of lipid nanoparticles containing the S-protein mRNA. With both vaccines, two intramuscular injections of the vaccine to healthy volunteers in one-month interval resulted in production of anti-viral antibodies binding to S-protein in ELISA and of SARS-CoV-2 live virus neutralizing antibodies. In addition, ELISPOT studies with SARS-CoV-2 S-protein stimulatory peptides revealed marked increase in T cell activation following the two immunizations. Thus, both vaccines demonstrate effective stimulation of the immune system for eliciting both antibody and T cell response against SARS-CoV-2.
The availability of DNA and RNA vaccines in Group 2 such as ChAdOx1 nCoV-19 and mRNA-1273, within the very-short period of few months indicates one of their major advantages: The ability to produce such vaccines in short time. Group 1 vaccines which involves production of the actual vaccinating virus or of S-protein to be used as vaccines is much more labor intensive and takes significantly longer time. However, in addition to the extensive experience gained with whole virus and subunit vaccines and the much easier ability to control the dose of the actual vaccinating material, a great advantage of Group 1 vaccines is that they can be engineered for increasing their immunogenicity. Since the immunizing antigens of Group 2 vaccines are produced within the vaccinated individuals, no engineering of the protein component of the vaccine is feasible. Development of methods for engineering prophylactic vaccines to increase their efficacy (i.e., immunogenicity) in preventing SARS-CoV-2 infections is of significance for several reasons: 1. Higher immunogenicity will enable the use of lower amounts of vaccinating materials, thus enabling sufficient production of vaccine for wide global immunization of billions of individuals for protection against Covid-19. 2. Vaccines that are effective in young populations may not suffice for protecting the elderly, as demonstrated with influenza vaccines [10], [11], [12]. The lower immune response to SARS-CoV-2 infection makes the elderly more susceptible to the detrimental effects of human to human transmission of the virus and is further indicated by the much higher mortality rate of Covid-19 among elderly than in young individuals [13], [14]. 3. Studies in convalescent patients following previous SARS infections demonstrated very-low anti-S-protein antibody titers [15] which has been associated with the low immunogenicity of coronavirus S-protein. This low immunogenicity is associated with the carbohydrate chains (glycans) forming the glycan-shield that “hides” immunogenic peptides of this envelope glycoprotein thereby evading neutralizing antibodies that prevent virus adhesion to cell surface receptors [16], [17], [18]. Shielding by glycans the receptor binding sites on viral glycoproteins that interact with cell surface receptors is a common feature of viral glycoproteins, as observed on SARS-CoV-1 S-protein [16], gp120 of HIV[19], [20] and influenza virus hemagglutinin (HA) [21], [22]. The principle of the methods described in this review is glycoengineering the glycan-shield on viral vaccines for its conversion from protein masking glycan into glycan that effectively targets vaccines to antigen presenting cells (APC) thereby markedly increasing the immunogenicity of viral vaccines. This effective targeting for the extensive uptake of viral vaccines by APC is achieved by harnessing the natural anti-Gal antibody which is abundant in all humans who are not severely immunocompromised. Since the proposed glycoengineering was found to increase immunogenicity of viral vaccines such as influenza virus and gp120 of HIV up to 100–200 fold, this review suggests that the glycoengineering methods presented here may greatly increase immunogenicity of vaccines containing attenuated or inactivated SARS-CoV-2, or the S-protein of this virus.
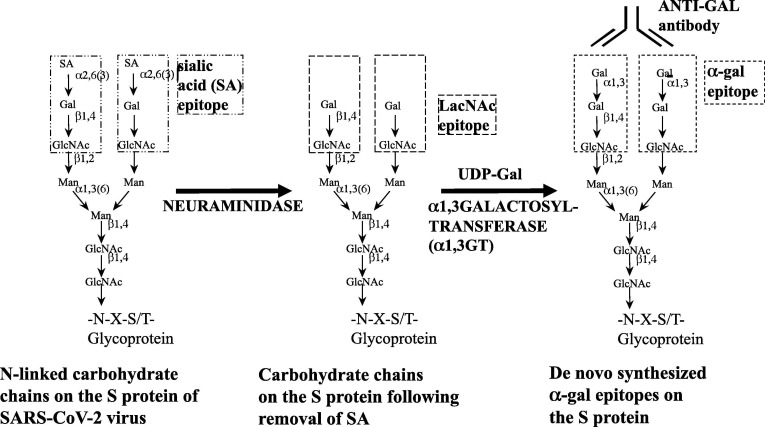
The S-protein sequence of SARS-CoV-2 has 22 asparagine (N)-linked glycans, synthesized on asparagine in amino acid sequences asparagine-any amino acid-serine or threonine (N-X-S/T) [18]. Part of the glycans are of the high-mannose type and the rest are of the complex-type. These glycans form the glycan-shield that covers >65% of the S-protein surface, potentially camouflaging antigenic peptides, thereby evading detection by neutralizing antibodies [16], [17], [18]. The low anti-S-protein antibody response in convalescent SARS patients [15] suggests that the glycan-shield of the S-protein further prevents effective exposure of the immunogenic peptides to B cells, thereby decreasing the extent of antibody response to this major envelope glycoprotein of SARS-CoV-2. A similar function of immune evasion has been attributed to the glycan-shield of HIV-gp120 [19], [20], [23] which has 24 N-linked glycans, of which 13 to 16 are of the complex type, each capped by 2–4 sialic acid residues (left glycan in Fig. 1 ) and the rest are of the high mannose type [24], [25]. Since glycans on virus envelope glycoproteins are synthesized within the Golgi apparatus by the host cell glycosylation machinery, it is probable that similar to gp120, a significant portion of the 22 N-linked glycans of the S-protein synthesized in various host cells, also are of the complex type, similar to the left glycan in Fig. 1. The ratio between the complex type and high mannose N-linked glycans depends on make-up and activity of the various glycosylation enzymes in the host cell in which the virus is propagated.
Fig. 1.
Glycoengineering of α-gal epitopes on Spike (S)-protein of SARS-CoV-2 virus. Left chain- Carbohydrate chains (glycans) of the complex type on viral envelope glycoproteins are synthesized on asparagine (N) in amino acid sequences of N-X-S/T-. Based on the information about a similar glycan shield of HIV-gp120, it is probable that many of these carbohydrate chains of the S-protein are capped by sialic acid (SA). Center chain- Sialic acid is removed from the carbohydrate chain by neuraminidase to expose the penultimate Galβ1-4GlcNAc-R, called N-acetyllactosamine (LacNAc). Right chain- Incubation of inactivated virus or soluble S-protein (split or subunit vaccine) carrying the desialylated glycan, with recombinant α1,3galactosyltransferase (rα1,3GT) and with UDP-Gal results in synthesis of α-gal epitopes (Galα1-3Galβ1-4GlcNAc-R) on the glycans in the same reaction as synthesis of these epitopes on glycoproteins and glycolipids within mammalian cells. These epitopes readily bind the natural anti-Gal antibody at the vaccination site and form immune complexes that are targeted for extensive uptake by APC.
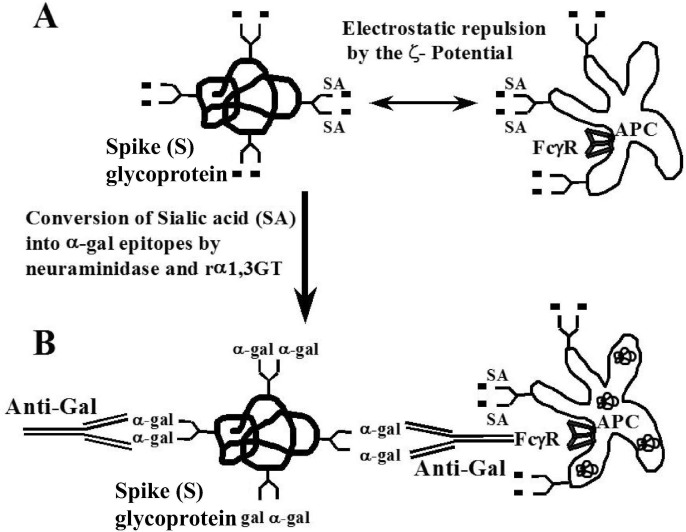
Since glycans are hydrophilic, they protrude from the S-protein like quills of a porcupine and those with sialic acid residues surround the vaccinating S-protein molecules with negative electrostatic charges (Fig. 2 A). Multiple sialic acid residues also cap cell surface glycans on APC. Negative charges on the vaccinating S-protein and those on the cell surface of APC create electrostatic repulsion (zeta [ζ] potential) that decreases the uptake of vaccinating S-protein molecules by APC [26]. Glycoengineering of the glycan-shield, as described in this review, is likely to convert this shield from an obstacle for uptake of vaccine by APC into a portion of the S-protein molecule that effectively targets it for extensive uptake by APC, thereby amplifying immunogenicity by increasing processing and presentation of SARS-CoV-2 antigens by the APC. This conversion is achieved by replacing sialic acid on the glycan-shield of the S-protein vaccine with terminal galactose linked α1-3 to the glycans in order to form multiple α-gal epitopes with the structure Galα1-3Galβ1-4GlcNAc-R on the S-protein (called here S-proteinα gal) (Fig. 1). The S-proteinα gal vaccine forms in situ immune complexes with the natural anti-Gal antibody of the vaccinated individual. The anti-Gal/S-proteinα gal immune complexes are targeted for extensive uptake by APC as a result of binding of the Fc portion of immunocomplexed anti-Gal IgG to Fcγ receptors on the APC (Fig. 2B). Binding of activated complement to complement receptors on APC may further increase the targeting of the anti-Gal/S-proteinα gal immune complexes to APC. Previous studies with inactivated influenza virus and recombinant HIV-gp120 vaccines glycoengineered to present α-gal epitopes [27], [28], [29], [30] strongly suggest that S-proteinα gal vaccine or inactivated SARS-CoV-2α gal vaccine will be much more effective in eliciting protective immune response against Covid-19 than the same vaccines having the original glycan-shield.
Fig. 2.
Anti-Gal mediated targeting of SARS-CoV-2 S-proteintoAPC. A. The negative charges of sialic acids (SA) on the glycan-shield of the S-protein and on APC surface glycoproteins and glycolipids generate electrostatic repulsion (ζ [zeta]-potential) between the SARS-CoV-2 inactivated virus or S-protein vaccines and the APC. This repulsion decreases the uptake by random endocytosis of the negatively charged vaccine into the APC. B. Synthesis of α-gal epitopes on the glycan-shield of S-protein (S-proteinαgal) eliminates the electrostatic repulsion and enables binding of the natural anti-Gal IgG antibody to the S-proteinαgal and formation of anti-Gal/S-proteinαgal immune complexes. These immune complexes are effectively targeted for binding to the Fcγ receptors (FcγR) on APC, further resulting in extensive active uptake of the vaccine by APC. Modified from [26].
2. Formation of immunocomplexes by viral vaccines and the natural anti-Gal antibody
Amplification of vaccine immunogenicity by immunocomplexing with the corresponding antibody has been a phenomenon known for more than 50 years. Marked increase in the immune response to immunocomplexed antigens was observed with tetanus toxoid [31], [32], hepatitis B antigen [33], Eastern equine encephalitis virus [34] and simian immunodeficiency virus vaccine studied in monkeys (SIV) [35]. Immunization with each of these vaccines immunocomplexed with the corresponding antibody increased the immune response by 10–1000-fold in comparison to the same vaccine that was delivered without an immunocomplexing antibody. With the understanding of the role of dendritic cells and macrophages as APC, it became evident that vaccines administered as immune complexes are targeted to APC by Fc/Fcγ receptors interaction [32], [33], [34], [35], [36], [37]. This interaction was also found to further induce differentiation and maturation of the APC into professional APC that effectively present immunogenic peptides, both on class I and class II MHC molecules for effective activation of CD8+ and CD4+ T cells, respectively [38], [39]. This method for amplifying immunogenicity of vaccines by immunocomplexing is regarded impractical for clinical immunization because of the technical difficulties associated with ex vivo preparation of immune complexes with the corresponding antibodies and the problems in vaccines associated with the use of antibodies from human donors or from other mammalian sources. However, this method is clinically feasible if the immunocomplexes are formed in situ at the vaccination site with a pre-existing natural antibody within the vaccinated individual. A natural antibody that is present in large amounts in all humans who are not severely immunocompromised and which can form immune complexes in situ with vaccinating glycoproteins and with inactivated enveloped virus vaccines is the natural anti-Gal antibody.
