Abstract
Objective:
In this study we assess whether changes in ZIP code–level density of medical marijuana facilities are related to changes in rates of opioid poisonings and opioid use disorder hospitalizations in California.
Method:
A panel study using California hospital discharge data was conducted to assess the relationship between density of medical marijuana dispensaries and opioid poisonings and use disorder. There were 8,536 space-time units at the ZIP code level. Outcome measures included ZIP code counts of opioid poisonings and opioid use disorder; independent variables were local- and adjacent-area medical marijuana dispensaries and demographic and economic characteristics.
Results:
Independent of effects for covariates, densities of medical marijuana dispensaries were positively related to opioid use disorder (RR = 1.05, CI [1.03, 1.06]) and opioid poisonings (RR = 1.04, CI [1.02, 1.05]) in local areas, but negatively related to opioid misuse in spatially adjacent areas (RR = 0.91, CI [0.88, 0.94] for opioid use disorder, RR = 0.89, CI [0.86, 0.93] for opioid poisonings).
Conclusions:
Although state-level studies suggest that more liberal marijuana policies may result in fewer opioid overdose deaths, our results within one state suggest that local availability of medical marijuana may not reduce those deaths. The relationship appears to be more complex, possibly based on socioeconomic conditions within and adjacent to areas with higher densities of medical marijuana dispensaries.
Drug overdose was the leading cause of death in the United States for those ages 25–44 in 2017, with prescription and illicit opioids being involved in most cases (Centers for Disease Control and Prevention, 2019). The increase in drug overdose deaths has been cited as one reason the life expectancy rate in the United States is decreasing (Dowell et al., 2017), particularly among middle-age Whites and Hispanics (Narayan et al., 2019). At the ZIP code level in California, opioid poisonings occur more often in ZIP code areas with more manufacturing or construction jobs and lower unemployment rates (Cerdá et al., 2017). Conversely, higher unemployment rates were related to higher rates of opioid abuse in Indiana at the county level (Wright et al., 2014) and heroin poisonings in Pennsylvania ZIP code areas (Mair et al., 2018). These findings suggest regional differences related to where opioid poisonings and abuse/ dependence occur.
The growth in opioid overdose deaths is partly attributable to an increase of opioid prescriptions provided for chronic pain management (Guy et al., 2017). However, this increase has not been consistent across the country. As one example, from 2013 to 2015 overdose deaths increased by 2% in California versus 38% in Pennsylvania (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2018). One reason for California’s slower rate of increase in overdose deaths may be that marijuana has been available there for medical use since 1996. Those who suffer from chronic pain may be medicating with marijuana, which has a practically nonexistent risk for overdose, as opposed to opioids.
The possible effectiveness of cannabis to address chronic pain has received renewed interest because of the rise in opioid overdoses and changes in the legal status of marijuana in many states. This is important because doctors most often provide recommendations for marijuana use to treat chronic pain (Aggarwal et al., 2009; Bonn-Miller al., 2014; Ilgen et al. 2013; Nunberg et al., 2011; Nussbaum et al., 2011, 2015; Reinarman et al., 2011; Walsh et al. 2013).
At the individual level, review studies suggest that cannabis can inhibit chronic pain, but little is known about the optimal dosage, how best to administer cannabis, and the potential adverse side effects (Hill et al., 2017). Patients using cannabis who report a reduction in chronic pain (Collen, 2012; Haroutounian et al., 2016; National Academies of Sciences, Engineering, and Medicine, 2017) are less likely to be diagnosed with a substance use disorder than those using opioids (Feingold et al., 2017) and are less likely to use opioids if also using cannabis (Kral et al., 2015; Reiman et al., 2017; Vyas et al., 2018). However, these studies rely primarily on patient reports of the changes in their pain symptoms. In some cases, patients report substituting prescription drugs with cannabis (Corroon et al., 2017; Vyas et al., 2018). Yet, at least one study suggests that those who used medical marijuana were more likely to use a variety of prescription drugs than those who did not use medical marijuana (Caputi & Humphreys, 2018). Campbell and colleagues (2018) found that patients who used medical marijuana for pain were not more likely to discontinue use of opioids or to report lower pain severity. Marijuana use over time was associated with more use of nonprescription opioids and higher rate of opioid use disorder (Olfson et al., 2018). Thus, although some evidence suggests that marijuana may be an effective treatment for chronic pain, this evidence is not universal. Further, studies at the individual level have not examined whether cannabis use for chronic pain—or as a substitution for opioids—decreases opioid overdose deaths.
In support of the hypothesis that the ability to use marijuana for medical purposes may reduce opioid overdose deaths, Bachhuber and colleagues (2014) found that states with medical cannabis laws have lower rates of opioid overdose deaths. Similarly, states that allow medical marijuana dispensaries (MMDs) have lower treatment admissions rates for opioid addictions (Powell et al., 2018). These reductions in opioid overdoses occurred in Colorado after increasing availability of cannabis through legalization of recreational use (Livingston et al., 2017). Examining prescribing patterns using data on Medicare Part D, Bradford and colleagues (2018) found that states that allowed dispensaries had a 14.4% lower rate for daily doses of opioids prescribed, whereas allowing home cultivation decreased daily doses of prescription opioids by 6.9%. A similar study examining prescriptions of opioids among Medicaid enrollees found a lower rate of prescribing when states had a law that allowed for medical marijuana use (Wen & Hockenberry, 2018). This work suggests that at the state level, medical marijuana laws are related to lower rates of prescribing and opioid overdose deaths, and these associations appear to be even stronger when states allow cannabis to be sold via dispensaries. However, these results are not universal. Shover and colleagues (2019) updated the study from Bachhuber et al. (2014) with an additional 7 years of data. That study found that medical marijuana laws were related to higher rates of opioid overdoses.
Early findings from studies of more liberal marijuana policies and opioid overdoses are consistent with availability theory (Stockwell & Gruenewald, 2004), which states that substances that are more readily available have higher rates of use, leading to a greater number of people who misuse those substances and more substance-related problems. In the case of opioids and marijuana, although marijuana does have adverse effects, the risk for overdose is much lower than that for opioids. Increasing the geographic availability of marijuana, then, could decrease opioid overdose deaths, assuming that substitution or self-medicating is occurring.
