Abstract
Hoarding disorder is characterized by difficulty parting with possessions and by clutter that impairs the functionality of living spaces. Cognitive behavioral therapy conducted by a therapist (individual or in a group) for hoarding symptoms has shown promise. For those who cannot afford or access the services of a therapist, one alternative is an evidence-based, highly structured, short-term, skills-based group using CBT principles but led by non-professional facilitators (the Buried in Treasures [BIT] Workshop). BIT has achieved improvement rates similar to those of psychologist-led CBT. Regardless of modality, however, clinically relevant symptoms remain after treatment, and new approaches to augment existing treatments are needed. Based on two recent studies - one reporting that personalized care and accountability made treatments more acceptable to individuals with hoarding disorder and another reporting that greater number of home sessions were associated with better clinical outcomes, we tested the feasibility and effectiveness of adding personalized, in-home uncluttering sessions to the final weeks of BIT. Participants (n=5) had 15 sessions of BIT and up to 20 hours of in-home uncluttering. Reductions in hoarding symptoms, clutter, and impairment of daily activities were observed. Treatment response rate was comparable to rates in other BIT studies, with continued improvement in clutter level after in-home uncluttering sessions. This small study suggests that adding in-home uncluttering sessions to BIT is feasible and effective.
Keywords: Hoarding disorder, Buried in Treasures, BIT, Clutter, CBT, uncluttering
Introduction
Individuals with hoarding disorder (HD) have persistent difficulties parting with possessions, and clutter that hinders the intended use of living spaces and causes distress (American Psychiatric Association, 2013). HD not only affects the individual, placing him or her at risk for eviction, but also neighbors by increasing risk of fire and pest infestation (Frost et al., 2012b). HD is common and impairing, with prevalence estimates ranging from 1.5% – 6%, depending on the assessment method used (Nordsletten et al., 2013; Timpano et al., 2011).
Targeting hoarding symptoms with cognitive behavior therapy (CBT) conducted by a therapist (via individual or group treatment) has shown therapeutic promise (Tolin et al., 2015). For those who cannot afford or access the services of a therapist, one alternative is a short-term, evidence-based, skills-based support group using CBT principles (Buried in Treasures [BIT] Workshop) but led by a non-professional facilitator student/trainee (Frost et al., 2011) or a peer (Frost et al., 2012a). The BIT manual’s 15 structured sessions are based on the book, Buried in Treasures: Help for Compulsive Acquiring, Saving and Hoarding (Tolin et al., 2007). The topics include psycho-education about hoarding disorder, enhancing motivation, learning to resist progressively stronger triggers to acquire (e.g., during trips to flea markets), cognitive restructuring exercises, and imagined and actual discarding. BIT significantly reduced hoarding symptoms compared to a wait-list control (Frost et al., 2012a) and achieved improvement rates similar to those of psychologist-led CBT (Mathews et al., 2016). Unfortunately, in many individuals with hoarding disorder, impairing symptoms remain after treatment (up to 75% when using a conservative estimate of hoarding symptom score change), especially with respect to the level of clutter in the home, regardless of modality or type of facilitator (Tolin et al., 2015)(Moulding et al., 2017). In addition, under-utilization of treatments and services for hoarding disorder by consumers remains a challenge (Frost et al., 2011) and identifying what aspects and types of current treatments are most acceptable can guide treatment development. Taken together, this suggests new and acceptable approaches are needed to help these individuals.
To assist individuals with residual hoarding symptoms, we first conducted an online survey study of treatment acceptability in participants (n=203) with clinically meaningful hoarding symptoms. Participants reported that personalization of care (e.g., individual sessions customized to the consumer’s unique in-home needs) and accountability made treatments most acceptable (Rodriguez et al., 2016). Based on these findings and a meta-analysis reporting that greater number of home sessions were associated with better clinical outcomes (Tolin et al., 2015), we hypothesized that adding a personalized, in-home unclutter component would augment BIT treatment by decreasing hoarding symptoms, reducing clutter levels and improving activities of daily living. We also posited that the in-home intervention would be feasible and well tolerated.