Anti-Gal is a polyclonal natural antibody constituting ~1% of IgG in human serum [40], [41]. It is produced also as IgM and IgA antibodies and is abundant as IgA antibodies in various secretions such as milk, colostrum, saliva and bile [42]. This antibody is continuously produced throughout life as a result of antigenic stimulation by several strains of gastrointestinal bacteria [43], [44], [45]. Anti-Gal binds specifically to a carbohydrate antigen called the “α-gal epitope” with the structure Galα1-3Galβ1-4GlcNAc-R (epitope in the rectangle on the right glycan in Fig. 1) [41], [46], [47]. The α-gal epitope is abundantly produced in nonprimate mammals, lemurs and New-World monkeys (monkeys of South-America), on cell membrane glycans [48], [49] and on secreted glycoproteins [50], [51]. In contrast, Old-World monkeys (monkeys of Asia and Africa), apes and humans, all completely lack α-gal epitopes [48], [49], [50], [51] because of inactivation in ancestral Old-World primates of the α1,3galactosyltransferase (α1,3GT) gene (also called GGTA1) encoding the α1,3GT enzyme that synthesized the α-gal epitope [52], [53]. However, similar to humans, Old-World monkeys and apes produce the natural anti-Gal antibody [40], [41], [48], [54]. Because of the ubiquitous presence of anti-Gal in large amounts in humans and because the α-gal epitope can be readily synthesized or obtained, the immunologic potential of this antibody may be harnessed for a number of immunotherapies in several clinical settings [26], [41].
The glycans on glycoproteins of enveloped viruses are synthesized by the glycosylation machinery within various compartments of the Golgi apparatus in host cells, in a manner similar to an assembly line in a car plant. Various glycosyltransferases add carbohydrate units to the nascent carbohydrate chain in a sequential order. Therefore, viruses produced in nonprimate mammalian cells present both α-gal epitopes and sialic acid on their glycans (right and left glycans, respectively in Fig. 1) [55], [56], [57], [58], [59], [60], [61], [62], [63]. In contrast, when produced in Old-World monkey, ape and human cells, the same viruses lack α-gal epitopes and present glycans capped with sialic acid (left chain in Fig. 1) and other carbohydrates, according to glycosyltransferases content of the host cell. Anti-Gal in human serum effectively binds to α-gal epitopes on virus envelope glycoproteins, neutralizes these viruses and destroys the envelope of the viruses by activation of the complement system [56], [57], [58], [59], [60], [61], [62], [63].
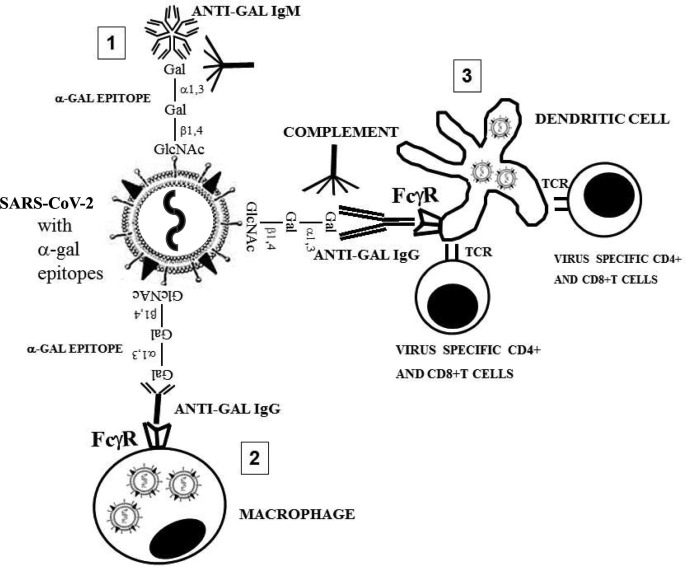
The ability of anti-Gal to form immunocomplexes with α-gal epitopes on viral envelope glycoproteins raised the assumption that vaccines in the form of inactivated virus, split, subunit, or recombinant viral glycoprotein may be glycoengineered to present α-gal epitopes on their glycans [64], [65]. It was hypothesized that these α-gal epitopes will eliminate the electrostatic repulsion by sialic acid on APC glycans and enable harnessing anti-Gal for targeting viral vaccines to APC as a result of binding of the Fc portion of the immunocomplexed anti-Gal to Fcγ receptors on the APC (Fig. 2). The sequence of events anticipated to occur following immunization with an inactivated virus presenting multiple α-gal epitopes is illustrated in Fig. 3 with inactivated SARS-CoV-2 as a hypothetical example. Step 1- Administration of inactivated virus or viral envelope glycoprotein vaccines presenting α-gal epitopes into humans will result in rapid formation of immune complexes with the natural anti-Gal antibody of the vaccinated individual. These immune complexes will activate the complement system for the formation of chemotactic complement cleavage peptides (e.g. C5a) that induce rapid recruitment of APC as dendritic cells and macrophages to the immunization sites, as observed in tumors converted into vaccines by intratumoral injection of α-gal glycolipids [66]. Step 2- Upon arrival to the vaccination site, the Fcγ receptors on these APC will bind the Fc portion of the immunocomplexed anti-Gal. This interaction will induce active endocytosis of the immunocomplexed vaccine. The C3b complement component attaching to the immunocomplexed anti-Gal, binds to C3b receptors (CR1) on APC and also induces uptake of the opsonized virus by these cells. Step 3- The uptake of the vaccine will be followed by processing and presentation of the immunogenic peptides on MHC molecules of the APC, maturation of the APC into professional APC and transport of the presented immunogenic peptides to regional lymph nodes. In the lymph nodes, the presented viral peptides will activate specific T cells with the corresponding T cell receptors (TCR) to proliferate and initiate effective anti-virus T cell and antibody immune response.
Fig. 3.
Suggested mechanism for amplification of SARS-CoV-2αgal vaccine immunogenicity by anti-Gal mediated targeting to APC. Inactivated SARS-CoV-2 presenting α-gal epitopes (SARS-CoV-2αgal) is used as a vaccine example. Step 1- Anti-Gal IgM and IgG bind to α-gal epitopes on the vaccinating virus at the vaccination site, activate the complement system which generates complement cleavage chemotactic peptides that recruit APC such as dendritic cells and macrophages. Step 2- Anti-Gal IgG coating the virus targets it for active extensive uptake by the recruited dendritic cells and macrophages, via Fc/Fcγ receptors (FcγR) interaction. Step 3- These APC transport the internalized virus vaccine to the regional lymph nodes and process the virus antigens. Within the lymph nodes, the APC present the immunogenic virus peptides on class I and class II MHC molecules for the activation of SARS-CoV-2 specific CD8 + and CD4 + T cells, respectively. TCR- T cell receptor. Modified from [26].
3. Increased immunogenicity of ovalbumin as a model vaccine
The proposed mechanism presented in Fig. 3 could be studied in knockout mice in which the α1,3GT gene (GGTA1) was disrupted (i.e., knocked out) [67]. These mice (called GT-KO mice) lack the α-gal epitope and thus can be induced to produce anti-Gal by immunization with xenogeneic tissues (e.g. porcine kidney homogenate) which contain high concentration of α-gal epitopes [66], [68]. Chicken ovalbumin (OVA) was used as the vaccine model that simulates a viral vaccine [30] since the most immunogenic peptide of OVA for CD8+ T cells was identified as the 8-amino acid peptide SIINFEKL [69]. Moreover, a mouse CD8+ T hybridoma cell line B3Z with a TCR specific for SIINFEKL was generated [70]. These B3Z cells are activated when they engage APC presenting SIINFEKL. This activation can be detected by β-galactosidase transgene LacZ under IL2 promoter. The activated LacZ transgene produces detectable β-galactosidase following engaging of the TCR on B3Z cells with SIINFEKL on MHC class I of H-2bKb of APC [70]. The OVA protein lacks N-linked glycans and thus, cannot be glycoengineered to carry α-gal epitopes. Therefore, anti-Gal mediated targeting of OVA to APC was studied with OVA encapsulated within liposomes that present multiple α-gal epitopes [30]. These liposomes mimic a virus presenting multiple α-gal epitopes, as that illustrated in Fig. 3.
Migration to regional (inguinal) lymph nodes of APC that internalized OVA encapsulated α-gal liposomes, was studied 7 days post injection of these liposomes into the thigh. APC presenting SIINFEKL were detected by coincubation of lymph node cells with B3Z T hybridoma cells for 20 h followed by flow cytometry analysis of β-galactosidase elevated production in activated B3Z cells. Such activation of B3Z cells was 5–8 fold higher in mice producing anti-Gal than in mice lacking the antibody [30]. This implied that many more APC internalizing and processing the OVA containing α-gal liposomes were migrating from the injection site to the regional lymph nodes in mice producing anti-Gal than in mice lacking this antibody. ELISPOT analysis of spleens from the immunized mice were studied for the presence of SIINFEKL specific CD8+ T cells 14 days post injection. This analysis demonstrated 15-fold higher number of SIINFEKL activated T cells in anti-Gal producing mice, than spleens of mice lacking the anti-Gal antibody. Moreover, mice producing anti-Gal displayed 30–100 fold higher titers of anti-OVA antibodies than mice lacking anti-Gal but receiving a similar vaccine of OVA encapsulate in α-gal liposomes [30]. These studies imply that immunocomplexing of anti-Gal with vaccines presenting α-gal epitopes greatly amplifies the cellular and antibody immune response to the vaccinating antigen. This is achieved by increased uptake of the immunocomplexed vaccine by APC via Fc/Fcγ receptors and possibly C3b/CR1 receptor interactions which is followed by increased processing of the vaccine within the APC and transport of the processed vaccine to the regional lymph-nodes. In the lymph nodes, the increased transport and processing of the vaccine by APC is followed by increased activation of the vaccine specific T and B cells. These studies on amplified immunogenicity of OVA encapsulated in α-gal liposomes suggest that it would be of interest to determine whether various Covid-19 vaccines containing S-protein display amplified immunogenicity by glycoengineering them to present α-gal epitopes. This suggestion is supported by studies described below, indicating that in situ immunocomplexing of anti-Gal with inactivated influenza virus and with recombinant HIV-gp120 vaccines that were glycoengineered to present α-gal epitopes results in much higher immunogenicity than original viral vaccines lacking this epitope.
4. Anti-viral protective immune response with α-gal influenza virus vaccine
A model which has been used for determining changes in immunogenicity of inactivated whole virus vaccine glycoengineered to present α-gal epitopes was that of influenza virus [28]. The hemagglutinin (HA) glycoprotein on influenza virus has the same role as S-protein on coronavirus in that it attaches the virus to cell membrane. HA uses sialic acid on cell glycans as “docking” receptor and has 5–7 N-linked carbohydrate chains of the complex type which have the terminal structure Galβ1-4GlcNAc-R, without capping sialic acid, as the center glycan in Fig. 1 [71], [72]. The sialic acid is removed by the viral neuraminidase on the envelope in order to prevent HA mediated adhesion between the virions. The influenza virus strain studied as vaccine was A/Puerto Rico/8/34- H1N1 (PR8 virus). The virus was produced in embryonated eggs and was inactivated by heat. α-Gal epitopes were synthesized on the N-linked glycans of the complex type of HA on PR8 virus by recombinant α1,3galactosyltransferase (rα1,3GT) using uridine-diphosphate-galactose (UDP-Gal) as sugar donor and in the presence of Mn++ ions, as illustrated in the second enzymatic reaction in Fig. 1 [28], [65]. Quantification of the de novo synthesized α-gal epitopes indicated that ~3000 such epitopes were synthesized on each virion [65]. The inactivated PR8 virus glycoengineered to present α-gal epitopes is referred to as PR8αgal vaccine whereas the control inactivated virus lacking α-gal epitopes is referred to as PR8 vaccine.