Missing from the work presented here is whether the early relationships seen at the state level are confirmed at smaller units of geography, such as Census tracts or ZIP codes. Having a state-level law that enables marijuana to be sold via dispensaries is not the same as measuring the actual availability of marijuana through dispensaries within smaller regions of states. For example, a state can allow MMDs to operate, but city officials could choose to ban dispensaries from opening within their city limits, as is the case in Irvine, California. In this case, availability of marijuana through dispensaries would be limited for residents in some cities but not others across a state. Thus, local effects of dispensaries may look different for community- or state-level access—as has been tested previously (Bachhuber et al., 2014; Livingston et al., 2017)—if the effects of dispensaries are localized to specific high demand or disadvantaged areas. Community-level access to marijuana might be better reflected through state-level policies, as in previous studies, or through the use of spatial lags (e.g., the density of MMDs in adjacent areas), where dispensaries may not be related to problems at larger aggregated units. We recognize that, as a population-level study, we are not able to speak to whether marijuana use reduces pain or is used by patients as a substitute to opioids. However, population-level studies, such as this, can point to potential levers that can be used by local communities to reduce problematic or harmful substance use.
In this study, we assess whether changes in ZIP code–level density of medical marijuana facilities are related to changes in rates of opioid overdose and opioid abuse/dependence hospitalizations in California. Our study is designed to understand the effect of medical marijuana dispensaries on opioid poisonings and abuse or dependence. For that reason, regardless of whether a dispensary was licensed, we included density of all dispensaries to understand this relationship. We hypothesize that greater physical availability of medical marijuana (as measured by density of MMDs) will be related to fewer opioid poisonings and lower rates of opioid abuse/dependence across ZIP codes. Findings from this study could point to local-level policy decisions concerned with whether to allow dispensaries or regulate the density of these dispensaries in local areas.
Method
Study design and sample
We conducted a panel study using California hospital discharge data from 2012 to 2016 to assess the relationship between density of medical marijuana dispensaries and opioid poisonings and abuse/dependence. There were 8,536 space-time units at the ZIP code level.
Measures
Data on hospital discharges were obtained from California’s Office of Statewide Health and Planning Development, which maintains data on all hospitalizations in which the patient remained hospitalized for at least one overnight. The study population includes individuals ages 13 and older, the age range that experiences opioid abuse/dependence and poisonings. Aggregate counts of opioid poisonings and opioid use disorders (OUDs) were calculated by ZIP code using patient-level records. As the classification system switched from ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) to ICD-10-CM in the last quarter of 2015, we used two sets of codes to compute outcome totals. For the majority of the data, the ICD-9-CM codes 965.0x (poisoning by opiates and related narcotics), E850.0 (accidental poisoning by heroin), E850.1 (accidental poisoning by methadone), and E850.2 (accidental poisoning by opiates and other narcotics) were used. Analogous ICD-10-CM codes were T40.0X1-4 (poisoning by opium), T40.1X1-4 (poisoning by heroin), T40.2X1-4 (poisoning by other opioids), T40.3X1-4 (poisoning by methadone), T40.4X1-4 (poisoning by other synthetic narcotics), T40.601-4 (poisoning by unspecified narcotics), and T40.691-4 (poisoning by other narcotics) (https://www.cdc.gov/drugoverdose/pdf/pdo_guide_to_icd-9-cm_and_icd-10_codes-a.pdf). For the transition between ICD-9-CM and ICD-10-CM, we relied on previous work (Hume et al., 2017; Moore & Barrett, 2017). We aggregated the number of events to the ZIP code of the patient. Of all the ZIP codes included, 109 ZIP codes had total population counts of fewer than five people (mostly zeros). Since our models adjusted for the expected counts of each outcome based on the entire population count in each ZIP code, we increased the total population to five people in these areas to allow for non-zero risks. These areas were also assigned the mean value of all other ZIP codes for variables derived from GeoLytics (2016) data. On average, ZIP codes had 34 hospitalizations for OUD and about four opioid poisonings per year (Table 1).
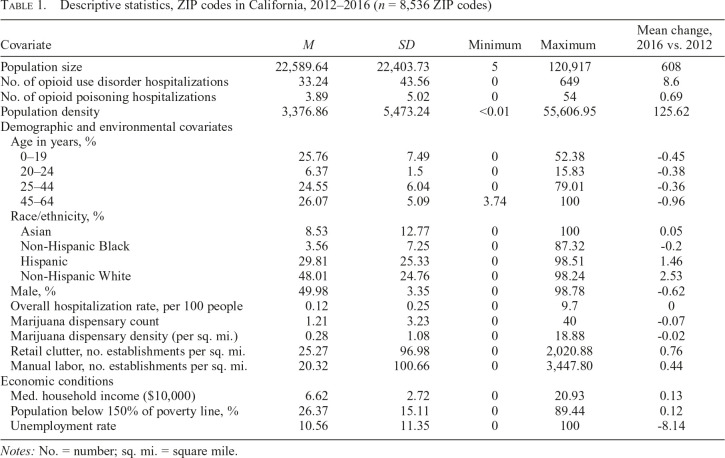
Table 1.
