Abstract
Recovery high schools are one form of continuing care support for adolescents with substance use or other co-occurring disorders. Using a controlled quasi-experimental design, we compared mental health symptom outcomes at 6 months for adolescents who attended recovery high schools vs. non-recovery high schools (e.g., traditional or alternative schools). The propensity score balanced sample included 194 adolescents (134 in recovery schools, 60 in non-recovery schools) enrolled in schools in MN, WI, or TX (average age = 16; 86% White; 51% female). Baseline data indicated that this is a dually diagnosed population—94% of students met criteria for at least one mental health diagnosis and 90% had received mental health treatment distinct from treatment for substance use disorders. Results from multilevel logistic regression models indicated that at the 6-month follow-up, adolescents attending both recovery and non-recovery high schools reported substantial improvements in mental health symptoms. However, there were no significant differences in mental health outcomes between the two groups. We conclude that although recovery high schools offer promise for reducing substance use and improving academic success, and while adolescents’ mental health symptoms improved between baseline and follow-up, recovery high schools may have minimal differential effects on adolescents’ mental health symptoms.
Keywords: Adolescents, Mental health, Recovery high schools, Substance use
Schools are influential social environments in the lives of adolescents, particularly for students struggling with substance use problems. Peer pressure, association with substance-using peers, and (perceived) availability of substances are some of the strongest risk factors for adolescent substance use, all of which are deeply embedded within school contexts (Derzon 2007; Mason et al. 2014; Svensson 2000; Wambeam et al. 2013). Indeed, a national survey of US high school students estimates that in 2013, 22% of students were offered, sold, or given an illegal drug on school property (Zhang et al. 2016). Adolescents who return to school after receiving substance use treatment thus face a range of unique risk factors embedded within the school environment (Spear and Skala 1995). Most high school settings may therefore be “recovery hostile” in the sense that they fail to provide the social and therapeutic supports needed by students in recovery from substance use disorders.
In response, recovery high schools have been developed as an alternative high school option for adolescents with substance use disorders (National Institute on Drug Abuse (NIDA) 2014; Office of National Drug Control Policy (ONDCP) 2014). These schools aim to foster adolescents’ recovery from substance use by providing a safe and supportive learning environment that promotes sobriety along with academic success (Finch and Frieden 2014; Finch et al. 2014). Recovery high schools may be free of charge for students or provide tuition scholarships, but they all meet state requirements for awarding secondary school diplomas (Association of Recovery High Schools 2016). In addition to meeting the academic needs of students in recovery from substance use, recovery schools also include therapeutic programming designed to address individual substance use and mental health issues and to foster strong peer and family support structures. This might include, for instance, daily group check-ins, community service requirements, or individual or group counseling sessions (Moberg and Finch 2007). Recovery high schools thus provide continuing care support for adolescents subsequent to formal substance use treatment, and seek to improve academic and behavioral adjustment by fostering social connectedness and social capital.
Despite the intuitive appeal of recovery high schools as a continuing care support for students with substance use disorders, to date there has been limited empirical research examining the effects of recovery high school attendance on students’ academic and behavioral outcomes. Prior research suggests that students attending recovery high schools have high levels of perceived peer support (Karakos 2014), and that recovery school attendance may yield modest improvements in students’ academic performance as well as reductions in substance use (Finch et al. 2014; Finch et al. 2017; Kochanek 2008; Moberg and Finch 2007; Moberg et al. 2014). However, no studies to date have examined whether recovery high school attendance may improve students’ mental health symptoms.
National research suggests that approximately 67% of adolescents have experienced at least one mental health disorder prior to the onset of alcohol or drug abuse (Conway et al. 2016). Research with clinical populations has demonstrated the high prevalence of mental health comorbidities in adolescents with substance use disorders, with substance dependent youth being highly likely to meet diagnostic criteria for multiple mental health disorders (Chan et al. 2008; Dennis et al. 2004; Norberg et al. 2012). Given the high rates of co-occurring mental health disorders among adolescents with substance use disorders (Armstrong and Costello 2002; Conway et al. 2016), and the disease burden associated with these co-occurring disorders (Whiteford et al. 2013), it is important to understand whether recovery high schools reduce not only substance use but also mental health problems.