Anti-Gal producing GT-KO mice received two immunizations in two-week interval with either 1 μg of PR8αgal vaccine, or with a similar amount of PR8 vaccine. These immunizations were performed with Ribi (trehalose dicorynomycolate) adjuvant. Production of anti-PR8 antibodies and activation of T cells against virus antigens were assayed two weeks after the second immunization [28]. Analysis of T cell response to PR8 virus antigens by ELISPOT measuring IFNγ secretion, demonstrated ~4-fold increase in T cells from spleens of the majority of mice immunized with PR8αgal in comparison to those immunized with PR8. Intracellular cytokine staining for IFNγ detected 6-fold increase in CD8+ T cells from most PR8αgal immunized mice vs. PR8 immunized mice, and >100 fold IFNγ stained CD4+ T cells in the former vs. the latter group. Anti-PR8 antibody production in the immunized mice was assayed by ELISA with PR8 virus as solid phase antigen. The titer of IgG and IgA anti-PR8 antibodies in PR8αgal immunized GT-KO mice was found to be on average ~100 fold higher than that in PR8 immunized mice. Anti-PR8 IgA antibodies were also found in lung lavage of PR8αgal immunized GT-KO mice, but not in the lavage of PR8 immunized mice. The much higher production of anti-PR8 antibodies in PR8αgal immunized mice was dependent on the presence of anti-Gal in the mice for targeting the vaccinating inactivated virus to APC. In the absence of anti-Gal (i.e. immunization of wild-type [WT] mice that are immunotolerant to the α-gal epitope), no differences in production of anti-PR8 antibodies were observed between mice immunized with PR8αgal and PR8 vaccines. Both groups of WT mice displayed ~100 fold lower production of anti-PR8 antibodies than GT-KO mice receiving PR8αgal vaccine. In neutralization plaque assays of PR8 virus with Madin-Darby canine kidney (MDCK) cells, sera from PR8αgal immunized GT-KO mice displayed ~20 fold higher neutralizing anti-PR8 activity (i.e. prevention of MDCK cell lysis) than sera from PR8 immunized mice.
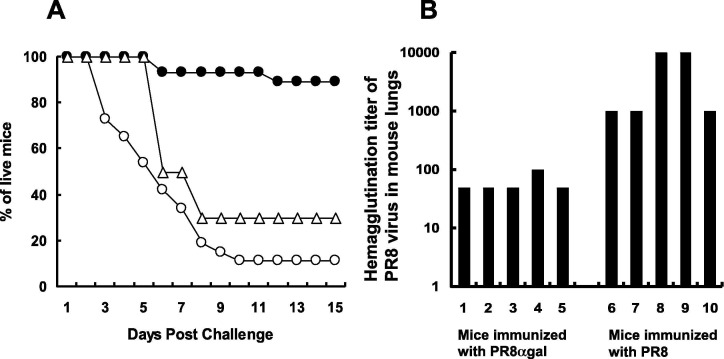
The protective efficacy of PR8αgal vaccine vs. PR8 vaccine was further evaluated in challenge studies by intranasal infection with a lethal dose (2000 plaque forming units [PFU]) of live PR8 virus. The survival among mice immunized with PR8αgal vaccine was 8-fold higher than in mice immunized with PR8 vaccine (Fig. 4 A). In WT mice immunized with PR8αgal, survival was much lower than in GT-KO mice receiving this vaccine, implying that the protective effects of PR8αgal virus vaccine require the present of the anti-Gal antibody. Survival data on Day 30 were the same as those on Day 15 post challenge. In parallel studies, mice immunized with PR8αgal or with PR8 vaccines were euthanized 3 days after the challenge with the lethal dose of live PR8 virus. Lungs of these mice were homogenized and supernatants of the homogenates measured for virus titer by hemagglutination of chicken red blood cells. In accord with the much higher survival of GT-KO mice immunized with PR8αgal, the dose of PR8 virus in the lungs of these mice was 10 to 100 fold lower than that measured in lungs of GT-KO mice receiving the PR8 vaccine (Fig. 4B). These findings with the inactivated influenza virus vaccine [28] suggest that glycoengineering of SARS-CoV-2 virus glycan-shield to present α-gal epitopes may result in increased efficacy of vaccines due to immunocomplexing with anti-Gal followed by targeting of the inactivated virus for extensive uptake by APC.
Fig. 4.
Protection against intranasal infection by a lethal dose of PR8 influenza virus in mice immunized with inactivated PR8 or PR8αgal virus. A. Survival of mice immunized twice with 1 μg inactivated PR8 vaccine (○) in GT-KO mice; PR8αgal (●) vaccine in GT-KO mice; or with PR8αgal (△) vaccine in wild-type mice. The mice were challenged with 2000 PFU of live PR8 in 50 μl (n = 25 per group). Survival data are presented as % of live mice at various days following the challenge. Survival results on Day 30 were similar to those on Day 15 post challenge. B. PR8 virus titers in lungs of GT-KO mice, 3 days after challenge with live virus. The virus titers were assayed in supernatants of lung homogenates from the immunized mice, by hemagglutination of chicken red blood cells (n = 5 per group). Modified from [28].
5. Amplified anti-gp120 immune response with gp120αgal vaccines
Recombinant gp120 of HIV produced in CHO cells containing the gp120 transgene served as a model for a recombinant envelope virus glycoprotein vaccine glycoengineered to present α-gal epitopes [27]. α-Gal epitope synthesis on gp120 was achieved in the two-step enzymatic reaction illustrated in Fig. 1, with neuraminidase and rα1,3GT. The two enzymatic reactions can be performed within the same solution. First, neuraminidase cleaves sialic acid from the glycans of the complex type on gp120. As indicated above, there are 13–16 such N-linked glycans on this envelope glycoprotein [24], [25]. Subsequently, rα1,3GT links galactose provided by high energy UDP-Gal to the desialylated glycan to form the α-gal epitope and generate gp120αgal. Gp120αgal was isolated from the reaction mixture by an affinity agarose column coupled with the lectin Bandeiraea (Griffonia) simplicifolia IB4 which binds specifically α-gal epitopes [73].
Gp120αgal immunogenicity was evaluated in anti-Gal producing GT-KO mice that were immunized twice in one-week interval with 5 μg gp120 or gp120αgal and Ribi adjuvant [27]. Anti-gp120 immune response was measured 17 days after the second injection to determine whether anti-Gal/gp120αgal immune complexes targeted to Fcγ receptors on dendritic cells and macrophages elicit a higher immune response than gp120. ELISA with gp120 as solid-phase antigen demonstrated ~200 fold higher anti-gp120 antibody titers in mice immunized with gp120αgal in comparison to mice immunized with gp120. However, low anti-gp120 antibody production (as that in GT-KO mice immunized with gp120) was found in WT mice (lacking anti-Gal despite immunizations with pig kidney membranes) immunized with either vaccines, further demonstrating the significance of anti-Gal in targeting gp120αgal to APC. The anti-gp120 antibodies produced following immunization of GT-KO mice with gp120αgal were further found to effectively neutralize HIV-1 strain MN (a strains convenient for manipulation in the lab) and thus, to prevent infection of host cells [27]. This neutralizing activity was determined by the extent of killing inhibition of the human T cell lymphoma MT-2 cells by the virus [74], [75]. No such neutralizing activity was found in sera from gp120 immunized GT-KO mice.
Immunization of anti-Gal producing GT-KO mice with gp120αgal also amplified gp120 specific T cell response in comparison to immunization with similar amount of gp120 vaccine. This was indicated by the ~15-fold higher number of IFNγ secreting T cells among splenocytes of gp120αgal immunized mice in ELISPOT assays with dendritic cells pulsed with gp120 [27]. Overall, the increased antibody and T cells responses in mice immunized with the recombinant gp120αgal vs. gp120 is similar to the increased immune response observed with PR8αgal vaccine vs. PR8 vaccine. These findings suggest that replacing the sialic acid of S-protein split, subunit, or recombinant vaccines with α-gal epitopes to form S-proteinαgal may markedly increase the immunogenicity of this glycoprotein, similar to the increase in vaccine potency observe with gp120αgal of HIV.
6. Efficacy of gp120αgal/p24 fusion protein vaccine
Fusion proteins between gp120αgal and vaccinating viral proteins lacking glycans was found to increase the immunogenicity of viral proteins with low immunogenicity, suggesting that S-protein of SARS-CoV-2 may fulfill a similar role. Gp120 of HIV is capable of mutating during infections, thus enabling the virus to evade the detrimental effects of neutralizing antibodies. For this reason, vaccination only with gp120 was reported not to induce a sufficient immune resistance to HIV infections in large populations [19], [20], [76], [77]. Therefore, there is the interest in developing effective vaccines against HIV internal proteins such as tat, rev, p17 or p24, which do not mutate in course of HIV infection and do not have glycans. Such vaccines may elicit a cellular immune response which effectively destroys HIV infected cells. However, because of poor targeting to APC, immunogenicity of these proteins may be low. Since these proteins are not glycosylated, studies were performed to determine whether vaccine made of a fusion protein between gp120αgal and one of the non-glycosylated, nonmutating internal HIV protein scan increase their immunogenicity. The core protein p24 was chosen as a model protein for this analysis [29]. A fusion protein gp120/p24 was produced by ligation of the gene regions of env coding for gp120 and of gag coding for p24. The fused gene was inserted into a plasmid containing a strong promoter (CMV) and the fusion product gp120/p24 was produced by transient transfection of 293 cells. Following the isolation of the secreted gp120/p24 fusion protein, it was glycoengineered into gp120αgal/p24 vaccine presenting multiple α-gal epitopes, as performed above for production of gp120αgal.
GT-KO mice received in two-week interval two subcutaneous immunizations with gp120/p24 or gp120αgal/p24 at 5 μg per injection, with Ribi adjuvant. The immune response was evaluated two weeks after the second injection. Analysis of T cells specific to p24 was performed by incubation of splenocytes with the p24 immunodominant peptide p24189-207 [78] which pulsed APC among the splenocytes. ELISPOT analysis for IFNγ secretion indicated that the number of p24 specific T cells among lymphocytes from gp120αgal/p24 immunized mice was ~12 fold higher than in gp120/p24 immunized mice [29]. Accordingly, flow cytometry analysis indicated that the number of p24 specific CD8+ T with intracellular staining of IFNγ in mice immunized with gp120αgal/p24 was 5–20-fold higher than in mice immunized with gp120/p24. Mice immunized with gp120αgal/p24 further demonstrated by ELISA with gp120 as solid-phase antigen a ~30-fold higher anti-gp120 antibody titer than mice immunized with gp120/p24. These observations suggest that the use of a fusion protein vaccine in which only gp120 portion presented α-gal epitopes, resulted in anti-Gal mediated increase in immunogenicity of both gp120 and p24 although the latter protein within the fusion protein vaccine lacks glycans. The studies on gp120αgal/p24 [29] suggest that S-proteinαgal may be considered in future vaccines as a similar platform for effective targeting to APC of internal SARS-CoV-2 proteins, if this virus displays evasion from protective immune response due to mutations in future epidemics. Such vaccines may elicit an effective anti-viral T cell response, as well as a protective antibody response against the mutated S-protein. A similar approach may be considered for production of influenza vaccines containing a fusion protein between HA and the M2 proton channel since M2 is nearly invariant in all influenza A strains [79], [80].
