Abstract
This case series summarizes our experience of delayed acute myocardial infarction presentations during the coronavirus disease-2019 pandemic predominantly driven by patient fear of contracting the virus in the hospital. Many presented with complications rarely seen in the primary percutaneous coronary intervention era including ventricular septal rupture, left ventricular pseudoaneurysm, and right ventricular infarction. (Level of Difficulty: Beginner.)
Key Words: coronary angiography, myocardial infarction, percutaneous coronary intervention
Abbreviations and Acronyms: ACS, acute coronary syndrome; COVID-19, coronavirus disease-2019; LV, left ventricle; MI, myocardial infarction; SARS-Cov-2, severe acute respiratory syndrome-coronavirus-2; STEMI, ST-segment elevation myocardial infarction
Graphical abstract
This case series summarizes our experience of delayed acute myocardial infarction presentations during the coronavirus disease-2019 pandemic predominantly…
Several reports have emerged highlighting a drastic drop in the number of acute myocardial infarctions (MIs), particularly ST-segment elevation myocardial infarctions (STEMI), since the coronavirus disease-2019 (COVID-19) pandemic began late last year. This seemingly has been an unintended yet not unexpected consequence of “social distancing,” which has “flattened” the curve of COVID-19 cases on the one hand while also dramatically decreasing STEMI presentations to the hospital. Is this phenomenon an added blessing of social distancing whereby elimination of the many population-attributable triggers of MI such as traffic exposure, air pollution, moderate to intense physical exertion, and stress have actually decreased the incidence of MI? (1). The concerning antithesis to this assumption is the following: Are patients with MIs too afraid to seek prompt medical attention out of fear of potential health care exposure to the virus with consequent morbidity and mortality? Although it may be too late to wait for the real answer until population-based studies with sound scientific methods are conducted, the recently reported 400% increase in at-home cardiac arrests in New York City being solely attributed to COVID-19 is alarming. Could a large proportion of these patients represent MI cases who are too petrified to come to the emergency department?
Learning Objectives
-
•
To understand the potential scope and adverse outcomes of late MI presentations during the pandemic due to fear of contracting infection.
-
•
To institute public awareness and education regarding the potential hazards of delayed presentation with concerning symptoms of MI.
New Jersey is the second most affected state in the United States by the COVID-19 pandemic with over 134,000 confirmed cases and nearly 9,000 deaths as of May 8, 2020 (2). We have seen a dramatic drop in all spectra of acute coronary syndrome (ACS) cases over the past 6 weeks. Among those who have presented with acute MI to our hospital, we present a case series of 10 patients from our cardiac catheterization laboratory in central New Jersey highlighting a concerning pattern.
This case series provides a troubling snapshot of acute MI presentations in non-COVID patients at one of the busiest cardiac care hospitals in New Jersey during the peak of the COVID-19 pandemic. From March 1, 2020, to April 25, 2020, our cardiac catheterization laboratory saw a significant drop in the number of STEMI cases. Ten patients presenting with acute MI, all of whom had delayed presentation, are summarized in Table 1. Details of their clinical presentations, electrocardiograms, procedures, and outcomes are summarized in the Supplemental Appendix and Supplemental Figures 1 to 20.
Table 1.