Method
Participants
With institutional review board approval, five participants were recruited (February to July 2015) via study advertisements posted online and in the local community, and by referrals from mental health professionals. All participants provided written informed consent and met DSM-5 criteria for HD (American Psychiatric Association, 2013), with clinically significant hoarding disorder (Saving Inventory-Revised [SI-R] ≥ 41) (Frost et al., 2012b) and clutter that impaired living conditions (Clutter Image Rating [CIR] ≥ 4) (Frost et al., 2008). Potential participants were excluded if they were severely depressed (Hamilton Depression Rating Scale ≥ 30; Hamilton, 1960) or at risk of suicide (Columbia Suicide Severity Rating Scale ≥ 4; Posner et al., 2011), unable to follow study procedures, unwilling to have unclutter volunteers enter the home, had clutter levels with the potential for objects falling on volunteers (CIR >8; approximately above shoulder height or higher), had evidence of pest infestation, animal hoarding, or were at high risk of eviction (e.g., eviction-related legal proceedings that may require a higher level of care coordination). Of the 24 individuals who contacted the clinic interested in participating in a hoarding disorder study, 10 were excluded for living out of town or not returning message to schedule a screening appointment. Of 14 individuals screened, 5 were eligible and enrolled. Nine of fourteen (64%) were excluded for being at risk for eviction (n=4), recently receiving an eviction notice (n=1), not able to comply with study procedures (n=2), and not being amenable to the in-home component (n=2). Study participants’ (n=5) median age was 59 years (range = 42–69), consistent with other HD treatment studies (Frost et al., 2012a, 2011). All five participants were females (4 were Caucasian and 1 was African-American). None of the participants met criteria for current comorbid major depression.
Measures
Participants completed the following assessments at baseline, 12 weeks, and 18 weeks.
Saving Inventory-Revised (SI-R). The SI-R is a 23-item self-report hoarding severity measure (Frost, Steketee, & Grisham, 2004). It assesses three distinct hoarding factors: clutter severity, difficulty discarding, and excessive acquisition. Individual items are measured on a 0 – 4 scale, with zero indicating “none” and four indicating “almost all.” Individual responses are summed and outcome measures include a total score of hoarding severity and three subscales – difficulty discarding, clutter, and excessive acquisition. The cut-off score (SI-R total score of 41) for clinical significance (i.e., distinguishing community control from individuals that meet hoarding disorder criteria) is based on receiver operating characteristics curves (Frost, Steketee, & Tolin, 2012; Tolin, Frost, & Steketee, 2010). Gilliam and colleagues suggested a definition for clinically significant change for hoarding disorder using the SI-R as “a 14 point or greater reduction from pre- to post-treatment and a post-treatment score of 42 or less, which is the point half-way between the means of the clinical and nonclinical populations (Frost et al., 2004)” (Gilliam et al., 2011). The SI-R has been shown to have good internal consistency and test-retest reliability (Frost et al., 2004). It is considered an appropriate instrument for assessing hoarding symptoms in clinical and non-clinical samples (Frost et al., 2004) and is sensitive to treatment effects (Steketee et al., 2010).
Clutter Image Rating (CIR). The CIR is a pictorial scale assessing clutter level in three major rooms: kitchen, bedroom, and living room. It consists of three sets of nine images (one set per room) with images varying from not cluttered to extremely cluttered rooms (for image examples see Frost, Steketee, Tolin, & Renaud, 2008). Participants selected the photograph with the level of clutter that most closely resembled their own. Scores for each room range from 1 (least cluttered) to 9 (most cluttered). A mean composite score is calculated for the three rooms of the home; this score has high internal consistency and test-retest reliability (Frost et al., 2008). Strong correlations between participant self-report in the clinic and experiment ratings of the CIR in the home (r = 0.74) suggest individuals with hoarding disorder are able to reliably rate the severity of their clutter (Frost et al., 2008). Independent studies have validated CIR’s psychometric properties in HD participants across the lifespan (Dozier and Ayers, 2015; Frost et al., 2008).
Activities of Daily Living for Hoarding (ADL-H). The ADL-H is a 15-item self-report questionnaire assessing the degree to which hoarding symptoms impair daily activities (Frost et al., 2013). Individuals rate the effects of hoarding or clutter on different activities. Items are measured on a scale from 1 (“can do it easily”) to 5 (“unable to do”). A response of “non-applicable” is given for activities that do not apply to the participant. Outcome measure is an average score of all applicable activities. ADL-H has good internal consistency and test-retest reliability (Frost et al., 2013).
Group Facilitator and Uncluttering Volunteer Recruitment, Training, and Supervision
Recruitment for group facilitators and uncluttering volunteers consisted of verbal announcements at lab meetings. All of the group facilitators (n=2) and uncluttering volunteers (n=4) had completed a bachelor’s degree within two years, were interested in the field, and were volunteers for multiple other lab studies. The uncluttering volunteers were distinct from the group facilitators; and only in one instance did a facilitator conduct an in-home session (as backup) when the regular uncluttering volunteers were unexpectedly unable attend the home session.
