Highlights
This article provides a comprehensive review of the recent National Academies of Science, Engineering and Medicine consensus committee report on Social Isolation and Loneliness (SI/L). The relevance specifically for mental health providers is emphasized.
-
•
What is the primary question addressed by this study?What are the physical and mental health consequences of SI/L?
What are the current evidence-based interventions for SI/L which can be implemented by mental health professionals?
-
•
SI/L are significant public health problems and are clear risks for death, depression, anxiety, and cognitive disorders such as major cognitive impairment (dementia). The evidence based interventions by mental health professionals for SI/L are limited yet some have emerged which are promising.
-
•
Health and mental healthcare professionals may be the first to identify socially isolated and lonely older adults as these older adults are at significant increased risk for serious adverse outcomes. For this reason, these professionals should know how to screen for and to initiate interventions that can be helpful.
Key Words: Social isolation, loneliness, social connection, social support, social integration, healthcare policy
Abstract
The authors of this review both served on the National Academy of Science, Engineering, and Medicine Committee that produced the report, “Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System.” In 2018, the AARP Foundation commissioned the National Academies to establish a committee to research and develop a report on social isolation and loneliness in persons 50 years of age and older. Emphasis was placed upon the role of the healthcare system in addressing this fundamental public health problem. The committee released the report in February 2020 as the Corona Virus Disease 2019 pandemic was beginning to spread to North America. In this review, the authors share central findings and conclusions from the report as well as how these findings may be relevant to the care and well-being of older adults during this historic pandemic. The health protective benefits of social distancing must be balanced by the essential need for sustaining social relationships.
INTRODUCTION
Biomedical models of human health and disease have been enhanced by decades of sustained research into the social determinants of physical and mental health, though social influences on health and disease often receive less attention in healthcare practices. Over the 20th century, factors such as socio-economic position, race/ethnicity, gender, sexual orientation, and others have populated the literature with every increasing evidences of their importance on health.1 Significant disparities in mortality were found for different occupations, as well as for different education and income strata. Many commentators noted that these inequities in health were often avoidable, arising from the circumstances in which people grow, live, work, and age, and the systems put in place to deal with illness. These circumstances, in turn, are shaped by political, social, and economic forces.2
Toward the end of the century, the importance of “social connections”, the quantity, quality, and benefits of human relationships, became a major focus of the empirical research into the social determinants of health. Within this extensive literature, social isolation and loneliness (SI/L), representing both objective and subjective experiences of social disconnection, emerged as two key constructs impacting human health. SI/L are particularly relevant to the physical and mental health and longevity of older adults because circumstances of aging, such as relationship losses, medical morbidities, and functional declines, are predisposing factors. Furthermore, the impacts of SI/L on the health and longevity of older adults are substantial. For example, meta-analyses have found that social isolation or loneliness in older adults is associated with a 50% increased risk of developing dementia,3 a 30% increased risk of incident coronary artery disease or stroke,4 , 5 and a 26% increased risk of all-cause mortality.6
In 2018 the AARP Foundation commissioned the National Academies of Science, Engineering and Medicine (NASEM) to stand up a committee to research and develop a report on SI/L in persons 50+ years of age.1 Emphasis was placed upon the role of the healthcare system in addressing this fundamental public health problem.
The committee released the report as the Corona Virus Disease 2019 (COVID-19) pandemic was beginning to spread to North America (https://www.nap.edu/catalog/25663/social-isolation-and-loneliness-in-older-adults-opportunities-for-the, accessed February 27, 2020). This pandemic focuses sharply on the critical issues faced by older adults with SI/L as a result of social distancing instructions to the general public. Healthcare professionals soon recognized the negative consequences of this isolation and the potential for increased loneliness across all age groups, but especially among already isolated older adults.7 , 8
In this review of the NASEM report, the authors, both members of the committee, assess central findings and conclusions from the report as well as how these findings may be applied to older adults during these unprecedented times. We begin our discussion with a review of definitions and how they may be appropriately categorized and measured to further explore the relation between these social determinants of health and their health outcomes. Next we briefly present the frequency and distribution of SI/L and why SI/L places the elderly at special risk. We follow with a discussion of risk and protective factors. We provide an overview of current measures of SI/L and emphasize the need to develop short assessment tools which can be placed in the electronic health record. Then we review the rapidly expanding literature documenting the adverse health consequences of SI/L with special attention to all-cause mortality, cardiovascular disease and stroke, minor and major neurocognitive impairment (dementia), depression and suicidal ideation and self-harm, anxiety, and quality of life (QoL). Then we provide a short overview of the emerging literature which informs us of potential mechanisms whereby SI/L lead to adverse health outcomes. The remainder of this review is devoted to interventions in which health and mental health professionals can be involved, often as the leading edge of care.
DEFINITIONS
Social connection is an overarching term that encompasses other commonly used terms describing structural, functional, and quality aspects of human relationships and interactions. Social isolation is the objective lack or limited extent of social contacts with others, for example, marital status, living alone or with others. Loneliness is the perception of social isolation or the subjective feeling of being lonely.1 The committee recognized a clear distinction between SI/L. Persons who are socially isolated may not be lonely (those who are naturally “loners” for example). In contrast, persons with many social connections may feel lonely (lonely in a crowd––a distinction dating back 70 years).9 Social support is a frequently used term in scientific studies over many years and refers to the availability of resources, such as informational, tangible, and emotional support from others in one's social network.10 In the NASEM report and in this paper we focus upon SI/L.
