The novel coronavirus (SARS-CoV-2) pandemic has raised difficult questions about how we will allocate hospital resources as the volume of severely ill patients threatens to exceed conventional capacity [1,2]. As emergency physicians, we are skilled at performing intubations and other critical life-saving procedures when patients arrive to us in extremis. However, palliative care is not as readily available in most emergency departments [3,4].
As of 2019, only 161 emergency physicians have obtained palliative care certification through ABEM [5]. During this ongoing pandemic, many agree that this is an important time to bridge the gap between the specialties of emergency medicine and palliative care [1]. Patients who are older than 65 years old and those with pre-existing chronic disease have demonstrated a higher risk of mortality due to COVID-19—the same patients who may wish to forgo prolonged life support and similar interventions at the end of life [1,6]. By developing tools to seamlessly integrate palliative care into emergency medicine practice, we can better deliver care that is compassionate, rational, and well-aligned with patients' values and goals [2,7].
We describe the experience of Partners' HealthCare, a tertiary healthcare system in Boston, and its innovative approach to creating an online, centralized compendium of reference materials for clinicians caring for patients who may not be expected to survive COVID-19 infection. PalliCOVID (https://pallicovid.app) is a web application that was developed by these authors for the rapid dissemination of hospital-specific clinical guidelines that are succinct and specific to the end stages of the COVID-19 disease process. These guidelines take into account the realities of our current practice environment, with its enhanced infection control measures and restricted visitor policies, that make end-of-life care in the emergency department especially challenging.
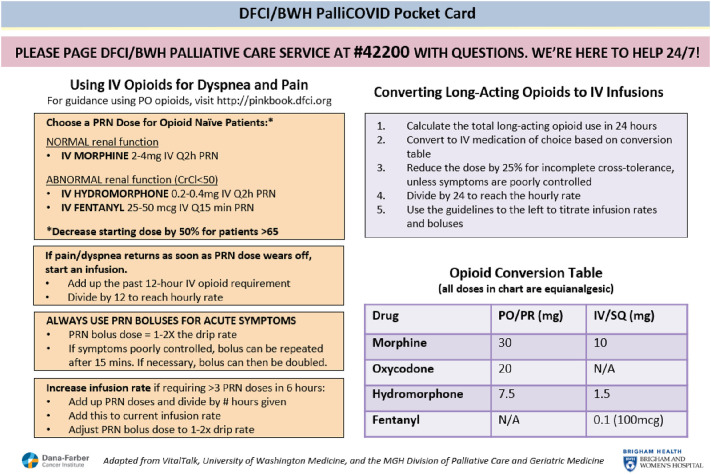
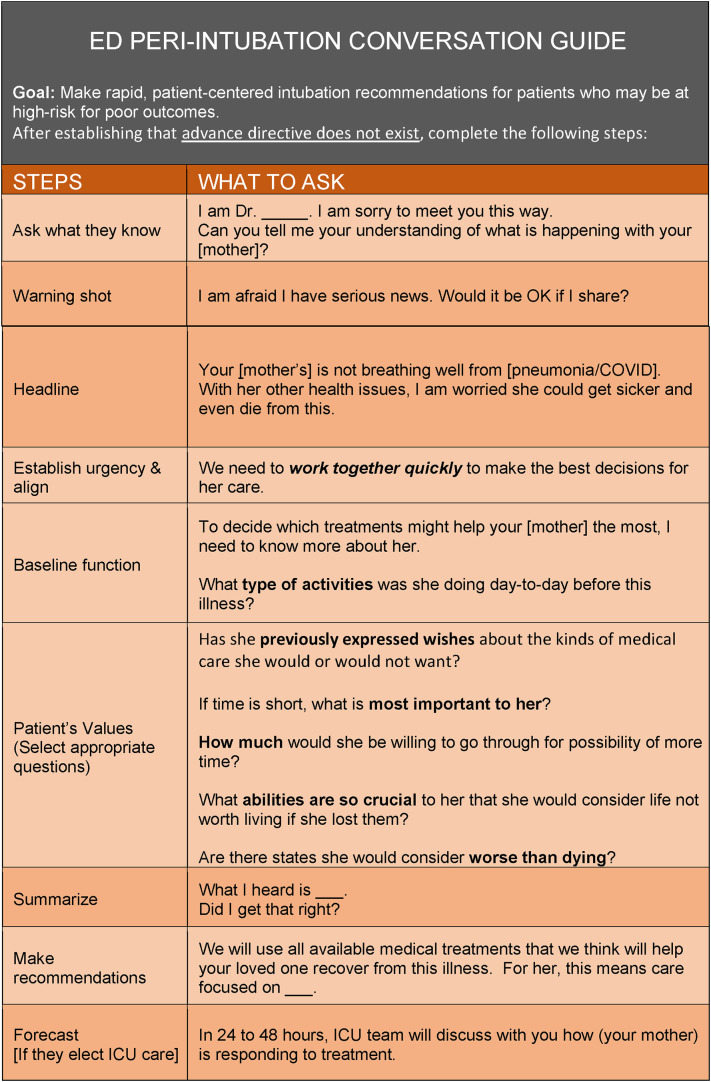
PalliCOVID is a mobile-responsive website that can be viewed from both mobile devices and desktop computers, making it easy to access evidence-based content such as opioid dosing recommendations for the treatment of dyspnea and pain at the end of life (Fig. 1 ) and a conversation guide for rapid code status determination in the peri-intubation setting (Fig. 2 ). Importantly, the content has been carefully reviewed by palliative care experts at Partners' prior to publication and is frequently updated to represent the best available evidence. We have made the majority of the content on PalliCOVID publicly accessible in order to lower the barriers to sharing best practices with other clinicians caring for seriously ill COVID-19 patients. Some specialized features of the application, such as one-click access to the hospital paging system, however, are limited in access to users within the Partners HealthCare System. By linking to the hospital's paging system, PalliCOVID allows clinicians to use their mobile devices to send stat consult requests to the palliative care service without having to leave the patient's bedside.