Training for all group facilitators and uncluttering volunteers consisted of a 2-day training course led by CIR (live) and RF and LS (video), and included content on hoarding disorder symptoms, treatment, BIT workshop, and in-home uncluttering. The course was interactive and included live role play exercises detailed in the Buried in Treasures workbook (Tolin et al., 2007) and the BIT facilitator’s guide (Shuer and Frost, 2014). In addition, all group facilitators and uncluttering volunteers read seminal research papers regarding hoarding disorder by RF and the BIT Facilitator’s guide by LS and RF. This initial training was augmented by ongoing weekly group phone supervision by CIR and an experienced peer support specialist (LS) to review materials for upcoming sessions, discuss cases, answer questions, and advise as needed.
Procedure
Participants completed both the BIT workshop and in-home uncluttering sessions. Participants made 17 study-related visits to the study site: a baseline visit at the study start, 15 weekly visits for the BIT workshop, and a close-out visit at the study’s completion. In addition, pairs of trained non-professional uncluttering volunteers visited each participant’s home up to 10 visits for the in-home uncluttering sessions.
The BIT workshop group met weekly for 15 weeks over the course of 17 weeks with a one-week break during week 9 and a two-week break during weeks 16–17 (see supplemental table S1). BIT consisted of the structured format detailed in the Buried in Treasures workbook (Tolin et al., 2007) and the BIT facilitator’s guide (Shuer and Frost, 2014). Each 2-hour group session was led by two trained, non-professional group facilitators (DS and CL). The BIT workshop followed the methods of Frost et al., (2012a), starting with psycho-education about HD and non-acquiring skills (i.e., identifying acquisition triggers and developing ways to tolerate urges to acquire items), before moving to content regarding skills for parting with possessions.
The in-home uncluttering component (10 two-hour sessions) was designed by RF, LS, and CIR to build in active uncluttering practice during the BIT workshop breaks (Table S1). After a single introductory session (consisting of participants meeting with their facilitators for the first time and discussing upcoming study procedures), participants were offered up to 20 hours of in-home uncluttering sessions (see Table S1 for flowchart), and naturalistic data was collected on number of hours used. Pairs of trained non-professional uncluttering volunteers (HW, CB, RGh, and RGi) made weekly home visits to each participant’s residence. During the in-home visits, the uncluttering volunteers and participants followed structured exercises as detailed in the Buried in Treasures workbook (Tolin et al., 2007) and the BIT facilitator’s guide (Shuer and Frost, 2014), which modeled content that participants learned during the BIT workshop. This structure included a brief check-in, guided unclutter time, and a final reflective period in which participants shared their thoughts and their objectives for the coming week. For individuals who were unable to meet their volunteers at their assigned times due to unforeseen circumstances or avoidance, sessions were rescheduled based on volunteer availability; otherwise, the session was not conducted.
Statistical Analysis
A non-parametric Wilcoxon signed-rank test was used to assess change over time in the primary outcome measure, SI-R score (Wilcoxon, 1945). In addition, we assessed median percent change on the SI-R subscales and on the secondary outcome measures (i.e., CIR and ADL-H; Table 1).
Table 1.
Change in hoarding related clinical measures and number of in-home uncluttering hours in study participants (n=5).
| In-Home Uncluttering (hours) | SI-R Total (weeks) | SI-R Clutter (weeks) | SI-R Difficulty Discarding (weeks) | SI-R Acquisition (weeks) | Clutter Image Rating (weeks) | ADL-H (weeks) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | 0 | 12 | 18 | 0 | 12 | 18 | 0 | 12 | 18 | 0 | 12 | 18 | 0 | 12 | 18 | 0 | 12 | 18 | |
| 1 | 16 | 74 | 70 | 66 | 32 | 32 | 33 | 25 | 20 | 19 | 17 | 18 | 14 | 4.0 | 4.7 | 6.3 | 1.9 | 2.0 | 1.9 |
| 2 | 13 | 71 | 64 | 58 | 30 | 29 | 26 | 24 | 24 | 20 | 17 | 11 | 12 | 4.7 | 4.7 | 3.3 | 2.6 | 2.4 | 1.9 |
| 3 | 8 | 75 | 55 | 53 | 35 | 29 | 27 | 25 | 16 | 14 | 15 | 10 | 12 | 5.0 | 3.3 | 2.7 | 1.9 | 1.6 | 1.3 |
| 4 | 20 | 67 | 45 | 37a | 31 | 24 | 14 | 23 | 17 | 14 | 13 | 4 | 9 | 4.3 | 4.7 | 2.7 | 2.1 | 2.0 | 1.5 |
| 5 | 4 | 62 | 47 | 23a | 25 | 18 | 1 | 19 | 13 | 10 | 18 | 16 | 12 | 7.0 | 2.7 | 1.0 | 4.0 | 2.4 | 1.1 |
| median | 12 | 71 | 55 | 53 | 31 | 29 | 26 | 24 | 17 | 14 | 17 | 11 | 12 | 4.7 | 4.7 | 2.7 | 2.1 | 2.0 | 1.5 |
| min | 4 | 62 | 45 | 23 | 25 | 18 | 1 | 19 | 13 | 10 | 13 | 4 | 9 | 4.0 | 2.7 | 1.0 | 1.9 | 1.6 | 1.1 |
| max | 20 | 75 | 70 | 66 | 35 | 32 | 33 | 25 | 24 | 20 | 18 | 18 | 14 | 7.0 | 4.7 | 6.3 | 4.0 | 2.4 | 1.9 |
ADL-H = Activities Daily Living for Hoarding; CIR = Clutter Image Rating; SI-R = Savings Inventory-Revised.