7. Differences in immunogenicity between vaccines immunocomplexed with specific anti-protein antibody and those immunocomplexed with anti-Gal
Anti-Gal immunocomplexed in situ at the vaccination site or in vitro with a glycoprotein vaccine such as gp120αgal [27], or BSAαgal [81] display a much higher processing and presentation by APC than non-immunocomplexed vaccine, as determined by activation of T cells with antigenic peptides presented on APC. A similar marked increase in activation of T cells was observed with vaccinating proteins immunocomplexed with the corresponding anti-protein antibodies [32], [33], [34], [35], [36], [37], [38], [39]. However, when the immunocomplexes are formed in the presence of excessive amounts of anti-protein antibodies, the T cell activation and antibody production were both found to diminish although the extensive uptake of the immune complexes by APC was not affected [32], [82]. Two of the reasons for this great decrease in the immune response to vaccinating antibody/protein immune complexes are: 1. Anti-protein antibody binding to the corresponding peptide epitopes is of high affinity because of involvement of ionic bonds with charged amino acids such as lysine and glutamic acid. Therefore, the dissociation of the multiple antibody molecules bound to protein vaccines is greatly decreased in the pH ~ 5 within the endosomes. This decreased dissociation prevents effective proteolytic degradation of the protein molecule within the immune complex in the lysosome, thus diminishing further antigen processing within the APC [32]. 2. The multiple antibody molecules bound to peptide epitopes mask the immunogenic peptides on the vaccine and prevent interaction of these peptides with the corresponding B cell receptors. These limiting factors are not applicable to the anti-Gal/glycoprotein immune complexes because the affinity of this antibody to the α-gal epitope is relatively low (105–106M−1) [83]. This low affinity is a result of the absence of electrostatic charges in the α-gal epitope thus, the immune complex taken up by APC readily dissociates in the low pH of endosomes, enabling effective proteolysis of the vaccine. In addition, anti-Gal is bound to the glycan of the vaccinating glycoprotein rather than to peptides, thus it does not mask the immunogenic peptides and does not prevent their interaction with the corresponding B cell receptors. Based on these considerations it may be assumed that although anti-Gal titers may vary from one individual to the other, amplification of immunogenicity of glycoengineered S-proteinαgal or SARS-CoV-2αgal virus vaccines will likely to occur also in individuals producing anti-Gal at very high titers.
8. Similarities between mouse and human anti-Gal antibodies
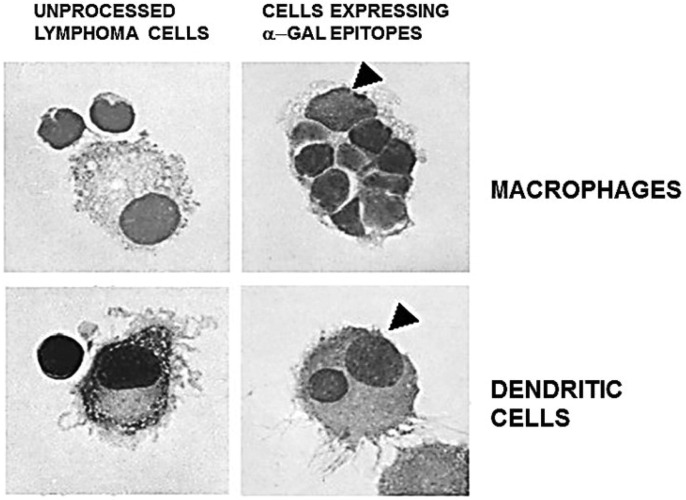
Anti-Gal in GT-KO mice was found to bind effectively to α-gal epitopes on viruses, induce targeting of the immunocomplexed virus to APC via Fc/Fcγ receptor interaction for extensive uptake of viral vaccines by the APC and thus, greatly increases the elicited protective anti-virus immune response in comparison to viral vaccines lacking α-gal epitopes [27], [28], [29], [30]. A similar anti-Gal mediated increased immunogenicity inducing protection against development of distant metastases was observed in tumors engineered to present α-gal epitopes in anti-Gal producing GT-KO mice [66], [84], [85]. These observations raise the question whether anti-Gal in humans may display effects similar to those of mouse anti-Gal. Although no direct parallel information has been achieved in human studies, the following experimental observations demonstrate activity of human anti-Gal similar to that described above for mouse anti-Gal: 1. Titer of anti-Gal in humans- In parallel ELISA studies with human and GT-KO mouse sera, using synthetic α-gal epitopes as solid-phase antigen, both demonstrated similar titers of anti-Gal (1:160–1:320) [27]. 2. Binding to viral α-gal epitopes- Natural anti-Gal antibody isolated from human serum was shown to bind to α-gal epitopes on glycoengineered influenza virus HA, similar to the binding of anti-Gal isolated from the serum of GT-KO mice producing this antibody [27], [65]. Accordingly, anti-Gal in human serum was found to bind and induce complement dependent virolysis of Friend Murine Leukemia Virus, porcine endogenous retrovirus (PERV), pseudo-rabies virus, rhabdo-, lenti-, and spumaviruses, Newcastle disease virus, Sindbis virus, vesicular stomatitis virus, measles virus and vaccinia virus, all replicating in cells containing active α1,3GT [56], [57], [58], [59], [60], [61], [62], [63]. 3. Increased uptake by APC- The major step in anti-Gal mediated increased immunogenicity of viral vaccines is the extensive uptake by APC via Fc/Fc receptor interaction of the virus vaccine immunocomplexed with anti-Gal (Fig. 2, Fig. 3). The ability of human anti-Gal to induce such an extensive uptake of vaccine was visualized with freshly obtained human lymphoma cells that were glycoengineered to present α-gal epitopes (by the use of recombinant α1,3GT, as described in Fig. 1). Macrophage and dendritic cell APC were obtained from the same lymphoma patient. The original and glycoengineered lymphoma cells were incubated with autologous anti-Gal and with macrophages and dendritic cells for 2 h, stained and evaluated microscopically for phagocytosis by the APC [86]. Anti-Gal bound to the glycoengineered lymphoma cells but not to the original (i.e. non-engineered) lymphoma cells lacking α-gal epitopes. Moreover, anti-Gal binding to α-gal epitopes on the glycoengineered tumor cells induced their extensive uptake by macrophages and to a lesser extent by dendritic cells (Fig. 5 ). As many as 70% of macrophages and 25% of dendritic cells displayed phagocytosis of the anti-Gal opsonized lymphoma cells, whereas no original lymphoma cells were taken up by macrophages or dendritic cells. The uptake by macrophages of anti-Gal opsonized lymphoma cells could be inhibited by anti-CD64 but not by anti-CD32 or anti-CD16 antibodies, implying that the uptake is mediate by high affinity FcγI receptor [86]. This high affinity FcγI receptor was reported to be present on human dendritic cells, as well [87]. 4. Increased processing and presentation by APC of viruses immunocomplexed with human anti-Gal - Co-incubation of influenza virus presenting α-gal epitopes with anti-Gal purified from normal human serum, with irradiated mouse spleen cells as APC and with mouse T cell clones with TCR specific for HA peptides, resulted in 8-fold higher proliferation of the T cells than in the absence of anti-Gal [64]. This implies that formation of immune complexes between human anti-Gal and influenza virions presenting α-gal epitopes resulted in much higher uptake, processing and presentation of antigenic viral peptides than in the absence of human anti-Gal. Similar observations were reported in studies on measles virus presenting α-gal epitopes and co-incubated with human anti-Gal, human dendritic cells and autologous T cells. The proliferation of T cells in response to measle virus peptides presented by the dendritic cells was much higher when the virus was immunocomplexed with the human anti-Gal than in the absence of anti-Gal [61]. Overall, the studies in this section indicate that human anti-Gal binds to α-gal epitopes on glycoengineered virus as well as GT-KO mouse anti-Gal. Furthermore, the immune complexes with human anti-Gal can induce extensive uptake, processing and presentation of α-gal presenting viral vaccine at levels much higher than the same vaccine lacking these epitopes. Thus, it is likely that anti-Gal mediated amplification of viral vaccine immunogenicity observed in GT-KO mice [27], [28], [29], [30] may also occur in humans immunized with viral vaccines glycoengineered to present α-gal epitopes.
Fig. 5.
In vitro demonstration of anti-Gal mediated uptake of human B lymphoma cells by autologous APC. Human fresh lymphoma cells (B cell lymphoma) were glycoengineered to present α-gal epitopes by incubation with neuraminidase, recombinant α1,3galactosyltranferase and UDP-Gal (as illustrated in Fig. 1). Lymphoma cells presenting α-gal epitopes or lacking this epitope (i.e. original cells) were incubated with autologous anti-Gal for 30 min, subsequently, for 2 h at 37 °C with autologous macrophages or dendritic cells, then washed and subjected to staining. Arrowheads mark nuclei of the APC. Note the uptake of 9 lymphoma cells presenting α-gal epitopes by the macrophage and one lymphoma cell by the dendritic cell. No uptake of lymphoma cells lacking α-gal epitopes was observed (May Grünwald Giemsa staining, ×1000). Adapted with permission from Manches et al., 2005 [86].
9. Glycoengineering of α-gal epitopes on SARS-CoV-2 vaccines
Some of the methods which may be considered for glycoengineering SARS-CoV-2 or its S-protein to present α-gal epitopes are the following:
9.1. Synthesis of α-gal epitopes by recombinant α1,3galactosyltransferase
The studies described above on synthesis of α-gal epitopes on PR8 influenza virus and on gp120 of HIV were performed with recombinant α1,3galactosyltransferase (rα1,3GT) encoded by the marmoset (New-World monkey) α1,3GT gene (GGTA1) [88]. Truncated cDNA lacking both cytoplasmic and trans-membrane domains and carrying a (His)6 tag was produced in transformed yeast expression system (Pichia pastoris). The secreted enzyme was isolated by affinity purification of rα1,3GT on a nickel-Sepharose column and elution with imidazole [89]. This enzyme links the galactose from the UDP-Gal sugar donor to the glycans of desialylated glycoproteins and glycolipids to form α-gal epitopes (Fig. 1). The formation of multiple α-gal epitopes by rα1,3GT was observed on human tumor cells [89], [90], [91], on influenza virus [28], [65], and on gp120 of HIV [27], [29]. Synthesis of α-gal epitopes on human tumor cell membranes by the enzymatic reactions in Fig. 1 was also reported by the use of bovine rα1,3GT [92], [93], [94]. In these studies, α-gal epitopes were synthesized on tumor cell membranes of human hepatocellular carcinoma, pancreatic carcinoma and lymphoma, and shown to be effectively targeted by anti-Gal to autologous dendritic cells. The dendritic cells with internalized tumor membranes were used as autologous vaccines in cancer patients and were found to elicit a robust immune response against autologous tumor antigens.
Production of rα1,3GT for the synthesis of α-gal epitopes on glycan was also feasible in the expression system of Sf9 insect cells transfected with virus containing the α1,3GT cDNA [65], [95]. It is of note that isolation on affinity columns of subunit or recombinant S-protein that presents α-gal epitopes (S-proteinαgal) from the reaction mixture of neuraminidase, rα13GT and UDP-Gal is a relatively easy process because of the effective binding of α-gal epitopes to the Bandeiraea simplicifolia IB4 lectin [73]. Only S-protein with linked α-gal epitopes will bind to a column of this lectin attached to Sepharose beads or any other type of porous beads, and the rest of the molecules and ions in the reaction mixture will pass through. The bound S-proteinαgal can be detached from such columns by applying α-methyl galactoside (100 mM) solution [27].
