Abstract
This case describes the successful pulmonary rehabilitation of a premorbidly independent female in the early 80s who was admitted for acute respiratory distress syndrome secondary to COVID-19 requiring 14 days of intubation. Patient was admitted to the acute rehabilitation unit 1 month after hospitalisation. Patient initially had poor endurance and was only able to ambulate with a front wheel walker for 150 feet, and also had tachycardia and decreased oxygen saturation after ambulation. During patient’s rehabilitation course, therapy was focused on improving activity tolerance. Ten days after admission, patient was able to ambulate without an assistive device for 250 feet and with a rollator for over 900 feet. Patient also showed improvement in gait speed, heart rate, oxygen saturation after ambulation and incentive spirometer volume. This case demonstrates that pulmonary rehabilitation is an important component of inpatient care for patients with COVID-19 to improve functional exercise capacity and aerobic capacity.
Keywords: pneumonia (respiratory medicine), physiotherapy (rehabilitation), rehabilitation medicine, geriatric medicine
Background
The spread of the COVID-19 has brought about global pandemic resulting in unprecedented times for the medical and rehabilitation communities. According to the Centers of Disease Control and Prevention, older adults are at higher risk, where 8 out of 10 reported deaths in the USA have been in adults 65 years and older.1 Additionally, of adults with confirmed COVID-19 reported in the USA, 31%–70% of patients 65 years and older are hospitalised, 6%–31% are admitted to the intensive care unit and 4%–27% pass away.1 Unfortunately, patients who return home after prolonged hospitalisation are at high risk of several adverse health effects from decreased respiratory movement, muscle weakness, skin breakdown and decreased rate of metabolism.2 An observational, prospective, quasi-experimental study of 72 patients in Hainan General Hospital, China demonstrated that a 6-week respiratory rehabilitation course led to significant differences in pulmonary function tests and 6 min Walk Test (6MWT) and improved respiratory function, quality of life and anxiety in elderly patients with COVID-19.3 Therefore, given the severity of dysfunction seen in these patients with COVID-19, rehabilitation is essential and needed to optimise physical and cognitive functioning to reduce the risk of disability and morbidity.2
Case presentation
A premorbidly independent female in the early 80s with medical history of diabetes mellitus type II, hypertension and obesity presented to the emergency room after 8 days of fever, chills, cough and lethargy and positive outpatient COVID-19 test. Patient was admitted for hypoxic respiratory failure and pneumonia complicated by acute respiratory distress syndrome (ARDS) secondary to COVID-19 (figure 1). She required intubation for 14 days in the intensive care unit (ICU). During her stay, her arterial blood gas analysis showed mixed respiratory acidosis with metabolic alkalosis and her PaO2/FiO2 ratio of 35.5 mm Hg/0.4 was 89 mm Hg, suggesting severe, 45% mortality.4 Her qSOFA (quick Sequential Organ Failure Assessment) score was 2 for tachypnoea and hypotension, suggesting high risk for in-hospital mortality,5 though her full SOFA score was 6 for PaO2/FiO2 ratio of 89 mm Hg, platelets 100–149, Mean Arterial Pressure (MAP) <70 mm Hg and being on mechanical ventilation, suggesting <33% mortality.6
Figure 1.
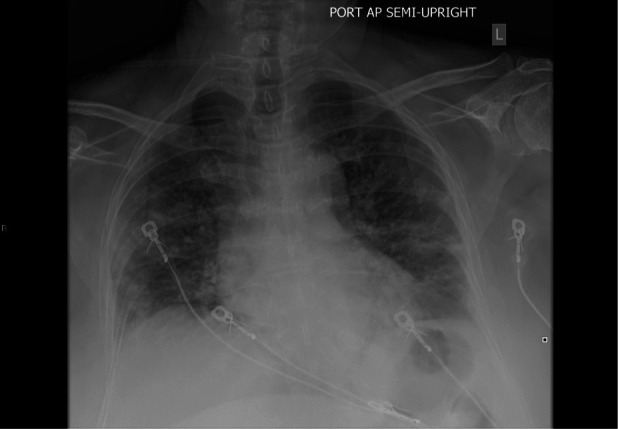
Chest X-ray demonstrating multifocal bilateral heterogeneous consolidation in peripheral mid through lower lungs, compatible with history of COVID-19 pneumonia.
Additionally, although patient has no history of any prior cardiac issues and thus no echocardiogram on file, she did have a troponemia to 0.629 during her admission. Her ECG showed sinus tachycardia without stigmata of acute coronary syndrome and the troponin eventually downtrended to 0.115. Therefore, her troponemia was concluded to be non-ST segment elevation myocardial infarction type 2.
After extubation, patient was downgraded to the telemetry floor for 14 more days. Patient slowly recovered after treatment with multiple medications, including hydroxychloroquine, azithromycin, ceftriaxone, vancomycin, cefepime, doxycycline and tocilizumab. One month after admission, patient was transferred to the Acute Rehabilitation Unit (ARU) after three negative COVID-19 tests while inpatient with goal of returning home with family.
Prior to admission to the ARU, patient’s Functional Independence Measure (FIM) scores were 5 out of 7 for bed mobility, transfers and ambulation with front wheel walker (FWW) to 150 feet which was limited by endurance. Patient was also noted to have a heart rate to the 130s and oxygen saturation of 88% after ambulation.
