Abstract
Background:
Suicidal ideation due to abortion has been used to justify U.S. abortion policies. Much research in abortion and mental health has relied on self-report, had low participation rates, or does not consider confounding factors. We used data that does not rely on self-report and we considered possible confounders to examine the association between abortion and nonfatal suicide attempts.
Methods:
Using Danish population registries, we conducted a cohort study by linking data from various registries. We followed women from their 18th birthday or January 1, 2000, whichever came last, until they had a first nonfatal suicide attempt, December 31, 2016, emigrated out of Denmark, or died, whichever came first. In survival analyses, we examined whether having a first abortion versus no abortion increased women’s risk of first-time nonfatal suicide attempts and whether this risk changed from before to after the abortion and over time after the abortion, adjusting for age, calendar year, mental health history, parental mental health history, childbirth history, physical health, and parental education.
Findings:
523,280 women were included in analyses (n = 48,990 had an abortion). In our fully adjusted model, the risk of nonfatal suicide attempts was the same in the year before (IRR = 2.46, 95% CI: 2.22–2.72) and after a first abortion (IRR = 2.54, 95% CI: 2.29–2.81), p = 0.509 relative to women not having an abortion, and decreased as time from the abortion increased (1–5 years afterwards IRR = 1.90, 95% CI: 1.75–2.06; 5+ years afterwards IRR = 1.73, 95% CI: 1.53–1.96).
Interpretation:
Women who had abortions were more likely to have suicide attempts. Because the increased risk was the same both the year before and after the abortion, it is not attributable to the abortion. Policies should not be justified by the notion that abortion increases women’s risk of suicide attempts.
Introduction
The claim that abortion increases women’s risk of mental health problems such as suicidal ideation (which includes thoughts, plans, and nonfatal attempts of suicide) are used to justify restrictive abortion policies in the U.S.1–3 A recent review on the safety and efficacy of abortion in the U.S. concluded abortion does not increase women’s risk of depression, anxiety, or posttraumatic stress disorder4. Other reviews by academic or professional organizations in the past 10 years that specifically focus on abortion and mental health, including suicidal ideation, have come to similar conclusions5,6. Nevertheless, one piece concluded abortion harms women’s mental health, including leading to suicidal ideation7. This piece has been shown to have serious methodological flaws such as including studies in which it is not known whether the mental health outcomes, including suicidal suicidal ideation came before or after the abortion7,8. In order to claim abortion (or any exposure) increases the risk of suicidal ideation, the abortion must occur before the increased risk of suicidal ideation.
There are fewer studies examining the association between abortion and nonfatal suicidal ideation than other more common mental health outcomes4–7,8,10–13. Those that exist are mostly based on self-report, data that are not longitudinally collected, have low participation rates, or have not been able to consider temporal precedence of the abortion versus the suicidal ideation8,10–12. The one exception to this found that among women with no psychiatric illness history, those who had an abortion had a higher rate of subsequent deliberate self-harm than women who had an unplanned pregnancy and did not request an abortion12. However, this study did not examine whether there were changes in rates or risk of self-harm from the year before to after an abortion relative to other women. This is important when drawing conclusions about whether abortion increases women’s risk of suicide attempts. If the increased risk of mental health problems is present the year before the abortion occurred and this increased risk is present and the same the year after the abortion occurred, then other confounding factors are likely the reason for the increased risk in the outcome.
Further evidence of confounding would be found if the association between abortion and nonfatal suicide attempts was attenuated in models that controlled for confounding factors compared to models that did not. Indeed, findings from a recent study using Danish population registries to examine the association between abortion and antidepressant use highlight the importance of controlling for mental health history and other possible confounders14. The current study used Danish population registries to examine the association between abortion and first-time nonfatal suicide attempts using a validated algorithm for nonfatal suicide attempts15. We examined the risk of first suicide attempts in the year before and year after the abortion, and as time after the abortion increased, adjusting for confounders including age, calendar, childbirth history, mental health history, parental mental health history, physical health, and socioeconomic status.
Methods
Study population
We used data on a cohort of women born in Denmark between January 1, 1980 and December 30, 1998 who did not die or emigrate from Denmark before their 18th birthday or study entry. Follow-up time started on the woman’s 18th birthday or January 1, 2000, whichever came last. Follow-up ended at the date of first-time suicide attempt, date of immigrating from Denmark, date of death, or December 31, 2016, whichever came first. Women were between the ages of 18 and 36 during the study period. Women who had a recorded nonfatal suicide attempts before the study period began (n = 13,075) were excluded from the study. In addition, those who had an abortion before age 18 were also excluded from this study, since abortions prior to this age require consent from parents or legal guardians. The study was approved by the Danish Protection Agency, The Danish National Board of Health, Statistics Denmark, and the University of Maryland, College Park’s IRB.
Measures
Outcome: Nonfatal suicide attempts
The main outcome was a first nonfatal suicide attempt or self-harm, which was based on information recorded in Danish population registries. First nonfatal suicide attempt or self-harm was defined using a Denmark algorithm (DK-algorithm)15, which uses two classification systems: 1) the International Classification of Disease 10th revision16 (ICD-10) of primary and secondary inpatient or outpatient discharge diagnoses at somatic and psychiatric hospitals indicating suicide attempt, intoxications, and self-injury or self-harm, and 2) the Nordic Medico Statistical Committee17 (NOMESCO) coding system (code 4 for suicide attempt or intentional self-harm). The information on hospital diagnoses were obtained from the Danish National Patient Registry18, which has information on treatment at all medical hospitals in Denmark, including dates and codes for inpatient admissions since 1970 and outpatient contacts since 1995, and the Danish Psychiatric Central Research Registry19. More specific coding information regarding the DK-algorithm were presented in a recent validation study of the DK-algorithm15.
First-time induced first-trimester abortion
First-abortions were identified through The Danish National Patient Registry18. This registry includes information on all induced abortions performed in Denmark except those performed at private clinics in 2005 or later (0.4% of all abortions in 200520). Induced first-trimester abortions were identified as the ICD-10 code: O04.