9.2. Intracellular synthesis of α-gal epitopes on SARS-CoV-2 virus
Synthesis of α-gal epitopes on SARS-CoV-2 may be achieved within cells in which the virus is replicating. The synthesis of α-gal epitopes within the trans-Golgi apparatus of nonprimate mammalian cells is similar to the second reaction illustrated in Fig. 1. Accordingly, influenza virus propagated in Madin-Darby bovine kidney cells (MDBK) or Madin-Darby canine kidney cells (MDCK) presents α-gal epitopes on its HA glycoprotein, since both cell types have active α1,3GT enzyme [64]. However, virus replicating in MDCK cells has markedly fewer α-gal epitopes on the glycan-shield than the same virus replicating in MDBK cells. Therefore, anti-Gal mediated targeting to APC of influenza virus replicating in MDBK cells, as measured by specific T cell activation was ~8 fold higher than that of the same virus produced in MDCK cells [64]. As discussed below, the reason for these differences is the different α1,3GT activity and the extent of competition of this enzyme with sialyltransferases in these two cell lines. In contrast, influenza virus propagated in chicken cells lacks α-gal epitopes since the α1,3GT gene appeared in early stages of mammalian evolution and it is absent in birds and other nonmammalian vertebrates [48], [49]. Similarly, Eastern equine encephalitis virus propagated in mouse cells presents α-gal epitopes whereas the same virus propagated in Vero cells (Old World monkey cells) lacks these epitopes [55] because the α1,3GT gene is inactivated in Old-World monkeys, apes and humans [48], [49], [52]. These observations suggest that some of the glycans on SARS-CoV-2 virus propagated in cells containing active α1,3GT will be synthesized with α-gal epitopes. Indeed, after stable transfection with the α1,3GT gene, even cells lacking α-gal epitope start synthesizing this epitope on cell surface glycans [84], [85]. The glycosyltransferases α1,3GT and sialyltransferases compete within the trans-Golgi compartment of host cells for capping the nascent complex type glycan with Galα1-3- to form the α-gal epitope (right glycan in Fig. 1) or with sialic acid (SA)α2-3-, or SAα2,6- to form the left glycan in Fig. 1 on both cellular and viral glycoproteins [96]. The reduced presentation of α-gal epitopes due to this competition and possibly low production of α1,3GT may explain the low immunogenicity of subunit vaccine prepared of influenza virus propagated in MDCK cells, which does not differ from that produced of virus propagated in embryonated eggs [97], [98]. Although MDCK cells contain active α1,3GT, the number of α-gal epitopes on the virus is several fold lower than that on influenza virus replicating in MDBK cells [64]. Since there are only 5–7 N-linked glycans on influenza virus HA, it is possible that because of low α1,3GT activity and high activity of competing sialyltransferases, there is less than one α-gal epitope per MDCK HA molecule. Accordingly, the efficacy of this vaccine in humans does not differ from that prepared from virus grown in embryonated eggs, which completely lacks α-gal epitopes [97], [98]. In view of these considerations, it is reasonable to assume that the efficacy of targeting vaccines to APC by anti-Gal is directly proportional to the number of α-gal epitopes on inactivated SARS-CoV-2 or on S-protein subunit vaccines.
Maximizing α-gal epitope synthesis on a virus such as SARS-CoV-2 replicating in a host cell line can be achieved by elevating the activity of α1,3GT, decreasing sialyltransferase activity, or both. For increasing α1,3GT activity, the propagating cells should undergo stable transfection with several copies of the α1,3GT gene (GGTA1) to ensure high production of α1,3GT. Alternatively, the α2-3 sialyltransferase, or α2-6 sialyltransferase genes, or both should be inactivated (i.e. knocked out) in order to minimize or completely prevent competition between sialyltransferases and α1,3GT. Combining the two approaches will maximize the extent of α-gal epitope synthesis on most and possibly all glycans of the complex type in the glycan-shield of the S-protein.
An alternative method which enables introduction of multiple copies of the α1,3GT gene in host cells for SARS-CoV-2 is transduction of such cells with replication defective adenovirus containing the α1,3GT gene (AdαGT) [99], prior to infection of the cells with replicating SARS-CoV-2. Transduction of human HeLa cells with AdαGT resulted in introduction of ~20 copies of the α1,3GT gene in < 1 h, appearance of α1,3GT mRNA within 4 h post-transduction and maximum production of α-gal epitopes on cell surface glycans (4x106 epitopes/cell) within 48 h [99]. Active copies of AdαGT were maintained for at least 5 days in proliferating HeLa cells. Thus, transduction of propagating cells with AdαGT, followed few hours later by infection of the cells with SARS-CoV-2 may result in effective synthesis of α-gal epitopes on the replicating virus. Since the number of glycans of the complex type vs. that of high mannose type may vary from one cell line to the other, a cell line producing virus with the highest number of glycans of the complex type may be preferable for intracellular synthesis of α-gal epitopes on SARS-CoV-2. Alternatively, glycoengineering the optimal cell line which lacks high mannose glycans may require the inactivation of gene(s) associated with synthesis of these glycans.
9.3. Synthesis of recombinant S-proteinαgal in glycoengineered yeasts and bacteria
Yeasts are considered an effective expression system for production of recombinant proteins. However, production of therapeutic glycoproteins for injection into humans is limited by the ability of yeasts to synthesize N-linked glycans that are only of the high mannose type. Therapeutic glycoproteins with high mannose N-linked glycans have short half-life in humans. To overcome this limitation, yeasts have been glycoengineered to synthesized humanized glycans which resemble the complex structure of the left glycan in Fig. 1 by introducing the corresponding glycosyltransferase genes into an yeast expression system [100], [101]. It is possible that introducing the α1,3GT gene (GGTA1) into the yeast instead of sialyltransferase gene(s) will result in synthesis of glycans capped with α-gal epitopes on recombinant S-protein and on other recombinant glycoproteins produced in this expression system.
Bacteria such as E. coli may also serve as expression system for production of recombinant S-proteinαgal. The difficulties in secretion of recombinant proteins through the periplasmic space between the inner and outer membranes and subsequently into the culture medium was overcome by the use of a nonionic detergent such as Triton X-100 which enables the release of recombinant proteins to the medium [102]. Alternatively, recombinant protein can be modified for targeting to environments beyond the periplasm, such as the outer membrane, the membrane vesicles and the extracellular medium [103]. Synthesis of α-gal epitope oligosaccharides in E. coli was achieved by engineering this bacterium to produce the sequence of mammalian glycosyltransferases including α1,3GT [104], [105]. In addition, E. coli was engineered to synthesize N-linked glycans by transfer into it an N-linked glycosylation system found in Campylobacter jejuni [103], [106]. Integrating these various systems in E. coli may enable the effective production of S-proteinαgal in a bacterial expression system.
10. Experimental animal models for SARS-CoV-2αgal and S-proteinαgal vaccines
Amplification of SARS-CoV-2αgal and S-proteinαgal immunogenicity can be studied only in experimental animal models that lack α-gal epitopes and thus, are capable of producing anti-Gal. The two nonprimate mammals suitable for such studies are GT-KO mice [67], [107] and GT-KO pigs [108], [109]. In both, the α1,3GT gene was inactivated and thus they do not synthesize α-gal epitopes. GT-KO mice produce anti-Gal following immunization with xenogeneic cell membranes expressing multiple α-gal epitopes such as pig kidney membranes homogenate [28], [66], [68], or rabbit red blood cells [110]. The GT-KO mice are kept under sterile conditions, therefore, production of anti-Gal in them is low because of ineffective colonization of their gastrointestinal tract with bacteria that elicit natural anti-Gal antibody production. GT-KO pigs produce the natural anti-Gal antibody with characteristics similar to those of human anti-Gal [111], [112], [113]. α-Gal vaccines may be studied also in Old-World monkeys such as baboon, rhesus, and cynomolgus monkeys, all lacking α-gal epitopes and producing the natural anti-Gal antibody [48], [49], [54].
11. Safety of α-gal vaccines in humans
A number of clinical trials have suggested that administration of α-gal epitopes into most humans is safe. Porcine heart valves (which present α-gal epitopes) are widely used for replacement of impaired heart valves in elderly patients. In addition, phase I clinical trials in cancer patients receiving intratumoral injection of α-gal glycolipids (for conversion of treated tumor into autologous vaccine) indicated that the treatment is safe with no adverse effects [114], [115]. In addition, injection of autologous tumor membranes processed to present α-gal epitopes and incubated with autologous dendritic cells was found to result in no adverse effects in cancer patients [92], [93], [94]. However, in the recent decade, a small proportion of populations in several continents was found to produce anti-Gal IgE antibodies following the bite of several kinds of ticks (e.g. Ambliomma americanum, mostly in the South of the USA). A proportion of these individuals develop allergic response to α-gal epitopes in meat such as beef and pork, called “α-gal syndrome” [116], [117], [118], [119], [120]. It is suggested that a skin test with an α-gal allergen (e.g. α-gal glycoprotein or glycolipid) may identify such individuals prior to immunization [26]. This analysis was used in a clinical trial with melanoma patients receiving two intratumoral injections of α-gal glycolipids in one-month interval. Prior to the second injection of α-gal glycolipids, patients received an intradermal injection in an extremity with 10 μg of α-gal glycolipids given as 0.1 ml from a concentration of 0.1 mg/ml. The patients were checked for any skin reaction after 1 h and all found to display no allergic reaction [115]. Glycolipids or glycoproteins presenting α-gal epitopes may be considered as test allergens for performing such a skin test prior to the injection of inactivated SARS-CoV-2αgal or S- proteinαgal vaccines. It should be further determined whether intradermal injection of such vaccines to individuals having the α-gal syndrome has any adverse effects which may prevent vaccination with these anti-Covid-19 vaccines.
12. Conclusions
The natural anti-Gal antibody (~1% of human immunoglobulins) may be harnessed for amplification of SARS-CoV-2 vaccine immunogenicity by glycoengineering the glycan-shield of the vaccine to present α-gal epitopes (Galα1-3Galβ1-4GlcNAc-R) which binds anti-Gal. This amplification is the result of targeting anti-Gal/SARS-CoV-2αgal or anti-Gal/S-proteinαgal immune complexes for extensive uptake by APC via Fc/Fcγ receptors interaction and possibly by C3b/CR1 receptors interaction. This amplified immune response may result in markedly higher titers of neutralizing antibodies and increased T cell response against cells infected with SARS-CoV-2, in comparison to vaccines that are not immuncomplexed with anti-Gal. Glycoengineering of inactivated SARS-CoV-2 virus or S-protein vaccines to present multiple α-gal epitopes is feasible either by use of neuraminidase, recombinant α1,3galactosyltransferase and UDP-Gal, or by propagating the virus in cell lines that contain high α1,3galactosyltrase activity. In addition, generation of yeast or bacterial expression systems that are glycoengineered to synthesize α-gal epitopes on glycans will enable production of recombinant S-protein with multiple α-gal epitopes. Similar glycoengineering of inactivated influenza virus vaccine and recombinant HIV-gp120 vaccine was found to increase their immunogenicity in anti-Gal producing mice by 10–200 fold and resulted in effective immune protection against challenge with lethal dose of live influenza virus. Efficacy analysis of the proposed vaccines presenting α-gal epitopes may be performed in anti-Gal producing experimental animal models including mice and pigs lacking α-gal epitopes as a result of the inactivation of the gene encoding for α1,3galactosyltransferase and in Old-World monkeys such as baboon, rhesus, and cynomolgus monkeys. Administration of α-gal epitopes on glycolipids and glycoproteins into most humans was found to be safe. However, the observed allergy to meat associated with production of anti-Gal IgE (called “α-gal syndrome”) in a small number of individuals, may require determination whether anti-Covid-19 vaccines presenting α-gal epitope have any adverse effect in individuals who have the α-gal syndrome.