Epidemiology
In a 2020 report from the National Health and Aging Trends Study, prior to the COVID outbreak, investigators found that 24% of community–dwelling adults age 65 and older in the United States (approximately 7.7 million people) were socially isolated and 4% (1.3 million people) were severely socially isolated.1 , 11. Using data from the nationally representative U.S. Health and Retirement study, Perissinotto et al. found that 43 percent of Americans aged 60 and older reported feeling lonely. Among this sample, 13% reported that these symptoms occurred “often.”1 , 12 The AARP foundation undertook a survey and found that 35% of adults age 45+ in the United States reported feeling lonely.1 , 13
The sizable burden of SI/L among older Americans should come as no surprise. Putman, in his widely distributed book, Bowling Alone in 2001, described the decline in all forms of in person intercourse and how this disrupts civil engagement across age groups.14 Though loneliness appears to be most prevalent among American adults under the age of 50,15 it is notable that older adults in the ninth and 10th decades of life also experience high rates of both severe SI/L.11 Older adults are more susceptible to adverse health consequences of loneliness and isolation (due to generally poorer health).
Adults in later life who are socially isolated are typically among the oldest old, unmarried, male, have low educational attainment and low income.11 Social isolation, defined as physical isolation, reduced size and diversity of social network or less frequent contact with family and friends, increases the risk of loneliness.13 Individuals who identify as LGBTQ or other groups in our society who tend to be marginalized are also more likely to report that they are lonely.13 Although prevalences vary across studies, in part due to different methods of measurement, the consistent finding is that both loneliness and social isolation are pervasive and significant problems across all age groups.
Additional Risk Factors for SI/L
The committee recognized many risk factors for SI/L yet from the beginning we emphasized that risk can be bidirectional. For example, psychiatric conditions such as depressive and anxiety disorders can lead to social withdrawal and loneliness16, 17, 18, 19, 20, and reciprocally, social isolation, and loneliness can also lead to clinically significant depression and anxiety.16 , 18
Cross-sectional and longitudinal studies provide evidence for the reciprocal impacts of SI/L with anxiety and depression disorders that may compound over time.21 Cross-sectional studies have frequently found associations of loneliness or lower measures of relationship quality and support with high depression.21, 22, 23 Close relationships and social support may be deficient or experienced as inadequate in those who are depressed because of the distress and disabilities imposed by their depressive state. Some depressed older adults experience broad deficits in social connectedness, including high loneliness, low social support, and fewer social connections.24 , 25 Other older adults with clinical depression or generalized anxiety report high levels of loneliness unrelated to structural measures of social network or support.25, 26, 27 In these cases, loneliness may reflect cognitive biases that appraise social interactions more negatively or perceive relationships as less rewarding.1 Personality traits such as low extraversion and high neuroticism have been shown to increase the risk of loneliness and moderate the risk of loneliness among older adults with depression and anxiety.1 , 27, 28, 29, 30 The committee noted that while SI/L are frequently associated with depression and anxiety, SI/L are validated constructs that are distinct from psychiatric nosology and are also commonly experienced by older adults without psychiatric disorders.
Other individual factors include living alone, inadequate family relations or support, caregiver burden, disruptive life events (such as a move to a different residence), bereavement (perhaps the most significant immediate cause of SL/L), illness and poor health and functional disability (which limits a person's ability to socialize), sensory deprivation (such as hearing loss), and retirement.
Risk factors for SI/Lin older adults also include cognitive deficits and dementia.31 , 32 Societal factors, such as availability of public transportation, may also contribute to SI/L. North Americans are independent by nature and have gravitated to the idea of aging in place.33 Aging in place may be both a risk and protective factor for SI/L. A private home can provide a sense of comfort and security yet also been a hazard if functional disabilities disrupt usual household routines. Residents in rural areas are more likely to confront challenges seeking home-based services. Older adults in long term care may also be isolated, especially during a challenge such as COVID-19 which restricts access to family members.
Measurement
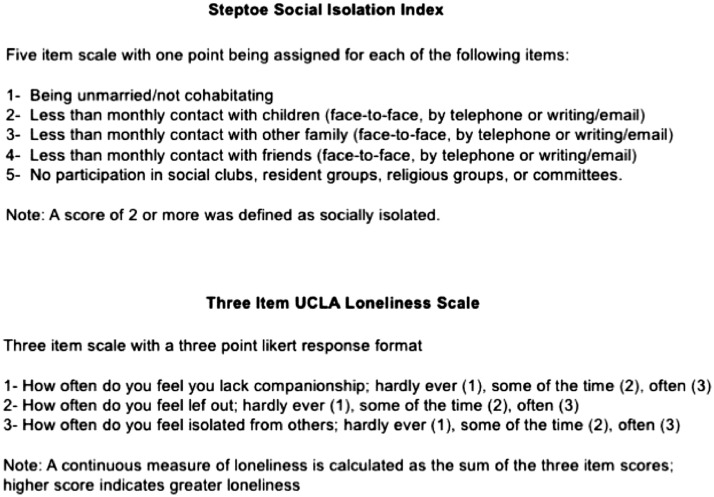
A variety of measurement scales have been developed to assess SI/L and related structural, functional, and quality aspects of social connection.34 Most of these scales are self-report questionnaires that have been designed and implemented for research purposes. The committee emphasized that researchers and healthcare practitioners should rely on validated measurement scales to assess SI/L. At the same, improved methods and tools are needed to capture newer modes of social interaction and communication and to leverage information technology and predictive analytics. Established measurement scales for the assessment of SI/L and social support are summarized below. Representative scales are shown in Figure 1 .
Figure 1.
Representative scales for measuring Social Isolation and Loneliness. References: Steptoe et al., 2013; Hughes et al. 2004.
