Abstract
Acute appendicitis (AA) is the most common nonobstetric surgical emergency during pregnancy. According to the current guidelines and meta-analyses, traditional open appendectomy (OA) is still recommended for pregnant patients over laparoscopic appendectomy (LA), which might be associated with higher rates of fetal loss. Previous studies and experiences indicated that LA might be safe in the second trimester of pregnancy. The current study aimed to evaluate the safety and feasibility of LA in pregnant women during the second trimester.
At our institution, a retrospective study was conducted with pregnant patients who underwent LA or OA during the second trimester between January 2016 and August 2018.
A total of 48 patients were enrolled. Of them, 12 were managed with laparoscopy and 36 with the open approach. We found that the LA group had higher BMIs than the OA group (4.0 ± 4.3 vs 21.5 ± 2.9, P = .031). The financial results showed that the average daily medical costs for patients who underwent LA was higher than those who underwent OA (444 ± 107 US$ vs 340 ± 115 US$, P = .009), while the total cost of hospitalization was comparable between the 2 approaches. The perioperative and obstetric outcomes were comparable between LA and OA. In each group, only 1 patient had fetal loss. No “Yinao” was found in any of the patients in the LA group.
In this study, with the proven advantages of the laparoscopic techniques, LA was found to be safe and feasible for pregnant women during the second trimester.
Keywords: appendectomy, laparoscopy, second trimester, Yinao
1. Introduction
Acute appendicitis (AA) is the most common nonobstetric surgical emergency during pregnancy, with an approximate incidence of one in every 500 to 2000 pregnancies.[1,2] The reported rate of appendiceal perforation during pregnancy can be as high as 43%, compared with 19% in the general population. In addition, complicated appendicitis can lead to very poor outcomes, such as fetal loss; thus, patients with AA during pregnancy should immediately undergo appendectomy, regardless of gestation of the fetus.[3] With the development of laparoscopic techniques, laparoscopic appendectomy (LA) has become the first choice for nonpregnant patients and has the advantages of less pain, shorter hospital stays and fewer wound infections than the open approach.[4] On the other hand, according to the current guidelines and a meta-analysis, traditional open appendectomy (OA) is still recommended for pregnant patients over LA, which might be associated with higher rates of fetal loss.[5–7] However, most of the included studies were small, and the selection bias was very high; therefore, whether LA should be chosen for pregnant patients is still under debate.
On the other hand, in some areas, Yinao (healthcare disturbance) is more likely to appear in pregnant women, such as those in China. To avoid Yinao, surgeons always choose the safest therapeutic approach for pregnant patients.[8] According to multiple scholars’ advice, Kirshtenin et al reported that LA is safest in the second trimester of pregnancy because the small size of the uterus makes it is less susceptible to traumatic injuries.[9] Cohen-Kerem et al reported that LA performed during the first trimester is usually associated with a greater risk for fetal loss because of teratogenicity of medications and reduced uterine blood flow due to the pneumoperitoneum.[10] Curet et al reported that the third trimester was previously regarded as a contraindication for LA because of the expected technical difficulties.[11] According to the medical environment in China, LA might be safe in the second trimester of pregnancy. Therefore, LA was performed in pregnant patients during the second trimester in our institution.
The current study retrospectively investigated the perioperative and obstetric outcomes between LA and OA and aimed to evaluate the safety and feasibility of LA in pregnant women during the second trimester.
2. Methods
2.1. Patients
All patients who were diagnosed with AA during pregnancy at our hospital (West China Hospital, Sichuan University, China) between January 2016 and August 2018 were initially screened. The inclusion criteria were pregnant women during the second trimester who underwent LA or OA with pathological reports that confirmed the diagnosis of AA. The exclusion criteria included the following:
-
1.
patients who intended to have an abortion after being discharged from the hospital;
-
2.
patients with incomplete or inaccurate obstetric outcomes;
-
3.
patients who underwent another abdominal operation before delivery; and
-
4.
patients with fetal loss during the hospital stay due to severe abdominal infection.
