Abstract
Background
ST-segment elevation myocardial infarction (STEMI) is a fatal cardiovascular emergency requiring rapid reperfusion treatment. During the coronavirus disease-2019 (COVID-19) pandemic, medical professionals need to strike a balance between providing timely treatment for STEMI patients and implementing infection control procedures to prevent nosocomial spread of COVID-19 among health care workers and other vulnerable cardiovascular patients.
Objectives
This study evaluates the impact of the COVID-19 outbreak and China Chest Pain Center’s modified STEMI protocol on the treatment and prognosis of STEMI patients in China.
Methods
Based on the data of 28,189 STEMI patients admitted to 1,372 Chest Pain Centers in China between December 27, 2019 and February 20, 2020, the study analyzed how the COVID-19 outbreak and China Chest Pain Center’s modified STEMI protocol influenced the number of admitted STEMI cases, reperfusion strategy, key treatment time points, and in-hospital mortality and heart failure for STEMI patients.
Results
The COVID-19 outbreak reduced the number of STEMI cases reported to China Chest Pain Centers. Consistent with China Chest Pain Center’s modified STEMI protocol, the percentage of patients undergoing primary percutaneous coronary intervention declined while the percentage of patients undergoing thrombolysis increased. With an average delay of approximately 20 min for reperfusion therapy, the rate of in-hospital mortality and in-hospital heart failure increased during the outbreak, but the rate of in-hospital hemorrhage remained stable.
Conclusions
There were reductions in STEMI patients’ access to care, delays in treatment timelines, changes in reperfusion strategies, and an increase of in-hospital mortality and heart failure during the COVID-19 pandemic in China.
Key Words: chest pain center, COVID-19, primary percutaneous coronary intervention, ST-segment elevation myocardial infarction, thrombolysis
Abbreviations and Acronyms: CCPC, China Chest Pain Center; CCPCEC, China Chest Pain Center Executive Committee; CI, confidence interval; COVID-19, coronavirus disease-2019; CPC, Chest Pain Center; FMC-to-N, time from first medical contact to needle (the beginning of thrombolysis); FMC-to-W, time from first medical contact to wire crossing; IQR, interquartile range; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; S-to-FMC, time from symptom onset to first medical contact
Central Illustration
ST-segment elevation myocardial infarction (STEMI), usually resulting from thrombotic occlusion of a coronary artery, is a fatal cardiovascular emergency requiring early diagnosis and rapid reperfusion therapy. The Chest Pain Center (CPC) was developed to accelerate this process (1,2). The growing coronavirus disease-2019 (COVID-19) pandemic caused by severe acute respiratory syndrome-coronavirus-2 poses a severe challenge to the care of STEMI patients. On the one hand, performing primary percutaneous coronary intervention (PCI)—the preferred reperfusion strategy recommended by most STEMI guidelines (3)—for a patient with unconfirmed COVID-19 status is a high-risk procedure that may expose health care workers and other hospitalized cardiovascular patients, who are particularly vulnerable if infected by severe acute respiratory syndrome-coronavirus-2 (4, 5, 6, 7). On the other hand, the screening and infectious control procedures required to reduce the nosocomial spread of COVID-19 may substantially delay primary PCI and negatively impact patient prognosis (8,9). The scarcity of personal protective equipment and rapid testing for COVID-19 further exacerbates the problem, as most medical facilities could not afford to engage full personal protective equipment for all STEMI patients with confirmed COVID-19 status.
As a result, medical professionals across the globe have been debating about the extent to which to initiate COVID-19 screening protocols for STEMI patients and to adjust treatment procedures to prevent nosocomial infection. Organizations or experts in the United States, Italy, Australia, and New Zealand have mostly recommended continuing with existing primary PCI protocols for STEMI patients except for confirmed COVID-19 patients and persons under investigation or cases in which primary PCI could not be performed within required time frames (10, 11, 12, 13). In contrast, experts in China, Iran, Palestine, and Jordan recommended prioritizing thrombolytic treatment for most patients with unconfirmed COVID-19 status (14, 15, 16).
However, there is no empirical study evaluating the impact of the COVID-19 pandemic and these different protocols on the prognosis of STEMI patients by the time of the writing of this paper, apart from 2 observational studies reporting 38% to 40% reduction in cardiac catheterization laboratory STEMI activities in Spain and United States and 1 small sample study reporting significant primary PCI delays in Hong Kong (8,17,18).