Case Series of 10 Acute MI Patients With Delayed Presentations
| Case # | Age (yrs)/Sex | Time to Presentation (Onset of Symptoms to Presentation to ER) | ECG Findings |
Anatomic Findings | Complications | LVEF (%) |
|---|---|---|---|---|---|---|
| 1 | 77/male | 48 h | Inferior STE and Q waves (II, III, aVF) | 100% RCA occlusion, TIMI flow grade 0 | CHF | 45 |
| 2 | 76/male | 48 h | Anteroseptal STE and Q waves (V1–V3) | 100% ostial LAD occlusion, TIMI flow grade 0 | LVEDP 36 mm Hg CHF |
35–40 |
| 3 | 86/female | 72 h | Anteroseptal STE and Q waves (V1–V3) | 95% mid-LAD stenosis, TIMI flow grade 2 | LVEDP 29 mm Hg CHF |
40–45 |
| 4 | 77/female | 48 h | T-wave inversion V1, V2 | 99% mid-LAD, TIMI flow grade 1 | None | 50–55 |
| 5 | 75/female | 7 days | Inferolateral STE Inferior Q waves Broad R waves V1–V2 |
Tortuous 100% mid-RCA occlusion with TIMI flow grade 0 80% distal left main 80% proximal LAD |
Post-MI VSD Basal inferolateral wall pseudoaneurysm IABP |
50–55 |
| 6 | 47/male | 5 days | Inferior STE ST-segment depressions V1–V2 |
100% LCX, TIMI flow grade 0 | Cardiac arrest on presentation CHF |
35–40 |
| 7 | 79/male | 24 h | Inferior STE Anterolateral STE |
100% ostial RCA occlusion, TIMI flow grade 0 Cardiac standstill |
Cardiogenic shock RV failure Ventricular fibrillation Impella CP |
20–25 |
| 8 | 64/male | 7 days | Inferior STE Posterior infarct |
Multiple lesions in sequential saphenous venous graft to posterior descending artery with 100% occluded posterolateral branch | None | 50 |
| 9 | 61/female | 14 days | Sinus arrhythmia Nonspecific T-wave abnormalities |
100% proximal RCA occlusion with TIMI flow grade 0 | None | 50 |
| 10 | 84/male | 48 h | Biventricular pacing PVC |
100% proximal LAD, TIMI flow grade 0, occluded LIMA to LAD 99% ramus intermedius stenosis Subtotally occluded left circumflex |
Prolonged hospital course, CHF, hemodialysis due to contrast-induced nephropathy | 20 |
A unifying theme among all cases was delayed presentation with extremely prolonged ischemic times defined as symptom onset to arrival to the emergency room. This delay was mainly driven by fear of seeking medical attention because of the risk of health care exposure and contracting the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) virus. However, all patients eventually tested negative for SARS-CoV-2 by polymerase chain reaction assays. Patients often presented critically ill with high-risk features such as significant left ventricular dysfunction, atrioventricular block, ventricular arrhythmias, and cardiac arrest. The majority required complex coronary interventions with some requiring mechanical circulatory support for cardiogenic shock. For example, Case 7 illustrates a patient who presented with a total ischemic time over 18 h and was found to be in complete heart block (Figure 1A). On arrival to the catheterization laboratory, the patient developed cardiac arrest and underwent complex coronary intervention of a totally occluded ostial right coronary artery (RCA) during active cardiopulmonary resuscitation and repeated defibrillation therapy, ultimately requiring mechanical circulatory support (Figure 1B, Videos 1, 2, 3, and 4). Case 5 demonstrates a patient who presented with an inferolateral STEMI after having chest discomfort for 1 week (Figure 2A). She was found to have an occluded mid-RCA with severe left main disease and a totally occluded left circumflex artery. Thrombolysis In Myocardial Infarction flow grade 3 was established during percutaneous intervention, and an intra-aortic balloon pump was placed (Figure 2B, Videos 5 and 6). The patient developed a ventricular septal rupture and a posterior wall pseudoaneurysm and was taken urgently to surgery (Figure 2C, Videos 7, 8, 9, and 10).