The Berkman-Syme Social Network Index is a widely-used scale measuring level of social isolation or integration based on four domains: marital status, frequency of contact with other people, participation in religious activities, and participation in other community groups. 35 This scale was recommended for inclusion in electronic health records by an Institute of Medicine committee in 2014, for the purpose of identifying socially isolated older adults in healthcare practices.36 In research studies and in clinical applications, a variety of scoring approaches have been used.
Building on the Berkman-Syme Social Network Index, the Lubben Social Network Scale was developed for use in older adults and to focus in greater detail on level of social integration with family and friends. Ten item and six item versions of this scale have been published.37, 38, 39 Social isolation has also been measured using the five item Steptoe Social Isolation Index, which queries marital/cohabitation status, monthly contact (face to face, telephone, and email/writing) with children, other family or friends, and group participation. Individuals scoring 0 on 2 or more items are identified as socially isolated (Fig. 1).40
The Revised UCLA Loneliness Scale is a validated 20-item questionnaire that is a standard scale for measuring perceived loneliness.41 An abbreviated version of this questionnaire, the Three-Item UCLA Loneliness Scale, is widely used in research studies and for clinical identification of lonely older adults (Fig. 1).42
The de Jong Gierveld Loneliness Scale is an 11-item self-administered questionnaire that is another well-established scale for measuring perceived loneliness.43 This scale has also been adapted to a shorter, six item version, with subscales for emotional loneliness (a perceived lack of intimate relationships) and social loneliness (a perceived lack of broader social relationships).44
The Duke Social Support Index is a multidimensional scale measuring social network, social interactions, perceived, and instrumental social support. Eleven item and 23 item scales are widely used.45
The Relationship of SI/L With Adverse Physical and Mental Health Outcomes
Social isolation has been associated with a significantly increased risk of premature mortality from all causes based on research studies spanning over 40 years. The excess mortality atrributable to social isolation risk rivals the impact of physical risk factors such as obesity and smoking.1 , 10 , 35 , 46 The evidence establishing loneliness as a risk factor for premature mortality is not as extensive, yet is mounting.12 , 47 Although SI/L often co-occur, their combined and interactive effects on health outcomes have rarely been studied. Holt-Lunstad et al.48 performed a comprehensive meta-analysis of 148 prospective studies that measured both SI/L as well as a combined, multifaceted measure of social connection. Complex measures of structural components of social connection which included marital status, network size, and network participation had the strongest effect sizes compared to unidimensional measures. Over an average follow up period of 7.5 years, participants without strong social connections experienced 50% greater odds of mortality.48
SI/L have been found to increase the risk of developing coronary artery disease and stroke independent of traditional cardiovascular disease risk factors, in numerous longitudinal studies.4 , 49 Meta-analysis found these risks to be increased by nearly one-third.4 Low social connectedness has also been associated with higher healthcare utilization and worse prognoses for patients with cardiac disease. Low social support was associated with increased rates of hospital readmission and mortality following myocardial infarction.50 In patients with heart failure, higher perceived loneliness was associated with more frequent ambulatory and emergency room visits and hospital admissions.51 Vascular pathology and morbidity associated with SI/L are likely to contribute to the onset and disease course of other late-life conditions such as geriatric depression and neurocognitive disorders.
Longitudinal studies provide evidence for both SI/L as antecedent risk factors for incident depression or worsening late-life depression in older adults.16 , 52 , 53 Notably, a study of over 11,000 older U.S. adults found that lower frequency of in-person social contacts was related to higher rates of depression over 2 years.54 Lower frequencies of telephone, written or email contacts were unrelated to future depression, pointing to a specific salutary impact of in-person contacts. Despite these well-documented associations, it is important to note that loneliness and clinical depression are distinct entities. Major depression is characterized by core deficits, either diminished interest and pleasure or depressed mood, as well as symptoms such as loss of appetite, sleep problems, and difficulty concentrating. Loneliness and social withdrawal are not diagnostic features of depression, although they may be associated symptoms. It is likely that SI/L influence each other and depression pathogenesis in multifaceted ways. Some observational data suggest that loneliness predisposes to avoidance of others, social isolation and subsequent depression.16 , 18 Other evidence supports that social isolation is an initial state that can precede loneliness, low perceived social support, and depression onset.21
SI/L have been associated with suicide for all ages.1 , 55 As would be expected, depression is the most relevant cause for suicide, yet loneliness and social isolation have been found to be independent contributing factors to increased risk of suicide attempts. Social disconnection has been associated with stress, suicide ideation, and self-harm in older adults. For example, elders who experience poor social relations and are mistreated are at greater risk for suicidal ideation.1 In a study of over 60,000 older adults, increased loneliness was among the primary motivations for self-harm.1 , 56
SI/L can also lead to an increased risk for anxiety disorders which have often been linked with depression in empirical studies.16 , 19 In one study of over 1,000 individuals who were followed over 6 months, earlier loneliness positively predicted future states of social anxiety. In addition, earlier social anxiety was a predictor of future loneliness, a bidirectional relationship.19 In the Irish Longitudinal Study on Aging of over 5,000 participants, the relationship between loneliness and generalized anxiety was bidirectional, but stronger when loneliness was the origin.16 However, social isolation was a unidirectional predictor of generalized anxiety.16
The committee documented that high levels of loneliness, a low frequency of interaction with family and friends, and low levels of participation in community based groups (such as religious gatherings and civic clubs) increased the risk of cognitive decline and incident major neurocognitive impairment (dementia).1 In a meta-analysis performed in 2015, Kuiper et al.3 found an increased risk of dementia to be associated with high levels of loneliness, infrequent social contacts and low-level group participation.3 These social factors increased the risk of dementia by approximately 50%. Similarly, in a subsequent meta-analysis, investigators found that living alone, having a limited social network, or a low frequency of social contact increased the risk for dementia.1 , 57 Notably, SI/L have been found to be independent risk factors with a cumulative effect on cognitive decline and dementia risk in some studies, suggesting both shared and distinct mechanisms.1 , 23 Social interactions are thought to enhance cognitive capacity through activation and maintenance of the efficiency of brain networks.1 , 58 In addition, among cognitively normal adults, increased perceptions of loneliness have been associated with higher levels of brain amyloid and regional accumulation of tau protein, linking loneliness with pathological changes of early Alzheimer's disease.1 , 59 , 60
Though SI/L have been found to increase the risk for specific psychiatric disorders and their consequences (such as suicide), social isolation also has been associated with a decreased QoL, such as measures of a person's overall physical and mental health, satisfaction with life and “happiness,” and perceived financial adequacy.1 In one study, social isolation had a significant, independent and negative effect on health related QoL (a more narrow approach to QoL which includes perceived physical and mental health).61 Less work has been performed regarding the role of loneliness. Yet it stands to reason that both severe and moderate loneliness reduce the physical and mental QoL among older adults.