We draw on data from the China Chest Pain Center (CCPC) Database to evaluate the impact of the COVID-19 pandemic on the care of STEMI patients and provide much needed empirical evidence for this challenge. Like those in other countries, CCPC’s regular STEMI protocol recommends primary PCI as the standard of care for STEMI patients (1). Anticipating infectious control measures needed during the COVID-19 outbreak, the CCPC Executive Committee (CCPCEC) modified its STEMI protocol on January 23, 2020. This modified protocol recommended thrombolysis as the preferred reperfusion strategy for patients with unconfirmed COVID-19 status in areas affected by the outbreak to ensure timely reperfusion and prevent nosocomial infection (15). In this paper, we use data from the CCPC Database to evaluate how the COVID-19 pandemic and the related changes in STEMI protocols have affected access to cardiac care, reperfusion strategies, reperfusion efficiency, and prognosis of STEMI patients.
Methods
Data source and sample
All data included in this study come from the CCPC Database, which was established in 2015. All Chinese hospitals with CPCs are required to register in this database and report the basic information, diagnosis and treatment procedures, and timelines of all patients presenting with acute chest pain. The CCPCEC uses the data in this database to accredit CPCs in China and monitor their operation.
The CPC of the General Hospital of the Southern Theatre Command created the first modified STEMI protocol—the “Treatment Protocol for Novel Coronavirus Pneumonia Patients with STEMI”—on January 23, 2020, the same day that the Chinese government announced the decision to lock down the epicenter Wuhan. CCPCEC immediately distributed and recommended this protocol to its network of 4,420 (accredited and unaccredited) CPCs across the country. On February 10, a refined version of this protocol was formally published as the “Chinese Expert Consensus on the Operation of Chest Pain Centers during the COVID-19 Pandemic” (15), jointly signed by the Chest Pain Committee of the Chinese College of Physicians, Chinese College of Cardiovascular Physicians, CCPCEC, and the Headquarters of the CCPC. The CCPC hosted 2 online training sessions on this protocol on February 7 and February 10, 2020, reaching a total of 24,705 participants.
In this study, we treated January 24, 2020, as the start time of the COVID-19 outbreak in China as well as the implementation of the revised protocol and analyzed changes in the treatment and prognosis of STEMI patients before and after this point. We included in our analysis all STEMI cases admitted to the 1,372 accredited CPCs from the 4 weeks before and the 4 weeks after January 24, 2020 (December 27, 2019 to February 20, 2020). We excluded cases when the records for key time points were incomplete and when transfer to other medical facilities prevented the collection of outcome data. Our research protocol was approved by the Medical Ethics Committee of the General Hospital of Southern Theatre Command of PLA.
Key variables
The key independent variables are the COVID-19 outbreak period (whether the patient was admitted between January 24, 2020 and February 20, 2020), Hubei (whether the patient was admitted to a CPC in Hubei province, the epicenter of the COVID-19 outbreak in China that accounted for 80.78% of the country’s confirmed cases as of April 26, 2020), and the interaction of these 2 variables. We analyzed the impact of these independent variables on 4 groups of key outcome variables: 1) indicators of STEMI patients’ access to care: the weekly total number of admitted STEMI cases at each accredited CPC and the time from symptom onset to first medical contact (S-to-FMC); 2) reperfusion strategy: primary PCI, thrombolysis, or conservative therapy; 3) indicators of STEMI reperfusion efficiency: time from first medical contact to wire crossing (FMC-to-W) for patients undergoing primary PCI, time from first medical contact to needle (the beginning of thrombolysis) (FMC-to-N) for patients undergoing thrombolytic therapy, effective reperfusion (successful thrombolysis or Thrombolysis In Myocardial Infarction flow grade 3), and timely reperfusion (FMC-to-N ≤30 min or FMC-to-W ≤120 min); and 4) indicators of patient prognosis: in-hospital mortality, in-hospital heart failure, and in-hospital hemorrhage. We included patient age and sex as control variables for all models of individual-level variables.