Covariates
We included the time-varying covariates of age, calendar year, childbirth, pre-existing mental health, parental mental health, and physical health, and the time-invariant covariate of socioeconomic status at age 15, all of which have been found to be associated with having abortions or with suicidal ideation or self-injurious behavior8,10–13,21–25.
Age and calendar year.
We included age and the calendar year, which were drawn from the Danish Civil Registration System26.
Childbirth.
Using the Danish Civil Registration System26, we identified whether and when women had a first childbirth during the study period.
Mental health history.
We included four measures to assess the woman’s mental health history: 1) prior inpatient or outpatient psychiatric contact (ICD-10 codes, entire F-chapter: Mental and Behavioral Disorders), 2) prior use of antidepressant medications (Anatomical Therapeutic Chemical [ATC] code N06A), 3) prior use of antipsychotic medications (ATC code: N05A), and 4) prior use of antianxiety medications (ATC codes: N05C, N05BA, N0AE01). The first measure was identified from the Danish Psychiatric Central Research Registry19, and the last three from The Danish National Prescription Registry27.
Parental mental health.
We identified whether each parent of the woman had an inpatient or outpatient psychiatric contact using the Danish Psychiatric Central Research Registry19.
Parental education.
Using the Integrated Database for Longitudinal Labor Market Research28, we identified each parent’s level of education at the woman’s 15th birthday as a measure of women’s socioeconomic status at age 15.
Charlson Comorbidity Index [CCI].
We computed a Charlson comorbidity index29, an indicator of somatic disease burden or physical health, for each woman using the Danish National Patient Registry18. The CCI consists of 19 severe, chronic diseases, each assigned a weight from one to six corresponding to the relative risk of mortality from the disease. Total possible scores range from 0–37. One’s CCI is calculated by summing all the weights. We coded women into a score of 0, 1, or 2 or more on this index.
Statistical analyses
We conducted two sets of analyses. First, survival analysis was used to examine the risk of first suicide attempts or self-harm associated with a first abortion compared to no abortion. In these survival analyses, women entered the study on their 18th birthday or January 1, 2000, whichever came last. Women ended the study at the date of first-time suicide attempt, date of immigrating from Denmark, date of death, or December 31, 2016, whichever came first. We used Poisson Regression with woman-years at risk as offset variables, which is equivalent to Cox Regression30,31, to examine incidence rate ratios (IRRs) associated with abortion. In order to examine whether the risk of suicide attempts changed from before to after the abortion and as time since abortion increased, we examined a basic model which estimated risk of suicide attempts in the year just before the abortion, the year just after the abortion, 1–5 years after the abortion, and 5 or more years after the abortion relative to not having had an abortion, and included only the time-varying covariates of age and cohort (calendar year). In the fully-adjusted model, the time-varying covariates of childbirth, prior mental health (prior psychiatric contact, prior antidepressant medications, prior antianxiety medications, prior antipsychotic medications), mother and father history of psychiatric contact, and the woman’s Charlson Comorbidity index and the time invariant covariates of mother’s and father’s education when the woman was 15 were added to the basic model.
Our second set of analyses were conducted only among women who had abortions during the study period. We examined monthly incidence rates of first-time suicide attempts of all women having an abortion in the year before and after the abortion. We also examined incidence rate ratios using the 11th and 12th month before the abortion as the reference category, adjusting for age and calendar year, allowing us to study if the incidence of suicide attempts was increased at any time in the first 12 months after an abortion. We examined these incidence rates and incidence rate ratios for all women having an abortion and stratified by previous psychiatric contact. These analyses allowed us to study whether the incidence of first suicide attempts varied in whole the year before to after the abortion, monthly in the 12 months before to after the abortion, and by whether the woman had a previous psychiatric contact.
Because the Danish algorithm may capture some individuals who did not intend to hurt themselves15, we conducted other analyses using only the ICD-10 codes of X60 to X84 or NOMESCO code 4. These codes are used for suicide attempts or intentional self-harm. Results did not change from our main analyses and so are reported in supplementary analyses. We did not investigate completed suicide because our methodology of examining relative risk and rates in the year before and after the abortion cannot be done with completed suicide and there were too few suicides in our sample for other meaningful analyses (n = 114).
Role of Funding Source
The funders of the study had no role in study design, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all data in the study and has final responsibility for the decision to submit for publication.
Results
A total of 523,280 women were included in this study. Of these, 48,990 had a record of at least one first-trimester abortion, and 10,216 women had a suicide attempt during the study period. Among women who had an abortion, 1,402 had a first suicide attempt after a first abortion.
Descriptive information of the study sample is presented in Table 1, as well as information by whether or not women had an abortion during the study period. Having an abortion was associated with having a childbirth, having prior mental health indicators, having parents with mental health indicators, worse physical health, and parental education level, ps < 0.0001; most noteworthy were the associations between having an abortion and having a childbirth, and having an abortion and prior antidepressant use.
Table 1.