Mechanisms
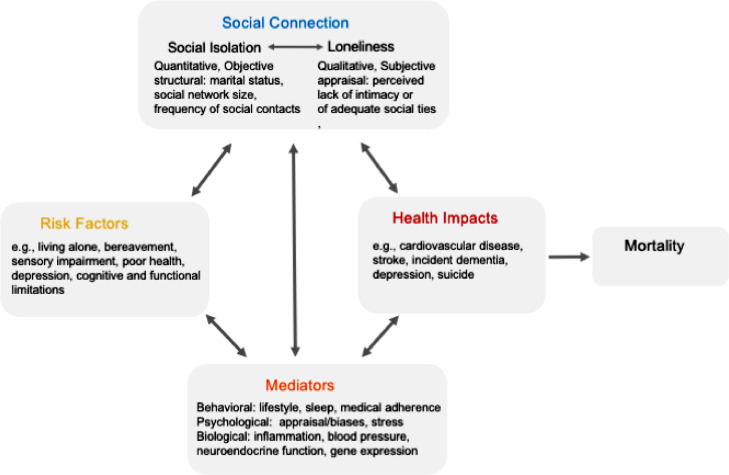
The committee report summarized key mediators (mechanisms or pathways) which link SI/L with health outcomes. Three categories of mediators were grouped according to behavioral, psychological, and biological mechanisms. These mechanisms and interrelationships are depicted in Figure 2 .
Figure 2.
Putative mechanisms by which social connections influence morbidity and mortality. Adapted, National Academies of Sciences, Engineering and Medicine, 2020 and Holt-Lunstad and Smith, 2016.
SI/L have been linked to adverse health outcomes via lifestyle or health-related behaviors. The quality and quantity of social relationships may exert favorable or unfavorable influences on health behaviors and health outcomes. A meta-analysis of patient adherence to medical treatment found that greater structural, functional, and quality measures of social connection were associated with better adherence, with the strongest effect for social support.62 Greater social support has also been strongly associated with favorable sleep outcomes,63 , 64 whereas loneliness has been associated with increased sleep fragmentation, poorer sleep quality and consequent metabolic, neural, and hormonal dysregulation.1 , 4 , 65, 66, 67, 68 A study examining the association of greater loneliness with cardiovascular disease, diabetes, and migraine among 8,600 older adults found significant mediation effects attributable to behavioral variables such as poor sleep, physical inactivity, and daily smoking.69
Psychological and stress-related mechanisms are a second category of mediators contributing to the health impacts of SI/L. Relationships with others are important to adapt to life stresses through practical guidance and aid (informational and tangible support) and emotional forms of social support. Social support has been shown to attenuate the physiological stress response, such as reducing blood pressure and the inflammatory response, in numerous studies (as reviewed in NASEM report).1 Conversely, an absence or low level of support heightens physiologic responses to stress.70 As previously noted, SI/L have been associated with greater likelihood of developing anxiety and depressive symptoms and conditions16 , 54 which, further, influence physiologic stress responses and health outcomes.
Biological studies investigating associations of SI/L with poor health outcomes implicate cardiovascular, neuroendocrine and inflammatory pathways, particularly in conditions of heightened stress. SI/L are associated with elevated vascular resistance and blood pressure as well as higher rates of metabolic syndrome.71, 72, 73 Meta-analyses have found loneliness to be associated with exaggerated blood pressure and inflammatory reactivity to acute stress.70 Social isolation has been associated with higher resting heat rate, higher systolic blood pressure, and unfavorable cholesterol parameters in response to stress.74 , 75 Strong evidences from both experimental and observational studies indicate that low social support, loneliness, and social isolation are associated with acute and chronic elevations in blood pressure and heart rate (as reviewed in the NASEM report).1
The relationship of social bonding and social isolation to hypothalamic-pituitary-adrenal axis activity in humans and animals has been extensively studied and reviewed.76 , 77 In studies of older adults, loneliness has been associated with lower cortisol output78 and lower cortisol response to stress.79 In an experimental paradigm of acute stress, loneliness was associated with both low cortisol reactivity and greater interleukin-6 and monocyte chemotactic protein 1 in older women, suggesting dysregulation of both neuroendocrine and inflammatory processes.79
Eisenberg et al.80 have comprehensively reviewed evidence for the reciprocal nature of social behavior and inflammatory processes.80 Research in both animals and humans has shown transient and sometimes long term activation of inflammatory processes in response to a range of social stressors such as social separation or loss, social defeat, and social exclusion.80 These studies include research in socially isolated older adults showing higher levels of circulating C-reactive protein, the inflammatory marker,81, 82, 83 and higher levels of the clotting factor fibrinogen, a biomarker of inflammation and cardiac risk.84 Loneliness has also been associated with higher levels of interleukin-6, fibrinogen, and C-reactive protein in a mid-life sample.85 Loneliness has been associated with greater expression of pro-inflammatory genes in older adults,86 an effect that was downregulated by mindfulness-based stress reduction in a randomized controlled trial.87
The Role of the Healthcare Sector in Addressing the impacts of SI/L in Older Adults
The committee developed five broad goals for the healthcare sector to address SI/L in older adults. These goals were, Goal 1: develop a more robust evidence base on effective assessment, prevention, and intervention strategies; Goal 2: translate current research into healthcare practices; Goals 3 and 4: improve awareness and strengthen ongoing education and training; and Goal 5: strengthen ties between the healthcare system and community-based networks and resources. Specific recommendations to advance these goals were formulated and are detailed in the full report.