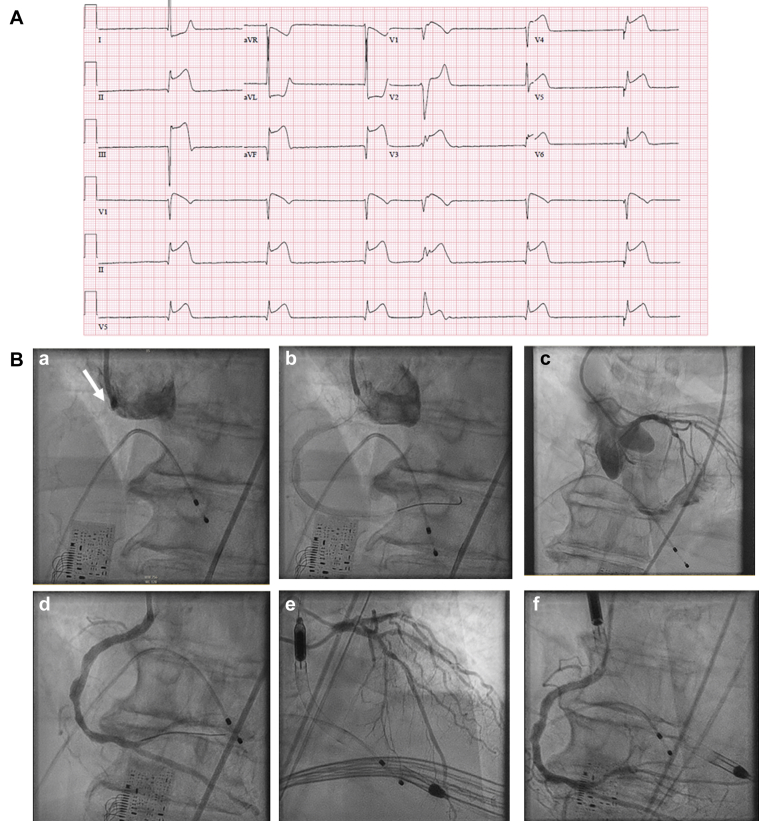
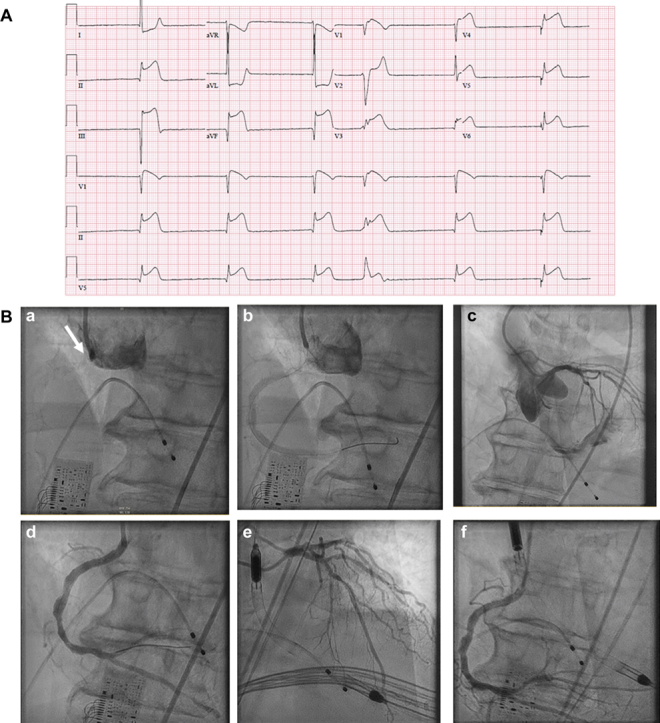
Figure 1.
Delayed Presentation Inferior Wall MI
(A) A 12-lead electrocardiogram showing complete heart block and inferoposterolateral ST-segment elevation myocardial infarction with junctional escape rhythm in a 79-year-old man with delayed presentation complicated by cardiogenic shock. (B) (a) Ostial right coronary artery (RCA) occlusion (arrow); (b) establishment of flow after wire passage and angioplasty; (c) patent left main, ostial left anterior descending (LAD), and left circumflex arteries with cardiac standstill; (d) after drug-eluting stent placement with normalized flow in the RCA; (e) after Impella CP (Abiomed, Danvers, Massachusetts) placement with mid-LAD and diagonal disease; and (f) the final angiography of the RCA.
Online Video 1.
Flush Occlusion of Ostial RCA in a 79-Year-Old Man With Delayed Presentation Complicated by Cardiogenic Shock
Online Video 2.
Left Coronary Angiography
Cardiac standstill can be appreciated.
Online Video 3.
PCI of RCA With Establishment of TIMI Flow Grade 3
Patient still in cardiac arrest requiring active chest compressions.