This study reports findings from a controlled quasi-experimental study examining the effects of recovery high school attendance on students’ academic and behavioral adjustment. Findings from this study (Finch et al. 2017) indicated that recovery high schools led to reductions in substance use and improvements in school attendance at 6 months. The current manuscript presents findings for students’ mental health outcomes. To our knowledge, this study is the first to use a rigorous longitudinal quasi-experimental design to examine the effects of recovery high school attendance on adolescents’ mental health symptoms.
We hypothesized that students attending recovery high schools would exhibit significantly better mental health symptoms than similar students attending non-recovery high schools, due to the additional school-based therapeutic support available to recovery high school students. Most recovery high schools have dedicated counselors located on site at the schools. However, most therapeutic staff employed full-time by recovery high schools have substance use-specific counseling certifications rather than clinical mental health licenses (Moberg et al. 2014). Recovery high schools may also employ mental health staff who periodically visits the school to hold counseling sessions, and/or refer students to community mental health agencies for additional counseling support (Finch et al. 2014). Although traditional (non-recovery focused) high schools may also offer some of these therapeutic services, many such schools report significant barriers or challenges for addressing students’ mental health needs (Foster et al. 2005; Teich et al. 2008).
Methods
Participants
This study used a quasi-experimental design to compare mental health outcomes for adolescents who received some formal substance use treatment and subsequently enrolled in a recovery high school (the intervention group) or subsequently enrolled in a non-recovery high school, such as a traditional school or other type of non-recovery alternative school (the comparison group). Adolescents and their families were recruited upon discharge from 10 substance use treatment facilities in MN, WI, or TX (baseline data collection period); these sites were selected because several recovery high schools were known to be in operation nearby at the time of study recruitment. Students in the intervention and comparison groups were recruited from the same treatment programs. After discharge from treatment, families were free to enroll adolescents in any type of formal schooling; some elected to enroll in recovery high schools and others enrolled in non-recovery oriented high schools. This recruitment strategy yielded a smaller number of recovery high school enrollees than expected, so after the first year of recruitment we also began recruiting adolescents who were newly enrolled in recovery high schools and had recently (within the past 12 months) been discharged from a substance use treatment program. This supplemental recruitment strategy served to increase the sample size for the intervention group only (i.e., no comparison group participants were recruited in this manner).
Participants were followed longitudinally after discharge at 3-month, 6-month, and 12-month follow-up periods. Study data were collected between 2011 and 2016, and the Institutional Review Board at the University of Minnesota approved all data collection procedures. Student assent and parent consent were secured for all research participants. All participants received Target gift cards at each assessment period to incentivize study participation.
The current paper uses data from the baseline and 6-month follow-up responses from adolescents enrolled in the study between December 2011 and May 2016 (12-month follow-up data are being analyzed and will be reported in later manuscripts). A total of 293 adolescents enrolled in the study; 229 completed 6-month follow-ups (78% retention).
Materials and Measures
Extensive youth assessments were conducted at baseline, 3-month, and 6-month follow-ups. Standardized assessments were collected in-person using computer assisted interviewing by a team of trained, primarily master’s level data collectors.
For this study, we examined adolescents’ self-reported mental health symptoms, collected using the M.I.N.I. Structured Clinical Interview (M.I.N.I.-SCID)—a brief structured diagnostic interview for major Axis I psychiatric disorders in DSM-IVand ICD-10 (Sheehan et al. 1999). Using the M.I.N.I.-SCID scoring criteria, we assessed whether students met criteria for major depressive disorder, generalized anxiety disorder, obsessive compulsive disorder, panic disorder, posttraumatic stress disorder, antisocial personality disorder, manic episode, hypomanic episode, and any current suicide risk (i.e., scoring as medium or high risk on the M.I.N.I.-SCID). At baseline, the assessment captured symptoms in the 12 months prior to substance use treatment; at 6-month follow-up, the assessment captured mental health symptoms in the past 6-months since baseline data collection.