Descriptive information of total sample, those having a first trimester abortion, and those not having a first-trimester abortion
| Total (n = 523,280) | Abortion (n = 48,990) | No abortion (n = 474,290) | |
|---|---|---|---|
|
Childbirth No Yes |
68.6% 31.4% |
42.6% 57.4% |
71.2% 28.8% |
|
Prior psychiatric contact No Yes |
84.8% 15.2% |
75.3% 24.7% |
85.8% 14.2% |
|
Prior antidepressant medication No Yes |
82.3% 17.6% |
67.8% 32.2% |
83.8% 16.2% |
|
Prior antianxiety medication No Yes |
87.2% 12.8% |
79.6% 20.4% |
88.0% 12.0% |
|
Prior antipsychotic medication No Yes |
95.3% 4.7% |
91.0% 9.0% |
95.8% 4.2% |
|
Father’s history of psychiatric contact No Yes |
90.1% 9.9% |
85.6% 14.4% |
90.6% 9.4% |
|
Mother’s history of psychiatric contact No Yes |
88.1% 11.9% |
83.1% 16.9% |
88.7% 11.3% |
|
Charlson Comorbidity Index 0 1 2 or more |
87.9% 10.9% 1.2% |
85.8% 12.5% 1.7% |
88.1% 10.8% 1.1% |
|
Mother’s education when women was 15 Level 1 Level 2 Level 3 Level 4 Level 5 Level 6 Level 7 Level 8 Level 9 Unknown |
24.4% 3.1% 1.5% 35.5% 3.7% 21.2% 0.7% 4.8% 0.3% 4.7% |
36.2% 2.6% 0.9% 33.7% 2.7% 16.0% 0.3% 2.4% 0.1% 5.2% |
23.1% 3.2% 1.6% 35.7% 3.8% 21.7% 0.8% 5.1% 0.3% 4.7% |
|
Father’s education when women was 15 Level 1 Level 2 Level 3 Level 4 Level 5 Level 6 Level 7 Level 8 Level 9 Unknown |
21.8% 2.9% 1.0% 41.7% 5.2% 10.7% 0.6% 7.6% 0.7% 7.7% |
29.9% 2.6% 0.7% 40.8% 3.9% 7.5% 0.4% 4.3% 0.3% 9.7% |
21.0% 3.0% 1.1% 41.8% 5.3% 11.0% 0.6% 8.0% 0.7% 7.5% |
Note. All variables differ by whether the woman had an abortion during the study period or not, p-values < 0.0001.
The number of women attempting suicide by study variables and the unadjusted rate of suicide attempts per 1000 woman-years at risk are presented in Table 2. Relative to women having no abortion (n = 474,380), women’s unadjusted rates of suicide attempts were higher in the year before, the year after, and 1–5 years after, but the same 5+ years after an abortion. The unadjusted rate of first suicide attempt was the same in the year before and after, p = 0.69, and decreased with more time from the abortion.
Table 2.
Study Variables by First-time Suicide Attempts
| Number of women with first suicide attempts (n = 10,216) | Woman-years at risk of first suicide attempts (n = 4,522,554 years) | Unadjusted rate of first suicide attempt per 1000 woman-years at risk (95% CI) | |
|---|---|---|---|
|
Abortion No abortion Year before abortion Year after abortion 1–5 years after abortion 5 + years after abortion |
8,413 401 396 692 314 |
4,137,575 45,205 45,911 149,656 144,207 |
2.03 (1.99–2.08) 8.87 (8.04–9.78) 8.63 (7.82–9.52) 4.62 (4.29–4.98) 2.18 (1.95–2.43) |
|
Childbirth No childbirth Childbirth |
9,160 1,056 |
3,666,880 866,675 |
2.51 (2.45–2.56) 1.22 (1.15–1.29) |
|
Prior psychiatric contact No Yes |
4,623 5,593 |
4,069,194 453,361 |
1.14 (1.10–1.17) 12.34 (12.02–12.66) |
|
Prior antidepressant medication No Yes |
5,365 4,851 |
3,931,084 591, 470 |
1.36 (1.33–1.40) 8.20 (7.97–8.44) |
|
Prior antianxiety medication No Yes |
7,592 2,624 |
4,124,087 398,467 |
1.84 (1.80–1.88) 6.59 (6.34–6.84) |
|
Prior antipsychotic medication No Yes |
8,151 2,065 |
4,399,557 122,997 |
1.85 (1.81–1.89) 16.79 (16.08–17.53) |
|
Mother’s history of psychiatric contact No Yes |
8,213 2,003 |
4,082,184 440,371 |
2.01 (1.97–2.06) 4.55 (4.35–4.75) |
|
Father’s history of psychiatric contact No Yes |
8,607 1,609 |
4,144,445 378, 109 |
2.08 (2.03–2.12) 4.26 (4.05–4.47) |
|
Charlson Comorbidity Index 0 (none) Score of 1 Score of 2 or more |
8,916 1,033 267 |
4,108,414 320, 893 93,248 |
2.17 (2.13–2.22) 3.22 (3.03–3.42) 2.86 (2.54–3.23) |
Results from the survival analysis are presented in Table 3. In the basic and fully adjusted model, relative to women who had not had an abortion, women who had an abortion had a higher risk of first-time suicide attempt. However, this risk of first-time nonfatal suicide attempts was similar in the year before (basic: IRR = 3.63, 95% CI: 3.29–4.02; and fully-adjusted: IRR = 2.46, 95% CI: 2.22–2.72) and after an abortion (basic: IRR = 3.89, 95% CI: 3.51–4.30, p = 0.28, and fully-adjusted: IRR = 2.54, 95% CI: 2.29–2.81, p = 0.509) and decreased with more time after the abortion (1–5 years basic: IRR = 3.02, 95% CI: 2.79–3.27; fully-adjusted: IRR = 1.90, 95% CI: 1.75–2.06; 5+ years: basic: IRR = 2.89, 95% CI: 2.56–3.27; fully-adjusted: IRR = 1.73, 95% CI: 1.53–1.96). Furthermore, the strength of the association between abortion and first nonfatal suicide attempts decreased from the basic model to the model fully-adjusted, indicating that childbirth, pre-existing mental health, parental mental health, physical health, and socioeconomic status are confounding the association between abortion and suicide attempts.
Table 3.