Descriptive statistics, ZIP codes in California, 2012–2016 (n = 8,536 ZIP codes)
| Covariate | M | SD | Minimum | Maximum | Mean change, 2016 vs. 2012 |
| Population size | 22,589.64 | 22,403.73 | 5 | 120,917 | 608 |
| No. of opioid use disorder hospitalizations | 33.24 | 43.56 | 0 | 649 | 8.6 |
| No. of opioid poisoning hospitalizations | 3.89 | 5.02 | 0 | 54 | 0.69 |
| Population density | 3,376.86 | 5,473.24 | <0.01 | 55,606.95 | 125.62 |
| Demographic and environmental covariates | |||||
| Age in years, % | |||||
| 0–19 | 25.76 | 7.49 | 0 | 52.38 | -0.45 |
| 20–24 | 6.37 | 1.5 | 0 | 15.83 | -0.38 |
| 25–44 | 24.55 | 6.04 | 0 | 79.01 | -0.36 |
| 45–64 | 26.07 | 5.09 | 3.74 | 100 | -0.96 |
| Race/ethnicity, % | |||||
| Asian | 8.53 | 12.77 | 0 | 100 | 0.05 |
| Non-Hispanic Black | 3.56 | 7.25 | 0 | 87.32 | -0.2 |
| Hispanic | 29.81 | 25.33 | 0 | 98.51 | 1.46 |
| Non-Hispanic White | 48.01 | 24.76 | 0 | 98.24 | 2.53 |
| Male, % | 49.98 | 3.35 | 0 | 98.78 | -0.62 |
| Overall hospitalization rate, per 100 people | 0.12 | 0.25 | 0 | 9.7 | 0 |
| Marijuana dispensary count | 1.21 | 3.23 | 0 | 40 | -0.07 |
| Marijuana dispensary density (per sq. mi.) | 0.28 | 1.08 | 0 | 18.88 | -0.02 |
| Retail clutter, no. establishments per sq. mi. | 25.27 | 96.98 | 0 | 2,020.88 | 0.76 |
| Manual labor, no. establishments per sq. mi. | 20.32 | 100.66 | 0 | 3,447.80 | 0.44 |
| Economic conditions | |||||
| Med. household income ($10,000) | 6.62 | 2.72 | 0 | 20.93 | 0.13 |
| Population below 150% of poverty line, % | 26.37 | 15.11 | 0 | 89.44 | 0.12 |
| Unemployment rate | 10.56 | 11.35 | 0 | 100 | -8.14 |
Notes: No. = number; sq. mi. = square mile.
We operationalized the physical availability of medical marijuana as the number of dispensaries open in a given ZIP code for a specific year per area (in square miles). Locations of MMDs were obtained from Weedmaps.com for 2012 through 2016 approximately monthly to better model locations of dispensaries. In a study of Los Angeles, Pedersen and colleagues (2018) found that Weedmaps was able to identify 95% of open dispensaries in Los Angeles County, using data from 2016 and verifying the search through multiple methods (e.g., Google maps, calling)1.
We aggregated MMDs to the ZIP code level, such that all unique medical marijuana locations in a given year were included, even if they were only open for a partial year. Our models included the number of MMDs/mile2 as well as MMD spatial lags. These lags were calculated as the total number of MMDs in all neighboring ZIP codes (i.e., ZIP codes sharing a border, regardless of length) divided by the total area of neighboring ZIP codes. We created an alternate measure of the physical availability of MMDs by only using those dispensaries that were open at the beginning of a year. This measure was used in sensitivity analyses discussed below.
We used sociodemographic measures from GeoLytics (2016). This data set contains annual population-level sociodemographic indicators for ZIP codes. We included measures of the percentage of individuals across various age groups (0–19 years, 20–24 years, 25–44 years, and 45–64 years), with the referent group the percentage of individuals 65 years or older. Asian/Asian American, non-Hispanic Black, and Hispanic were designated race/ethnicity covariates (with percentage of White individuals as the referent group). We also included the percentage male and population density quartiles, with ZIP codes with less than 41.52 people/mile2 used as the reference group.
GeoLytics data also provided several measures of ZIP code–level economic conditions. We included the percentage of individuals in local and spatially lagged areas living below 150% of the poverty level, the median household income (per $10,000), and the percentage of unemployed individuals. Last, we included Office of Statewide Health and Planning Development data on the overall hospitalization rate for each ZIP code.
We used measures of manual labor and retail clutter densities. Counts of these establishments were aggregated using the North American Industry Classification System (NAICS) codes from ZIP Code Business Patterns data (U.S. Census Bureau, 2016). For manual labor, we used the following codes: Agriculture, Forestry, Fishing and Hunting (NAICS Sector 11); Mining, Quarrying, and Oil and Gas Extraction (Sector 21); Construction (Sector 23); Manufacturing (Sectors 31–33); Wholesale Trade (Sector 42); Transportation and Warehousing (Sectors 48–49); and Utilities (Sector 22). NAICS Sectors 44–45 (Retail Trade) and 72 (Accommodation and Food Services) were used to create the retail clutter variable. We divided counts of these establishments by the total area (in square miles) of each ZIP code. These were subsequently multiplied by 10 (i.e., the number of establishments per 10 square miles) to aid interpretation as resulting credible intervals were otherwise too narrow.
Because ZIP code designations and boundaries may shift over time, we included a measure reflecting this misalignment (Mair et al., 2013). This measure was calculated as the proportion of the population that would have fallen outside the boundaries of each best-matched previous-year ZIP code.
Data analysis procedures
We used a Bayesian hierarchical approach to analyze 5 years of space-time ZIP code–level data. To account for similarity among neighboring spatial units as well as over-dispersion, we incorporated two random effects. A spatially autocorrelated conditionally autoregressive (CAR) random effect was included in conjunction with a spatially unstructured random effect for each space-time unit. This is a standard modeling approach for analyzing spatial disease data (Besag et al., 1991; Gelfand et al., 2010). Since our outcome measures were counts, we used Poisson regression:
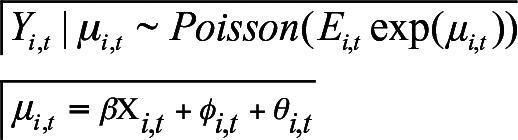 |
Yi,t is the count of opioid poisonings or OUDs in each ZIP code i per year t. Ei,t is the expected count of each outcome calculated relative to the total population count for each space-time unit i,t. exp( ) is each unit’s relative rate.
) is each unit’s relative rate.  is composed of
is composed of  a vector of coefficient estimates for the intercept and each fixed effect as observed in Xi,t, and
a vector of coefficient estimates for the intercept and each fixed effect as observed in Xi,t, and  and
and  vectors of spatially structured and nonspatial random effects, respectively.
vectors of spatially structured and nonspatial random effects, respectively.