13. ICMJE criteria
The author attests he meets the ICMJE criteria for authorship.
14. Submission declaration
This manuscript is a review. The information included was previously published in specific manuscripts which are cited correspondingly.
Funding
No organization funded this review.
Declaration of Competing Interest
The author declares the following financial interests/personal relationships which may be considered as potential competing interests: The author is the inventor in US patents 9662383 and 10201601 (Assignee, University of Massachusetts), which include some of the methods described in this review.
References
- 1.Koirala A., Joo Y.J., Khatami A., Chiu C., Britton P.N. Vaccines for COVID-19: The current state of play [published online ahead of print, 2020 Jun 18] Paediatr Respir Rev. 2020 doi: 10.1016/j.prrv.2020.06.010. S1526-0542(20)30095-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amanat F., Krammer F. SARS-CoV-2 Vaccines: Status Report. Immunity. 2020;52:583–589. doi: 10.1016/j.immuni.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen W.H., Strych U., Hotez P.J., Bottazzi M.E. The SARS-CoV-2 Vaccine Pipeline: an Overview [published online ahead of print, 2020 Mar 3] Curr Trop Med Rep. 2020:1–4. doi: 10.1007/s40475-020-00201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang T, Bidon M, Jaimes JA, Whittaker GR, Daniel S. Coronavirus membrane fusion mechanism offers as a potential target for antiviral development [published online ahead of print, 2020 Apr 6]. Antiviral Res 2020;104792. [DOI] [PMC free article] [PubMed]
- 5.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.W., Berne M.A., et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. J Virol 2020;94: e00127–20. [DOI] [PMC free article] [PubMed]
- 7.Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. The Lancet, Published online July 20, 2020. 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed]
- 9.Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, et al. An mRNA Vaccine against SARS-CoV-2 — Preliminary Report. N Engl J Med July 14, 2020. 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed]
- 10.Webster R.G. Immunity to influenza in the elderly. Vaccine. 2000;18:1686–1689. doi: 10.1016/s0264-410x(99)00507-1. [DOI] [PubMed] [Google Scholar]
- 11.Katz J.M., Plowden J., Renshaw-Hoelscher M., Lu X., Tumpey T.M., Sambhara S. Immunity to influenza: the challenges of protecting an aging population. Immunol Res. 2004;29:113–124. doi: 10.1385/IR:29:1-3:113. [DOI] [PubMed] [Google Scholar]
- 12.Chang Y.T., Guo C.Y., Tsai M.S., Cheng Y.Y., Lin M.T., Chen C.H., et al. Poor immune response to a standard single dose non-adjuvanted vaccination against 2009 pandemic H1N1 influenza virus A in the adult and elder hemodialysis patients. Vaccine. 2012;30:5009–5018. doi: 10.1016/j.vaccine.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect 2020 [published online ahead of print, 2020 Mar 27]. [DOI] [PMC free article] [PubMed]
- 14.CDC COVID-19 Response Team. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:343–6. [DOI] [PMC free article] [PubMed]
- 15.Han D.P., Kim H.G., Kim Y.B., Poon L.L., Chon M.W. Development of a safe neutralization assay for SARS-CoV and characterization of S-glycoprotein. Virology. 2004;326:140–149. doi: 10.1016/j.virol.2004.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walls A.C., Tortorici M.A., Frenz B., Snijder J., Li W., Rey F.A., et al. Glycan shield and epitope masking of a coronavirus spike protein observed by cryo-electron microscopy. Nat Struct Mol Biol. 2016;23:899–905. doi: 10.1038/nsmb.3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang T.J., Chang Y.C., Ko T.P., Draczkowski P., Chien Y.C., Chang Y.C., et al. Cryo-EM analysis of a feline coronavirus spike protein reveals a unique structure and camouflaging glycans. Proc Natl Acad Sci USA. 2020;117:1438–1446. doi: 10.1073/pnas.1908898117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watanabe Y, Allen JD, Wrapp D, McLellan JS, Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science [published online ahead of print, 2020 May 4] 2020. [DOI] [PMC free article] [PubMed]
- 19.Jardine J., Julien J.P., Menis S., Ota T., Kalyuzhniy O., McGuire A., et al. Rational HIV immunogen design to target specific germline B cell receptors. Science. 2013;340:711–716. doi: 10.1126/science.1234150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei X., Decker J.M., Wang S., Hui H., Kappes J.C., Wu X., et al. Antibody neutralization and escape by HIV-1. Nature. 2003;422:307–312. doi: 10.1038/nature01470. [DOI] [PubMed] [Google Scholar]
- 21.Wei C.-J., Boyington J.C., Dai K., Houser K.V., Pearce M.B., Kong W.P., et al. Cross-neutralization of 1918 and 2009 influenza viruses: Role of glycans in viral evolution and vaccine design. Sci Transl Med. 2010;2:24ra21. doi: 10.1126/scitranslmed.3000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu R., Ekiert D.C., Krause J.C., Hai R., Crowe J.E., Jr., Wilson I.A. Structural basis of preexisting immunity to the 2009 H1N1 pandemic influenza virus. Science. 2010;328:357–360. doi: 10.1126/science.1186430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crooks E., Tong T., Chakrabarti B., Narayan K., Georgiev I., Menis S. Vaccine-Elicited Tier 2 HIV-1 Neutralizing Antibodies Bind to Quaternary Epitopes Involving Glycan-Deficient Patches Proximal to the CD4 Binding Site. PLoS Pathog. 2015;11 doi: 10.1371/journal.ppat.1004932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leonard C.K., Spellman M.W., Riddle L., Harris R.J., Thomas J.N., Gregory T.J. Assignment of intrachain disulfide bonds and characterization of potential glycosylation sites of the type 1 recombinant human immunodeficiency virus envelope glycoprotein (gp120) expressed in Chinese hamster ovary cells. J Biol Chem. 1990;265:10373–10382. [PubMed] [Google Scholar]
- 25.Mizuochi T., Matthews T., Kato M., Hamako J., Titani K., Solomon J., et al. Diversity of oligosaccharide structures on the envelope glycoprotein gp120 of human immunodeficiency virus 1 from the lymphoblastoid cell line H9. Presence of complex-type oligosaccharides with bisecting N-acetylglucosamine residues. J Biol Chem. 1990;265:8519–8524. [PubMed] [Google Scholar]
- 26.Book Galili U. Academic Press/Elsevier Publishers; London: 2018. The natural anti-Gal antibody as foe turned friend in medicine. [Google Scholar]
- 27.Abdel-Motal U., Wang S., Lu S., Wigglesworth K., Galili U. Increased immunogenicity of human immunodeficiency virus gp120 engineered to express Galα1-3Galβ1-4GlcNAc-R epitopes. J Virol. 2006;80:6943–6951. doi: 10.1128/JVI.00310-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdel-Motal U.M., Guay H.M., Wigglesworth K., Welsh R.M., Galili U. Immunogenicity of influenza virus vaccine is increased by anti-Gal-mediated targeting to antigen-presenting cells. J Virol. 2007;81:9131–9141. doi: 10.1128/JVI.00647-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdel-Motal U.M., Wang S., Awad A., Lu S., Wigglesworth K., Galili U. Increased immunogenicity of HIV-1 p24 and gp120 following immunization with gp120/p24 fusion protein vaccine expressing α-gal epitopes. Vaccine. 2010;28:1758–1765. doi: 10.1016/j.vaccine.2009.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdel-Motal U.M., Wigglesworth K., Galili U. Mechanism for increased immunogenicity of vaccines that form in vivo immune complexes with the natural anti-Gal antibody. Vaccine. 2009;27:3072–3082. doi: 10.1016/j.vaccine.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 31.Stoner R.D., Terres G. Enhanced antitoxin responses in irradiated mice elicited by complexes of tetanus toxoid and specific antibody. J Immunol. 1963;91:761–770. [PubMed] [Google Scholar]
- 32.Manca F., Fenoglio D., Li Pira G., Kunkl A., Celada F. Effect of antigen/antibody ratio on macrophage uptake, processing, and presentation to T cells of antigen complexed with polyclonal antibodies. J Exp Med. 1991;173:37–48. doi: 10.1084/jem.173.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Celis E., Chang T.W. Antibodies to hepatitis B surface antigen potentiate the response of human T lymphocyte clones to the same antigen. Science. 1984;224:297–299. doi: 10.1126/science.6231724. [DOI] [PubMed] [Google Scholar]
- 34.Houston W.E., Kremer R.J., Crabbs C.L., Spertzel R.O. Inactivated Venezuelan equine encephalomyelitis virus vaccine complexed with specific antibody: enhanced primary immune response and altered pattern of antibody class elicited. J Infect Dis. 1977;135:600–610. doi: 10.1093/infdis/135.4.600. [DOI] [PubMed] [Google Scholar]
- 35.Villinger F., Mayne A.E., Bostik P., Mori K., Jensen P.E., Ahmed R. Evidence for antibody-mediated enhancement of simian immunodeficiency virus (SIV) Gag antigen processing and cross presentation in SIV-infected rhesus macaques. J Virol. 2003;77:10–24. doi: 10.1128/JVI.77.1.10-24.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clynes R., Takechi Y., Moroi Y., Houghton A., Ravetch J.V. Fc receptors are required in passive and active immunity to melanoma. Proc Natl Acad Sci USA. 1998;95:652–656. doi: 10.1073/pnas.95.2.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rafiq K., Bergtold A., Clynes R. Immune complex-mediated antigen presentation induces tumor immunity. J Clin Invest. 2002;110:71–79. doi: 10.1172/JCI15640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Regnault A., Lankar D., Lacabanne V., Rodriguez A., Théry C., Rescigno M., et al. Fcγ receptor-mediated induction of dendritic cell maturation and major histocompatibility complex class I-restricted antigen presentation after immune complex internalization. J Exp Med. 1999;189:371–380. doi: 10.1084/jem.189.2.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schuurhuis D.H., Ioan-Facsinay A., Nagelkerken B., van Schip J.J., Sedlik C., Melief C.J. Antigen-antibody immune complexes empower dendritic cells to efficiently prime specific CD8+ CTL responses in vivo. J Immunol. 2002;168:2240–2246. doi: 10.4049/jimmunol.168.5.2240. [DOI] [PubMed] [Google Scholar]