Adjusted Incidence Rate Ratios (and 95% CI) of Suicide Attempt by Time Relative to First-abortion (n = 523,280)
| Basic Model* | Fully adjusted model** | |
|---|---|---|
|
Abortion No abortion*** Year beforehand abortion Year after abortion 1–5 years after abortion 5 + years after abortion |
1.00 (reference) 3.63 (3.29–4.02) 3.89 (3.51–4.30) 3.02 (2.79–3.27) 2.89 (2.56–3.27) |
1.00 (reference) 2.46 (2.22–2.72) 2.54 (2.29–2.81) 1.90 (1.75–2.06) 1.73 (1.53–1.96) |
|
Childbirth No Yes |
--- --- |
1.00 (reference) 0.78 (0.73–0.84) |
|
Prior psychiatric contact No Yes |
--- --- |
1.00 (reference) 5.88 (5.59–6.18) |
|
Prior antidepressant medication No Yes |
--- --- |
1.00 (reference) 2.77 (2.63–2.92) |
|
Prior antianxiety medication No Yes |
--- --- |
1.00 (reference) 1.48 (1.41–1.56) |
|
Prior antipsychotic medication No Yes |
--- --- |
1.00 (reference) 1.69 (1.60–1.79) |
|
Mother’s history of psychiatric contact No Yes |
--- --- |
1.00 (reference) 1.21 (1.15–1.27) |
|
Father’s history of psychiatric contact No Yes |
--- --- |
1.00 (reference) 1.24 (1.18–1.31) |
|
Charlson Comorbidity Index 0 (none) Score of 1 Score of 2 or more |
--- --- --- |
1.00 (reference) 1.15 (1.08–1.23) 1.05 (0.93–1.19) |
Model includes abortion, age, and cohort (calendar year)
Model includes abortion, childbirth, age, cohort (calendar year), prior psychiatric contact, prior antianxiety medication, prior antipsychotic medication, mother’s and father’s history of psychiatric illness, and mother’s and father’s education level when woman was 15 years old
Excluding the year prior to first abortion
not included in basic model
Across all women in the sample (n = 523,380), the strongest risk factors of suicide attempts (Table 3) in the fully-adjusted model were having a previous psychiatric contact (IRR = 5.88, 95% CI: 5.59–6.18), previously obtaining an antidepressant (IRR = 2.77, 95% CI: 2.63–2.92), previously obtaining antianxiety medication (IRR = 1.48, 95% CI: 1.41–1.56), and previously obtaining antipsychotic medication (IRR = 1.69, 95% CI: 1.60–1.79).
Examining the unadjusted incidence rates in monthly increments during the year before and after an abortion, we found rates of suicide attempts were relatively stable for all women having an abortion, for women with a previous psychiatric contact having an abortion, and for women without a previous psychiatric contact having an abortion (Figure 1). When we compared the unadjusted incident rates from the whole year before to the whole year after the abortion for all women, women with a previous psychiatric contact, and women without a previous psychiatric contact, there were no changes from the year before (all women IR = 8.87, 95% CI: 8.04–9.76; women with a previous psychiatric contact IR = 30.99, 95% CI:26.96–35.62; women without a previous psychiatric contact IR = 5.23; 95% CI:4.56–6.00) to the year after an abortion (all women IR = 8.62, 95% CI: 7.82–9.52, p = 0.69; women with a previous psychiatric contact IR = 27.18, 95% CI:23.57–31.34, p = 0.40; women without a previous psychiatric contact IR = 5.31; 95% CI:4.64–6.09, p = 0.40). Furthermore, suicide attempt rates in the year before and after the abortion differed by whether women had a previous psychiatric contact as indicated by the nonoverlapping confidence intervals in Figure 1B.
Figure 1.
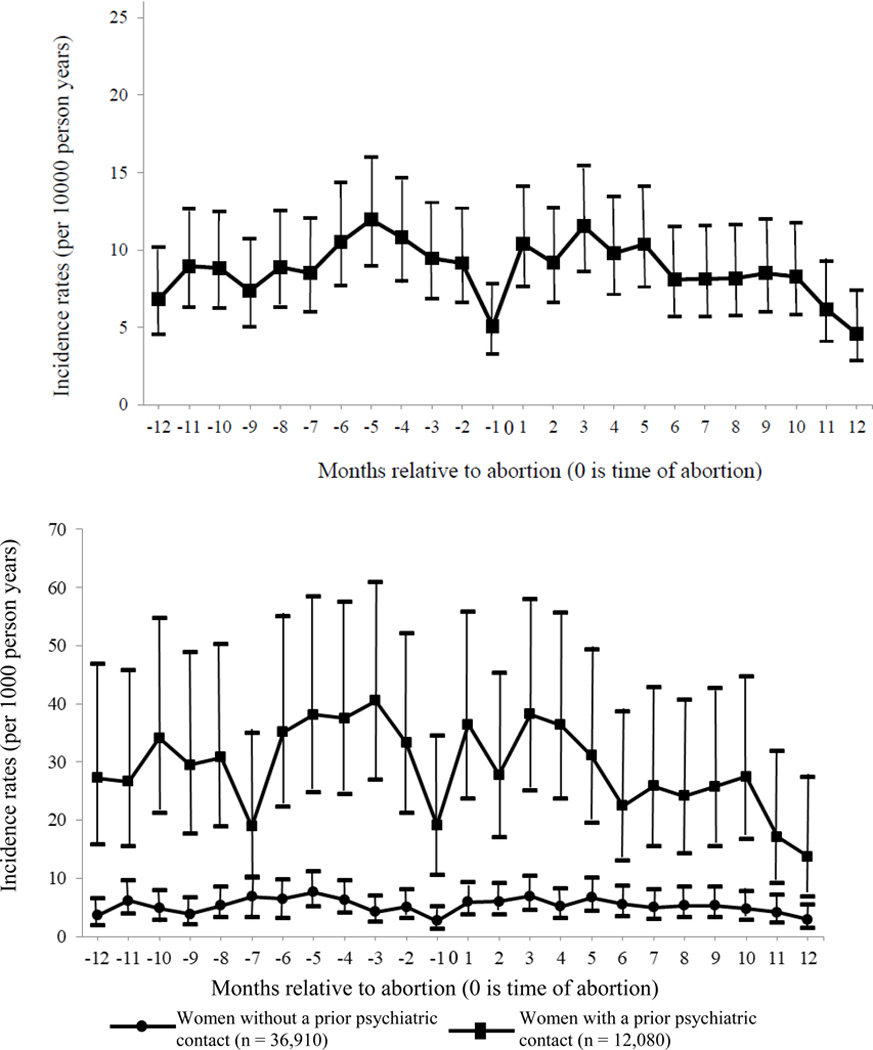
Unadjusted Incidence Rates of First Suicide Attempt in the Year Before and Year After a First First-trimester Abortion. Panel A: All Women Having an Abortion; Panel B: Women Having an Abortion Stratified by Prior Psychiatric Contact.