Interventions
The committee report included a compilation of 92 published interventions for SI/L in older adults and 48 unpublished interventions that were identified by outreach to community organizations. These interventions were heterogeneous with respect to the target older adult population (general older population, health condition focus, vulnerable group, and residential setting), the level of intervention (one-on-one, group, and community-based), and the type of intervention (intentionally addressed SI/L, general social engagement, or environmental change/new resource (e.g., transportation). A limited number quantified the impact of interventions on SI/L, few used a randomized-controlled or quasi-experimental methodology and most studies involved convenience samples that did not specifically target the most socially isolated or lonely older adults.
Findings from seven published reviews of interventions for SI/L were reported and summarized. Across these reviews, the most effective interventions were those that specifically targeted social isolated or lonely individuals, had a sound theoretical basis, used a multileveled approach, and involved active engagement of the participant. There were inconsistent findings regarding greater effectiveness for group compared to one-on-one interventions. Individual reviews highlighted particular effectiveness of psychoeducational approaches and social skills training,88 , 89 the need to better understand mechanisms (such as maladaptive thinking) underlying SI/L90 , 91 and the need to incorporate and evaluate technology in future interventions.89
The committee report further summarized indirect and direct interventions for SI/L relevant to the healthcare system. Indirect interventions for SI/L in older adults address underlying conditions or risk factors such as hearing aids or cochlear implants to mitigate the impact of hearing loss on SI/L. Examples of other indirect interventions include enhancing physical mobility or access to transportation. SI/L may also be addressed indirectly by providing resources or support for older adults who have recently relocated or who are bereaved. Social prescribing is a common practice in which practitioners help patients access nonclinical sources of support within the community. This may be either an indirect or direct means of reducing SI/L, either by facilitating patient engagement in voluntary organizations and community groups broadly or by facilitating specific referrals to community organizations which directly address SI/L.
Psychotherapeutic approaches to reduce SI/L have included cognitive behavioral therapy and mindfulness-based approaches, with some studies showing efficacy for reducing loneliness and improving social interactions. Research suggests that lonely individuals interpret social interactions more negatively92 and are more likely to perceive social threat93 compared to those who are not lonely. Lonely individuals have also been found to score lower on tests of executive function compared to their nonlonely peers.94 It is hypothesized that these cognitive-emotional biases may lead to a cycle of worsening withdrawal and loneliness.
Mann et al.95 reviewed 10 published randomized controlled trials examining cognitive approaches to improving loneliness and other aspects of social connection in nongeriatric samples who were affected by a range of mental health conditions. Two online CBT (Cognitive Behavioral Therapy) therapies for depression (one with added motivational training and one with added brief advice) were associated with reductions in both depression and loneliness ratings at 12 months. Other trials within this review showed mixed or null effects on loneliness or social support outcomes.
The committee report also noted that a smartphone based training in mindfulness techniques of awareness and acceptance was associated with reductions in daily loneliness ratings compared to a control group in a nongeriatric sample.96 Additionally, a recent study published after the release of the NASEM report compared a 5-week, tele-delivered behavioral activation intervention for homebound lonely older adults to a tele-delivered friendly visit and found greater improvements in social interaction, perceived social support, and loneliness in the tele-delivered behavioral activation group at 6 and 12 weeks.97
There is currently no evidence for the use of pharmacologic interventions to reduce loneliness or isolation. The potential use of selective serotonin reuptake inhibitors, neurosteroids, or oxytocin to reduce anxiety and fear and promote social affiliation has been proposed as possible therapeutic avenues based primarily on animal data.93
The Role of Technology
Technological applications relevant to SI/L in older adults range from established tools such as social media groups and video-conferencing to more advanced artificial language and virtual reality functions designed for older adults. Established tools allow for greater connection through video-mediated visits and engagement in virtual communities. Artificial intelligence applications are designed to provide companionship or support function via social robots, conversational agents, or through virtual reality systems which facilitate reminiscence with familiar experiences or engagement with new stimulations. In evaluating technological interventions for SI/L, questions of accessibility, acceptability, cost, and feasibility need to be addressed.1 The committee emphasized that while new technologies have the potential to positively impact the health of older adults, potential harms also need to be considered, particularly in the areas of privacy, informed consent, and autonomy.1
CONCLUSION
The world has changed since the release of the National Academies report in early 2020 because of the COVID-19 pandemic. SI/L are now everyday concerns for populations worldwide and are a special burden for older adults. Older adults are at high risk for morbidity and mortality due to COVID-19 and, on that basis, are likely to experience prolonged isolation. In communities where “stay-at-home” instructions have been imposed, older persons, especially those in residential or long term care facilities, may be restricted from interacting with spouses, family and friends who live within or outside these communities. Thus while social isolation during COVID-19 can be life-saving, it also deprives older adults of fundamental human needs for companionship and community. Many older adults do not have access to email, social media, or video-conferencing which has been widely implemented to compensate for the lack of in-person social contacts. Furthermore, the adequacy of these technologies is unstudied and their advantages maybe offset by missing aspects of human interaction such as touch and three-dimensional perspective. Reliance on technology solutions places a higher burden on those who lack access, such as older adults who are socioeconomically disadvantaged or those with cognitive impairment or sensory impairments. During this historic pandemic, decades of social epidemiologic research inform us that the health protective benefits of social distancing must be balanced by the human needs for sustaining social relationships. This report is a valuable resource to advance collective action and solutions during the period of COVID-19 and beyond.