Recovery high school attendance was measured using information collected at the baseline, 3-month, and 6-month follow-ups, based on students’ self-reports of the school(s) they attended during the study period. Students who enrolled in a recovery high school for at least 28 calendar days (i.e., approximately 1 month in school) during the period between baseline and the 6-month follow-up were considered the intervention group; all other students were included in the comparison group. This operationalization of the intervention and comparison conditions was intended to capture the effects of at least 1 month of recovery high school attendance. In the final propensity score balanced sample, among the 134 students in the intervention condition, 83 were still enrolled at a recovery high school at the 6-month follow-up (days attending the recovery high school mean = 296.78, SD = 213.26; the high mean is due to recovery high school enrollment prior to the research baseline interview for a number of these students). Among the 60 students in the comparison condition, only two of those students had ever attended a recovery high school (days attending the recovery high school mean = 5.50, SD = 4.95).
We collected data on a range of other adolescent characteristics (e.g., family functioning, substance use history, mental health treatment history, crime, and delinquency), which were used in the propensity score models used to balance the intervention and comparison conditions (see Finch et al. 2017 and Tanner-Smith and Lipsey 2014 for more details on the propensity score models).
Analytic Strategies
Because adolescents self-selected into the intervention and comparison conditions, we used propensity scores to address potential baseline non-equivalence between the two conditions (Guo and Fraser 2010; Imbens and Rubin 2015; Tanner-Smith and Lipsey 2014). Due to survey nonresponse, there was a small amount of missing data on the covariates used in the propensity score estimation model. We used multiple imputation (Graham 2009; Schafer and Graham 2002) to handle this missing data on the baseline covariates. We created 20 imputed datasets based on all key variables of interest, and then pooled values across the 20 imputed datasets to yield a single dataset with complete baseline data for all cases.
Propensity scores were estimated as the predicted probability of attending a recovery high school. Predicted recovery high school attendance was estimated with multilevel logistic regression models that included baseline values of all outcome variables and a range of covariate controls measuring students’ demographic, academic, behavioral, and emotional adjustment. The linearized propensity score, and the square of this propensity score, were then used as covariate controls in the final outcome models. Thirty-five participants (all in the comparison condition) were outside the propensity score region of common support, and were dropped from the final analysis model. The final analytic sample included 194 participants who were well balanced on the estimated propensity score and thus well balanced at baseline (134 in recovery schools; 60 in non-recovery schools).
We used multilevel logistic regression models to examine the effects of recovery high school attendance on adolescents’ mental health symptoms. Models were estimated separately for each of the nine mental health outcomes; all models statistically controlled for baseline values of the outcome variable, the linearized propensity score, and the squared propensity score. To account for clustering of adolescents within schools, multilevel models that included random intercepts for schools were estimated. We also included fixed-effects for recruitment sites to account for clustering within study recruitment sites.
Results
Table 1 presents descriptive statistics for the baseline characteristics of the propensity score balanced sample. On average, participants were age 16 and enrolled in 11th grade. The sample was split evenly by gender, and was predominantly White (86%). Participants reported high levels of substance use at baseline, reporting 19 days of alcohol use, 55 days of marijuana use, and 30 days of other substance use in the past 90 days. Along with formal substance use treatment, most participants (90%) reported having received some type of mental health treatment; most (88%) had previously received a prescription for a psychiatric medication; the average age at first mental health treatment was 11.24 (SD = 3.60). Notably, this sample of youth with substance use disorders had high rates of symptoms of multiple mental health disorders at baseline: 80% met criteria for major depressive disorder, 64% met criteria for generalized anxiety disorder, 44% were at risk of suicide, and 45% met criteria for antisocial personality disorders. Almost all (94%) met the criteria for at least one of the nine disorders.