The clinical diagnosis of AA was obtained through the patients’ medical history, physical examination, laboratory results, and ultrasounds. The Alvarado score, which is one of the most common scoring systems used for AA, was evaluated in all patients.[12] An obstetrician routinely assessed the status of the mother and fetus before the operation and provided tocolytic treatment during the hospital stay. Regard to the surgical group, first of all, in our hospital every surgeon will explain the advantages and disadvantages of LA and OA to the patients. Then, the selection of LA or OA was decided by the surgeons based on the patient's condition and the skills of the surgeon. Finally, the patient's own choice will be given priority. Written informed consent was not required because of the anonymous nature of the data. This retrospective study was approved by the Ethical Committee of the West China Hospital.
2.2. Laparoscopic appendectomy technique
The patient was placed on the table in the supine position with her head tilted down by 20° and body tilted down by 30° to the left. Routinely, prophylactic antibiotics were provided intravenously for 30 minutes before the incision was made. LA was performed with the patient under general anesthesia, but no Foley catheter was inserted unless the operation time was over 2 hours. A conventional 3-port technique with a 30° angled camera was used in all patients. First, we used the Veress needle to establish a pneumoperitoneum and maintained the pressure at 12 mm Hg. Then, we inserted a 10 mm trocar supraumbilically, depending on the location of the uterus. The telescope was inserted through this route to initially evaluate the condition of the abdominal cavity. Then, another 10 mm trocar was inserted through the anti-McBurney point. At this time, the assistant changed the telescope route to the anti-McBurney point, and the chief surgeon used the first port to locate the appendix. Next, a 5 mm trocar was inserted at the location of the appendix, but sometimes we could not find the appendix using one hand; then, the 5 mm port was inserted at McBurney point. The locations of these 3 ports varied according to the gestation time (Fig. 1). The appendicular artery and stump were excised with Hemo locks, and the specimen was then placed in a Lap bag and removed through the umbilical port site. A drainage tube was placed on the left side of the stump if needed.
Figure 1.
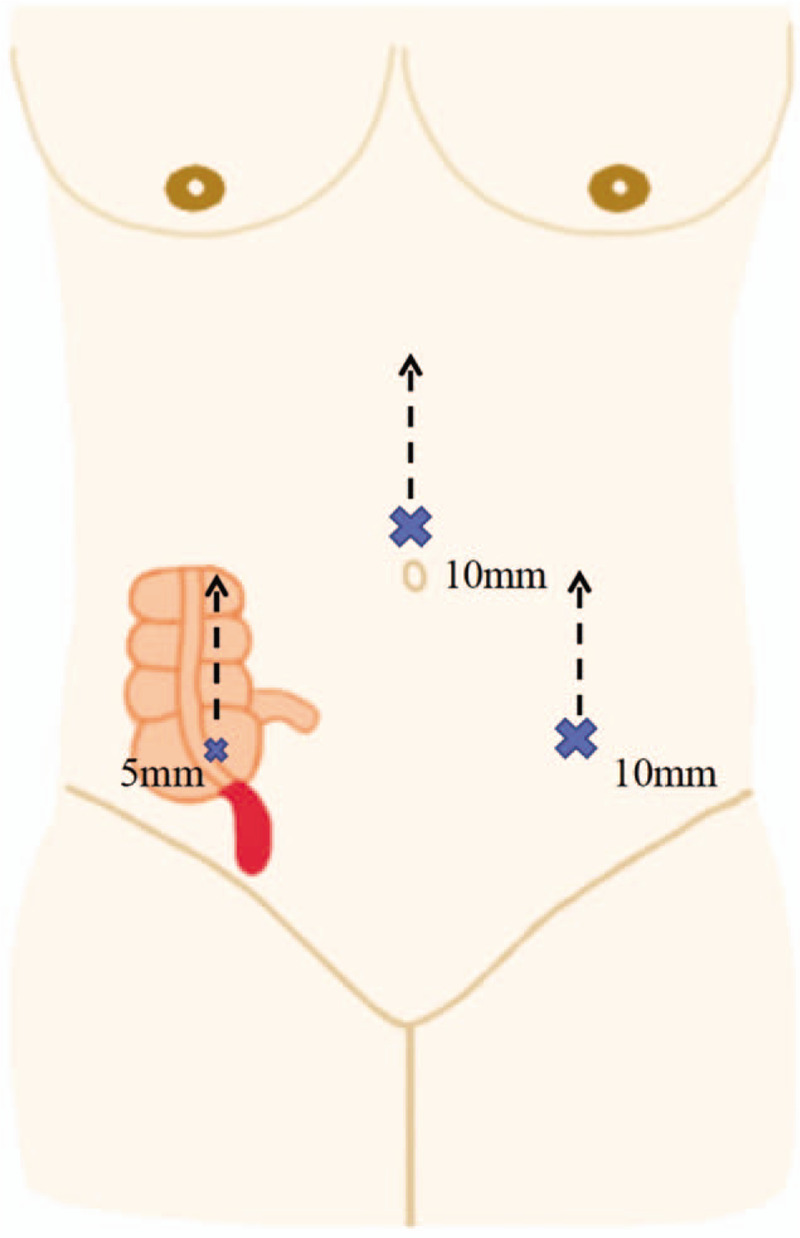
Trocar placement for laparoscopic appendectomy. The locations of these 3 ports varied according to the gestational age.