Author Contributions
The preparation of this paper was a joint effort. Both authors are responsible for the entire manuscript.
The authors recognize and thank each of the members of the National Academies Committee on Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System: Dan G Blazer (Chair), Susan Beane, Cynthia Boyd, Linda Burnes Bolton, George Demiris, Nancy Donovan, Robert Espinoza, Colleen Galambos, Julianne Holt-Lunstad, James S House, Laurie Lovett Novak, Kathleen McGarry, Jeanne Miranda, Carla Perissinotto, Julianne G 132 Sebastian, Tracy A Lustig (Study Director), Jennifer Cohen (Program Officer)
Conflict of Interest and Funding : The authors report no conflict of interests. Both authors were members of the NASEM consensus committee and received no remuneration for this effort.
References
- 1.National Academies of Sciences E, and Medicine . The National Academies Press; Washington, D.C.: 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. [PubMed] [Google Scholar]
- 2.Health CoSDo . World Health Organization; Geneva: 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. [Google Scholar]
- 3.Kuiper JS, Zuidersma M, Oude Voshaar RC. Social relationships and risk of dementia: asystematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015;22:39–57. doi: 10.1016/j.arr.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Valtorta NK, Kanaan M, Gilbody S. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J, Smith TB. Loneliness and social isolation as risk factors for CVD: implications for evidence-based patient care and scientific inquiry. Heart. 2016;102:987–989. doi: 10.1136/heartjnl-2015-309242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holt-Lunstad J, Smith TB, Baker M. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 7.ML S. Preventing loneliness among the senior population during the COVID 19 crisis. Am J Manag Care (In Focus Blog). 2020 [Google Scholar]
- 8.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5:e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riesman D GN, Denny R. Yale University Press; New Haven: 1950. The Lonely Crowd. [Google Scholar]
- 10.Blazer DG. Social support and mortality in an elderly community population. Am J Epidemiol. 1982;115:684–694. doi: 10.1093/oxfordjournals.aje.a113351. [DOI] [PubMed] [Google Scholar]
- 11.Cudjoe TKM, Roth DL, Szanton SL. The Epidemiology of social isolation: National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci. 2020;75:107–113. doi: 10.1093/geronb/gby037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–1084. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson GOaT C.E. AARP Foundation; Washington, DC: 2018. Loneliness and Social Connections: A National Survey of Adults 45 and Older. [Google Scholar]
- 14.Putnam RD. Simon & Schuster; New York: 2000. Bowling Alone: the Collapse and Revival of American Community. [Google Scholar]
- 15.DiJulio BL HL, Munana C, Brodie M. Kaiser Family Foundation; 2018. Loneliness and social isolation in the United States, the United Kingdom, and Japan: An International Survey. [Google Scholar]
- 16.Domenech-Abella J, Mundo J, Haro JM. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA) J Affect Disord. 2019;246:82–88. doi: 10.1016/j.jad.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 17.Falk Dahl CA, Dahl AA. Lifestyle and social network in individuals with high level of social phobia/anxiety symptoms: a community-based study. Soc Psychiatry Psychiatr Epidemiol. 2010;45:309–317. doi: 10.1007/s00127-009-0069-6. [DOI] [PubMed] [Google Scholar]
- 18.Luo Y, Hawkley LC, Waite LJ. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74:907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim MH, Rodebaugh TL, Zyphur MJ. Loneliness over time: the crucial role of social anxiety. J Abnorm Psychol. 2016;125:620–630. doi: 10.1037/abn0000162. [DOI] [PubMed] [Google Scholar]
- 20.McHugh Power J, Hannigan C, Hyland P. Depressive symptoms predict increased social and emotional loneliness in older adults. Aging Ment Health. 2020;24:110–118. doi: 10.1080/13607863.2018.1517728. [DOI] [PubMed] [Google Scholar]
- 21.Schwarzbach M, Luppa M, Forstmeier S. Social relations and depression in late life-a systematic review. Int J Geriatr Psychiatry. 2014;29:1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- 22.Taylor HO, Taylor RJ, Nguyen AW. Social isolation, depression, and psychological distress among older adults. J Aging Health. 2018;30:229–246. doi: 10.1177/0898264316673511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donovan NJ, Wu Q, Rentz DM. Loneliness, depression and cognitive function in older U.S. adults. Int J Geriatr Psychiatry. 2016;32:564–573. doi: 10.1002/gps.4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barger SD, Messerli-Burgy N, Barth J. Social relationship correlates of major depressive disorder and depressive symptoms in Switzerland: nationally representative cross sectional study. BMC Public Health. 2014;14:273. doi: 10.1186/1471-2458-14-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Domenech-Abella J, Lara E, Rubio-Valera M. Loneliness and depression in the elderly: the role of social network. Soc Psychiatry Psychiatr Epidemiol. 2017;52:381–390. doi: 10.1007/s00127-017-1339-3. [DOI] [PubMed] [Google Scholar]
- 26.Evans IEM, Llewellyn DJ, Matthews FE. Social isolation, cognitive reserve, and cognition in older people with depression and anxiety. Aging Ment Health. 2019;23:1691–1700. doi: 10.1080/13607863.2018.1506742. [DOI] [PubMed] [Google Scholar]
- 27.Peerenboom L, Collard RM, Naarding P. The association between depression and emotional and social loneliness in older persons and the influence of social support, cognitive functioning and personality: A cross-sectional study. J Affect Disord. 2015;182:26–31. doi: 10.1016/j.jad.2015.04.033. [DOI] [PubMed] [Google Scholar]