Bold (and blue highlight) = Three out of five participants (number 3, 4, and 5) had a 14 point or greater SI-R reduction from pre- to post-treatment.
Two out of five patients (number 4 and 5) met clinically significant change criteria (i.e., a 14 point or greater reduction from pre- to post-treatment and a post-treatment score of 42 or less on SI-R).
Results
All five participants completed the workshop and the baseline, 12-week, and 18-week assessments. Four of five participants received between 8 and 20 in-home uncluttering hours. One participant declined further assistance after 4 hours, reporting no longer having clutter that impaired her living conditions (confirmed by both in-home volunteers and assessment scales).
Baseline median SI-R score was 71 (range = 62–75), comparable to earlier BIT studies (Frost et al., 2011, 2012). All participants reported hoarding symptom reduction (i.e., lower SI-R score) at 18 weeks compared to baseline, with median 29% reduction (22 points; range = 10–62%; z = −2.02, p = 0.043; Figure 1 and Table 2). At 12 weeks, median SI-R score was 55 (range = 45 – 70). At 18 weeks, median SI-R score was 53 (range = 23–66; Table 1). The majority of SI-R percent reduction occurred from the first to 12th week (median = 24% reduction; range 5–33%; z = −2.02, p = .043). SI-R scores also decreased in all participants from 12 to 18 weeks (median = 9% reduction; range = 4–51%; z = −2.02, p = .043; Figure 1). Three out of five participants had a 14 point or greater SI-R reduction from pre- to post-treatment. Two out of five patients met clinically significant change criteria (i.e., a 14 point or greater reduction from pre- to post-treatment and a post-treatment SI-R score of 42 or less).
Figure 1:
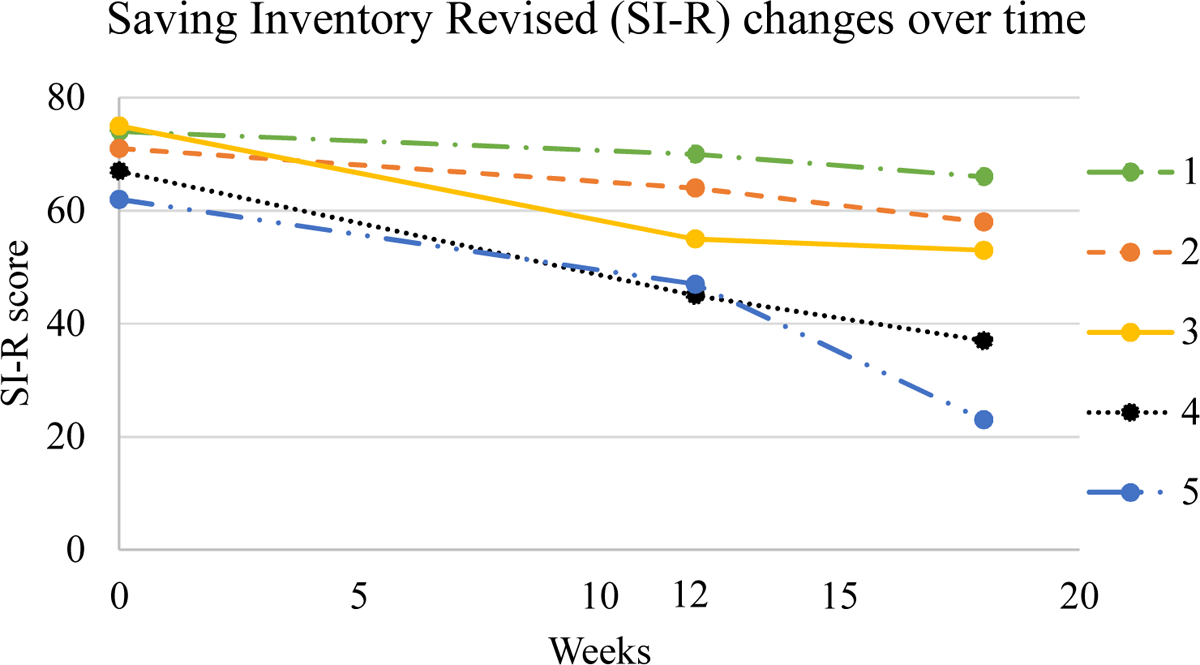
Individual trajectories of participants hoarding severity as measured by the SI-R total score change from baseline to 18 Weeks
Table 2.