We assessed analogous models for opioid poisoning and OUD outcomes. Of primary interest, each model included MMD density with a ZIP code and its spatial lag. We adjusted for economic conditions (percentage of the population below 150% of the poverty level, percentage of the population that is unemployed, and median household income), population demographics (race and ethnicity distributions, age distributions, percentage male, population density), retail clutter and manual labor establishment densities, and the overall hospitalization rate.
Bayesian hierarchical models are commonly run using Markov Chain Monte Carlo (MCMC) simulations. Integrated nested Laplace approximation (INLA) is a deterministic approach that has consistently produced similar estimates with greatly improved computational efficiency. As such, we used the R package R-INLA to estimate our models (Rue et al., 2009).
Results
There were an average of 33.24 (SD = 43.56) OUD hospitalizations and 3.89 (SD = 5.02) opioid poisoning hospitalizations per ZIP code per year from 2012 to 2016 (Table 1). Each space-time unit had a mean count of 1.21 (SD = 3.23) marijuana dispensaries, which decreased by 0.07 from 2012 to 2016. The average dispensary density was 0.28 per square mile (SD = 1.08). The mean population density was 3,376.86 per square mile (SD = 5,473.24). Race/ethnicity percentages were, on average, as follows: 8.53 (SD = 12.77) Asian/Asian American, 3.56 (SD = 7.25) Black/African
American, 29.81 (SD = 25.33) Hispanic, and 48.01 (SD = 24.76) non-Hispanic White. The median household income was $66,194 (SD = $2,723), and an average of 26.37% (SD = 15.11) of the population lived below 150% of the poverty line. The percentage of unemployed residents per ZIP code per year was 10.56% (SD = 11.35) during the study period. Densities of retail and manual labor establishments were 25.27 (SD = 96.98) and 20.32 (SD = 100.66) per square mile, respectively.
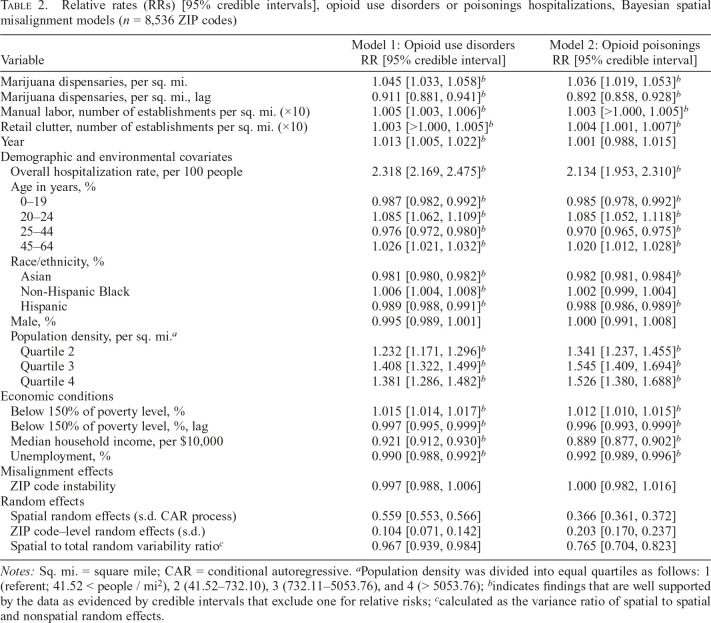
Table 2 presents the results from our Bayesian CAR models. Model 1 shows the results for number of OUDs, whereas Model 2 provides the results for opioid poisonings. In general, findings were fairly consistent across both outcome measures. For OUDs, the density of MMDs in local areas was related to higher rates of OUD and opioid poisonings. However, the density of MMDs in spatially adjacent (e.g., lagged) areas was associated with lower rates of OUDs and poisonings. Retail clutter (i.e., more establishments/mile2) was related to higher rates of OUD and opioid poisonings. Number of manual labor establishments and overall hospitalization rate all had a positive relationship with both OUDs and poisonings. Over time, there is a well-supported effect of an increase in the rate of OUDs, but not for opioid poisonings.
Table 2.
Relative rates (RRs) [95% credible intervals], opioid use disorders or poisonings hospitalizations, Bayesian spatial misalignment models (n = 8,536 ZIP codes)
| Variable | Model 1: Opioid use disorders RR [95% credible interval] | Model 2: Opioid poisonings RR [95% credible interval] |
| Marijuana dispensaries, per sq. mi. | 1.045 [1.033, 1.058]b | 1.036 [1.019, 1.053]b |
| Marijuana dispensaries, per sq. mi., lag | 0.911 [0.881, 0.941]b | 0.892 [0.858, 0.928]b |
| Manual labor, number of establishments per sq. mi. (×10) | 1.005 [1.003, 1.006]b | 1.003 [>1.000, 1.005]b |
| Retail clutter, number of establishments per sq. mi. (×10) | 1.003 [>1.000, 1.005]b | 1.004 [1.001, 1.007]b |
| Year | 1.013 [1.005, 1.022]b | 1.001 [0.988, 1.015] |
| Demographic and environmental covariates | ||
| Overall hospitalization rate, per 100 people | 2.318 [2.169, 2.475]b | 2.134 [1.953, 2.310]b |
| Age in years, % | ||
| 0–19 | 0.987 [0.982, 0.992]b | 0.985 [0.978, 0.992]b |
| 20–24 | 1.085 [1.062, 1.109]b | 1.085 [1.052, 1.118]b |
| 25–44 | 0.976 [0.972, 0.980]b | 0.970 [0.965, 0.975]b |
| 45–64 | 1.026 [1.021, 1.032]b | 1.020 [1.012, 1.028]b |
| Race/ethnicity, % | ||
| Asian | 0.981 [0.980, 0.982]b | 0.982 [0.981, 0.984]b |
| Non-Hispanic Black | 1.006 [1.004, 1.008]b | 1.002 [0.999, 1.004] |
| Hispanic | 0.989 [0.988, 0.991]b | 0.988 [0.986, 0.989]b |
| Male, % | 0.995 [0.989, 1.001] | 1.000 [0.991, 1.008] |
| Population density, per sq. mi.a | ||
| Quartile 2 | 1.232 [1.171, 1.296]b | 1.341 [1.237, 1.455]b |
| Quartile 3 | 1.408 [1.322, 1.499]b | 1.545 [1.409, 1.694]b |
| Quartile 4 | 1.381 [1.286, 1.482]b | 1.526 [1.380, 1.688]b |
| Economic conditions | ||
| Below 150% of poverty level, % | 1.015 [1.014, 1.017]b | 1.012 [1.010, 1.015]b |
| Below 150% of poverty level, %, lag | 0.997 [0.995, 0.999]b | 0.996 [0.993, 0.999]b |
| Median household income, per $10,000 | 0.921 [0.912, 0.930]b | 0.889 [0.877, 0.902]b |
| Unemployment, % | 0.990 [0.988, 0.992]b | 0.992 [0.989, 0.996]b |
| Misalignment effects | ||
| ZIP code instability | 0.997 [0.988, 1.006] | 1.000 [0.982, 1.016] |
| Random effects | ||
| Spatial random effects (s.d. CAR process) | 0.559 [0.553, 0.566] | 0.366 [0.361, 0.372] |
| ZIP code–level random effects (s.d.) | 0.104 [0.071, 0.142] | 0.203 [0.170, 0.237] |