Panel A. Women having had a first first-trimester abortion (n = 48,990)
Panel B. Women having had a first first-trimester abortion stratified by prior psychiatric contact
Notes: The period −12 to 0 refers to the period from 12 months before the abortion. І indicates 95% confidence intervals.
Figure 2 presents age and calendar-year adjusted incidence rate ratios (IRRs) of first-time suicide attempts in monthly increments from the year before and after an abortion compared to the 11th and 12th month beforehand (our defined reference group). Panel A presents IRRs for all women who had an abortion; Panel B for all women who had an abortion who had a prior psychiatric contact; and Panel C for all women who had an abortion without a prior psychiatric contact. All panels show that there are no changesin the monthly adjusted rates relative to the 11th and 12 months before an abortion from the 10 months before to the year after an abortion.
Figure 2.
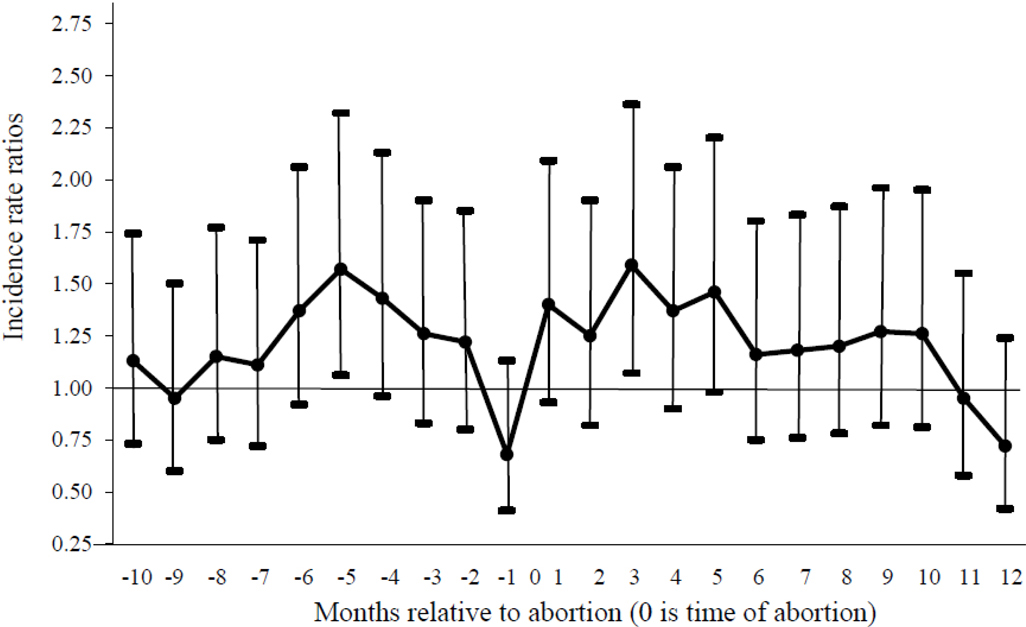
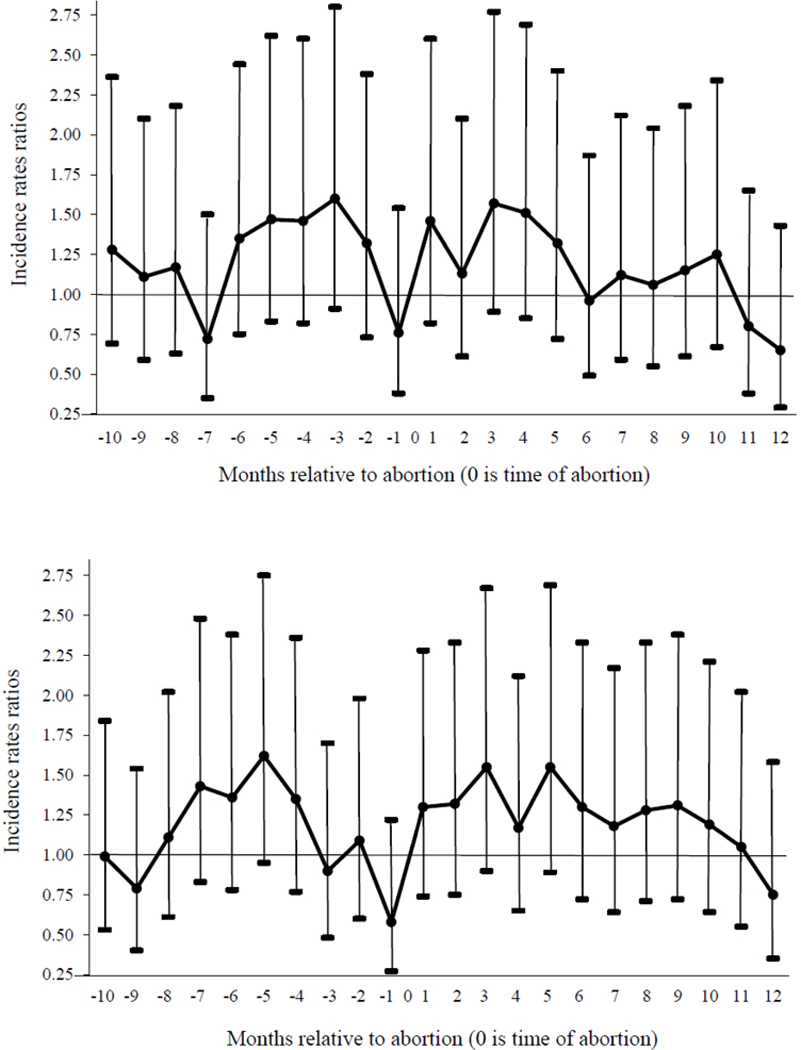
Age and calendar year adjusted Incidence Rate Ratios of First Suicide Attempt Before and After a First First-Trimester Abortion for All Women Who had an Abortion (Panel A), Women Having had an Abortion Who Had a Prior Psychiatric Contact (Panel B), and Women Having had an Abortion Who Did Not Have a Prior Psychiatric (Panel C).