Fig. 1.
Opioids for Treatment of Dyspnea and Pain Pocket Card.
Fig. 2.
Rapid Code Status Determination Conversation Guide for Use in Peri-Intubation Situations in the Emergency Department.
By using digital health innovation to incorporate palliative care practices into our workflows, emergency physicians will be empowered to provide high-quality, goal-concordant care to critically ill patients, with a focus on dignity, symptom management, and avoidance of invasive or potentially harmful interventions [8].
This pandemic has shown us that, despite our best efforts, we will not be able to save the life of every patient infected with COVID-19. By working closely with our palliative care colleagues to develop innovative solutions like PalliCOVID, we can support emergency physicians doing their best to provide ethical, humanistic care on the front lines.
Author contributions
This manuscript was written primarily by LL, with significant editorial contributions from KO. The digital health application described, PalliCOVID.app, was originally developed by HMZ, RS, and ABL and is now being maintained by LL, RS, and HMZ.
This paper should be published in American Journal of Emergency Medicine because it is highly relevant to the current pandemic environment and addresses key challenges related to end of life care for COVID patients. This paper shares insights as to what technological innovations other healthcare organizations can adopt in order to better integrate palliative care services into the emergency department workflow.
We verify that this submission has not been previously published and, if accepted here, will not be published elsewhere.
Conflict of Interest Disclosure
LL, RS, KO, ABL, and HMZ report no conflict of interest.
Funding and support
This work did not receive any specific grant from funding agencies in the public, commercials, or not-for-profit sectors.
Prior presentations
N/A.
References
- 1.Curtis J.R., Kross E.K., Stapleton R.D. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19) JAMA. 2020;27 doi: 10.1001/jama.2020.4894. Published online March. [DOI] [PubMed] [Google Scholar]
- 2.Fausto J., Hirano L., Lam D., et al. Creating a palliative care inpatient response plan for COVID19 - the UW medicine experience. J Pain Symptom Manage. 2020;30 doi: 10.1016/j.jpainsymman.2020.03.025. Published online March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamba S., Nagurka R., Zielinski A., Scott S.R. Palliative care provision in the emergency department: barriers reported by emergency physicians. J Palliat Med. 2013;16(2):143–147. doi: 10.1089/jpm.2012.0402. [DOI] [PubMed] [Google Scholar]
- 4.Stone S.C., Mohanty S., Grudzen C.R., et al. Emergency medicine Physicians’ perspectives of providing palliative Care in an Emergency Department. J Palliat Med. 2011;14(12):1333–1338. doi: 10.1089/jpm.2011.0106. [DOI] [PubMed] [Google Scholar]
- 5.American Board of Emergency Medicine 2018–2019 Annual Report. 2019. https://www.abem.org/public/docs/default-source/publications/2018-2019-annual-report.pdf?sfvrsn=dc52cff4_8 Accessed May 20, 2020.
- 6.Du R.-H., Liang L.-R., Yang C.-Q., et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Powell V.D., Silveira M.J. What should palliative Care’s response be to the COVID-19 epidemic? J Pain Symptom Manage. 2020;27 doi: 10.1016/j.jpainsymman.2020.03.013. Published online March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferguson L., Barham D. Palliative care pandemic pack: a specialist palliative care service response to planning the COVID-19 pandemic. J Pain Symptom Manage. 2020;1 doi: 10.1016/j.jpainsymman.2020.03.026. Published online April. [DOI] [PMC free article] [PubMed] [Google Scholar]