Abstract
A significant concern in current coronavirus disease-2019 (COVID-19) pandemic era is delay in first medical contact in patients with ST-segment elevation myocardial infarction (STEMI), due to reluctance to visit the hospital. We report a case of delayed presentation of STEMI as ventricular septal rupture during the COVID-19 pandemic, a rare presentation in the current age of primary percutaneous coronary intervention. (Level of Difficulty: Beginner.)
Key Words: coronavirus disease-2019, COVID-19, pandemic, ST-segment elevation myocardial infarction, ventricular septal rupture
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; ECG, electrocardiogram; MI, myocardial infarction; PA, pulmonary artery; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction; TTE, transthoracic echocardiogram; VSR, ventricular septal rupture
Graphical abstract
A significant concern in current coronavirus disease 2019 (COVID-19) pandemic era is delay in first medical contact in patients with ST-segment elevation…
History of presentation
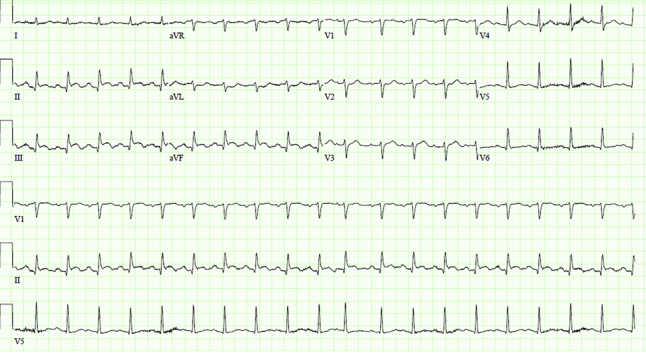
On March 14, 2020, a 65-year-old man presented to the emergency department with shortness of breath. The current symptoms started gradually 3 days before and worsened, prompting him to call the emergency medical squad. On presentation, the patient had tachycardia (heart rate of 115 beats/min), normal blood pressure of 117/90 mm Hg, tachypnea (respiratory rate of 24 breaths/min), and a temperature of 98.2°F. Physical examination revealed the patient to be in respiratory distress, and a grade 3/6 holosystolic murmur was heard over the left sternal border on chest auscultation. The electrocardiogram (ECG) revealed ST-segment elevation in leads II, III, and aVF with small Q waves (Figure 1). High-sensitivity troponin was elevated to 1,506 ng/l (normal <12 ng/l), and the patient was immediately transferred to the cardiac catheterization laboratory.
Learning Objectives
-
•
Patient-based anxiety and concerns of contracting COVID-19 in the hospital is delaying as well as decreasing the timely presentation and interventions for emergencies such as ST-segment elevation myocardial infarction.
-
•
Delayed presentations of ST-segment elevation myocardial infarction such as a ventricular septal rupture is a very rare presenting encounter, but in the current era of the COVID-19 pandemic, the incidence of this catastrophic complication as a delayed presenting complaint may increase.
Figure 1.
Electrocardiogram on Presentation
The electrocardiogram on presentation shows ST-segment elevation in leads II, III, and aVF with small Q waves.
Past Medical History
Past medical history was significant for a 60-pack-year history of cigarette smoking. He had not seen a physician for many years and had no prior cardiac evaluation. The patient recalled an episode of severe left-sided chest pain while performing push-ups 7 days before admission, which resolved after he stopped. He was reluctant to visit the hospital and getting exposed to the ongoing viral pandemic, hence stayed at home, and the pain abated on its own. Family history was also remarkable for heart disease in both parents in their 50s.
Differential diagnosis
Differential diagnosis incudes ST-segment elevation myocardial infarction (STEMI), takotsubo cardiomyopathy, acute pericarditis/myocarditis, hyperkalemia, pulmonary embolism, and Prinzmetal’s angina.
Investigations
Repeat ECG revealed persistence of ST-segment elevation with Q waves in leads II, III, and aVF. Complete blood count and basic metabolic panel were unremarkable. N-terminal pro-B-type natriuretic peptide was elevated to 3,231 pg/ml (normal <125 pg/ml). Creatine kinase and creatine kinase-myocardial band fractions were within normal limits, and troponin T was elevated to 1.2 ng/ml (normal 0 to 0.029 ng/ml) and trended downward on repeat testing. Coronavirus testing via nasopharyngeal swab was negative.