| Spatial to total random variability ratioc | 0.967 [0.939, 0.984] | 0.765 [0.704, 0.823] |
Notes: Sq. mi. = square mile; CAR = conditional autoregressive. aPopulation density was divided into equal quartiles as follows: 1 (referent; 41.52 < people / mi2), 2 (41.52–732.10), 3 (732.11–5053.76), and 4 (> 5053.76); bindicates findings that are well supported by the data as evidenced by credible intervals that exclude one for relative risks; ccalculated as the variance ratio of spatial to spatial and nonspatial random effects.
A higher percentage of Asian and Hispanic residents was related to fewer hospitalizations for OUDs and poisonings, whereas a higher percentage of non-Hispanic Blacks was associated with more OUDs and poisonings. A higher percentage of men in a ZIP code was related to fewer OUDs and poisonings. ZIP codes with higher population densities had more OUDs and poisonings.
The relationship of the percentage of individuals living 150% below the poverty level to OUDs was similar to what was found with MMDs: associated with greater OUDs in local ZIP codes, but fewer in adjacent ZIP codes. Both median household income and percentage unemployment were related to fewer OUDs and poisonings.
Effects related to ZIP code instability were not well supported in our model. The high spatial-to-total random variability ratios (e.g., 0.966 [95% credible interval 0.937, 0.983] for Model 1) suggests that substantial spatial autocorrelation exists, and neighboring ZIP codes tend to exhibit similarities in opioid-related outcomes even after adjusting for other local covariates. Sensitivity analyses using only dispensaries open in January of each year showed similar findings as they related to MMDs.
Discussion
In our study, we sought to understand how changes in density of medical marijuana dispensaries were related to changes in opioid poisonings and abuse/dispensaries. Because our study was conducted with ZIP codes as the unit analysis, we were not able to assess mechanisms by which density is related to opioid misuse at the individual level, if ecological relationships were found. We are careful in how we discuss our findings in order to not overstate our conclusions or attribute our results to individual-level behaviors.
Specifically, we hypothesized that the density of both local and spatially lagged MMDs would be negatively related to OUDs and opioid poisonings. Although we did find this negative relationship for spatially lagged (e.g., adjacent) ZIP codes, we did not find it in local ZIP code areas. In fact, a higher density of MMDs in local ZIP codes was positively related to both outcome measures. Although our study cannot identify the individual-level mechanisms that contribute to these findings, the results may be indicative of polydrug use occurring in these areas, placing individuals at greater risk for opioid misuse (Caputi & Humphreys, 2018).
Although some chronic pain patients may be self-medicating with marijuana (Corroon et al., 2017; Vyas et al., 2018), our results suggest that geographic availability of MMDs is not related to lower rates of opioid misuse within the same ZIP code, as has been seen in previous work at the state level (Bachhuber et al., 2014; Livingston et al., 2017; Powell et al., 2018). Our findings within ZIP codes are more similar to findings from Shover and colleagues (2019), who found a positive relationship between medical and recreational marijuana laws and opioid overdoses when studying this relationship over a longer period. It may be that dispensaries are locating themselves in areas where they expect the greatest concentration of consumers/patients, which are also the areas with higher levels of opioid use for medical conditions. Although we do control for overall hospital utilization, certain types of diagnoses requiring an overnight hospital stay more often result in opioid prescriptions, with entrepreneurial dispensary owners seeking to capitalize on locations with higher concentrations of these populations to increase their medical marijuana sales.
As hypothesized, we found a negative association between lagged MMDs and OUD and opioid poisonings. The discrepancy in associations between within-area versus spatially lagged dispensaries with opioid-related outcomes may be due to several factors. Individuals who use medical marijuana for chronic pain treatment (rather than opioids) may have the resources to live somewhat near locations of dispensaries, but not within the same ZIP code. The similar pattern between spatially lagged measures of percentage of population living below 150% of the poverty level and opioid-related outcomes might suggest that people living in slightly wealthier areas may be using dispensaries and opioids differently. People living in areas with less poverty may be using marijuana as a substitute for opioids and not along with opioids; they may also be less likely to live in a ZIP code with dispensaries. At the ecological level, the relationships that we posit above cannot be assessed (c.f. Caputi, 2019; Caputi & Sabet, 2018), but our ecological findings might provide direction for future inquiry into this area using individual-level data.