- 40.Galili U., Rachmilewitz E.A., Peleg A., Flechner I.A. A unique natural human IgG antibody with anti-α-galactosyl specificity. J Exp Med. 1984;160:1519–1531. doi: 10.1084/jem.160.5.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Galili U. Anti-Gal: an abundant human natural antibody of multiple pathogeneses and clinical benefits. Immunology. 2013;140:1–11. doi: 10.1111/imm.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hamadeh R.M., Galili U., Zhou P., Griffiss J.M. Anti-α-galactosyl immunoglobulin A (IgA), IgG, and IgM in human secretions. Clin Diagn Lab Immunol. 1995;2:125–131. doi: 10.1128/cdli.2.2.125-131.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galili U., Mandrell R.E., Hamadeh R.M., Shohet S.B., Griffiss J.M. Interaction between human natural anti-α-galactosyl immunoglobulin G and bacteria of the human flora. Infect Immun. 1988;56:1730–1737. doi: 10.1128/iai.56.7.1730-1737.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Posekany K.J., Pittman H.K., Bradfield J.F., Haisch C.E., Verbanac K.M. Induction of cytolytic anti-Gal antibodies in α-1,3-galactosyltransferase gene knockout mice by oral inoculation with Escherichia coli O86:B7 bacteria. Infect Immun. 2002;70:6215–6222. doi: 10.1128/IAI.70.11.6215-6222.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mañez R., Blanco F.J., Díaz I., Centeno A., Lopez-Pelaez E., Hermida M., et al. Removal of bowel aerobic gram-negative bacteria is more effective than immunosuppression with cyclophosphamide and steroids to decrease natural α-galactosyl IgG antibodies. Xenotransplantation. 2001;8:15–23. doi: 10.1034/j.1399-3089.2001.00082.x. [DOI] [PubMed] [Google Scholar]
- 46.Galili U., Macher B.A., Buehler J., Shohet S.B. Human natural anti-α-galactosyl IgG. II. The specific recognition of α(1–3)-linked galactose residues. J Exp Med. 1985;162:573–582. doi: 10.1084/jem.162.2.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Towbin H., Rosenfelder G., Wieslander J., Avila J.L., Rojas M., Szarfman A., et al. Circulating antibodies to mouse laminin in Chagas disease, American cutaneous leishmaniasis, and normal individuals recognize terminal galactosyl(α1-3)-galactose epitopes. J Exp Med. 1987;166:419–432. doi: 10.1084/jem.166.2.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Galili U., Clark M.R., Shohet S.B., Buehler J., Macher B.A. Evolutionary relationship between the anti-Gal antibody and the Galα1-3Gal epitope in primates. Proc Natl Acad Sci USA. 1987;84:1369–1373. doi: 10.1073/pnas.84.5.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Galili U., Shohet S.B., Kobrin E., Stults C.L.M., Macher B.A. Man, apes, and Old World monkeys differ from other mammals in the expression of α-galactosyl epitopes on nucleated cells. J Biol Chem. 1988;263:17755–17762. [PubMed] [Google Scholar]
- 50.Spiro R.G., Bhoyroo V.D. Occurrence of α-D-galactosyl residues in the thyroglobulin from several species. Localization in the saccharide chains of the complex carbohydrate units. J Biol Chem. 1984;259:9858–9866. [PubMed] [Google Scholar]
- 51.Thall A., Galili U. Distribution of Galα1-3Galβ1-4GlcNAc residues on secreted mammalian glycoproteins (thyroglobulin, fibrinogen, and immunoglobulin G) as measured by a sensitive solid-phase radioimmunoassay. Biochemistry. 1990;29:3959–3965. doi: 10.1021/bi00468a024. [DOI] [PubMed] [Google Scholar]
- 52.Galili U., Swanson K. Gene sequences suggest inactivation of α-1,3-galactosyltransferase in catarrhines after the divergence of apes from monkeys. Proc Natl Acad Sci USA. 1991;88:7401–7404. doi: 10.1073/pnas.88.16.7401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galili U. Evolution in primates by “Catastrophic-selection” interplay between enveloped virus epidemics, mutated genes of enzymes synthesizing carbohydrate antigens, and natural anti-carbohydrate antibodies. Am J Phys Anthropol. 2019;168:352–363. doi: 10.1002/ajpa.23745. [DOI] [PubMed] [Google Scholar]
- 54.Teranishi K., Manez R., Awwad M., Cooper D.K. Anti-Gal α1-3Gal IgM and IgG antibody levels in sera of humans and Old World non-human primates. Xenotransplantation. 2002;9:148–154. doi: 10.1034/j.1399-3089.2002.1o058.x. [DOI] [PubMed] [Google Scholar]
- 55.Repik P.M., Strizki M., Galili U. Differential host dependent expression of α-galactosyl epitopes on viral glycoproteins: A study of Eastern equine encephalitis virus as a model. J Gen Virol. 1994;75:1177–1181. doi: 10.1099/0022-1317-75-5-1177. [DOI] [PubMed] [Google Scholar]
- 56.Rother R.P., Fodor W.L., Springhorn J.P., Birks C.W., Setter E., Sandrin M.S., et al. A novel mechanism of retrovirus inactivation in human serum mediated by anti-α-galactosyl natural antibody. J Exp Med. 1995;182:1345–1355. doi: 10.1084/jem.182.5.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Welsh R.M., O'Donnell C.L., Reed D.J., Rother R.P. Evaluation of the Galα1-3Gal epitope as a host modification factor eliciting natural humoral immunity to enveloped viruses. J Virol. 1998;72:4650–4656. doi: 10.1128/jvi.72.6.4650-4656.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takeuchi Y., Porter C.D., Strahan K.M., Preece A.F., Gustafsson K., Cosset F.L., et al. Sensitization of cells and retroviruses to human serum by (α1-3) galactosyltransferase. Nature. 1996;379:85–88. doi: 10.1038/379085a0. [DOI] [PubMed] [Google Scholar]
- 59.Hayashi S., Ogawa S., Takashima Y., Otsuka H. The neutralization of pseudorabies virus by anti-α-galactosyl natural antibody in normal serum. Virus Res. 2004;99:1–7. doi: 10.1016/j.virusres.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 60.Neil S.J.D., McKnight A., Gustafsson K., Weiss R.A. HIV-1 incorporates ABO histo-blood group antigens that sensitize virions to complement-mediated inactivation. Blood. 2005;105:4693–4699. doi: 10.1182/blood-2004-11-4267. [DOI] [PubMed] [Google Scholar]
- 61.Dürrbach A., Baple E., Preece A.F., Charpentier B., Gustafsson K. Virus recognition by specific natural antibodies and complement results in MHC I cross-presentation. J Immunol. 2007;37:1254–1265. doi: 10.1002/eji.200636129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Preece A.F., Strahan K.M., Devitt J., Yamamoto F., Gustafsson K. Expression of ABO or related antigenic carbohydrates on viral envelopes leads to neutralization in the presence of serum containing specific natural antibodies and complement. Blood. 2002;99:2477–2482. doi: 10.1182/blood.v99.7.2477. [DOI] [PubMed] [Google Scholar]
- 63.Kim N.Y., Jung W.W., Oh Y.K., Chun T., Park H.Y., Lee H.T., et al. Natural protection from zoonosis by α-gal epitopes on virus particles in xenotransmission. Xenotransplantation. 2007;14:104–111. doi: 10.1111/j.1399-3089.2007.00377.x. [DOI] [PubMed] [Google Scholar]
- 64.Galili U., Repik P.M., Anaraki F., Mozdzanowska K., Washko G., Gerhard W. Enhancement of antigen presentation of influenza virus hemagglutinin by the natural human anti-Gal antibody. Vaccine. 1996;14:321–328. doi: 10.1016/0264-410x(95)00189-8. [DOI] [PubMed] [Google Scholar]
- 65.Henion T.R., Gerhard W., Anaraki F., Galili U. Synthesis of α-gal epitopes on influenza virus vaccines, by recombinant α1,3galactosyltransferase, enables the formation of immune complexes with the natural anti-Gal antibody. Vaccine. 1997;15:1174–1182. doi: 10.1016/s0264-410x(96)00300-3. [DOI] [PubMed] [Google Scholar]
- 66.Galili U., Wigglesworth K., Abdel-Motal U.M. Intratumoral injection of α-gal glycolipids induces xenograft-like destruction and conversion of lesions into endogenous vaccines. J Immunol. 2007;178:4676–4687. doi: 10.4049/jimmunol.178.7.4676. [DOI] [PubMed] [Google Scholar]
- 67.Thall A.D., Malý P., Lowe J.B. Oocyte Galα 1,3Gal epitopes implicated in sperm adhesion to the zona pellucida glycoprotein ZP3 are not required for fertilization in the mouse. J Biol Chem. 1995;270:21437–21440. doi: 10.1074/jbc.270.37.21437. [DOI] [PubMed] [Google Scholar]
- 68.Tanemura M., Yin D., Chong A.S., Galili U. Differential immune responses to α-gal epitopes on xenografts and allografts: implications for accommodation in xenotransplantation. J Clin Invest. 2000;105:301–310. doi: 10.1172/JCI7358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rötzschke O., Falk K., Stevanović S., Jung G., Walden P., Rammensee H.G. Exact prediction of a natural T cell epitope. Eur J Immunol. 1991;21:2891–2894. doi: 10.1002/eji.1830211136. [DOI] [PubMed] [Google Scholar]
- 70.Shastri N., Gonzalez F. Endogenous generation and presentation of the ovalbumin peptide/Kb complex to T cells. J Immunol. 1993;150:2724–2736. [PubMed] [Google Scholar]
- 71.Matsumoto A., Yoshima H., Kobata A. Carbohydrates of influenza virus hemagglutinin: structures of the whole neutral sugar chains. Biochemistry. 1983;22:188–196. doi: 10.1021/bi00270a028. [DOI] [PubMed] [Google Scholar]
- 72.Keil W., Geyer R., Dabrowski J., Dabrowski U., Niemann H., Stirm S., et al. Carbohydrates of influenza virus. Structural elucidation of the individual glycans of the FPV hemagglutinin by two-dimensional 1H n.m.r. and methylation analysis. EMBO J. 1985;4:2711–2720. doi: 10.1002/j.1460-2075.1985.tb03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wood C., Kabat E.A., Murphy L.A., Goldstein I.J. Immunochemical studies of the combining sites of the two isolectins, A4 and B4, isolated from Bandeiraea simplicifolia. Arch Biochem Biophys. 1979;198:1–11. doi: 10.1016/0003-9861(79)90389-8. [DOI] [PubMed] [Google Scholar]
- 74.Montefiori D.C., Pantaleo G., Fink L.M., Zhou J.T., Zhou J.Y., Bilska M., et al. Neutralizing and infection-enhancing antibody responses to human immunodeficiency virus type 1 in long-term nonprogressors. J Infect Dis. 1996;173:60–77. doi: 10.1093/infdis/173.1.60. [DOI] [PubMed] [Google Scholar]
- 75.Wang S., Arthos J., Lawrence J.M., Van Ryk D., Mboudjeka I., Shen S., et al. Enhanced immunogenicity of gp120 protein when combined with recombinant DNA priming to generate antibodies that neutralize the JR-FL primary isolate of human immunodeficiency virus type 1. J Virol. 2005;79:7933–7937. doi: 10.1128/JVI.79.12.7933-7937.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goulder P.J., Watkins D.I. HIV and SIV CTL escape: implications for vaccine design. Nat Rev Immunol. 2004;4:630–640. doi: 10.1038/nri1417. [DOI] [PubMed] [Google Scholar]
- 77.Lewis G.K., DeVico A.L., Gallo R.C. Antibody persistence and T-cell balance: two key factors confronting HIV vaccine development. Proc Natl Acad Sci USA. 2014;111:15614–15621. doi: 10.1073/pnas.1413550111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Qiu J.T., Song R., Dettenhofer M., Tian C., August T., Felber B.K., et al. Evaluation of novel human immunodeficiency virus type 1 Gag DNA vaccines for protein expression in mammalian cells and induction of immune responses. J Virol. 2010;73:9145–9152. doi: 10.1128/jvi.73.11.9145-9152.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fiers W., De Filette M., Birkett A., Neirynck S., Min Jou W. A “universal” human in fluenza A vaccine. Virus Res. 2004;103:173–176. doi: 10.1016/j.virusres.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 80.Estrada L.D., Schultz-Cherry S. Development of a Universal Influenza Vaccine. J Immunol. 2019;202:392–398. doi: 10.4049/jimmunol.1801054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Benatuil L., Kaye J., Rich R.F., Fishman J.A., Green W.R., Iacomini J. The influence of natural antibody specificity on antigen immunogenicity. Eur J Immunol. 2005;35:2638–2647. doi: 10.1002/eji.200526146. [DOI] [PubMed] [Google Scholar]
