Abstract
Background:
The objective of this study is to investigate the effects of humanistic care and psychological counseling (HCPC) on psychological disorders (PD) in medical students after coronavirus disease 2019 (COVID-19) outbreak.
Methods:
We will search randomized controlled trials or case-controlled studies of HCPC on PD in medical students after COVID-19 outbreak in the following electronic databases: PUBMED/MEDLINE, EMBASE, Cochrane Library, CINAHL, AMED, WANGFANG, and CNKI. The time is restricted from the construction of each database to the present. All process of study selection, data collection, and study quality evaluation will be carried out by two independent authors. Any different opinions will be solved by a third author through discussion. We will employ RevMan 5.3 software to conduct statistical analysis.
Results:
This study will provide a better understanding of HCPC on PD in medical students after COVID-19 outbreak.
Conclusions:
This study may offer strong evidence for clinical practice to treat PD in medical students after COVID-19 outbreak.
Study registration:
CRD42020193199.
Keywords: COVID-19, humanistic care, psychological counseling, psychological disorders
1. Introduction
Coronavirus disease 2019 (COVID-19) is a new coronavirus that has never been found in humans before.[1–3] It can cause severe acute respiratory syndrome and spread rapidly worldwide.[4–8] It manifests as fever or chills, cough, shortness of breath, fatigue, muscle or body aches, sore throat, congestion or runny nose, and dyspnea.[9–11] If it cannot be treated fairly well, it can further develop to pneumonia, severe acute respiratory syndrome, kidney failure, and even death.[12–15] According to the report of World Health Organization, by June 24, there are more than 9.1 million cases of COVID-19 in total, and more than 470,000 deaths worldwide.[16]
Outbreak of COVID-19 is associated with considerable psychological disorders (PD), such as depression, anxiety, and fear in general public, specific communities, or medical students, especially when the infection rate and deaths are considerable.[17–23] After the period of COVID-19 outbreak, tackling PD of medical students is crucial. Studies suggested that humanistic care and psychological counseling (HCPC) can effectively treat PD in medical students after COVID-19 outbreak.[24–29] However, no systematic review has investigated this issue. Thus, this systematic review protocol will appraise the effects of HCPC on PD in medical students after COVID-19 outbreak.
2. Methods
2.1. Study registration
We registered this study protocol on CRD42020193199. We reported it based on the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols.[30]
2.2. Inclusion and exclusion criteria for study selection
2.2.1. Types of studies
We will include randomized controlled trials (RCTs) or case-controlled studies (CCSs) of HCPC on PD in medical students after COVID-19 outbreak. We will not consider other studies, such as animal study, review, editorial comment, case report, and case series.
2.2.2. Types of participants
The target population is medical students with confirmed PD after COVID-19 outbreak irrespective of ethnicity, sex, and severity of PD.
2.2.3. Types of interventions
The experimental interventions are any forms of HCPC combination.
Besides any types of HCPC, no limitations will be made on comparators.
2.2.4. Types of outcome measurements
The primary outcomes are depression and anxiety, as reported by any scales in the trial, such as Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale.
The secondary outcomes are mental disorder, panic disorder, health-related quality of life, and adverse events.
2.3. Search methods for study selection
2.3.1. Electronic databases
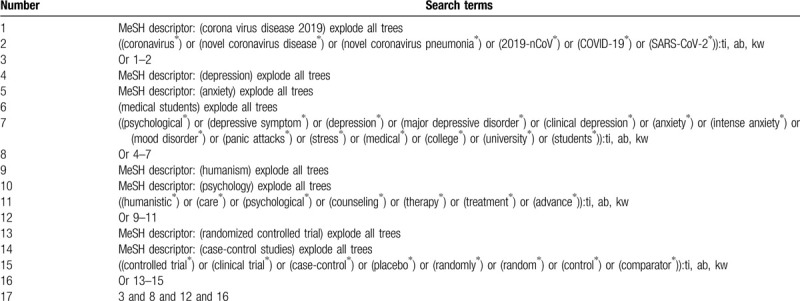
We will search the following electronic databases from the construction of each database to the present: PUBMED/MEDLINE, EMBASE, Cochrane Library, CINAHL, AMED, WANGFANG, and CNKI. We will build search strategy for Cochrane Library and will be presented in Table 1. Similar search strategy for other electronic databases will be adapted. As for Chinese databases, equivalent search words will be applied.