- 28.Teo AR, Lerrigo R, Rogers MA. The role of social isolation in social anxiety disorder: a systematic review and meta-analysis. J Anxiety Disord. 2013;27:353–364. doi: 10.1016/j.janxdis.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 29.von Soest T, Luhmann M, Hansen T. Development of loneliness in midlife and old age: its nature and correlates. J Pers Soc Psychol. 2020;118:388–406. doi: 10.1037/pspp0000219. [DOI] [PubMed] [Google Scholar]
- 30.Wagner J, Ram N, Smith J. Personality trait development at the end of life: antecedents and correlates of mean-level trajectories. J Pers Soc Psychol. 2016;111:411–429. doi: 10.1037/pspp0000071. [DOI] [PubMed] [Google Scholar]
- 31.Holmen K, Ericsson K, Winblad B. Social and emotional loneliness among non-demented and demented elderly people. Arch Gerontol Geriatr. 2000;31:177–192. doi: 10.1016/s0167-4943(00)00070-4. [DOI] [PubMed] [Google Scholar]
- 32.Cohen-Mansfield J, Dakheel-Ali M, Marx MS. Which unmet needs contribute to behavior problems in persons with advanced dementia? Psychiatry Res. 2015;228:59–64. doi: 10.1016/j.psychres.2015.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benefield LE, Holtzclaw BJ. Aging in place: merging desire with reality. Nurs Clin North Am. 2014;49:123–131. doi: 10.1016/j.cnur.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Valtorta NK, Kanaan M, Gilbody S. Loneliness, social isolation and social relationships: what are we measuring? a novel framework for classifying and comparing tools. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 36.IOM . 2014. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington DC. [PubMed] [Google Scholar]
- 37.Lubben JE. Assessing social networks among elderly populations. Fam Community Health. 1988;11:42–52. [Google Scholar]
- 38.Lubben JE GM., Social work and health care in an aging world . Springer; New York: 2003. Centrality of Social Ties to the Health and Well Being of Older Adults. [Google Scholar]
- 39.Lubben J, Blozik E, Gillmann G. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 40.Steptoe A, Shankar A, Demakakos P. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 42.Hughes ME, Waite LJ, Hawkley LC. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Jong Gierveld J KF. The development of a Rasch-type loneliness scale. Applied Psychological Measurement. 1985;9:289–299. [Google Scholar]
- 44.De Jong Gierveld JVT. Vol. 28. Research on Aging; 2006. (A 6-Item Scale for Overall, Emotional, and Social Loneliness). T. [Google Scholar]
- 45.Koenig HG, Westlund RE, George LK. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34:61–69. doi: 10.1016/S0033-3182(93)71928-3. [DOI] [PubMed] [Google Scholar]
- 46.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 47.Drageset J, Eide GE, Kirkevold M. Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: a five-year follow-up study. J Clin Nurs. 2013;22:106–114. doi: 10.1111/j.1365-2702.2012.04209.x. [DOI] [PubMed] [Google Scholar]
- 48.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hakulinen C, Pulkki-Raback L, Virtanen M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. 2018;104:1536–1542. doi: 10.1136/heartjnl-2017-312663. [DOI] [PubMed] [Google Scholar]
- 50.Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72:229–238. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- 51.Manemann SM, Chamberlain AM, Roger VL. Perceived social isolation and outcomes in patients with heart failure. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.008069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jeuring HW, Stek ML, Huisman M. A six-year prospective study of the prognosis and predictors in patients with late-life depression. Am J Geriatr Psychiatry. 2018;26:985–997. doi: 10.1016/j.jagp.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 54.Teo AR, Choi H, Andrea SB. Does mode of contact with different types of social relationships predict depression in older adults? evidence from a nationally representative survey. J Am Geriatr Soc. 2015;63:2014–2022. doi: 10.1111/jgs.13667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Calati R, Ferrari C, Brittner M. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord. 2019;245:653–667. doi: 10.1016/j.jad.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 56.Troya MI, Babatunde O, Polidano K. Self-harm in older adults: systematic review. Br J Psychiatry. 2019;214:186–200. doi: 10.1192/bjp.2019.11. [DOI] [PubMed] [Google Scholar]
- 57.Penninkilampi R, Casey AN, Singh MF. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2018;66:1619–1633. doi: 10.3233/JAD-180439. [DOI] [PubMed] [Google Scholar]
- 58.Stern Y. Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol. 2012;11:1006–1012. doi: 10.1016/S1474-4422(12)70191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Donovan NJ, Okereke OI, Vannini P. Association of Higher Cortical Amyloid burden with loneliness in cognitively normal older adults. JAMA psychiatry. 2016;73:1230–1237. doi: 10.1001/jamapsychiatry.2016.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.d'Oleire Uquillas F, Jacobs HIL, Biddle KD. Regional tau pathology and loneliness in cognitively normal older adults. Transl Psychiatry. 2018;8:282. doi: 10.1038/s41398-018-0345-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hawton A, Green C, Dickens AP. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res. 2011;20:57–67. doi: 10.1007/s11136-010-9717-2. [DOI] [PubMed] [Google Scholar]
- 62.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 63.Kent de Grey RG, Uchino BN, Trettevik R. Social support and sleep: a meta-analysis. Health Psychol. 2018;37:787–798. doi: 10.1037/hea0000628. [DOI] [PubMed] [Google Scholar]