Panel A. Women having had a first first-trimester abortion (n = 48,990)
Panel B. Women having had a first first-trimester abortion with a prior psychiatric contact (n = 12,080)
Panel C. Women having had a first first-trimester abortion without a prior psychiatric contact (n = 36,910)
Notes. The horizontal line indicates the reference group of the 11th and 12th months before the abortion for each group. Error bars indicate 95% Cis. All numbers in Figure 2 are adjusted for age and cohort.
Discussion
Using longitudinal data on abortion and nonfatal suicide attempts available in population registries, we examined risk of first nonfatal suicide attempt associated with a first abortion. These data allowed us to not rely on women’s self-report of mental health experiences or abortion. Compared to women who did not have an abortion, those who did had a higher risk of nonfatal suicide attempts. However, a close look at the data, including all analyses presented here, suggests that abortion itself did not contribute to the higher risk, supporting conclusions from other research4–6. First, the increased relative risk was the same in the whole year before and after the abortion. And the rates of first time suicide attempts did not change from the whole year before to after the abortion. That is, we found that monthly suicide attempt rates from the 10 months before the abortion to 12 months afterwards are similar to the combined 11th and 12th month rate before the abortion, which is approximately 9 months before conception (see Figures 1 and 2). Second the relative risk of suicide attempts decreased as more time from the abortion increased, countering the notion that the effects of abortion are not experienced until a long time after the abortion32. Third, the relative risk associated with abortion decreased from the basic adjusted model, which controlled for only age and calendar year, to the fully adjusted model which also controlled for childbirth history, mental health history, parental mental health history, physical health history, and socioeconomic status. Together these findings provide evidence that there are shared risk factors such as mental health history for both having an abortion and having suicide attempts.
When we examined incidence rates in the year before and after an abortion for all women who had an abortion, for women with a previous psychiatric contact, and for women with no previous psychiatric contact, we found no changes in incidence rates from the year before to the year after the abortion for all three groups. Noteworthy, we found the incidence rates in the year before and after an abortion for women having a previous psychiatric contact were much higher (IR = 30.99 beforehand and IR = 27.18 and afterwards) than for women having no previous psychiatric contact (IR = 5.23 beforehand and IR = 5.31 afterwards).
Interestingly, the association between abortion and suicide attempts for all times relative to an abortion (compared to no abortion) decreased in the fully adjusted model relative to the basic model, indicating that pre-existing mental health and the other covariates are confounding the association between abortion and suicide attempts. Other research has not found a statistically significant association between abortion and suicidal ideation in models that adjusted for confounding factors such as prior mental health, intimate partner violence, childhood adversities, or pregnancy intention10–12. Had we in the present study been able to consider other confounding factors both proximal to the pregnancy such as pregnancy intention or wantedness or intimate partner violence or more distal such as childhood adversities, the observed association may have been reduced further. Moreover, the strongest predictors of first-time suicide attempts were indicators of prior mental health problems, and particularly having had treatment at psychiatric facilities. It should be noted that we also did not control for miscarriage history in our analyses. Another study examining the association between abortion and subsequent suicidal ideation has not found miscarriage history to be associated with subsequent suicidal ideation in adjusted models10,41.
Our results support and strengthen other research that has used Danish population registries and found that abortion does not increase women’s risk of other mental health indicators13,32. They also suggest that the abortion care setting may be an appropriate place to integrate mental health screenings. Integrating such services may help women seek treatment for pre-existing mental health issues and prevent future mental health problems.
Our study has limitations worth mentioning. Our measure of nonfatal suicide attempts includes suicide attempts, self-harm with intention to hurt oneself, and self-harm without intention to die15. Thus, not all suicide attempts may have been with the intention to harm oneself or die. However, when we conducted supplementary analyses in which we only examined the outcome of suicide attempts or intentional self-harm, we found similar results (see supplementary analyses). Second, it is not clear whether the results generalize to other contexts, particularly where access to abortion is legally restricted. Nevertheless, one study in the U.S. that compared suicidal ideation after being denied an abortion versus being allowed to have an abortion did not find differences in the five years afterwards12. Third, while we were able to control for prior mental health problems that had been recorded in the Danish registries, it is likely that women experienced mental health problems which were not recorded because they did not receive treatment or seek medical advice. Thus, prior mental health problems may have been underestimated.
In addition, we do not examine recurrent suicide attempts or suicide attempts around a second or more abortion. Other studies in the abortion and mental health literature have examined recurrent mental health problems separate from incident ones33–35; and scholars have suggested or research found recurrent suicide attempts or mental health problems are distinct from incident or new suicide attempts or mental health problems36–38. Researchers also contend that having a second or more abortion is distinct from having a first abortion39. Thus, future studies could examine recurrent mental health problems, including suicide attempts, and mental health around second or more abortions.
Our findings do not support the notion that abortion causes or increases women’s risk of suicide attempts. In fact, our findings support the conclusion that heightened suicide attempts is not due to abortion but differences in other risk factors for suicide attempts. Consequently, policies based on the notion that abortion increases women’s risk of suicide attempts are misinformed.
Supplementary Material
Research in Context.