2.3. Definitions and outcomes
This study focused on AA women during the second trimester. In China, the first, second and third trimesters were defined as gestational weeks 1 to 12, 13 to 28, and 29 to 42, respectively. The demographics and preoperative data included age, body mass index, gestation time at the operation, nulliparous count, temperature, white blood cell count, neutrophil ratio, Alvarado score, and previous abdominal surgeries. The American Society of Anesthesiologists physical status classification system was used to evaluate the patient's physical state before she underwent surgery. The perioperative outcomes included anesthesia time, operative time, type of anesthesia, blood loss, complications, pathology and total length of hospital stay. A gangrenous or perforated appendix was defined as complicated appendicitis. Regarding the financial outcomes, the total expense of the treatment included the hospital basic fee and the cost of the medications, surgery, and anesthesia. The obstetric and fetal outcomes were collected through a telephone follow-up and included fetal loss, delivery period, delivery type, and birth weight. Preterm delivery was defined as childbirth occurring before 37 completed weeks or 259 days of gestation, and postterm delivery was defined as childbirth beyond 42 weeks or 294 days, according to the World Health Organization and International Federation of Obstetrics and Gynecology.[13] The purpose of this study was to evaluate the safety of LA in pregnant patients during the second trimester; thus, the primary outcomes were surgical complications, fetal loss and preterm delivery, and the secondary outcomes were other related parameters and financial outcomes.
2.4. Statistical analysis
Statistical analysis was performed using SPSS (version 25.0, SPSS Inc. Chicago, IL). Continuous variables with a normal distribution were expressed as the mean ± standard deviation (SD) and compared using independent Student t-tests. The other continuous variables were expressed as the median (range) and compared using Mann-Whitney U tests. Categorical data were expressed as the number (percentage) and compared using chi-square or Fisher exact tests, as appropriate. A P value <.05 was deemed to be significant.
3. Results
A total of 127 women with AA during pregnancy were identified between January 2016 and August 2018. Among these patients, 24 did not undergo surgery, and 46 pregnant women were in the first or third trimester. Moreover, 9 patients were excluded based on the exclusion criteria. Finally, the remaining 48 eligible patients were enrolled: 12 patients in the LA group and 36 patients in the OA group (Fig. 2).
Figure 2.
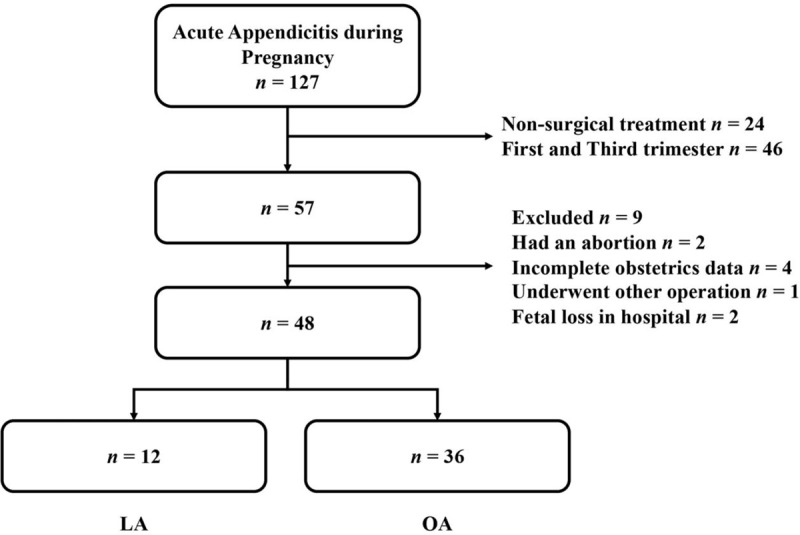
Flowchart of the included participants.