Table 1.
Details of search strategy of Cochrane Library.
2.3.2. Other resources
We will also check other resources, such as conference abstracts, dissertation/thesis, and reference lists of relevant review.
2.4. Study selection and data extraction
2.4.1. Study selection
Two authors will independently carry out study selection. Any disagreements will be solved by a third author through consultation. All searched records will be imported to the citation management software (EndNote 7.0), and all duplications will be eliminated. Then, titles and abstracts of all potential studies will be scanned to remove unrelated studies. After that, we will carefully check full-text of all potential articles according to the eligibility criteria. We will present the process of study selection in a flowchart.
2.4.2. Data extraction and management
Two authors will independently undertake data extraction using a standard data extraction sheet. Any confusion will be resolved by a third author through discussion. The extracted information includes general information (such as title, first author, and time of publication), study information (such as design, setting, methods, and sample size), patient information (such as ethnicity, age, sex, diagnostic criteria, and eligibility criteria), outcomes (such as primary and secondary outcomes, and follow-up data), and other information (such as funding and conflict of interest). If there is unclear or missing data, we will contact primary authors to obtain it by email or telephone or fax.
2.4.3. Risk of bias assessment
Two independent authors will carry out study quality assessment using Cochrane Risk of Bias Tool for RCTs, and Newcastle-Ottawa Quality Assessment for CCSs, respectively. Any discrepancies will be settled down by a third author through discussion or consultation.
2.5. Statistical analysis
2.5.1. Data synthesis
This study will utilize RevMan 5.3 software to perform statistical analysis. We will estimate treatment effect of dichotomous outcomes as risk ratio and 95% confidence intervals (CIs), and that of continuous outcomes as mean difference (MD) or standardized MD and 95% CIs. We will identify statistical heterogeneity using I2 test. I2 ≤50% means reasonable heterogeneity, and we will employ a fixed-effect model. If sufficient data are extracted from eligible trials, we will conduct meta-analysis based on similarity in study information, patient information, interventions, controls, and outcomes. I2 > 50% exerts considerable heterogeneity, and we will place a random-effect model. In addition, we will carry out a subgroup analysis to explore its sources. If the meta-analysis is not possible, we will perform a narrative synthesis of study findings.
2.5.2. Unit of analysis
We will only collect and analyze data from the first period of eligible study if cross-over study is included.
2.5.3. Subgroup analysis
We will preside over a subgroup analysis in accordance with different study information, subject characteristics, specifics of interventions and controls, and study quality.
2.5.4. Sensitivity analysis
We will undertake a sensitivity analysis to check the robustness of study findings by removing low quality studies.
2.5.5. Reporting bias
When more than 10 eligible studies on the same outcome are included, we will investigate reporting bias using Funnel plot and Egger's linear regression test.[31,32]
2.5.6. Overall quality of evidence
Two authors will independently appraise the overall quality of evidence for each outcome using the Grading of Recommendations Assessment, Development and Evaluation approach.[33] It will be further divided into five aspects of high, moderate, low or very low quality.[33]
2.6. Dissemination and ethics
We expect to publish this study on a peer-reviewed journal or a conference meeting. This study will not require ethic approval, because it will not collect individual patient data and privacy.
3. Discussion
The outbreak of COVID-19 pandemic creates challenges for clinicians and scientific researchers.[1,2] It also brings tremendous PD for general population, doctors, nurses and medical students.[17–23] Previous studies reported that HCPC can benefit PD in medical students after COVID-19 outbreak.[24–29] However, there is no systematic review focusing on this topic, and evidence-based medicine literature is very necessary to explore its effects. Thus, in this study, we will summarize recent associated studies to appraise the effects of HCPC on PD in medical students after COVID-19 outbreak. The findings of this study may yield helpful evidence for both clinicians and health-related policy makers.