Table 1.
Baseline sample characteristics—propensity score balanced sample
| Recovery high school (n = 134) | Non-recovery high school (n = 60) | Total sample (n = 194) | |||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Range | ||||
| Student background | |||||||
| Age | 16.49 | (1.01) | 16.25 | (1.00) | 16.41 | (1.01) | 14–19 |
| Grade in school | 11.09 | (0.91) | 11.00 | (0.96) | 11.06 | (0.92) | 9–12 |
| Male (%) | 50.00 | 51.67 | 50.51 | 0–100 | |||
| White (%) | 85.07 | 86.67 | 85.57 | 0–100 | |||
| African-American (%) | 7.46 | 6.67 | 7.22 | 0–100 | |||
| Other race (%) | 7.47 | 6.66 | 7.21 | 0–100 | |||
| Days used alcohol (past 90) | 19.26 | (25.50) | 17.65 | (24.32) | 18.76 | (25.09) | 0–91 |
| Days used marijuana (past 90) | 53.58 | (35.57) | 57.20 | (34.38) | 54.70 | (35.16) | 0–91 |
| Days used other drugs (past 90) | 34.16 | (36.86) | 20.88 | (29.47) | 30.05 | (35.21) | 0–91 |
| Ever received mental health treatment (%) | 91.13 | 85.96 | 89.50 | 0–100 | |||
| Age at first mental health treatment | 11.37 | (3.58) | 10.96 | (3.68) | 11.24 | (3.60) | 2–18 |
| Ever received psychiatric medication (%) | 88.33 | 86.79 | 87.86 | 0–100 | |||
| Days of mental health services received (past 90) | 50.14 | (58.47) | 49.78 | (60.69) | 50.03 | (59.01) | 0–268 |
| Mental health symptoms (% lifetime) | |||||||
| Any of the nine symptoms | 95.52 | 90.00 | 93.81 | 0–100 | |||
| Major depressive disorder | 82.09 | 75.00 | 79.90 | 0–100 | |||
| Generalized anxiety disorder | 64.93 | 63.33 | 64.43 | 0–100 | |||
| Obsessive-compulsive disorder | 12.69 | 11.67 | 12.37 | 0–100 | |||
| Panic disorder | 35.82 | 43.33 | 38.14 | 0–100 | |||
| Posttraumatic stress disorder | 35.82 | 21.67 | 31.44 | 0–100 | |||
| Antisocial personality disorder | 49.25 | 35.00 | 44.85 | 0–100 | |||
| Manic episode | 15.67 | 20.00 | 17.01 | 0–100 | |||
| Hyponranic episode | 18.66 | 21.67 | 19.59 | 0–100 | |||
| Suicide risk | 47.01 | 38.33 | 44.33 | 0–100 | |||
Means and standard deviations (SDs) are for unadjusted baseline data
Figure 1 displays the proportion of participants who met criteria for mental health diagnoses at baseline and at 6-month follow-up, shown separately for the recovery high school and non-recovery high school students. All 6-month follow-up proportions were estimated using predicted probabilities from the multilevel logistic regression models, which adjusted for the baseline values of the outcomes, the estimated propensity scores, and included school random-effects and recruitment site fixed-effects.
Fig. 1.