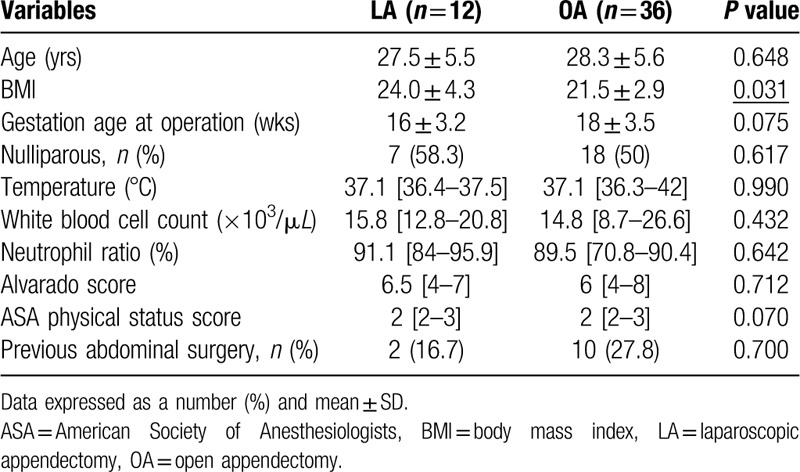
The demographics and preoperative variables are summarized in Table 1. All of the pregnant women were from China. There were no significant differences between the 2 groups in terms of age, gestation age, parous status, temperature, white blood cell count, Alvarado score, American Society of Anesthesiologists score or history of abdominal surgeries. However, interestingly, we found that the LA group had higher BMIs than the OA group (4.0 ± 4.3 vs 21.5 ± 2.9, P = .031).
Table 1.
Demographics and preoperative variables of pregnant women at second trimester undergoing laparoscopic or open appendectomy.
The perioperative data and total hospital charges are shown in Table 2. Generally, spinal anesthesia was provided for patients who underwent OA, but the anesthesia approach of 9 patients (25%) was switched to general anesthesia due to intolerable pain during the operation. Regarding surgery, the anesthesia time and blood loss volume were similar between the 2 groups. Although the operative time seemed shorter in the LA group than in the OA group, no significant difference was found [52.5 (30–150) vs 80 (35–165), P = .066]. The surgical-related complications were the primary outcomes in this study (0–30 days after operation). In the LA group, an intra-abdominal abscess developed in only 1 patient (8.3%), who was 23 years old at 24 gestational weeks. This patient was discharged from the hospital on the third day after surgery. At that time, the laboratory data were normal, and the abdominal symptoms nearly disappeared. Unfortunately, 2 weeks later, the patient developed a fever, and an abdominal cavity abscess was found; a miscarriage occurred during the anti-infective treatment. In the OA group, 3 patients had wound problems, 1 patient developed intra-abdominal abscess, and 1 patient developed pneumonia. All of these patients received routine anti-infective treatment and recovered well. A 30-year-old pregnant woman had a functional ileus with persistent abdominal distention, and the CT scan did not find any cause of the obstruction. Later, she was treated successfully by conservative treatment in the Department of Gastroenterology for 5 days. No significant difference was observed in the complication rate between the groups. We also performed a statistical analysis of the postoperative pathological types. Suppurative appendicitis was the most common type of AA in this study, accounting for 41.7% and 69.4% of the LA group and OA group, respectively. There was no significant difference in the composition ratio of the pathological types between the 2 groups. In developing countries, such as China, the patient's own choice in surgical approach is often affected by the cost of treatment. Therefore, we compared the total cost of hospitalization and cost per day between the 2 groups. As shown in Table 2, the cost per day in the LA group was higher than that in the OA group (444 ± 107 US$ vs 340 ± 115 US$, P = 0.009). However, the total cost was similar between the 2 groups (1190 ± 286 US$ vs 1184 ± 789 US$, P = .979).
Table 2.
Perioperative and financial outcomes of pregnant women at second trimester undergoing laparoscopic or open appendectomy.