Left heart catheterization revealed a completely occluded right coronary artery (RCA) at the mid-segment (Video 1). Because no antiplatelet agents were administered before the catheterization, the patient was maintained on a bivalirudin drip.
Online Video 1.
Coronary angiogram LAO 29 Caudal 4 View shows completely occluded right coronary artery (RCA) at the mid-segment.
Management
The RCA lesion was difficult to cross because the lesion appeared hard and fibrotic, but eventually, the lesion was successfully crossed, and a wire placed in the distal RCA. Owing to the difficulties encountered while crossing, it was elected to perform balloon angioplasty with the smallest balloon available. Three inflations were performed using a 1.5 × 10-mm balloon with no change in the intraprocedural ECG. Dye injection with balloon pullback revealed extravasation of contrast involving what appeared to be the trabeculae of the right ventricle, with delayed washout (Video 2). Bivalirudin was discontinued, and 50 mg of intravenous protamine administered. Repeated injections were administered, and eventually after 10 min, no further extravasation was noted. The patient was hemodynamically stable with no hypotension, chest pain, arrhythmias, or heart block.
Online Video 2.
Coronary angiogram LAO 29 Caudal 4 View shows extravasation of contrast involving what appeared to be the trabeculae of the right ventricle, with delayed contrast washout.
A transthoracic echocardiogram (TTE) was performed, which did not show a pericardial effusion, but instead, revealed a large ventricular septal defect involving the distal interventricular septum with moderate tricuspid regurgitation (Figure 2). A pulmonary artery (PA) catheter was placed in the right heart with measurements of hemodynamics and cardiac chamber pressures. Cardiac output was measured using the Fick’s principle. Right heart catheterization showed an elevated PA pressure, a PA oxygen saturation level of 77.9%, and a Qp/Qs ratio of 4.6 (Table 1).
Figure 2.

Transthoracic Echocardiogram Still Image of the Ventricular Septal Rupture
Transthoracic echocardiogram still image of the subcostal view with color flow shows ventricular septal rupture with large left-to-right shunt (pink arrow).
Table 1.
Right Heart Catheterization
| Aortic pressure, systolic/diastolic (mean), mm Hg | 87/62 (74) |
| Right ventricle pressure, systolic/diastolic (mean), mm Hg | 50/18 (22) |
| Pulmonary artery pressure, systolic/diastolic (mean), mm Hg | 48/21 (34) |
| Right atrium pressure, mean, mm Hg | 16 |
| Pulmonary capillary wedge pressure, mean, mm Hg | 22 |
| Pulmonary blood flow, Qp, l/min | 14.34 |
| Systemic blood flow, Qs, l/min | 3.07 |
| Qp/Qs ratio | 4.6 |
The case was concluded, the PA catheter was removed, and via the pigtail catheter, a ventriculogram obtained in the left anterior oblique projection confirming large left-to-right shunt (Video 3). The patient subsequently underwent a computed tomography scan of his chest revealing large 2.5-cm ventricular septal rupture (VSR) in the mid-inferoseptum with thinning of the basal and mid-inferior wall and inferoseptum (Figure 3).
Online Video 3.
Left ventriculogram LAO 35 Caudal 3 view shows large left-to-right shunt.
Figure 3.
Computed Tomography Angiography of the Ventricular Septal Rupture
Chest computed tomographic angiography reveals 2.5-cm ventricular septal rupture in the mid-inferoseptum with thinning of the basal and mid-inferior wall and inferoseptum in the axial, coronal, and sagittal views (yellow arrows).