Our study found relationships that are similar to previous work. Having more manual labor establishments may be an indicator of the local demand for solutions to address chronic pain (Cerdá et al., 2017; Mair et al., 2018). Our findings are consistent with the relationship Cerdá et al. (2017) found with unemployment rates, yet not consistent with the work from Wright and colleagues (2014) in Indiana or Mair et al. (2018) in Pennsylvania. Both our study and that by Cerdá and colleagues were conducted in California, suggesting that how unemployment is related to OUDs and poisonings may differ regionally across the United States.
Last, we note that our time trend variable is positive and well supported for OUDs but not for opioid poisonings. This trend may be an indication of the potency of opioids being misused. As tighter controls on prescription practices are being placed on physicians, heroin and fentanyl use is rising. When individuals overdose on these—especially fentanyl—fatalities are more common. Thus, the lack of change in poisonings may signal that emergency medical personnel are not arriving in time to transport these individuals to the hospital for care.
Limitations
The current study has several important limitations. Our study is ecological in nature, in that we are examining population-level data. We are not able to identify specific individual mechanisms that may result in the outcomes found here. Thus, the findings should be interpreted cautiously. Our study uses data from Weedmaps.com to determine open dispensaries. During the study period, Weedmaps.com required fees to be included on their listings of dispensary locations. Although the locations of these dispensaries have shown to be relatively accurate in recent years (see Pedersen et al., 2018), we did not assess their accuracy in early years of collecting these data.
We do not have measures of prescribing practices by physicians. Understanding how the supply of prescription opioids affects the relationship between MMDs and hospitalizations for opioid misuse may provide more context about why density of local dispensaries is related to higher rates of OUD and poisonings. Using hospital discharge data allows us to assess correlates of OUD and poisonings that result in at least one overnight stay (as a proxy of the seriousness of the disorder), but it does not provide information on the type of opioid that was abused/misused. We also have no data on substitution of cannabis for opioids at the individual level or specific prescriptions for those in the hospital. We have seen that the nature of opioid misuse in some locations has progressed from prescription drugs to heroin, and currently to fentanyl (Gladden et al., 2016; Peterson et al., 2016). Patients who have legitimate needs for opioids may be those who substitute marijuana for opioids. Others, who are using marijuana recreationally, may be engaging in polydrug use at higher rates, resulting in higher rates of OUDs and poisonings. Our study looks at hospitalizations due to opioid poisonings, rather than mortality data. Opioid overdose deaths may have a different spatial signature than those found here, limiting the generalizability of our poisoning results.
Other factors, not measured here, may also be important in elucidating this relationship, such as access to other services or rates of homelessness in the area. We are unable to determine the underlying mechanisms that result in the findings we see here. The intriguing findings related to local versus spatially lagged dispensaries and opioid misuse suggest that the relationship is likely to be complex. By studying who uses dispensaries, how they use them, and other drugs being concurrently used, we can identify underlying mechanisms that might result in the spatial relationships observed here.
Conclusions
Although state-level studies suggest that more liberal marijuana policies may result in fewer opioid overdose deaths, our results within one state suggest that local availability of marijuana may not reduce those deaths. In this study, the relationship appears to be more complex, possibly based on socioeconomic conditions within and adjacent to areas with higher densities of medical marijuana dispensaries. Our results should be interpreted cautiously as we are not able to assess the individual-level mechanisms that may result in the findings presented here or how this might change as states exert greater control of licensing restrictions. Thus, more work that assesses how local availability of marijuana may affect opioid misuse and overdose is warranted.
Footnotes
This project was supported by National Institute on Alcohol Abuse and Alcoholism Grant No.P60-AA-006282 and National Institute on Drug Abuse Grant No. R01-DA-032715, and by the Clinical and Translational Science Institute (CTSI) at the University of Pittsburgh Virginia Kaufman Endowment Fund. The content is solely the responsibility of the authors and does not necessarily represent the National Institutes of Health.
Dispensaries across the state were loosely regulated during this period, which could result in dispensaries operating in disadvantaged areas where they may face less scrutiny from law enforcement. However, Thomas and Freisthler (2016, 2017) showed that in Los Angeles, the city with the largest number of dispensaries, areas with a greater percentage of commercially zoned, areas with highway ramp access, greater density of on- and off-premise alcohol outlets, and higher percentage of Hispanic residents were more likely to have higher densities (2016) and moved to areas with higher proportion of African American residents and lower percentage of area zoned for commercial use (2017). Neither study found a relationship between disadvantage and density of dispensaries.