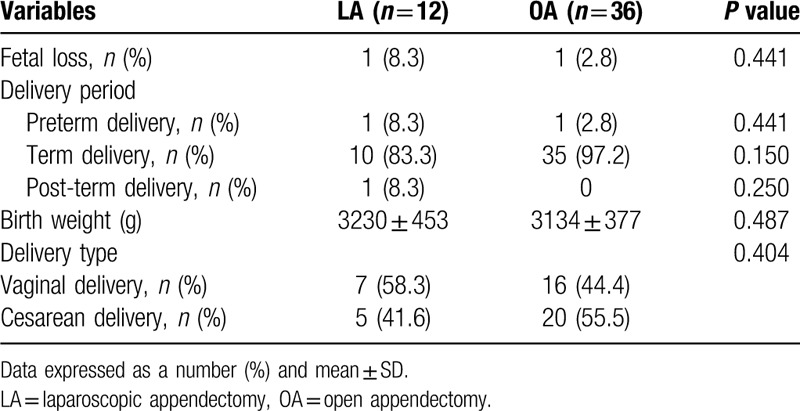
The obstetric and fetal outcomes are shown in Table 3. In each group, only 1 patient had fetal loss (8.3% vs 2.8%, P = .441). In regard to the delivery period, in the LA group, 1 patient (8.3%) suffered from preterm delivery, 10 patients (83.3%) gave birth at full term, and 1 patient (8.3%) had a postterm delivery. In the OA group, preterm delivery occurred in 1 patient (2.8%), and the remaining 35 women (97.2%) had normal deliveries at term. No significant differences were found. Similarly, there were no differences in the proportion of delivery types between the 2 groups. The birth weight and APGAR scores are very important indicators in assessing the condition of the newborn. For the former, the data between the 2 groups were equivalent (3230 ± 453 vs 3134 ± 377, P = .487). Unfortunately, for the latter, we were unable to obtain information on the APGAR score due to the limitations of the follow-up telephone interviews, and medical information is not networked in China. According to the telephone follow-up, we know that these newborns were very normal and there were no babies with birth defect, such as deformities or cerebral palsy.
Table 3.
Obstetric and fetal outcomes of pregnant women at second trimester undergoing laparoscopic or open appendectomy.
4. Discussion
Compared with other countries, the medical environment of China is very special. Most of the pregnant women and their husband in these years are single children due to 30 years of “one child policy” in China, which was just abolished at the end of 2015. Therefore, pregnancy has become a top priority for both families, leading to maternal patients becoming high-risk groups that can create medical disputes or medical problems. Hence, surgeons in China usually choose conventional OA for pregnant patients with AA to avoid potential Yinao (healthcare disturbance). However, the proven advantages of LA, which include less postoperative pain, better intraoperative visualization, better cosmetic results and so on, are very important for pregnant patients.[14] It is very unreasonable to simply abandon LA. It is very necessary to develop a complete guide for surgical indications for LA in pregnant patients. In fact, gestation time is an essential factor for pregnant patients undergoing laparoscopic operation, but well-designed studies are lacking. For example, a recent Australian study reported that OA appears to be a safer approach than LA for pregnant patients with suspected appendicitis, but there were seven (5.6%) fetal losses in the LA group, 6 of which occurred in the first trimester.[15] Thus, the results only could imply that fetal risk was very high for the patients in the LA group in the first trimester, and the study did not compare the outcomes of the patients in the second and third trimesters. In this study, only pregnant women in their second trimester were enrolled, and we compared the surgical, financial, obstetric and fetal outcomes between the LA and OA groups to assess the safety of LA.
The current results indicated that similar to OA, LA is a safe and feasible approach for pregnant women with AA during the second trimester. According to the Chinese standards, the definition of overweight and obesity is a BMI ≥ 24 kg/m2.[16] The demographics data showed that the BMI was higher in the LA group, which had a mean BMI of 24 kg/m2, indicating that the women in the LA group are more likely to be overweight or obese than those in the OA group. This difference implies that surgeons tend to choose LA for overweight patients. The reason for this trend is due to the various advantages of laparoscopic surgery in obese patents, such as lower wound infection rates, decreased incisional hernia, and better surgical exposure.[17,18] The comparable perioperative and obstetric outcomes indicated that LA is suitable for overweight or obese pregnant women. Therefore, although sufficient data is still lacking, we believe that obesity should be considered a surgical indication for LA in pregnant women during the second trimester. In the future, we will continue to study LA and this issue separately.