Change in hoarding related clinical measures in current sample and previous HD treatment studies led by non-professional facilitators using Buried in Treasures Workshop. Parentheses represent percent change.
| Study | Clinical Measures Score Change Pre- to Post- Treatment | ||
|---|---|---|---|
| SI-R | CIR | ADL-H | |
| Current sample | 22 (29%) | 1.67 (38%) | .67 (31%) |
| Frost et al., 2011; Study 1 | 15 (23%) | 0.9 (20%) | 0.5 (22%) |
| Frost et al., 2011; Study 2 | 12 (21%) | 1 (24%) | 0.3 (18%) |
| Frost et al., 2012 | 15 (24%) | 0.45 (13%) | 0.26 (14%) |
| Mathews et al., 2016 | 14.4* (22.6%) | NA | NA |
SI-R = Saving Inventory Revised; CIR = Clutter Image Rating; ADL-H = Activities of Daily Living for Hoarding.
Represents weighted mean and percent change across HD treatment studies in this meta-analysis that includes several studies led by non-professional facilitators using Buried in Treasures Workshop.
We also explored the effects of in-home uncluttering on symptom dimensions by examining changes in SI-R’s three subscales (i.e., clutter, difficulty discarding, and excessive acquisition) from week 12 to 18. During this in-home uncluttering period, discarding and clutter scores improved in more participants (N = 5, N = 4, respectively) than did excessive acquisition scores (N = 2). Indeed, the median change in difficulty discarding scores was a reduction (improvement) of 17%; participants’ changes ranged from 5% to 23% decrease. On the clutter subscale, median change was a 10% reduction; participants’ changes ranged from a 94% reduction (from a score of 18 at 12 weeks to 1 at 18 weeks) to 3% increase. On the excessive acquisition scale, the median percent change from 12 to 18 weeks was an increase (worsening) of 9%, which was driven by one client with a large increase in acquisition (125%) after the death of a family member during the study period.
Four out of five participants experienced clutter reduction (i.e., lower CIR score) at 18 weeks compared to baseline, with median 2-point reduction (Table 1). At baseline, median CIR score was 4.7 (range = 4.0–7.0). At 12 weeks, median CIR score was also 4.7 (range = 2.7 – 4.7). At 18 weeks, median CIR score was 2.7 (range = 1.0–6.3; Table 1). This decrease was more pronounced between weeks 12 to 18 (median change = 29%) compared to the first half of BIT, where the median percent change from baseline to 12 weeks was zero. Of note, two of five participants did not have any improvement between week 0 and 12, and yet had decrease between week 12 and 18.
The ADL-H corroborated the positive effects of in-home uncluttering, as all five participants reported improved daily functioning. At baseline, median ADL-H score was 2.1 (range = 1.9–4.0). At 12 weeks, median ADL-H score was again 2.0 (range = 1.6 – 2.4). At 18 weeks, median ADL-H score was 1.5 (range = 1.1–1.9; Table 1).
Participants described their experience in BIT group sessions as overall positive: (a) “enjoyable – I feel safe” (b) “group is going great – it’s helpful to talk to others who ‘get it’ and understand what I’m going through” (c)“[facilitators CL and DS] are compassionate, kind, [had] good eye-contact and [were] non-judgmental.” (d) “the group is helpful” (e) “I had spent a lot of time thinking my problem was because I was lazy and not focusing on the emotional part, and now I feel ready to tackle it.”