Online Video 4.
Stabilization of Hemodynamics Following Impella Placement
Successful PCI of RCA with good flow.
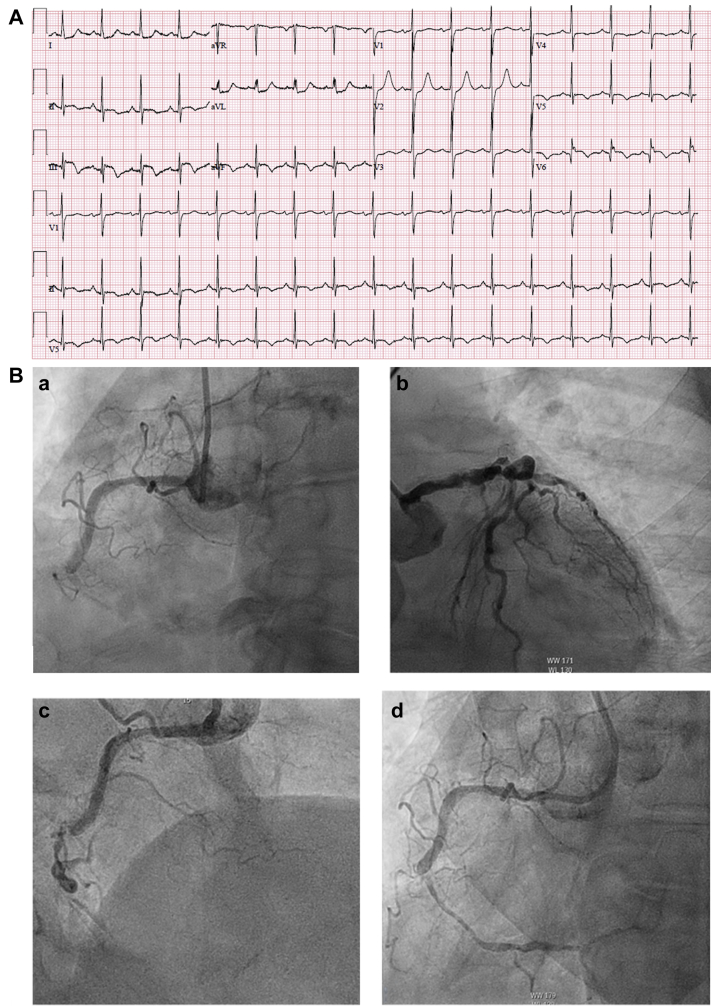
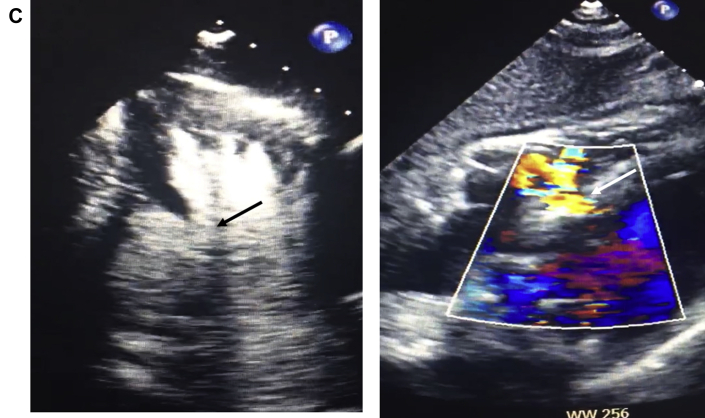
Figure 2.
Delayed Presentation Inferolateral Wall MI
(A) A 12-lead electrocardiogram showing inferoposterior ST-segment elevation myocardial infarction with posterolateral infarct pattern. (B) (a) RCA occlusion; (b) severe distal left main disease, proximal LAD disease, and occluded LCX; and (c and d) post wiring improved TIMI flow grade 3, revealing a severely calcified mid-RCA lesion. (C) Basal inferolateral pseudoaneurysm and ventricular septal rupture. LCX = left circumflex artery; TIMI = Thrombolysis In Myocardial Infarction; other abbreviations as in Figure 1.