The anesthesia time and operative time were similar between the 2 groups. This finding is consistent with previous studies and meta-analyses.[5,19,20] However, Maimaiti et al recently reported a significantly shorter operative time in the LA group than in the OA group.[21] In our study, we found that in the first 2 cases, the operative time was over 100 minutes; however, the operative time in the last 2 patients was shortened to only 30 minutes. This finding demonstrated that the effect of the learning curve on laparoscopic operations and that the accumulation of experience could significantly reduce the operative time.[22] Whether LA has the advantage of a shortened operative time is still controversial, and more high-volume studies are needed to clarify this issue. The financial results showed that the average daily medical cost for patients who underwent LA was higher than that for patients who underwent OA, while the total cost of hospitalization was comparable between LA and OA. We believe that LA was associated with higher costs due to the need for more surgical devices and general anesthesia. The possible reason for the similar total charge is because the LA group had a shorter average hospital stay than the OA group, although there was no significant difference (2.83 ± 0.93 vs 3.78 ± 2.75, P = .253). A shorter hospitalization has been proved as an advantage of laparoscopic surgery. In our study, the lack of statistical differences may be due to our lack of experiences in LA postoperative management. In addition, due to pregnant women belong to a special patient group, surgeons may intentionally increase the length of hospital stay after surgery for safety. In China, economic factors always affect patient satisfaction and treatment decisions because the Chinese National Health Insurance only covers part of the costs; thus, the costs of some surgical instruments and medicines are borne by the patients themselves. Moreover, some patients do not even have insurance. Therefore, patients should be informed that the cost of LA surgery is higher due to the use of laparoscopic equipment and general anesthesia, but the overall cost of hospitalization is not much different.
The purpose of this study was to evaluate the feasibility and safety of LA in pregnant patients during the second trimester; therefore, the primary outcomes are the complication rates and obstetric/fetal outcomes. According to the results, the complication rates were very low, and there were no significant differences between the 2 groups. A previous study from Denmark reported that only 1 patient suffered from wound infections among 19 patients in the LA group; in contrast, 6 patients in the OA group developed complications.[23] Although there was no statistically significant difference, no wound infections were found in the LA group, supporting the hypothesis that laparoscopic surgery has an advantage regarding wound problems. Moreover, minimal incisions have favorable cosmetic results, which cannot be ignored for female patients. Particularly among young mothers, tiny and unnoticeable incisions can give lead to a high degree of satisfaction. Regarding fetal loss, complicated was is associated with a risk of fetal loss, ranging from 3% in uncomplicated appendicitis up to 20% in cases of perforated appendicitis.[24] Therefore, to better compare fetal loss, the proportions of complicated appendicitis in the 2 groups must be consistent. In our study, the rates of complicated appendicitis were 25% in the LA group and 13.9% in the OA group, which was not a significant difference. In these groups, we did not find a significant difference in the rates of fetal loss. Similarly, LA was comparable with OA in terms of the delivery period, birth weight and delivery type. Nevertheless, using CO2 for the pneumoperitoneum in a pregnant woman is worrisome. According to the latest Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines of the use laparoscopic techniques during pregnancy, CO2 insufflation of 10 to 15 mm Hg can be safely used for laparoscopy in the pregnant patients.[25] However, some surgeons argued that insufflation less than 12 mm Hg may not provide adequate visualization of the intraabdominal cavity.[26,27] In our study, the pressure was maintained at 12 mm Hg, which we considered to be very safe and reasonable. Thus, our study demonstrated that LA can be performed safely during the second trimester with good maternal and fetal outcomes.
In China, a safe operation not only means that the operation itself is safe and reliable but also that the treatment that does not lead to disagreements between the doctors and patients. The results of our study provide evidence that Chinese surgeons have reason to choose LA for pregnant patients during the second trimester. The advantages of existing laparoscopic techniques for surgery can allow more women in the second trimester, especially obese pregnant women, to achieve better treatment results and satisfaction than they could with open approaches.