- 82.Hjelm F., Carlsson F., Getahun A., Heyman B. Antibody-mediated regulation of the Immune response. Scand J Immunol. 2006;64:177–184. doi: 10.1111/j.1365-3083.2006.01818.x. [DOI] [PubMed] [Google Scholar]
- 83.Galili U., Matta K.L. Inhibition of anti-Gal IgG binding to porcine endothelial cells by synthetic oligosaccharides. Transplantation. 1996;62:256–262. doi: 10.1097/00007890-199607270-00018. [DOI] [PubMed] [Google Scholar]
- 84.LaTemple D.C., Abrams J.T., Zhang S.Y., Galili U. Increased immunogenicity of tumor vaccines complexed with anti-Gal: studies in knockout mice for α1,3galactosyltransferase. Cancer Res. 1999;59:3417–3423. [PubMed] [Google Scholar]
- 85.Rossi G.R., Mautino M.R., Unfer R.C., Seregina T.M., Vahanian N., Link C.J. Effective treatment of preexisting melanoma with whole cell vaccines expressing α(1,3)-galactosyl epitopes. Cancer Res. 2005;65:10555–10561. doi: 10.1158/0008-5472.CAN-05-0627. [DOI] [PubMed] [Google Scholar]
- 86.Manches O., Plumas J., Lui G., Chaperot Laurence, Molens Jean-Paul, Sotto Jean-Jacques, et al. Anti-Gal-mediated targeting of human B lymphoma cells to antigen-presenting cells: a potential method for immunotherapy using autologous tumor cells. Haematologica. 2005;90:625–634. [PubMed] [Google Scholar]
- 87.Fanger N.A., Wardwell K., Shen L., Tedder T.F., Guyre P.M. Type I (CD64) and type II (CD32) Fc gamma receptor-mediated phagocytosis by human blood dendritic cells. J Immunol. 1996;157:541–548. [PubMed] [Google Scholar]
- 88.Henion T.R., Macher B.A., Anaraki F., Galili U. Defining the minimal size of catalytically active primate α1,3 galactosyltransferase: structure-function studies on the recombinant truncated enzyme. Glycobiology. 1994;4:193–201. doi: 10.1093/glycob/4.2.193. [DOI] [PubMed] [Google Scholar]
- 89.Chen Z.C., Tanemura M., Galili U. Synthesis of α-gal epitopes (Galα1-3Galβ1-4GlcNAc-R) on human tumor cells by recombinant α1,3galactosyltransferase produced in Pichia cells lacking α-gal epitopes and pastoris. Glycobiology. 2001;11:577–586. doi: 10.1093/glycob/11.7.577. [DOI] [PubMed] [Google Scholar]
- 90.Furukawa K., Tanemura M., Miyoshi E., Eguchi H., Nagano H., Matsunami K., et al. A practical approach to pancreatic cancer immunotherapy using resected tumor lysate vaccines processed to express α-gal epitopes. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0184901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Galili U., Chen Z.C., DeGeest K. Expression of α-gal epitopes on ovarian carcinoma membranes to be used as a novel autologous tumor vaccine. Gynecol Oncol. 2003;90:100–108. doi: 10.1016/s0090-8258(03)00148-3. [DOI] [PubMed] [Google Scholar]
- 92.Qiu Y., Xu M.B., Yun M.M., Wang Y.Z., Zhang R.M., Meng X.K., et al. Hepatocellular carcinoma-specific immunotherapy with synthesized α1,3-galactosyl epitope-pulsed dendritic cells and cytokine-induced killer cells. World J Gastroenterol. 2011;17:5260–5266. doi: 10.3748/wjg.v17.i48.5260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Qiu Y., Yun M.M., Xu M.B., Wang Y.Z., Yun S. Pancreatic carcinoma-specific immunotherapy using synthesized α-galactosyl epitope-activated immune responders: findings from a pilot study. Int J Clin Oncol. 2013;18:657–665. doi: 10.1007/s10147-012-0434-4. [DOI] [PubMed] [Google Scholar]
- 94.Qiu Y., Yun M.M., Dong X., Xu M., Zhao R., Han X., et al. Combination of cytokine-induced killer and dendritic cells pulsed with antigenic α-1,3-galactosyl epitope-enhanced lymphoma cell membrane for effective B-cell lymphoma immunotherapy. Cytotherapy. 2016;18:91–98. doi: 10.1016/j.jcyt.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 95.Joziasse D.H., Shaper N.L., Salyer L.S., Van den Eijnden D.H., van der Spoel A.C., Shaper J.H. α1-3-galactosyltransferase: the use of recombinant enzyme for the synthesis of α-galactosylated glycoconjugates. Eur J Biochem. 1990;191:75–83. doi: 10.1111/j.1432-1033.1990.tb19095.x. [DOI] [PubMed] [Google Scholar]
- 96.Smith D.F., Larsen R.D., Mattox S., Lowe J.B., Cummings R.D. Transfer and expression of a murine UDP-Galβ-D-Gal-α1,3-galactosyltransferase gene in transfected Chinese hamster ovary cells. Competition reactions between the α1,3-galactosyltransferase and the endogenous α2,3-sialyltransferase. J Biol Chem. 1990;265:6225–6234. [PubMed] [Google Scholar]
- 97.Szymczakiewicz-Multanowska A., Groth N., Bugarini R., Lattanzi M., Casula D., Hilbert A., et al. Safety and immunogenicity of a novel influenza subunit vaccine produced in mammalian cell culture. J Infect Dis. 2009;200:841–848. doi: 10.1086/605505. [DOI] [PubMed] [Google Scholar]
- 98.Ambrozaitis A., Groth N., Bugarini R., Sparacio V., Podda A., Lattanzi M. A novel mammalian cell-culture technique for consistent production of a well-tolerated and immunogenic trivalent subunit influenza vaccine. Vaccine. 2009;27:6022–6029. doi: 10.1016/j.vaccine.2009.07.083. [DOI] [PubMed] [Google Scholar]
- 99.Deriy L., Chen Z.C., Gao G.P., Galili U. Expression of α-gal epitopes on HeLa cells transduced with adenovirus containing α1,3galactosyltransferase cDNA. Glycobiology. 2002;12:135–144. doi: 10.1093/glycob/12.2.135. [DOI] [PubMed] [Google Scholar]
- 100.Choi B.K., Bobrowicz P., Davidson R.C., Hamilton S.R., Kung D.H., Li H., et al. Use of combinatorial genetic libraries to humanize N-linked glycosylation in the yeast Pichia pastoris. Proc Natl Acad Sci USA. 2003;100:5022–5027. doi: 10.1073/pnas.0931263100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wildt S., Gerngross T.U. The humanization of N-glycosylation pathways in yeast. Nat Rev Microbiol. 2005;3:119–128. doi: 10.1038/nrmicro1087. [DOI] [PubMed] [Google Scholar]
- 102.Fu X.Y. Extracellular accumulation of recombinant protein by Escherichia coli in a defined medium. Appl Microbiol Biotechnol. 2010;88:75–86. doi: 10.1007/s00253-010-2718-9. [DOI] [PubMed] [Google Scholar]
- 103.Fisher A.C., Haitjema C.H., Guarino C., Çelik E., Endicott C.E., Reading C.A., et al. Production of secretory and extracellular N-linked glycoproteins in Escherichia coli. Appl Environ Microbiol. 2011;77:871–881. doi: 10.1128/AEM.01901-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen X., Liu Z., Wang J., Fang J., Fan H., Wang P.G. Changing the donor cofactor of bovine α1,3-galactosyltransferase by fusion with UDP-galactose 4-epimerase. More efficient biocatalysis for synthesis of α-Gal epitopes. J Biol Chem. 2000;275:31594–31600. doi: 10.1074/jbc.M004005200. [DOI] [PubMed] [Google Scholar]
- 105.Gebus C., Cottin C., Randriantsoa M., Drouillard S., Samain E. Synthesis of α-galactosyl epitopes by metabolically engineered Escherichia coli. Carbohydr Res. 2012;361:83–90. doi: 10.1016/j.carres.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 106.Wacker M, Linton D, Hitchen PG, Nita-Lazar M, Haslam SM, North SJ, et al. N-linked glycosylation in Campylobacter jejuni and its functional transfer into E. coli. Science 2002;298:1790–3. [DOI] [PubMed]
- 107.Tearle R.G., Tange M.J., Zannettino Z.L., Katerelos M., Shinkel T.A., Van Denderen B.J., et al. The α-1,3-galactosyltransferase knockout mouse. Implications for xenotransplantation. Transplantation. 1996;61:13–19. doi: 10.1097/00007890-199601150-00004. [DOI] [PubMed] [Google Scholar]
- 108.Lai L., Kolber-Simonds D., Park K.W., Cheong H.T., Greenstein J.L., Im G.S., et al. Production of α-1,3-galactosyltransferase knockout pigs by nuclear transfer cloning. Science. 2002;295:1089–1092. doi: 10.1126/science.1068228. [DOI] [PubMed] [Google Scholar]
- 109.Phelps C.J., Koike C., Vaught T.D., Boone J., Wells K.D., Chen S.H., et al. Production of α1,3-galactosyltransferase-deficient pigs. Science. 2003;299:411–414. doi: 10.1126/science.1078942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.LaTemple D.C., Galili U. Adult and neonatal anti-Gal response in knock-out mice for α1,3galactosyltransferase. Xenotransplantation. 1998;5:191–196. doi: 10.1111/j.1399-3089.1998.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 111.Dor F.J.M., Tseng Y.L., Cheng J., Moran K., Sanderson T.M., Lancos C.J., et al. α1,3-Galactosyltransferase gene-knockout miniature swine produce natural cytotoxic anti-Gal antibodies. Transplantation. 2004;78:15–20. doi: 10.1097/01.tp.0000130487.68051.eb. [DOI] [PubMed] [Google Scholar]
- 112.Fang J., Walters A., Hara H., Long C., Yeh P., Ayares D., et al. Anti-gal antibodies in α1,3-galactosyltransferase gene-knockout pigs. Xenotransplantation. 2012;19:305–310. doi: 10.1111/j.1399-3089.2012.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Galili U. α1,3Galactosyltransferase knockout pigs produce the natural anti-Gal antibody and simulate the evolutionary appearance of this antibody in primates. Xenotransplantation. 2013;20:267–276. doi: 10.1111/xen.12051. [DOI] [PubMed] [Google Scholar]
- 114.Whalen G.F., Sullivan M., Piperdi B., Wasseff W., Galili U. Cancer immunotherapy by intratumoral injection of α-gal glycolipids. Anticancer Res. 2012;32:3861–3868. [PubMed] [Google Scholar]
- 115.Albertini MR, Ranheim EA, Zuleger CL, Sondel PM, Hank JA, Bridges A, et al. Phase I study to evaluate toxicity and feasibility of intratumoral injection of α-gal glycolipids in patients with advanced melanoma. Cancer Immunol Immunother 65, 897–907. [DOI] [PMC free article] [PubMed]
- 116.Chung C.H., Mirakhur B., Chan E., Le Q.T., Berlin J., Morse M., et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-α-1,3-galactose. N Engl J Med. 2008;358:1109–1117. doi: 10.1056/NEJMoa074943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Commins S.P., Satinover S.M., Hosen J., Mozena J., Borish L., Lewis B.D., et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-α-1,3-galactose. J Allergy Clin Immunol. 2009;123:426–4233. doi: 10.1016/j.jaci.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nunez R., Carballada F., Gonzalez-Quintela A., Gomez-Rial J., Boquete M., Vidal C., et al. Delayed mammalian meat-induced anaphylaxis due to galactose-α-1,3-galactose in 5 European patients. J Allergy Clin Immunol. 2011;128:1122–1124. doi: 10.1016/j.jaci.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 119.Commins S.P., Platts-Mills T.A. Tick bites and red meat allergy. Curr Opin Allergy Clin Immunol. 2013;13:354–359. doi: 10.1097/ACI.0b013e3283624560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.van Nunen S. Tick-induced allergies: mammalian meat allergy, tick anaphylaxis and their significance. Asia Pac Allergy. 2015;5:3–16. doi: 10.5415/apallergy.2015.5.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]