With regard to in-home uncluttering, participants expressed appreciation for the “company and support” through the “overwhelming challenge of getting started.” Many verbalized throughout the process that simply the presence of a “support person,” or “another set of eyes” to hold them “accountable” was “an immense help” to the challenge of uncluttering. All participants described the difficulty starting uncluttering (initial sessions): (a) “[I’m] reluctant to start… [I can] only do tiny time segments” (b) “I feel frustrated about the progress…angry and overwhelmed” (c) “I felt awful all day because I didn’t do what I committed to do” (d) “I spent more time thinking about everything I had to do rather than taking action” (e) “I felt frozen…I thought a lot about the item and when on thinking about it.” Through the course of the home visits, the language became increasingly positive for some participants (later sessions): (a) “it was painful at first, but became bearable after a while” (b) “lots more to do, but feel like real progress” (c) “my success this week has been maintaining the uncluttering” (d) “still felt resistant…it was more comfortable to avoid all thought and “numb out” on TV and internet.” (e) “felt I am doing ok, but still seems so far to go…[I] organized paper bags – kept many, but all fit in one large container…I am feeling relieved.” At the end of the in-home uncluttering, some participants felt like they did not accomplish enough: “I felt grateful for the study, but it was not enough time.”
In-home uncluttering volunteers described positive experiences working with clients in the home: “I found the experience to be bonding, as through the process of sorting items, participants invariably opened up about significant events in their lives—joys, losses, milestones and accomplishments,” and “participants told stories through items or mementos to both showcase who they were before their lives became dominated by hoarding, and to reconnect with chapters of their lives they felt proud of.” The uncluttering volunteers also noted the variability in participant engagement in uncluttering in-between home sessions, ranging from “the initial one or two uncluttering sessions for this participant increased her motivation for uncluttering, and made her more hopeful/optimistic that she could unclutter and maintain her living areas on her own” to “we would begin to make progress towards uncluttering goals during in-home sessions, but specifically one participant had difficulty continuing to unclutter on their own (and/or would acquire more in-between sessions).” Challenges reported by unclutter volunteers included that “for those who did not make significant progress during or between sessions, I believe this made them less motivated and hopeful that they could unclutter their space.” Impactful aspects of the home experience included: “helping participants navigate what to discard/whether or not to discard items, challenging negative cognitions related to participants’ beliefs about the importance or relevance of clutter during the sessions (this also helped decrease anxiety during sessions once items were discarded), and support/positive reinforcement for participants as they uncluttered their space during and in-between sessions.”
Discussion
We conducted an open-label pilot study to assess the feasibility of augmenting the evidence-based BIT workshop with up to 20 hours of in-home uncluttering sessions in adults with hoarding disorder. There were four main findings. (1) Participants showed improvement in overall hoarding symptoms from baseline to study end. (2) The in-home unclutter component (week 12 to week 18) improved overall clutter level in the home and may have benefited some individuals who might not have otherwise had clutter level reduction. (3) Participants reported improvement in activities of daily living. (4) Procedures were feasible and well tolerated by study participants. This is the first study to report findings of in-home unclutter sessions added to the BIT workshop. Findings support earlier work (Frost et al., 2012a, 2011) on BIT workshop effectiveness and raise the possibility that in-home visits may augment BIT workshop hoarding outcomes including clutter level.
The reductions in hoarding symptoms, median SI-R score decrease of 22 points (29%) over 18 weeks, is consistent with earlier studies of the BIT workshop (Table 2). The results are also consonant with a review of prior BIT workshop treatment studies that reported a weighted mean SI-R score decrease of 14 points (23%) (Mathews et al., 2016).
Improvements in clutter, as measured by the CIR, compare favorably with earlier BIT workshop studies (Table 2). The CIR change from baseline to week 18 in the present study, a decrease of 2 points, was nearly double the change observed in BIT studies without in-home sessions. The largest CIR percentage decrease occurred between weeks 12 and 18, when all but one of the in-home uncluttering sessions were conducted. Of note, two of five participants did not have any improvement between week 0 and 12, and yet had decrease between week 12 and 18, suggesting in-home sessions may have benefited some individuals who might not have otherwise had clutter level reduction. Taken together with prior BIT workshop findings, our CIR data suggest that in-home uncluttering sessions contribute substantially to BIT workshop outcome in complementary ways (i.e., targeting clutter level).
Like earlier studies, the present study found improvements in the ability to carry out normal daily activities, as measured by the ADL-H. The groups’ median ADL-H score decrease is consistent with prior BIT workshop studies (Table 2).