References
- Aggarwal S. K., Carter G. T., Sullivan M. D., ZumBrunnen C., Morrill R., Mayer J. D. Characteristics of patients with chronic pain accessing treatment with medical cannabis in Washington State. Journal of Opioid Management. 2009;5:257–286. doi: 10.5055/jom.2009.0028. doi:10.5055/jom.2009.0028. [DOI] [PubMed] [Google Scholar]
- Bachhuber M. A., Saloner B., Cunningham C. O., Barry C. L. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Internal Medicine. 2014;174:1668–1673. doi: 10.1001/jamainternmed.2014.4005. doi:10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besag J., York J., Mollie A. Bayesian image restoration, with two applications in spatial statistics. Annals of the Institute of Statistical Mathematics. 1991;43:1–20. doi:10.1007/BF00116466. [Google Scholar]
- Bonn-Miller M. O., Boden M. T., Bucossi M. M., Babson K. A. Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. American Journal of Drug and Alcohol Abuse. 2014;40:23–30. doi: 10.3109/00952990.2013.821477. doi:10.3109/00952990.2013.821477. [DOI] [PubMed] [Google Scholar]
- Bradford A. C., Bradford W. D., Abraham A., Bagwell Adams G. Association between US state medical cannabis laws and opioid prescribing in the Medicare Part D population. JAMA Internal Medicine. 2018;178:667–672. doi: 10.1001/jamainternmed.2018.0266. doi:10.1001/jamainternmed.2018.0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell G., Hall W. D., Peacock A., Lintzeris N., Bruno R., Larance B., Degenhardt L.2018Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: Findings from a 4-year prospective cohort study The Lancet Public Health 3e341–e350.. doi:10.1016/S2468-2667(18)30110-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caputi T. L. Medical marijuana, not miracle marijuana: Some wellpublicized studies about medical marijuana do not pass a reality check. Addiction. 2019;114:1128–1129. doi: 10.1111/add.14580. doi:10.1111/add.14580. [DOI] [PubMed] [Google Scholar]
- Caputi T. L., Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. Journal of Addiction Medicine. 2018;12:295–299. doi: 10.1097/ADM.0000000000000405. doi:10.1097/ADM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- Caputi T. L., Sabet K. A. Population-level analyses cannot tell us anything about individual-level marijuana-opioid substitution. American Journal of Public Health. 2018;108:e12. doi: 10.2105/AJPH.2017.304253. doi:10.2105/AJPH.2017.304253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Vital Statistics System, Mortality. CDC WONDER. Atlanta, GA: Author; 2018. Retrieved from https://wonder.cdc.gov. [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2019. Retrieved from www.cdc.gov/injury/wisqars. [Google Scholar]
- Cerdá M., Gaidus A., Keyes K. M., Ponicki W., Martins S., Galea S., Gruenewald P. Prescription opioid poisoning across urban and rural areas: Identifying vulnerable groups and geographic areas. Addiction. 2017;112:103–112. doi: 10.1111/add.13543. doi:10.1111/add.13543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collen M. Prescribing cannabis for harm reduction. Harm Reduction Journal. 2012;9:1, 5. doi: 10.1186/1477-7517-9-1. doi:10.1186/1477-7517-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corroon J. M. J., Jr., Mischley L. K., Sexton M. Cannabis as a substitute for prescription drugs - a cross-sectional study. Journal of Pain Research. 2017;10:989–998. doi: 10.2147/JPR.S134330. doi:10.2147/JPR.S134330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D., Arias E., Kochanek K., Anderson R., Guy G. P., Jr., Losby J. L., Baldwin G. Contribution of opioid-involved poisoning to the change in life expectancy in the United States, 2000-2015. JAMA. 2017;318:1065–1067. doi: 10.1001/jama.2017.9308. doi:10.1001/jama.2017.9308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold D., Goor-Aryeh I., Bril S., Delayahu Y., Lev-Ran S. Problematic use of prescription opioids and medicinal cannabis among patients suffering from chronic pain. Pain Medicine. 2017;18:294–306. doi: 10.1093/pm/pnw134. [DOI] [PubMed] [Google Scholar]
- Gelfand A. E., Diggle D. J., Fuentes M., Guttorp P. Handbook of spatial statistics. Boca Raton, FL: Chapman & Hall/CRC Press; 2010. [Google Scholar]
- GeoLytics. GeoLytics estimates premium [DVD] (geolytics.com) Branchburg; NJ: 2016. [Google Scholar]
- Gladden R. M., Martinez P., Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-Involved overdose deaths – 27 states, 2013-2014. Morbidity and Mortality Weekly Report. 2016;65:837–843. doi: 10.15585/mmwr.mm6533a2. doi:10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- Guy G. P., Jr., Zhang K., Bohm M. K., Losby J., Lewis B., Young R., Dowell D. Vital signs: Changes in opioid prescribing in the United States, 2006–2015. Morbidity and Mortality Weekly Report. 2017;66:697–704. doi: 10.15585/mmwr.mm6626a4. doi:10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haroutounian S., Ratz Y., Ginosar Y., Furmanov K., Saifi F., Meidan R., Davidson E. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: A prospective open-label study. Clinical Journal of Pain. 2016;32:1036–1043. doi: 10.1097/AJP.0000000000000364. doi:10.1097/AJP.0000000000000364. [DOI] [PubMed] [Google Scholar]
- Hill K. P., Palastro M. D., Johnson B., Ditre J. W. Cannabis and pain: A clinical review. Cannabis and Cannabinoid Research. 2017;2:96–104. doi: 10.1089/can.2017.0017. doi:10.1089/can.2017.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hume B., Gabella B., Hathaway J., Proescholdbell S., Sneddon C., Brutsch E., Drucker C. J. Assessment of selected overdose poisoning indicators in health care administrative data in 4 states, 2012. Public Health Reports. 2017;132:488–495. doi: 10.1177/0033354917718061. doi:10.1177/0033354917718061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen M. A., Bohnert K., Kleinberg F., Jannausch M., Bohnert A. S. B., Walton M., Blow F. C. Characteristics of adults seeking medical marijuana certification. Drug and Alcohol Dependence. 2013;132:654–659. doi: 10.1016/j.drugalcdep.2013.04.019. doi:10.1016/j.drugalcdep.2013.04.019. [DOI] [PubMed] [Google Scholar]