Author contributions
Conceptualization: Hao Tian, Yu Xue, Rong-rong Yao, Da-yin Chen, Fan-bo Wang, Qing-hui Ji.
Data curation: Hao Tian, Rong-rong Yao, Yu Yan, Yong Xue, Da-yin Chen, Fan-bo Wang, Chun-feng Li.
Formal analysis: Hao Tian, Yu Xue, Yong Xue, Chun-feng Li.
Investigation: Qing-hui Ji.
Methodology: Hao Tian, Rong-rong Yao, Yong Xue, Da-yin Chen, Fan-bo Wang.
Project administration: Qing-hui Ji.
Resources: Hao Tian, Yu Xue, Rong-rong Yao, Yu Yan, Yong Xue, Da-yin Chen, Fan-bo Wang, Chun-feng Li.
Software: Hao Tian, Yu Xue, Rong-rong Yao, Yu Yan, Yong Xue, Da-yin Chen, Fan-bo Wang, Chun-feng Li.
Supervision: Qing-hui Ji.
Validation: Hao Tian, Yu Xue, Yu Yan, Yong Xue, Da-yin Chen, Fan-bo Wang, Chun-feng Li, Qing-hui Ji.
Visualization: Hao Tian, Rong-rong Yao, Yu Yan, Yong Xue, Qing-hui Ji.
Writing – original draft: Hao Tian, Yu Xue, Rong-rong Yao, Yu Yan, Yong Xue, Da-yin Chen, Fan-bo Wang, Chun-feng Li, Qing-hui Ji.
Writing – review & editing: Hao Tian, Yu Xue, Yong Xue, Fan-bo Wang, Chun-feng Li, Qing-hui Ji.
Footnotes
Abbreviations: CCSs = case-controlled studies, CIs = confidence intervals, COVID-19 = coronavirus disease 2019, HCPC = humanistic care and psychological counseling, MD = mean difference, PD = psychological disorders, RCTs = randomized controlled trials.
How to cite this article: Tian H, Xue Y, Yao Rr, Yan Y, Xue Y, Chen Dy, Wang Fb, Li Cf, Ji Qh. Humanistic care and psychological counseling on psychological disorders in medical students after COVID-19 outbreak: A protocol of systematic review. Medicine. 2020;99:33(e21484).
HT and YX contributed equally to this work.
This work was supported by the Heilongjiang Provincial Educational Science Planning Special Project (Special Project of “Research on Epidemic Prevention and Control Strategies and Education Reflection Under the Background of COVID-19 Outbreak”). The funder did not involve in any parts of this study.
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the present study.