Evidence before this study
Understanding the association between abortion and suicidal ideation (including thoughts, plans, or attempts of suicide) has policy implications in the U.S. and beyond. In 2008 and 2011, two independent professional and academic organizations published systematic reviews or meta-analyses on abortion and mental health4,40. In these reviews, only 6 studies examined the association between abortion and suicidal ideation. However, as noted by one of the systematic reviews, the studies were of varying quality4. Both reviews concluded that abortion does not cause or increase women’s risk of mental health problems4,40. We searched pubmed, psycinfo, and web of science for articles published between January 1, 2008 and July 15, 2019 using the search terms of “abortion” and “suicidal ideation”; “abortion” and “suicide attempts”; “abortion” and “self-harm”; “abortion” and “self harm”; “abortion” and “suicidal behavior/behaviour”; “termination of pregnancy” and “suicidal ideation”; “termination of pregnancy” and “suicide attempts”; “termination of pregnancy” and “self-harm”; “termination of pregnancy” and “self harm”; “termination of pregnancy” and “suicidal behaviour/behaviour”. From this search, we found 103 articles, 13 of which were tested the association between abortion and suicidal ideation, suicide attempts, or self-harm. We also searched the references of these articles and found 1 more study on suicidal ideation published since 2008. Of these 14 articles, there were 3 data sets each with two different articles published using them (for a total of 6 of the 14 articles). For two of the data sets, the results of the two articles were the same, and so we only include one of these two. For one of the data sets, results differed and so we discuss both of these two below. Thus, we discuss a total of 12 i articles on abortion and suicidal ideation since 2008. 6 of the 12 studies found no statistically significant association between abortion and suicidal ideation, and 6 found a statistically significant association. Studies were of varying quality. Two of the six that found statistically significant associations were not able to determine whether the abortion came before or after suicidal ideation; and one was a cross sectional study of postmenopausal women, thus relying on women reporting on abortions that occurred several years in the past.
Added value of this study
The existing studies on abortion and suicidal ideation (or attempts or self-harm) are all based on self-report of abortion and suicidal ideation, and none have examined the risk or rates of suicide attempts or ideation, or self-harm in the year before versus after the abortion. It is important to examine rates and risk of suicide attempts before and after abortion and use data not based on self-report, in order to understand whether abortion increases women’s risk or causes suicidal ideation. The current study uses Danish population registries to examine the association between abortion and first-time nonfatal suicide attempts, and examines rates and risk (relative to women who do not have abortions) in the year before and after an abortion, and as time from the abortion increases.
Implications of all the available evidence
The current study findings suggest that women who have abortions are more likely to have first-time nonfatal suicide attempts than women who do not have abortions. Because rates and risk of suicide attempts were the same before and after the abortion, the association is not due to the abortion but other factors associated with both having an abortion and mental health problems. Thus, policies based on the notion that abortion causes or increases women’s risk of suicidal ideation are not supported by evidence.
Acknowledgments
Funding: Society of Family Planning; The American Foundation for Suicide Prevention; iPSYCH The Lundbeck Foundation Initiative for Integrative Psychiatric Research.
Footnotes
Declariations of Interest: Dr. Steinberg has served as a scientific expert on the topic of abortion and mental health in 4 legal challenges to state laws in the United States. In this role as a scientific expert, Dr. Steinberg has served as a consultant for legal teams at the Center for Reproductive Rights and Planned Parenthood Federation of America.
References
- 1.South Dakota Codified Law. 34-23A-10.1. 2005. Available at: http://legis.state.sd.us/statutes/DisplayStatute.aspx?Type=Statute&Statute=34-23A-10.1. Accessed March 8, 2019.
- 2.Texas Department of State Health Services (2016). A Woman’s Right to Know: Informational Material. Available at: https://www.dshs.texas.gov/wrtk/. Accessed March 11, 2019.
- 3.Stotland NL, Shrestha AD. More evidence that abortion is not associated with increased risk of mental illness. JAMA-Psychiatry 2018; 75(8): 775–776. [DOI] [PubMed] [Google Scholar]
- 4.National Academies of Science, Engineering, and Medicine. The safety and quality of abortion care in the United States 2018; Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 5.Major B, Appelbaum M, Beckman L, Dutton MA, Russo NF, West C. Abortion and mental health: Evaluating the Evidence 2009; 64 (9): 863–890. [DOI] [PubMed] [Google Scholar]
- 6.National Collaborating Centre for Mental Health. Induced abortion and mental health: A systematic review of the mental health outcomes of induced abortion, including their prevalence and associated factors 2011; London, UK: Academy of Medical Royal Colleges. [Google Scholar]
- 7.Coleman PK. Abortion and mental health; quantitative synthesis and analysis of research published 1995–2009. British Journal of Psychiatry 2011; 199 (3) 180–186. [DOI] [PubMed] [Google Scholar]
- 8.Mota NP, Burnett M, Sareen J. Associations between abortion, mental disorders, and suicidal behavior in a nationally representative sample. The Canadian Journal of Psychiatry 2010; 55 (4): 239–247. [DOI] [PubMed] [Google Scholar]
- 9.Steinberg JR, Trussell J, Hall KS, Guthrie K. Fatal flaws in a recent meta-analysis on abortion and mental health. Contraception 2012; 86 (5): 430–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinberg JR, McCulloch CE, Adler NE. Abortion and mental health: Findings from the National Comorbidity Survey-Replication. Obstetrics & Gynecology 2014; 123 (2): 263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fergusson DM, Horwood LJ, Boden JM. Does abortion reduce the mental health risks of unwanted or unintended pregnancy? A reappraisal of the evidence. Australian & New Zealand Journal of Psychiatry 2013; 47 (9): 819–827. [DOI] [PubMed] [Google Scholar]