- 64.Williams NJ, Grandner MA, Wallace DM. Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 2016;18:103–107. doi: 10.1016/j.sleep.2015.02.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cacioppo JT, Hawkley LC, Crawford LE. Loneliness and health: potential mechanisms. Psychosom Med. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 66.Hawkley LC, Thisted RA, Masi CM. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jacobs JM, Cohen A, Hammerman-Rozenberg R. Global sleep satisfaction of older people: the Jerusalem Cohort Study. J Am Geriatr Soc. 2006;54:325–329. doi: 10.1111/j.1532-5415.2005.00579.x. [DOI] [PubMed] [Google Scholar]
- 68.Kurina LM, Knutson KL, Hawkley LC. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011;34:1519–1526. doi: 10.5665/sleep.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Soc Sci Med. 2016;152:80–86. doi: 10.1016/j.socscimed.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 70.Brown EG, Gallagher S, Creaven AM. Loneliness and acute stress reactivity: a systematic review of psychophysiological studies. Psychophysiology. 2018;55:e13031. doi: 10.1111/psyp.13031. [DOI] [PubMed] [Google Scholar]
- 71.Hawkley LC, Masi CM, Berry JD. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 72.Blanquet M, Debost-Legrand A, Gerbaud L. Metabolic syndrome and social deprivation: results of a French observational multicentre survey. Fam Pract. 2016;33:17–22. doi: 10.1093/fampra/cmv086. [DOI] [PubMed] [Google Scholar]
- 73.Whisman MA. Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychol. 2010;29:550–554. doi: 10.1037/a0020760. [DOI] [PubMed] [Google Scholar]
- 74.Grant N, Hamer M, Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Ann Behav Med. 2009;37:29–37. doi: 10.1007/s12160-009-9081-z. [DOI] [PubMed] [Google Scholar]
- 75.McCrory C, Finucane C, O'Hare C. Social disadvantage and social isolation are associated with a higher resting heart rate: evidence from the irish longitudinal study on ageing. J Gerontol B Psychol Sci Soc Sci. 2016;71:463–473. doi: 10.1093/geronb/gbu163. [DOI] [PubMed] [Google Scholar]
- 76.Hostinar CE, Sullivan RM, Gunnar MR. Psychobiological mechanisms underlying the social buffering of the hypothalamic-pituitary-adrenocortical axis: a review of animal models and human studies across development. Psychol Bull. 2014;140:256–282. doi: 10.1037/a0032671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cacioppo JT, Cacioppo S, Capitanio JP. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66:733–767. doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schutter N, Holwerda TJ, Stek ML. Loneliness in older adults is associated with diminished cortisol output. J Psychosom Res. 2017;95:19–25. doi: 10.1016/j.jpsychores.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 79.Hackett RA, Hamer M, Endrighi R. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37:1801–1809. doi: 10.1016/j.psyneuen.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 80.Eisenberger NI, Moieni M, Inagaki TK. In sickness and in health: the co-regulation of inflammation and social behavior. Neuropsychopharmacology. 2017;42:242–253. doi: 10.1038/npp.2016.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ford ES, Loucks EB, Berkman LF. Social integration and concentrations of C-reactive protein among US adults. Ann Epidemiol. 2006;16:78–84. doi: 10.1016/j.annepidem.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 82.Heffner KL, Waring ME, Roberts MB. Social isolation, C-reactive protein, and coronary heart disease mortality among community-dwelling adults. Soc Sci Med. 2011;72:1482–1488. doi: 10.1016/j.socscimed.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shankar A, McMunn A, Banks J. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011;30:377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- 84.Kim DA, Benjamin EJ, Fowler JH. Social connectedness is associated with fibrinogen level in a human social network. Proc Biol Sci. 2016;283:1–7. doi: 10.1098/rspb.2016.0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nersesian PV, Han HR, Yenokyan G. Loneliness in middle age and biomarkers of systemic inflammation: findings from midlife in the united states. Soc Sci Med. 2018;209:174–181. doi: 10.1016/j.socscimed.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cole SW, Hawkley LC, Arevalo JM. Social regulation of gene expression in human leukocytes. Genome Biol. 2007;8:R189. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Creswell JD, Irwin MR, Burklund LJ. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sander R. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Nurs Older People. 2005;17:40. doi: 10.7748/nop.17.1.40.s11. [DOI] [PubMed] [Google Scholar]
- 89.Ageing CfPo: Rapid Review:Loneliness-Evidence of the effectiveness of Interventions. Center for Policy on Ageing - Rapid Review, 2014; 1--55
- 90.Masi CM, Chen HY, Hawkley LC. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26:147–157. doi: 10.1111/hsc.12367. [DOI] [PubMed] [Google Scholar]
- 92.Hawkley L, Preacher KJ, Cacioppo JT. Oxford Handbook of Methods in Positive Psychology. Oxford Press; New York: 2007. Multilevel modeling of social interactions and mood in lonely and socially connected individuals: the MacArthur social neuroscience studies; pp. 559–575. [Google Scholar]
- 93.Cacioppo S, Grippo AJ, London S. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10:238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13:447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mann F, Bone JK, Lloyd-Evans B. A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2017;52:627–638. doi: 10.1007/s00127-017-1392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lindsay EK, Young S, Brown KW. Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc Natl Acad Sci U S A. 2019;116:3488–3493. doi: 10.1073/pnas.1813588116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Choi NG PR, Marti CN, Stevens CJ. Improving social connectedness for homebound older adults: randomized controlled tiral of tele-delivered behavioral activation versus tele-delivered friendly visits. Am J Geriatr Psychiatry. 2020;28:698–708. doi: 10.1016/j.jagp.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]