References
- [1].Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Peak CM, Childs LM, Grad YH, et al. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proc Natl Acad Sci USA 2017;114:4023–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gao Q, Hu Y, Dai Z, et al. The epidemiological characteristics of 2019 novel coronavirus diseases (COVID-19) in Jingmen, Hubei, China. Medicine (Baltimore) 2020;99:e20605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ceylan Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci Total Environ 2020;729:138817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mohammadzadeh N, Shahriary M, Shirmohammadlou N, et al. A glance at the prevalence of coronavirus disease 19 (COVID-19) in Iran: strengths and weaknesses. Infect Control Hosp Epidemiol 2020;1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Muurlink OT, Taylor-Robinson AW. COVID-19: cultural predictors of gender differences in global prevalence patterns. Front Public Health 2020;8:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pizzichini MMM, Patino CM, Ferreira JC. Measures of frequency: calculating prevalence and incidence in the era of COVID-19. J Bras Pneumol 2020;46:e20200243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Baj J, Karakuła-Juchnowicz H, Teresiński G, et al. COVID-19: specific and non-specific clinical manifestations and symptoms: the current state of knowledge. J Clin Med 2020;9:E1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Özdağ Acarli AN, Samanci B, Ekizoğlu E, et al. Coronavirus disease 2019 (COVID-19) from the point of view of neurologists: observation of neurological findings and symptoms during the combat against a pandemic. Noro Psikiyatr Ars 2020;57:154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].González-Silva Y, Bahíllo Marcos E, Martín Gutiérrez R, et al. Clinical involvement and symptoms of patients older than 65 years with COVID-19. Aten Primaria 2020;S0212-6567(20)30101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Parohan M, Yaghoubi S, Seraji A. Cardiac injury is associated with severe outcome and death in patients with coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Eur Heart J Acute Cardiovasc Care 2020;2048872620937165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Piano S, Dalbeni A, Vettore E, et al. Abnormal liver function tests predict transfer to intensive care unit and death in COVID-19. Liver Int 2020;doi: 10.1111/liv.14565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Polonikov A. Endogenous deficiency of glutathione as the most likely cause of serious manifestations and death in COVID-19 patients. ACS Infect Dis 2020;doi: 10.1021/acsinfecdis.0c00288. [DOI] [PubMed] [Google Scholar]
- [15].Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ 2020;368:m1198. [DOI] [PubMed] [Google Scholar]
- [16].World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19-24; June 2020. Available at https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---24-june-2020 [accessed June 25, 2020]. [Google Scholar]
- [17].Qi R, Chen W, Liu S, et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv 2020;20031666. [Google Scholar]
- [18].Uvais NA. Mania precipitated by COVID-19 pandemic-related stress. Prim Care Companion CNS Disord 2020;22: doi: 10.4088/pcc.20l02641. [DOI] [PubMed] [Google Scholar]
- [19].Zhou Q, Hu Z, Bian G, et al. Mental health and psychosocial function of general population during the COVID-19 epidemic in China. Clin Transl Med 2020;doi: 10.1002/ctm2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Luo X, Estill J, Wang Q, et al. The psychological impact of quarantine on coronavirus disease 2019 (COVID-19). Psychiatry Res 2020;291:113193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Courtney D, Watson P, Battaglia M, et al. COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can J Psychiatry 2020;doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Serafini G, Parmigiani B, Amerio A, et al. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020;doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Renjun G, Ziyun L, Xiwu Y, et al. Psychological intervention on COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99: doi: 10.1097/md.0000000000020335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Zhang LL, Liu X, Guo SS, et al. Mental health status of medical students and non-medical students under the epidemic of new coronavirus pneumonia. Chin J Health Psychol 2020;1–7. [Google Scholar]
- [25].Wang KX, Xu DC, He WF, et al. Anxiety status and influencing factors of medical staff during the outbreak of new coronavirus pneumonia. Chin Hosp Manage 2020;40:29–32. [Google Scholar]
- [26].Han Y. Psychological intervention and counseling in the outbreak of new coronary pneumonia. J Party Govern Cadres 2020;5:75–80. [Google Scholar]
- [27].Wang ZH, Chen LL, Li L, et al. The effect of new coronavirus pneumonia on the mental health of medical students. J Changchun Univ Tradit Chin Med 2020;1–4. [Google Scholar]
- [28].Yu QX, Zeng YM, Lu WJ. Investigation and analysis of the mental health status of middle school students in the outbreak of new coronary pneumonia. Jiangsu Educ 2020;32:44–7. [Google Scholar]
- [29].Zhou X, Li E, Yu JJ, et al. The effect of psychological counseling on the emotional management of nurses in the isolation area of new coronavirus pneumonia. Nurs Rehabilit 2020;19:84–6. [Google Scholar]
- [30].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sutton AJ, Duval SJ, Tweedie RL, et al. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Higgins J, Green S. Collaboration C. Cochrane handbook for systematic reviews for interventions. Cochrane Database Syst Rev 2011;2011:S38. [Google Scholar]