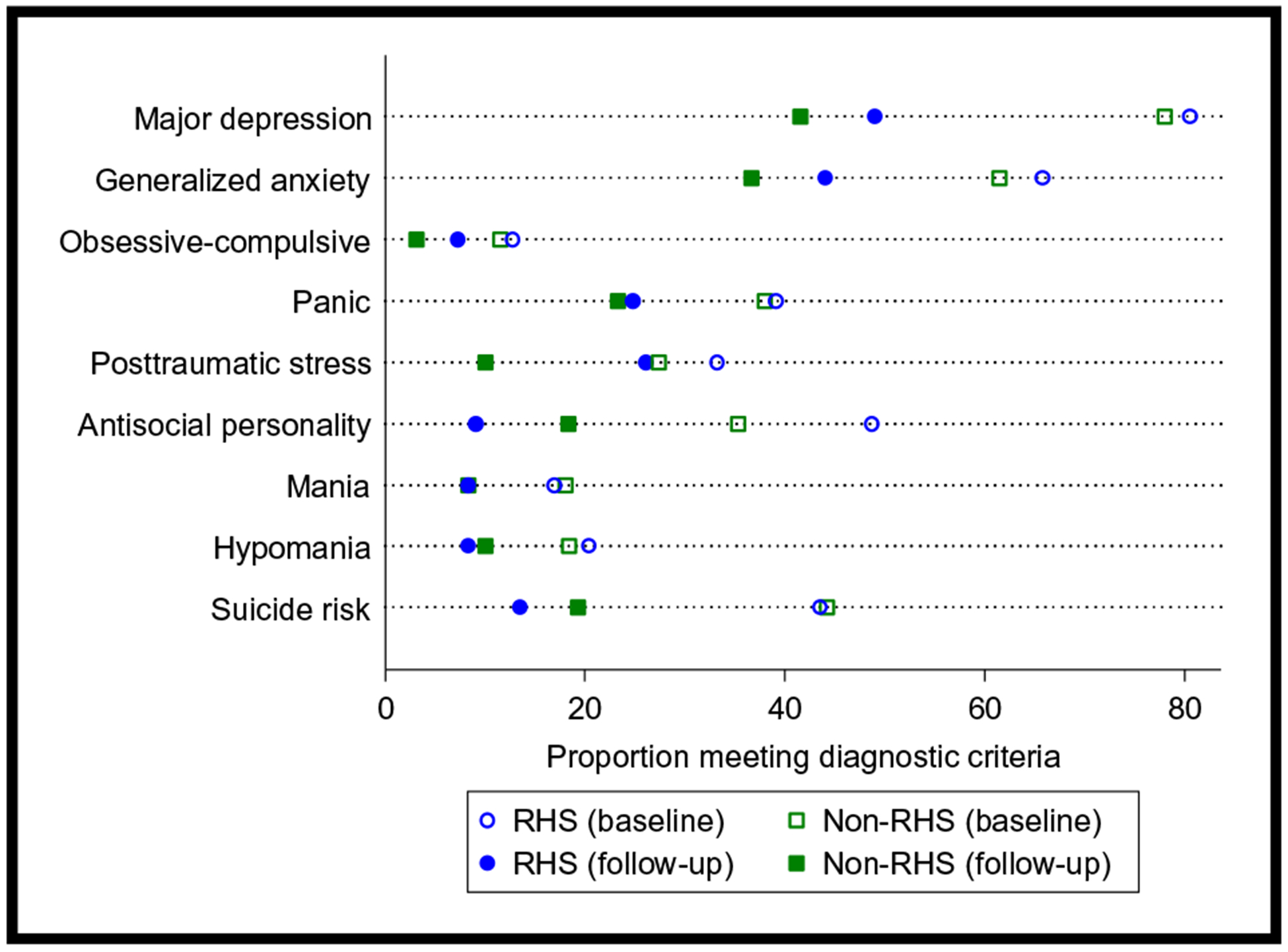
Changes in mental health symptoms after substance use treatment, by recovery high school (RHS) attendance status; all follow-up estimates adjusted for propensity scores, school, recruitment site, and baseline values
As shown in Fig. 1, students in both conditions reported substantially less mental health symptomatology at follow-up than they did at baseline. For example, although 82% of the recovery high school sample experienced symptoms of major depression at baseline, only 49% were experiencing these symptoms at the 6-month follow-up. After adjusting for baseline mental health symptoms and the propensity scores, there were no statistically significant differences in the odds of mental health symptoms at follow-up for the recovery high school students relative to non-recovery high school students. Thus in both groups, symptoms had decreased at a similar magnitude.