- Kral A. H., Wenger L., Novak S. P., Chu D., Corsi K. F., Coffa D., Bluthenthal R. N. Is cannabis use associated with less opioid use among people who inject drugs? Drug and Alcohol Dependence. 2015;153:236–241. doi: 10.1016/j.drugalcdep.2015.05.014. doi:10.1016/j.drugalcdep.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston M. D., Barnett T. E., Delcher C., Wagenaar A. C. Recreational cannabis legalization and opioid-related deaths in Colorado, 2000-2015. American Journal of Public Health. 2017;107:1827–1829. doi: 10.2105/AJPH.2017.304059. doi:10.2105/AJPH.2017.304059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C., Gruenewald P. J., Ponicki W. R., Remer L. Varying impacts of alcohol outlet densities on violent assaults: Explaining differences across neighborhoods. Journal of Studies on Alcohol and Drugs. 2013;74:50–58. doi: 10.15288/jsad.2013.74.50. doi:10.15288/jsad.2013.74.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C., Sumetsky N., Burke J. G., Gaidus A. Investigating the social ecological contexts of opioid use disorder and poisoning hospitalizations in Pennsylvania. Journal of Studies on Alcohol and Drugs. 2018;79:899–908. doi: 10.15288/jsad.2018.79.899. doi:10.15288/jsad.2018.79.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore B. J., Barrett M. L. Case study: Exploring how opioid-related diagnosis codes translate from ICD-9-CM to ICD-10-CM. U.S. Agency for Healthcare Research and Quality; 2017. Retrieved from https://www.hcup-us.ahrq.gov/datainnovations/ICD-10CaseStudyonOpioid-RelatedIPStays042417.pdf. [Google Scholar]
- Narayan K. M. V., Patel S. A., Cunningham S. A., Curran J. Ominous reversal of health gains in the United States: Time to rethink research priorities? Annals of Internal Medicine. 2019;170:330–331. doi: 10.7326/M18-3653. doi:10.7326/M18-3653. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences. The health effects of cannabis and cannabinoids: Current state of evidence and recommendations for research. Washington, DC: The National Academies Press; 2017. Engineering, and Medicine. [PubMed] [Google Scholar]
- Nunberg H., Kilmer B., Pacula R. L., Burgdorf J. R. An analysis of applicants presenting to a medical marijuana specialty practice in California. Journal of Drug Policy Analysis. 2011;4 doi: 10.2202/1941-2851.1017. Article 1. doi:10.2202/1941-2851.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum A. M., Boyer J. A., Kondrad E. C. “But my doctor recommended pot”: Medical marijuana and the patient-physician relationship. Journal of General Internal Medicine. 2011;26:1364–1367. doi: 10.1007/s11606-011-1840-4. doi:10.1007/s11606-011-1840-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum A. M., Thurstone C., McGarry L., Walker B., Sabel A. L. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. American Journal of Drug and Alcohol Abuse. 2015;41:166–172. doi: 10.3109/00952990.2014.949727. doi:10.3109/00952990.2014.949727. [DOI] [PubMed] [Google Scholar]
- Olfson M., Wall M. M., Liu S. M., Blanco C. Cannabis use and risk of prescription opioid use disorder in the United States. American Journal of Psychiatry. 2018;175:47–53. doi: 10.1176/appi.ajp.2017.17040413. doi:10.1176/appi.ajp.2017.17040413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen E. R., Zander-Cotugno M., Shih R. A., Tucker J. S., Dunbar M. S., D’Amico E. J. Online methods for locating medical marijuana dispensaries: Practical considerations for future research. Cannabis. 2018;1:22–35. doi: 10.26828/cannabis.2018.02.003. doi:10.26828/cannabis.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson A. B., Gladden R. M., Delcher C., Spies E., Garcia-Williams A., Wang Y., Goldberger B. A. Increases in fentanyl-related overdose deaths – Florida and Ohio. Morbidity and Mortality Weekly Report. 2016;2013-2015;65:844–849. doi: 10.15585/mmwr.mm6533a3. doi:10.15585/mmwr.mm6533a3. [DOI] [PubMed] [Google Scholar]
- Powell D., Pacula R. L., Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? Journal of Health Economics. 2018;58:29–42. doi: 10.1016/j.jhealeco.2017.12.007. doi:10.1016/j.jhealeco.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman A., Welty M., Solomon P. Cannabis as a substitute for opioid-based pain medication: Patient self-report. Cannabis and Cannabinoid Research. 2017;2:160–166. doi: 10.1089/can.2017.0012. doi:10.1089/can.2017.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinarman C., Nunberg H., Lanthier F., Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. Journal of Psychoactive Drugs. 2011;43:128–135. doi: 10.1080/02791072.2011.587700. doi:10.1080/02791072.2011.587700. [DOI] [PubMed] [Google Scholar]
- Rue H., Martino S., Chopin N. Approximate Bayesian inference for latent Gaussian models using integrated nested Laplace approximations. Journal of the Royal Statistical Society. Series B, Methodological. 2009;71:319–392. doi:10.1111/j.1467-9868.2008.00700.x. [Google Scholar]
- Shover C. L., Davis C. S., Gordon S. C., Humphreys K. Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proceedings of the National Academy of Sciences of the United States of America. 2019;116:12624–12626. doi: 10.1073/pnas.1903434116. doi:10.1073/pnas.1903434116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell T., Gruenewald P. J. Controls on the physical availability of alcohol. In: Heather N., Stockwell T., editors. The essential handbook of treatment and prevention of alcohol problems. Chichester, England: John Wiley & Sons; 2004. pp. 213–234. [Google Scholar]
- Thomas C., Freisthler B. Examining the locations of medical marijuana dispensaries in Los Angeles. Drug and Alcohol Review. 2016;35:334–337. doi: 10.1111/dar.12325. doi:10.1111/dar.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas C., Freisthler B. Evaluating the change in medical marijuana dispensary locations in Los Angeles following the passage of local legislation. Journal of Primary Prevention. 2017;38:265–277. doi: 10.1007/s10935-017-0473-8. doi:10.1007/s10935-017-0473-8. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. ZIP code business patterns. Washington, DC: Department of Commerce; 2016. [Google Scholar]
- Vyas M. B., LeBaron V. T., Gilson A. M. The use of cannabis in response to the opioid crisis: A review of the literature. Nursing Outlook. 2018;66:56–65. doi: 10.1016/j.outlook.2017.08.012. doi:10.1016/j.outlook.2017.08.012. [DOI] [PubMed] [Google Scholar]
- Walsh Z., Callaway R., Belle-Isle L., Capler R., Kay R., Lucas P., Holtzman S. Cannabis for therapeutic purposes: Patient characteristics, access, and reasons for use. International Journal on Drug Policy. 2013;24:511–516. doi: 10.1016/j.drugpo.2013.08.010. doi:10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Wen H., Hockenberry J. M. Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Internal Medicine. 2018;178:673–679. doi: 10.1001/jamainternmed.2018.1007. doi:10.1001/jamainternmed.2018.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright E. R., Kooreman H. E., Greene M. S., Chambers R. A., Banerjee A., Wilson J. The iatrogenic epidemic of prescription drug abuse: County-level determinants of opioid availability and abuse. Drug and Alcohol Dependence. 2014;138:209–215. doi: 10.1016/j.drugalcdep.2014.03.002. doi:10.1016/j.drugalcdep.2014.03.002. [DOI] [PubMed] [Google Scholar]