Online Video 5.
Mid-RCA Occlusion With TIMI Flow Grade 3
Online Video 6.
TIMI Flow Grade 3 in RCA With Persistent High-Grade Mid-RCA Stenosis
Online Video 7.
Apical 4-Chamber View on Transthoracic Echocardiography Showing Basal Inferoseptal Ventricular Septal Defect With Left-to-Right Color Flow During Systole
Online Video 8.
Subcostal 4-Chamber View on Echo Showing Ventricular Septal Defect With Left-to-Right Shunt
Online Video 9.
Two-Chamber View on Echo Showing Basal Inferior Wall Pseudoaneurysm
Online Video 10.
Contrast Echo Showing Basal Inferior Wall Pseudoaneurysm
Multiple reports from areas deeply impacted by COVID-19 have shown a similar drop in acute MI presentations to their hospitals. A recent study from 9 hospital systems in the United States demonstrated a 38% drop in acute MI cases (3). Another large study from Northern California demonstrated weekly rates of hospitalization for acute MI decreased by 48% during the COVID-19 period (4). Other countries have shown similar data with up to 40% declines in STEMIs in Spain and parts of Italy (5). One may expect an increase in the number of acute MIs during a pandemic because of heightened environmental and psychosocial stressors such as job and financial insecurity. However, while the exact reasons for the observed decline are not clearly understood, it is hypothesized that fear of contracting SARS-CoV-2 by presenting to health care facilities is a major determinant. Our experience demonstrates an alarming pattern of delayed MI presentations associated with higher rates of adverse outcomes such as left ventricular dysfunction, cardiogenic shock, mechanical complications, and death. Another very concerning aspect of our experience was that these cases were not due to patients being unable to recognize their symptoms but rather, that they were often ignoring their symptoms in the hope they would resolve, thereby avoiding any potential health care exposure risk.
Although the concern of contracting SARS-CoV-2 is real for both patients and health care workers, it is important that it not be a deterrent in providing optimal treatments known to improve outcomes. In response to the COVID-19 pandemic at our hospital, where we have treated over 1,200 COVID patients thus far, we have developed algorithms to help streamline patients who would benefit from immediate percutaneous coronary intervention while maintaining patient and health care worker safety. One major challenge is that patients with COVID-19 may present with a STEMI syndrome but often have other conditions such as myocarditis, stress cardiomyopathy, or supply-demand mismatch that differs from an acutely occluded coronary artery. Therefore, a high index of clinical suspicion and a low threshold for testing are critical in identifying patients with known or suspected SARS-CoV-2 infection. Once the decision has been made to take the patient urgently to the cardiac catheterization laboratory, the patient should be tested and treated as a COVID-19 person under investigation until the test has resulted. Staff must use proper personal protective equipment including N95 masks, face shields or fully protective eye goggles, a bouffant cap, standard sterile gloves and gown, and a powered air-purifying respirator when performing endotracheal intubations.
Our experience demonstrates the consequences of delaying seeking medical care for patients with acute coronary syndrome. As we start to experience a second surge of the COVID-19 pandemic in the United States, it is crucial to educate the public that even during this pandemic, we continue to use the necessary measures needed to minimize exposure to SARS-CoV-2 and to therefore not disregard symptoms out of fear but rather seek prompt medical attention.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental material, figures, and videos, please see the online version of this paper.
Appendix
References
- 1.Nawrot T.S., Perez L., Künzli N., Munters E., Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377:732–740. doi: 10.1016/S0140-6736(10)62296-9. [DOI] [PubMed] [Google Scholar]
- 2.State of New Jersey Department of Health. Communicable Disease Service. COVID-19. Available at: https://www.state.nj.us/health/cd/topics/ncov.shtml. Accessed May 8, 2020.
- 3.Garcia S., Albadghdadi M., Perwaiz M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020 May 19 doi: 10.1056/NEJMc2015630. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.De Filippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.