For instance, although recovery high school students reported lower rates of anti-social personality disorder (9 vs. 18%), hypomanic episodes (8 vs. 10%), and suicide risk (14 vs. 19%) than non-recovery high school students, these differences were not statistically significant in the adjusted models. Recovery high school students also reported higher levels of symptomatology on major depression (49 vs. 42%), generalized anxiety disorder (44 vs. 37%), obsessive compulsive disorder (7 vs. 3%), panic disorder (25 vs. 23%), and post-traumatic stress disorder (26 vs. 10%) than non-recovery high school students; but again, none of these differences were statistically significant in the adjusted logistic regression models.
Discussion
This study examined whether adolescents with substance use disorders who attend recovery high schools have improved mental health outcomes, compared to similar adolescents who attend traditional (non-recovery-oriented) high schools. We used a quasi-experimental design with propensity scores to compare mental health outcomes for 134 adolescents attending recovery high schools and 60 similar adolescents attending non-recovery high schools. At baseline, this sample of youth mirrored other previous substance use disorder research demonstrating high rates of co-occurring psychiatric mental health diagnoses (Chan et al. 2008; Dennis et al. 2004). Participants in this sample demonstrated even higher prevalence estimates for individual diagnoses compared to other similar samples (Tanner-Smith et al., in review). The primary lifetime prevalence in this sample included major depressive disorder (80%), generalized anxiety disorder (64%), risk of suicide (44%), and antisocial personality disorders (45%). Adolescents in both study conditions reported substantial decreases in mental health problems between baseline and six-month follow-up. This overall decrease in symptomatology may be partially a result of ongoing care received by both groups of adolescents outside of school settings, as well as the impact of prior treatment experiences, social support, regression to the mean, and possibly maturation. There was no evidence that adolescents attending recovery high schools had significantly better or worse mental health outcomes relative to students attending traditional or other alternative high schools. Thus, we can conclude that recovery high schools do not appear to have any harmful effects on students’ mental health, but there is also no evidence that recovery high schools are any more or less effective in affecting mental health relative to other high school environments.
Although the results from this study provided no evidence that recovery high school attendance had significant beneficial or harmful effects on students’ mental health outcomes when compared to non-recovery high school students, the study findings should nonetheless be useful for treatment providers, educators, and researchers working with adolescents in recovery. Indeed, the adolescents in this sample exhibited both high rates of substance use and mental health problems. Thus, providers who are developing and implementing substance use continuing care programs (such as recovery high schools) will need to attend to these comorbidities. Recovery high schools, for instance, may want to consider hiring staff with training and certifications in mental health as well as substance use issues, particularly given that many staff employed full-time by recovery high schools may only have substance use counseling certifications (Moberg et al. 2014). Recovery high schools may also want to increase mental health counseling services and opportunities for students to access these services, in efforts to provide more integrated and holistic continuing care services to address the complex sets of issues faced by these adolescent clients (Butler et al. 2008).