Treatment
During patient’s rehabilitation course, therapy was focused on improving activity tolerance and endurance. Patient’s functional outcome was measured with multiple assessments: The Chair Stand Test (30 s) measures the number of times a patient can stand up repeatedly from a chair in 30 s, the Timed Up & Go (TUG) test measures the time it takes for a patient to stand from a chair and walk 3 m away and back to sit down, and the 6MWT measures the distance an individual is able to walk over 6 min. These measures were recorded on days 1, 5 and 10 during her rehabilitation stay. Cardiopulmonary Exercise (CPX) testing was also considered for the patient to further evaluate her status, however the hospital’s CPX lab was unfortunately closed during that time due to COVID-19.
Outcome and follow-up
Table 1 lists patient’s scores for her functional outcome measures. For the Chair Stand Test, patient initially was only able to stand up eight times with hands pushing up from armrest in 30 s, however on day 10 she was able to stand up 11 times. Similarly, in her TUG test with FWW, she initially required 35.30 s to stand and walk 3 m and back, however on day 5 her time improved to 28.15 s. Her TUG test without assistive device also showed significant change, improving from 17.20 s on admission to only 10.16 s on day 10, which suggests that patient is no longer classified as high risk of falling in the community (>13.5 s).7 Lastly, patient’s 6MWT reflected her increase in endurance. Initially, patient only tolerated 150 feet with FWW, however on day 10 she was able to ambulate 967.4 feet with a rollator. Her gait speed, heart rate, oxygen saturation after ambulation and incentive spirometer volume showed similar improvements.
Table 1.
Functional outcome measures during rehabilitation stay
| Chair Stand Test | TUG test with FWW | TUG test without assistive device | Gait speed (15 feet) | 6MWT | Heart rate after ambulation | Oxygen saturation after ambulation (%) | Incentive spirometer volume (cc) | |
| Day 1 | Eight with hands pushing up from armrests | 35.30 s | 17.20 s | 0.44 m/s with FWW | 150 feet with FWW | 130 | 88 | 250–500 |
| Day 5 | Six with hands pushing up from armrests | 28.15 s | 12.50 s | 0.62 m/s with FWW | 722.4 feet with rollator | 105 | 94 | 500–750 |
| Day 10 | Eleven with hands pushing up from armrests | Not tested | 10.16 s | 1.04 m/s with rollator | 967.4 feet with rollator | 99 | 98 | 1000–1250 |
FWW, front wheel walker; 6MWT, 6 min Walk Test; TUG, Timed Up & Go.
On day 11, patient was discharged home with family. She was prescribed a rollator as well as home and outpatient cardiopulmonary therapy for continued rehabilitation and to obtain CPX testing once the lab reopens. Her FIM scores on discharge were 7 for mobility, 6 for transfers, 7 for ambulation without assistive device at 250 feet and 6 for ambulation with rollator at over 900 feet.
Discussion
This was the hospital’s first case of successful pulmonary postacute inpatient rehabilitation in an elderly female patient after ARDS secondary to COVID-19 and intubation. Activity tolerance and endurance training were the most important factors for patient recovery given their association with pulmonary distress commonly seen in COVID-19 infections.8 The media focuses heavily on the disease process during its acute phase while patient is in the ICU or medical ward. However, this case report highlights that intensive pulmonary rehabilitation is also an important component of inpatient care for patients with COVID-19 in the postacute setting for maximal functional recovery in both exercise capacity and aerobic capacity.
Patient’s perspective.
My children are still worried about me, but I feel that I will get stronger and stronger. I mentally tell myself ‘I don’t have time for this’ and I think that’s how I got through [this experience]. I really feel extremely blessed and extremely lucky.
Learning points.
Pulmonary rehabilitation is an important component of inpatient rehabilitation for patients with COVID-19 to improve functional exercise capacity, aerobic capacity and quality of life.
Patients would benefit from incorporation of pulmonary rehabilitation along with the interdisciplinary treatments while in the acute inpatient rehabilitation setting.
Activity tolerance and endurance can be measured with the Chair Stand Test, the Timed Up & Go Test, and the 6 min Walk Test.
Acknowledgments
We would like to acknowledge Eric Harden and Patricia Heck for their contributions to this patient’s rehabilitation care.
Footnotes
Contributors: MXS was involved with informed consent, literature review, manuscript write-up and patient management. YMT was involved in treatment as a therapist. KTV was involved with case identification and managed the patient as an attending. BCE was involved with literature review and review of manuscript as the senior author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Coronavirus disease 2019 (COVID-19). centers for disease control and prevention, 2020. Available: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html [Accessed 14 May 2020].
- 2.Prvu Bettger J, Thoumi A, Marquevich V, et al. . COVID-19: maintaining essential rehabilitation services across the care continuum. BMJ Glob Health 2020;5:e002670. 10.1136/bmjgh-2020-002670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu K, Zhang W, Yang Y, et al. . Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract 2020;39:101166. 10.1016/j.ctcp.2020.101166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horovitz JH, Carrico CJ, Shires GT. Pulmonary response to major injury. Arch Surg 1974;108:349–55. 10.1001/archsurg.1974.01350270079014 [DOI] [PubMed] [Google Scholar]
- 5.Seymour CW, Liu VX, Iwashyna TJ, et al. . Assessment of clinical criteria for sepsis: for the third International consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:762–74. 10.1001/jama.2016.0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent JL, Moreno R, Takala J, et al. . The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. on behalf of the Working group on sepsis-related problems of the European Society of intensive care medicine. Intensive Care Med 1996;22:707–10. 10.1007/BF01709751 [DOI] [PubMed] [Google Scholar]
- 7.Barry E, Galvin R, Keogh C, et al. . Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr 2014;14:14. 10.1186/1471-2318-14-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D, Hu B, Hu C, et al. . Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]