Although this study was conducted in China, there are several reasons support our experiences could be applied in other countries. First, among hospitals in developed countries or top centers in developing countries, LA is a standard and matured surgical approach for AA patients. Surgeons coming from these hospitals have enough techniques and experiences to perform LA for pregnant patients during the second trimester. Second, our study provided satisfied perioperative and obstetric outcomes in LA group, and the relationship between doctors and patients in other countries is very good. Thus, we think choosing LA for pregnant patients during second trimester is allowable and reasonable in other countries. Third, our results showed LA is very safe and feasible for obese patients. Like China, in some other areas or counties where overweight or obese young patients are very common, so surgeons in these areas choose LA for those patients are justified.
There are several limitations in the current study. First, retrospective studies are associated with inevitable selection bias and follow-up bias. Second, the number of patients in this study is relatively small since the inclusion criteria are limited to pregnant women during the second trimester. Moreover, as mentioned earlier, these patients have a high risk of “Yinao”; thus, old surgeons are not willing to perform LA. Our hospital represents a top-level hospital in China but only began to perform LA in 2016. In addition, because of the ethical protections for pregnant women in clinical trials, a randomized control study is difficult to conduct. Nevertheless, the most important finding of our study is that LA is a safe surgery and is associated with equal operative and obstetric outcomes for pregnant patients during the second trimester compared with OA.
In summary, based on this study, LA is comparable with OA in the second trimester. No “Yinao” was found in any of the patients in the LA group, indicating that LA is a safe and feasible surgical approach in China. Within the proven advantages of better surgical visualization, better cosmetic results, less wound problems, and less pain than OA, LA could improve the satisfaction of pregnant patients in their second trimester, especially overweight or obese young patients. We hope our study will allow more surgeons from Chinese or other countries to try to perform LA in the second trimester. According to the current guidelines, OA is still the preferred recommended procedure for pregnant women. In the future, LA could be the first choice for AA patients during the second trimester, and well-designed prospective trials are needed to address this controversy.
Author contributions
Conceptualization: Yu-Long Cai, Nan-Sheng Cheng.
Data curation: Si-Shu Yang, Ding-Zhong Peng, Nan-Sheng Cheng.
Formal analysis: Ding-zhong Peng.
Investigation: Yu-Long Cai, Si-Shu Yang, Ding-Zhong Peng.
Methodology: Si-Shu Yang.
Project administration: Qian-Bin Jia, Hui Ye, Nan-Sheng Cheng.
Resources: Qian-Bin Jia, Fu-Yu Li, Nan-Sheng Cheng.
Software: Yu-Long Cai.
Supervision: Qian-Bin Jia, Fu-Yu Li, Hui Ye, Nan-Sheng Cheng.
Visualization: Fu-Yu Li, Nan-Sheng Cheng.
Writing – original draft: Yu-Long Cai.
Writing – review & editing: Fu-Yu Li, Hui Ye, Nan-Sheng Cheng.
Footnotes
Abbreviations: AA = acute appendicitis, LA = laparoscopic appendectomy, OA = open appendectomy.
How to cite this article: Cai YL, Yang SS, Peng DZ, Jia QB, Li FY, Ye H, Cheng NS. Laparoscopic appendectomy is safe and feasible in pregnant women during second trimester: a retrospective study in a top-level Chinese center. Medicine. 2020;99:33(e21801).
This research was supported by Sichuan Science and Technology Program (No.2020YFS0098); 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University.