To our knowledge, this is the first study to use a rigorous quasi-experimental design to examine the effects of recovery high school attendance on adolescents’ mental health outcomes; thus, this study contributes to the small but growing literature examining the effectiveness of recovery high schools as a form of continuing care support for adolescents. Nevertheless, this study has several limitations. First, because it was not feasible to allocate students randomly to recovery or non-recovery high schools, we used a controlled quasi-experimental design to compare outcomes for students who self-selected into the intervention and comparison conditions. Although this design has a risk of selection bias due to non-random allocation to conditions, we addressed this limitation by using a propensity score procedure to balance the two groups on a wide range of baseline characteristics. Additional high quality experimental and quasi-experimental trials will be needed to attempt to replicate these findings. Second, the small sample size in this study limited our power to detect statistically significant effects. Although the propensity score balancing procedure reduced our final analytic sample size, this reduction in sample size was necessary for ensuring the baseline equivalence and balance of the intervention and comparison conditions. Future studies with larger sample sizes will be needed to attempt to replicate these findings. We did not take into account the influence of ongoing or relapsing substance use on mental health outcomes in this analysis, another important interaction to examine in future research. Finally, we only examined outcomes for a relatively short-term follow-up at 6-months; additional research will be needed to examine whether similar patterns will persist at longer-term follow-ups. Despite these limitations, the current study suggests that although recovery high schools offer promise as an effective continuing care support for adolescents in terms of reducing their substance use, these schools may have minimal spillover effects on students’ mental health symptoms.
Funding Information
This work was supported by Award Number R01DA029785 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Footnotes
Conflict of Interest ETS and EAH declare that they have no conflicts of interest. AJF declares that he is a non-voting unpaid board member for the Association of Recovery Schools, but he will receive no financial benefit from the findings published in this article. DPM declares that he is a board member for a private nonprofit recovery high school, with no financial interests or remuneration.
Statement of Human Rights All procedures followed were in accordance with the ethical standards of the University of Minnesota Institutional Review Board and with the Helsinki Declaration of 1975, as revised in 2000.
Informed Consent Parental informed consent and individual assent was obtained from all participants included in the study.
References
- Armstrong TD, & Costello EJ (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology, 70(6), 1224 10.1037/0022-006X.70.6. [DOI] [PubMed] [Google Scholar]
- Association of Recovery High Schools. (2016). State of recovery high schools, 2016 biennial report. Denton: Association of Recovery High Schools. [Google Scholar]
- Butler M, Kane RL, McAlpine D, Kathol RG, Fu SS, Hagedorn H, & Wilt TJ (2008). Integration of mental health/substance abuse and primary care. (prepared by the Minnesota evidence-based practice center under contract no. 290-02-0009.) AHRQ publication no. 09-E003. Rockville: Agency for Healthcare Research and Quality. [Google Scholar]
- Chan Y, Dennis ML, & Funk RR (2008). Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment, 34(1), 14–24. 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Swendsen J, Husky MM, He JP, & Merikangas KR (2016). Association of lifetime mental disorders and subsequent alcohol and illicit drug use: results from the National Comorbidity Survey-Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry, 55(4), 280–288. 10.1016/j.jaac.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. (2004). The cannabis youth treatment (CYT) study: main findings from two randomized trials. Journal of Substance Abuse Treatment, 27(3), 197–213. 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Derzon JH (2007). Using correlational evidence to select youth for prevention programming. Journal of Primary Prevention, 28, 421–447. 10.1007/s10935-007-0107-7. [DOI] [PubMed] [Google Scholar]
- Finch AJ, & Frieden G (2014). The ecological and developmental role of recovery high schools. Peabody Journal of Education, 89(2), 271–287. 10.1080/0161956X.2014.897106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Moberg DP, & Krupp AL (2014). Continuing care in high schools: a descriptive study of recovery high school programs. Journal of Child & Adolescent Substance Abuse, 23(2), 116–129. 10.1080/1067828X.2012.751269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Tanner-Smith EE, Hennessy EA, & Moberg DP (2017). Recovery high schools: effect of schools supporting recovery from substance use disorders. The American Journal of Drug and Alcohol Abuse. 10.1080/00952990.2017.1354378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster S, Rollefson M, Doksum T, Noonan D, Robinson G, & Teich J (2005). School mental health services in the United States, 2002–2003. DHHS pub. no. (SMA) 05–4068. Rockville: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Graham JW (2009). Missing data analysis: making it work in the real world. Annual Review of Psychology. 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Guo S, & Fraser MW (2010). Propensity score analysis: statistical methods and applications. Thousand Oaks: Sage. [Google Scholar]
- Imbens GW, & Rubin DB (2015). Causal inference in statistics, social, and biomedical sciences. New York: Cambridge University Press. [Google Scholar]
- Karakos HL (2014). Positive peer support or negative peer influence? The role of peers among adolescents in recovery high schools. Peabody Journal of Education, 89(2), 214–228. 10.1080/0161956X.2014.897094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek TT (2008). Recovery high schools in Massachusetts: a promising, comprehensive model for adolescent substance abuse and dependence. Retrieved from http://massrecoveryhs.org/documents/RecoveryHighSchooloverview.pdf.