- 12.Biggs MA, Gould H, Barar RE, Foster DG. Five-year suicidal ideation trajectories among women receiving or being denied an abortion. American Journal of Psychiatry 2018; 175 (9): 845–852. [DOI] [PubMed] [Google Scholar]
- 13.Gilchrist AC, Hannaford PC, Frank P, Kay CR. Termination of pregnancy and psychiatric morbidity. British Journal of Psychiatry 1995; 167 (2): 243–248. [DOI] [PubMed] [Google Scholar]
- 14.Steinberg JR, Laursen TM, Adler NE, Gasse C, Agerbo E, Munk-Olsen T. Examining the association of antidepressant prescriptions with first abortion and first childbirth. JAMA-Psychiatry 2018; 75 (8): 828–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gasse C, Danielsen AA, Pedersen MG, Pedersen CB, Mors O, Christensen J. Positive predictive value of a register-based algorithm using the Danish National Registries to identify suicidal events. Pharmacoepidemiology Drug Safety 2018; 27 (10): 1131–1138. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines 1992; Geneva: World Health Organization. [Google Scholar]
- 17.Nordic Medico-Statistical Committee. NOMESCO Classification of External Causes of Injuries, 4th revised edition 2007; Copenhagen, Denmark: p. 28 Available at: https://norden.diva-portal.org/smash/get/diva2:1201255/FULLTEXT01.pdf Accessed March 11, 2019. [Google Scholar]
- 18.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clinical Epidemiology 2015; 7: 449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scandinavian Journal of Public Health 2011; 39 (7) (suppl): 54–57. [DOI] [PubMed] [Google Scholar]
- 20.Legalt Provokerede Aborter 2005. (oreløbig opgørelse). Copehagen, Denmark: Sundhedsstyrelsen; 2006: 1–10. [Google Scholar]
- 21.Jerman J, Jones RK, Onda T. Characteristics of U.S. abortion patients in 2014 and changes since 2008. New York: Guttmacher Institute, 2016. Available at: https://www.guttmacher.org/report/characteristics-us-abortion-patients-2014. Accessed March 11, 2019. [Google Scholar]
- 22.Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, Hammad TA, Temple R, Rochester G. Risk of Suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. British Medical Journal 2009; 339 (b2880): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Offson M, Blanco C, Wall M, Saha TD, Pickering RP, Grant BF. National trends in suicide attempts among adults in the United States. JAMA Psychiatry 2017; 74 (11): 1095–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodday SM, Shuldiner J, Bondy S, Rhodes AE. Exposure to parental psychopathology and offspring’s risk of suicide-related thoughts and behaviours: a systematic review. Epidemiology and Psychiatric Sciences 2019; 28 (2): 179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mather AA, Cox BJ, Enns MW, Sareen J. Associations of obesity and psychiatric disorders and suicidal behaviors in a nationally representative sample. Journal of Psychosomatic Research 2009; 66 (4): 277–285. [DOI] [PubMed] [Google Scholar]
- 26.Pedersen CB. The Danish Civil Registration System. Scandinavian Journal of Public Health 2011; 39 (7) (suppl): 22–25. [DOI] [PubMed] [Google Scholar]
- 27.Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scandinavian Journal of Public Health 2011; 39 (7) (suppl): 38–41. [DOI] [PubMed] [Google Scholar]
- 28.Timmermans B The Danish Integrated Database for Labor Market Research: towards demystification for the English speaking audience . DRUID Working Paper No 10–16. 2010. Available at: https://www.researchgate.net/publication/46451548_The_Danish_Integrated_Database_for_Labor_Market_Research_Towards_Demystification_for_the_English_Speaking_Audience. Accessed March 11, 2019. [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies. Journal of Chronic Disease 1987; 40 (5): 373–383. [DOI] [PubMed] [Google Scholar]
- 30.Efron B Logistic Regression, Survival Analysis, and the Kaplan-Meier Curve. Journal of the American Statistical Association 1988; 83 (402): 414–425. [Google Scholar]
- 31.Iacobelli S, Carstensen B. Multiple time scales in multi-state models. Statistics in Medicine 2013; 32 (30): 5315–5327. [DOI] [PubMed] [Google Scholar]
- 32.Speckhard AC, Rue VM. Post abortion syndrome: an emerging public health concern. Journal of Social Issues 1992; 48 (3): 95–119. [Google Scholar]
- 33.Munk-Olsen T, Laursen TM, Pedersen CB, Lidegaard Ø, Mortensen PB. Induced first-trimester abortion and risk of mental disorder. New England Journal of Medicine 2011; 364 (4): 332–339. [DOI] [PubMed] [Google Scholar]
- 34.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. American Journal of Psychiatry 2008; 164 (7): 1035–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munk-Olsen T, Laursen TM, Pedersen CB, Lidegaard Ø, Mortensen PB. First-time first-trimester induced abortion and risk of readmission to a psychiatric hospital in women with a history of treated mental disorder. Archives of General Psychiatry 2012; 69 (2): 159–165. [DOI] [PubMed] [Google Scholar]
- 36.van Ditzhuijzen J, Ten Have M, de Graaf R, Lugtig P, van Nijnatten CHCJ, Vollebergh WAM. Incidence ad recurrence of common mental disorders after abortion: Results from a prospective cohort study. Journal of Psychiatric Research 2017; 84: 200–2006. [DOI] [PubMed] [Google Scholar]
- 37.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). 2013; Washington, DC; American Psychiatric Association. [Google Scholar]
- 38.Beghi M, Rosenbaum JF, Cerri C, Cornaggia CM. Risk factors for fatal and nonfatal repetition of suicide attempts: a literature review. Neuropsychiatric Disease and Treatment 2013; 9: 1725–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewinsohn PM, Allen NB, Seeley JR, Gotlib IH. First onset versus recurrence of depression: Differential process of psychosocial risk. Journal of Abnormal Psychology 1999; 108 (3): 483–489. [DOI] [PubMed] [Google Scholar]
- 40.American Psychological Association. Task force report on mental health and abortion Report of the Task Force on Mental Health and Abortion 2008. Washington, DC: American Psychological Association; Available at: https://www.apa.org/pi/women/programs/abortion/mental-health.pdf. Retrieved August 29, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