One individual, who suffered a personal loss during the study procedures, had progressively increased acquiring behaviors atypical of this and other BIT workshop studies, suggesting acquiring may have served as a coping strategy. This case serves to highlight that in clinical practice, it is important to explore other life-stressor or comorbid conditions that may be contributing to increasing hoarding behaviors during treatment, and which may require additional targeted treatments to maximize outcomes.
That the study procedures were feasible, well-tolerated and resulted in improved activities of daily living also supports our hypothesis. All participants completed all the assessments, allowed study staff to enter their homes, and shared many positive comments about the benefits of the group treatment and the uncluttering. This is striking given that individuals who struggle with hoarding often refrain from inviting loved ones to their homes due to shame and embarrassment about the clutter.
Taken together, our results are consistent with a meta-analysis suggesting that in-home visits moderate treatment effects seen in other HD treatments (Tolin et al., 2015) and theories that increasing variability of exposure contexts may improve learning generalization (for a review see Craske et al., 2008). Our results also add to several emerging treatment options for HD (Ayers et al., 2014; Muroff et al., 2010; O’Neill et al., 2013)(Moulding et al., 2017). Supporting the intervention’s practical significance, the unclutter volunteers were not professional mental health-care providers, suggesting that health care professionals may enlist community non-professionals to increase the number of care providers.
Several limitations deserve consideration. First, this pilot study had a small sample size. Data are preliminary and should be interpreted with caution. Replication is needed. Second, given the open-label design and overlap of the in-home component with four BIT workshop sessions, the effects may be due solely to BIT workshop and its carry-over effects/benefits. Third, without a control group, it was not possible to test the benefits of home sessions alone. Fourth, we did not systematically collect data on the percentage of time and quality of uncluttering within in-home sessions.
In summary, this study preliminarily suggests that complementing evidence-based BIT workshop with in-home uncluttering sessions can facilitate treatment gains for individuals with HD. Future research must clarify the dosing and timing of an uncluttering intervention in a randomized controlled trial.
Supplementary Material
Highlights.
In-home uncluttering sessions augment evidence-based hoarding treatment (BIT)
Augmented BIT improved overall hoarding symptoms, clutter, and functioning
Study procedures were feasible and well tolerated by study participants
Acknowledgments:
The authors thank the individuals who generously donated their time to participate in this research study.
Funding support: This study was supported by the National Institutes of Mental Health K23MH092434 (Dr. Rodriguez) and Stanford Small Grants Program (Dr. Rodriguez).
Role of the sponsor: The study sponsor had no role in the design, analysis, interpretation or publication of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures: Drs. Linkovski, La Lima, Filippou-Frye, Jo, Mss. Zwerling, Cordell, Sonnenfeld, Baker, Ghazzaoui, Girson/Brooke, Sanchez, Wright, Varias, Shen and Mr. Alford, Shuer and Willis report no additional financial or other relationships relevant to the subject of this manuscript. Dr. Frost reports royalties from Oxford University Press. Dr. Rodriguez reports being a consultant for Allergan, BlackThorn Therapeutics, and Rugen Therapeutics.
Clinicaltrials.gov Registry Numbers: NCT02377986
References
- American Psychiatric Association (Ed.), 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, fifth ed. American Psychiatric Association, Washington, D.C. [Google Scholar]
- Ayers CR, Saxena S, Espejo E, Twamley EW, Granholm E, Wetherell JL, 2014. Novel treatment for geriatric hoarding disorder: an open trial of cognitive rehabilitation paired with behavior therapy. Am. J. Geriatr. Psychiatry 22, 248–252. 10.1016/j.jagp.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A, 2008. Optimizing inhibitory learning during exposure therapy. Behav. Res. Ther 46, 5–27. 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Dozier ME, Ayers CR, 2015. Validation of the clutter image rating in older adults with hoarding disorder. Int. Psychogeriatr 27, 769–776. 10.1017/S1041610214002403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Hristova V, Steketee G, Tolin DF, 2013. Activities of daily living scale in hoarding disorder. J. Obsessive-Compuls. Relat. Disord 2, 85–90. 10.1016/j.jocrd.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Pekareva-Kochergina A, Maxner S, 2011. The effectiveness of a bibliobased support group for hoarding disorder. Behav. Res. Ther 49, 628–634. 10.1016/j.brat.2011.06.010. [DOI] [PubMed] [Google Scholar]