- Mason MJ, Mennis J, Linker J, Bares C, & Zaharakis N (2014). Peer attitudes effects on adolescent substance use: the moderating role of race and gender. Prevention Science, 15(1), 56–64. 10.1007/s11121-012-0353-7. [DOI] [PubMed] [Google Scholar]
- Moberg DP, & Finch AJ (2007). Recovery high schools: a descriptive study of school programs and students. Journal of Groups in Addiction & Recovery, 2, 128–161. 10.1080/15560350802081314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberg DP, Finch AJ, & Lindsley SM (2014). Recovery high schools: students and responsive academic and therapeutic services. Peabody Journal of Education, 89(2), 165–182. 10.1080/0161956X.2014.895645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA). (2014). Principles of adolescent substance use disorder treatment: a research-based guide. Retrieved from http://www.drugabuse.gov/sites/default/files/podata_1_17_14.pdf.
- Norberg MM, Battisti RA, Copeland J, Hermens DF, & Hickie IB (2012). Two sides of the same coin: cannabis dependence and mental health problems in help-seeking adolescent and young adult outpatients. International Journal of Mental Health and Addiction, 10(6), 818–828. 10.1007/s11469-012-9378-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of National Drug Control Policy (ONDCP). (2014). National drug control strategy. Washington, D.C.: Office of National Drug Control Policy; Retrieved from http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/ndcs_2014.pdf. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: our view of the state of the art. Psychological Methods, 7(2), 147–177. 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Janavs R, Baker R, Harnett-Sheehan K, Knapp E, & Sheehan M (1999). Mini international neuropsychiatric interview. Tampa: University of South Florida Press. [Google Scholar]
- Spear SF, & Skala SY (1995). Posttreatment services of chemically dependent adolescents In Rahdert E & Czechowicz D (Eds.), Adolescent drug abuse: clinical assessment and therapeutic interventions (NIDA research monograph 156) (pp. 341–364). Rockville: U.S. Department of Health and Human Services, National Institute on Drug Abuse. [Google Scholar]
- Svensson R (2000). Risk factors for different dimensions of adolescent drug use. Journal of Child and Adolescent Substance Abuse, 9(3), 67–90. 10.1300/J029v09n03_05. [DOI] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2014). Identifying baseline covariates for use in propensity scores: a novel approach illustrated for a non-randomized study of recovery high schools. Peabody Journal of Education, 89, 183–196. 10.1080/0161956X.2014.895647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teich JL, Robinson G, & Weist MD (2008). What kinds of mental health services do public schools in the United States provide? Advances in School Mental Health Promotion, 1, 13–22. 10.1080/1754730X.2008.9715741. [DOI] [Google Scholar]
- Wambeam RA, Canen EL, Linkenbach J, & Otto J (2013). Youth misperceptions of peer substance use norms: a hidden risk factor in state and community prevention. Prevention Science, 15(1), 75–84. 10.1007/s11121-013-0384-8. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1575–1586. https://doi.org/10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Zhang A, Musu-Gillette L, & Oudekerk BA (2016). Indicators of school crime and safety: 2015. (report no. NCES 2016–079/NCJ 249758). Washington, DC: National Center for Education Statistics, U. S. Department of Education, and Bureau of Justice Statistics, Office of Justice Programs, U. S. Department of Justice. [Google Scholar]