Discussion
There has been a decrease in admissions for STEMI during the coronavirus disease-2019 (COVID-19) pandemic. The Interventional Cardiology Association of the Spanish Society of Cardiology reported a 40% reduction in cases of interventions with STEMI across Spain (1). Recently, Garcia et al. (2) quantified and analyzed STEMI activations for 9 high-volume cardiac catheterization laboratories in the United States from January 1, 2019, to March 31, 2020, with the time period after March 1, 2020, classified as “after COVID” for comparative analysis. This analysis during the early phase of the COVID-19 pandemic showed an estimated 38% reduction in the cardiac catheterization laboratory STEMI activations. An avoidance of medical care due to social distancing, concerns of contracting COVID-19 in the hospital, STEMI misdiagnosis, and increased use of pharmacological reperfusion due to COVID-19 has been the commonly attributed etiologies for a decrease in STEMI primary interventions (2). We presume our patient likely had the index myocardial infarction (MI) 7 days before presentation with a delayed presentation with a post-infarction VSR.
VSR is a devastating complication following acute MI, and its incidence has decreased from 1% to 3% following STEMI in the pre-reperfusion era to 0.17% to 0.31% following primary percutaneous coronary intervention (3). The Becker and van Mantgem classification is the most commonly accepted, and our patient exhibited a Becker type 3 rupture, which results from perforation of thinned aneurysmal myocardium in the late-phase post-MI and frequently in the absence of reperfusion injury (4). VSR in such cases occurs subacutely, typically 3 to 5 days after an index MI. The RCA is the most common infarct-related artery, accounting for 46% of total cases of VSR (5). VSRs are known to cause left-to-right shunting, and right ventricular volume and pressure overload. TTE is essential to diagnose the presence, size, and impact of the VSR and exclude other etiologies in cases of hemodynamic compromise. In occasions with unexplained hemodynamic compromise in the cardiac catheterization laboratory, left ventriculography can help confirm the presence of VSR, as exhibited by our case. Pulmonary artery catheterization reveals a step-up in oxygen saturation in the right ventricle and can be used to calculate the Qp/Qs, as was performed in our case. Surgical repair is the definitive treatment of choice and was adapted for our patient with good post-surgical recovery (6).
Follow-Up
The patient was transferred to the cardiac intensive care unit, and an intra-aortic balloon pump was inserted to reduce shunting and improve forward flow. Cardiothoracic surgery was consulted, and the patient underwent coronary artery bypass grafting of the posterior descending coronary artery, and a patch repair of the VSD with a tricuspid annulus repair. The patient tolerated the procedure well and was weaned off the balloon pump support within 48 h. Post-operative TTE showed a left ventricular ejection fraction of 40% with a residual VSR; however, a subsequent right heart catheterization ruled out any residual shunt. The patient was discharged home on post-operative day 10 with cardiology follow-up as an outpatient.
Conclusions
In the current scenario of the COVID-19 pandemic, there has been a considerable decrease in STEMI volume. Physicians should be prepared to encounter late complications of STEMI such as VSR, which is a rare presenting encounter in the era of primary percutaneous intervention.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Rodríguez-Leor O., Alvarez-Álvarez B., Ojeda S. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 2.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones B.M., Kapadia S.R., Smedira N.G. Ventricular septal rupture complicating acute myocardial infarction: a contemporary review. Eur Heart J. 2014;35:2060–2068. doi: 10.1093/eurheartj/ehu248. [DOI] [PubMed] [Google Scholar]
- 4.Honda S., Asaumi Y., Yamane T. Trends in the clinical and pathological characteristics of cardiac rupture in patients with acute myocardial infarction over 35 years. J Am Heart Assoc. 2014;3 doi: 10.1161/JAHA.114.000984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menon V., Webb J.G., Hillis L.D. Outcome and profile of ventricular septal rupture with cardiogenic shock after myocardial infarction: a report from the SHOCK Trial Registry. J Am Coll Cardiol. 2000;36(Suppl 1):1110–1116. doi: 10.1016/s0735-1097(00)00878-0. [DOI] [PubMed] [Google Scholar]
- 6.Arnaoutakis G.J., Zhao Y., George T.J., Sciortino C.M., McCarthy P.M., Conte J.V. Surgical repair of ventricular septal defect after myocardial infarction: outcomes from the Society of Thoracic Surgeons National Database. Ann Thorac Surg. 2012;94:436–443. doi: 10.1016/j.athoracsur.2012.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]