- Frost RO, Ruby D, Shuer LJ, 2012a. The buried in Treasures workshop: waitlist control trial of facilitated support groups for hoarding. Behav. Res. Ther 50, 661–667. 10.1016/j.brat.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Grisham J, 2004. Measurement of compulsive hoarding: saving inventory-revised. Behav. Res. Ther 42, 1163–1182. 10.1016/j.brat.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Tolin DF, 2012b. Diagnosis and assessment of hoarding disorder. Annu. Rev. Clin. Psychol 8, 219–242. 10.1146/annurevclinpsy-032511-143116. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Tolin DF, Renaud S, 2008. Development and validation of the clutter image rating. J. Psychopathol. Behav. Assess 30, 193–203. 10.1007/s10862-007-9068-7. [DOI] [Google Scholar]
- Gilliam CM, Norberg MM, Villavicencio A, Morrison S, Hannan SE, Tolin DF, 2011. Group cognitive-behavioral therapy for hoarding disorder: an open trial. [Clinical Trial]. Behav. Res. Ther 49 (11), 802–807. 10.1016/j.brat.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23(1), 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews CA, Uhm S, Chan J, Gause M, Franklin J, Plumadore J, Stark SJ, Yu W, Vigil O, Salazar M, Delucchi KL, Vega E, 2016. Treating hoarding disorder in a real-world setting: results from the mental health association of san Francisco. Psychiatr. Res 237, 331–338. 10.1016/j.psychres.2016.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulding R, Nedeljkovic M, Kyrios M, Osborne D, Morgan C, 2017. Short-term cognitive-behavioural group treatment for hoarding disorder: a naturalistic treatment outcome study. Clin. Psychol. Psychother 24, 235–244. [DOI] [PubMed] [Google Scholar]
- Muroff J, Steketee G, Himle J, Frost R, 2010. Delivery of internet treatment for compulsive hoarding (D.I.T.C.H.). Behav. Res. Ther 48, 79–85. 10.1016/j.brat.2009.09.006. [DOI] [PubMed] [Google Scholar]
- Nordsletten AE, Reichenberg A, Hatch SL, Cruz LF de la, Pertusa A, Hotopf M, Mataix-Cols D, 2013. Epidemiology of hoarding disorder. Br. J. Psychiatry 203, 445–452. 10.1192/bjp.bp.113.130195. [DOI] [PubMed] [Google Scholar]
- O’Neill J, Gorbis E, Feusner JD, Yip JC, Chang S, Maidment KM, Levitt JG, Salamon N, Ringman JM, Saxena S, 2013. Effects of intensive cognitive-behavioral therapy on cingulate neurochemistry in obsessive–compulsive disorder. J. Psychiatr. Res 47, 494–504. 10.1016/j.jpsychires.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ, 2011. The Columbia–suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 168, 1266–1277. 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez CI, Levinson A, Patel SR, Rottier K, Zwerling J, Essock S, Shuer L, Frost RO, Simpson HB, 2016. Acceptability of treatments and services for individuals with hoarding behaviors. J. Obsessive-Compuls. Relat. Disord 11, 1–8. 10.1016/j.jocrd.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuer L, Frost RO, 2014. Leading the Buried in Treasures Workshop: Facilitators Guide.
- Steketee G, Frost RO, Tolin DF, Rasmussen J, Brown TA, 2010. Waitlist-controlled trial of cognitive behavior therapy for hoarding disorder. Depress. Anxiety 27, 476–484. 10.1002/da.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timpano KR, Exner C, Glaesmer H, Rief W, Keshaviah A, Brähler E, Wilhelm S, 2011. The epidemiology of the proposed DSM-5 hoarding disorder: exploration of the acquisition specifier, associated features, and distress. J. Clin. Psychiatr 72, 780–786. 10.4088/JCP.10m06380. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, 2007a. Buried in Treasures: Help for Compulsive Acquiring, Saving, and Hoarding, first ed. Oxford University Press, New York. [Google Scholar]
- Tolin DF, Frost RO, Steketee G, 2007b. An open trial of cognitive-behavioral therapy for compulsive hoarding. Behav. Res. Ther 45, 1461–1470. 10.1016/j.brat.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, 2010. A brief interview for assessing compulsive hoarding: the Hoarding Rating Scale-Interview. Psychiatr. Res 178 (1), 147–152 doi: S0165-1781(09)00178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Muroff J, 2015. Cognitive behavioral therapy for hoarding disorder: a meta-analysis. Depress. Anxiety 32, 158–166. 10.1002/da.22327. [DOI] [PubMed] [Google Scholar]
- Wilcoxon Frank, 1945. Individual comparisons by ranking methods. Biom. Bull 1 (6), 80–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