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Augustin G, Majerovic M. Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol 2007;131:4–12. [DOI] [PubMed] [Google Scholar]
- [2].Pearl J, Price R, Richardson W, et al. Society of American Gastrointestinal Endoscopic S. Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 2011;25:3479–92. [DOI] [PubMed] [Google Scholar]
- [3].Andersen B, Nielsen TF. Appendicitis in pregnancy: diagnosis, management and complications. Acta Obstet Gynecol Scand 1999;78:758–62. [PubMed] [Google Scholar]
- [4].de Bakker JK, Dijksman LM, Donkervoort SC. Safety and outcome of general surgical open and laparoscopic procedures during pregnancy. Surg Endosc 2011;25:1574–8. [DOI] [PubMed] [Google Scholar]
- [5].Prodromidou A, Machairas N, Kostakis ID, et al. Outcomes after open and laparoscopic appendectomy during pregnancy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 2018;225:40–50. [DOI] [PubMed] [Google Scholar]
- [6].Di Saverio S, Birindelli A, Kelly MD, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 2016;11:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bhangu A, Soreide K, Di Saverio S, et al. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 2015;386:1278–87. [DOI] [PubMed] [Google Scholar]
- [8].Zhang L, Stone TE, Zhang J. Understanding the rise of Yinao in China: a commentary on the little known phenomenon of healthcare violence. Nurs Health Sci 2017;19:183–7. [DOI] [PubMed] [Google Scholar]
- [9].Kirshtein B, Perry ZH, Avinoach E, et al. Safety of laparoscopic appendectomy during pregnancy. World J Surg 2009;33:475–80. [DOI] [PubMed] [Google Scholar]
- [10].Cohen-Kerem R, Railton C, Oren D, et al. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg 2005;190:467–73. [DOI] [PubMed] [Google Scholar]
- [11].Curet MJ, Allen D, Josloff RK, et al. Laparoscopy during pregnancy. Arch Surg 1996;131:546–50. discussion 550-541. [DOI] [PubMed] [Google Scholar]
- [12].Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986;15:557–64. [DOI] [PubMed] [Google Scholar]
- [13].Morken NH, Klungsoyr K, Skjaerven R. Perinatal mortality by gestational week and size at birth in singleton pregnancies at and beyond term: a nationwide population-based cohort study. BMC Pregnancy Childbirth 2014;14:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lyass S, Pikarsky A, Eisenberg VH, et al. Is laparoscopic appendectomy safe in pregnant women? Surg Endosc 2001;15:377–9. [DOI] [PubMed] [Google Scholar]
- [15].Winter NN, Guest GD, Bozin M, et al. Laparoscopic or open appendicectomy for suspected appendicitis in pregnancy and evaluation of foetal outcome in Australia. ANZ J Surg 2017;87:334–8. [DOI] [PubMed] [Google Scholar]
- [16].Lin WY, Tsai SL, Albu JB, et al. Body mass index and all-cause mortality in a large Chinese cohort. CMAJ 2011;183:E329–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dindo D, Muller MK, Weber M, et al. Obesity in general elective surgery. Lancet 2003;361:2032–5. [DOI] [PubMed] [Google Scholar]
- [18].Leroy J, Ananian P, Rubino F, et al. The impact of obesity on technical feasibility and postoperative outcomes of laparoscopic left colectomy. Ann Surg 2005;241:69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chung JC, Cho GS, Shin EJ, et al. Clinical outcomes compared between laparoscopic and open appendectomy in pregnant women. Can J Surg 2013;56:341–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yoo KC, Park JH, Pak KH, et al. Could laparoscopic appendectomy in pregnant women affect obstetric outcomes? A multicenter study. Int J Colorectal Dis 2016;31:1475–81. [DOI] [PubMed] [Google Scholar]
- [21].Maimaiti A, Aierkin A, Mahmood KM, et al. Laparoscopic appendectomy in pregnancy with acute appendicitis: single center experience with world review. Surg Laparosc Endosc Percutan Tech 2017;27:460–4. [DOI] [PubMed] [Google Scholar]
- [22].van Uitert A, d’Ancona FCH, Deinum J, et al. Evaluating the learning curve for retroperitoneoscopic adrenalectomy in a high-volume center for laparoscopic adrenal surgery. Surg Endosc 2017;31:2771–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Laustsen JF, Bjerring OS, Johannessen O, et al. Laparoscopic appendectomy during pregnancy is safe for both the mother and the fetus. Dan Med J 2016;63:A5259. [PubMed] [Google Scholar]
- [24].McGee TM. Acute appendicitis in pregnancy. Aust N Z J Obstet Gynaecol 1989;29:378–85. [DOI] [PubMed] [Google Scholar]
- [25].Pearl JP, Price RR, Tonkin AE, et al. SAGES guidelines for the use of laparoscopy during pregnancy. Surg Endosc 2017;31:3767–82. [DOI] [PubMed] [Google Scholar]
- [26].Affleck DG, Handrahan DL, Egger MJ, et al. The laparoscopic management of appendicitis and cholelithiasis during pregnancy. Am J Surg 1999;178:523–9. [DOI] [PubMed] [Google Scholar]
- [27].Rollins MD, Chan KJ, Price RR. Laparoscopy for appendicitis and cholelithiasis during pregnancy: a new standard of care. Surg Endosc 2004;18:237–41. [DOI] [PubMed] [Google Scholar]