Statistical procedures
Continuous variables are summarized as mean ± SD for symmetric distributions and median (interquartile range [IQR]) for skewed distributions. Discrete variables are presented as frequency (percentage). We conducted Student’s t-tests (for continuous variables) and chi-square tests (for discrete variables) to compare the characteristics of the outbreak sample and those of the pre-outbreak sample for Hubei and for other regions, respectively. We then estimated multivariate linear regression models for continuous outcome variables and logistic regression models for dichotomous outcome variables, except for using a mixed-effects model for weekly STEMI cases to account for dependence among the weekly numbers reported by the same CPC. We also produced descriptive plots based on weekly means of outcome variables to provide an intuitive understanding of trends in the raw data. All statistical analysis was conducted using SAS software version 9 (SAS Institute, Cary, North Carolina).
Results
A total of 28,189 STEMI cases were reported by 1,372 accredited CPCs during the 8-week sampling period. Among these cases, 25,150 (89.22%) met the inclusion criteria of having complete information regarding key time points and patient outcome. The final COVID-19 sample included slightly more male patients and slightly younger patients (Table 1 ). There were also statistically significant differences in key time points, proportion of effective reperfusion and timely reperfusion, and patient prognosis, which will be analyzed in the following 4 sections.
Table 1.
Sample Baseline Characteristics
| Hubei Sample |
Non-Hubei Sample |
|||||
|---|---|---|---|---|---|---|
| Pre-Outbreak | Outbreak | p Value | Pre-Outbreak | Outbreak | p Value | |
| Total STEMI cases reported | 626 | 236 | — | 15,729 | 11,598 | — |
| Included cases∗ | 564 | 220 | 0.740 | 14,070 | 10,296 | 0.838 |
| S-to-FMC ≤12 | 425 (75.35) | 158 (71.82) | 11,151 (79.25) | 8,126 (78.92) | ||
| Male | 427 (75.7) | 170 (77.3) | 0.644 | 10,592 (75.3) | 7,816 (76.0) | 0.245 |
| Age, yrs | 62.86 ± 12.33 | 61.59 ± 13.10 | 0.203 | 62.91 ± 12.95 | 62.37 ± 12.81 | 0.001 |
| Pattern of patient arrival | 0.352 | 0.005 | ||||
| Walk-in | 283 (50.2) | 126 (57.3) | 7,740 (55.0) | 5,562 (54.0) | ||
| EMS | 51 (9.0) | 16 (7.3) | 1,498 (10.7) | 1,150 (11.2) | ||
| Transfer | 208 (36.9) | 71 (32.3) | 4,536 (32.2) | 3,420 (33.2) | ||
| In-hospital onset | 22 (3.9) | 7 (3.2) | 296 (2.1) | 163 (1.6) | ||
| S-to-FMC, h† | 2.57 (1.12–7.67) | 3.22 (1.34–7.86) | 0.114 | 2.33 (1.05–6.16) | 2.53 (1.15–6.38) | <0.001 |
| FMC-to-N, min† | 33.0 (20.0–52.0) | 45.0 (27.0–83.0) | 0.098 | 35.0 (24.0–62.0) | 38.0 (26.0–70.0) | <0.001 |
| FMC-to-W, min† | 101.5 (74.0–187.0) | 108.5 (75.5–204.5) | 0.245 | 93.0 (69.0–154.0) | 99.0 (73.0–159.0) | <0.001 |
| Effective reperfusion | 58 (68.2) | 38 (67.9) | 0.962 | 3,070 (79.4) | 2,165 (78.7) | 0.496 |
| Timely reperfusion | 214 (59.44) | 66 (51.56) | 0.121 | 6,261 (65.13) | 4,224 (60.10) | <0.001 |
| In-hospital mortality | 26 (4.6) | 16 (7.3) | 0.137 | 566 (4.0) | 480 (4.7) | 0.015 |
| In-hospital heart failure | 78 (14.2) | 40 (18.4) | 0.139 | 1,794 (13.2) | 1,404 (14.0) | 0.081 |
| Hemorrhage | 4 (0.9) | 4 (2.3) | 0.176 | 108 (1.1) | 68 (0.9) | 0.320 |
Values are n, n (%), mean ± SD, or median (interquartile range).
EMS = emergency medical services; FMC-to-N = time from first medical contact to needle (the beginning of thrombolysis); FMC-to-W = time from first medical contact to wire crossing; S-to-FMC = time from symptom onset to first medical contact; STEMI = ST-segment elevation myocardial infarction.
Cases are included if they were admitted during the sampling period, had complete key time point information, and had complete outcome information.
The z estimates are from the Mann-Whitney U test
COVID-19 and STEMI patients’ access to care
Hospitalized STEMI cases
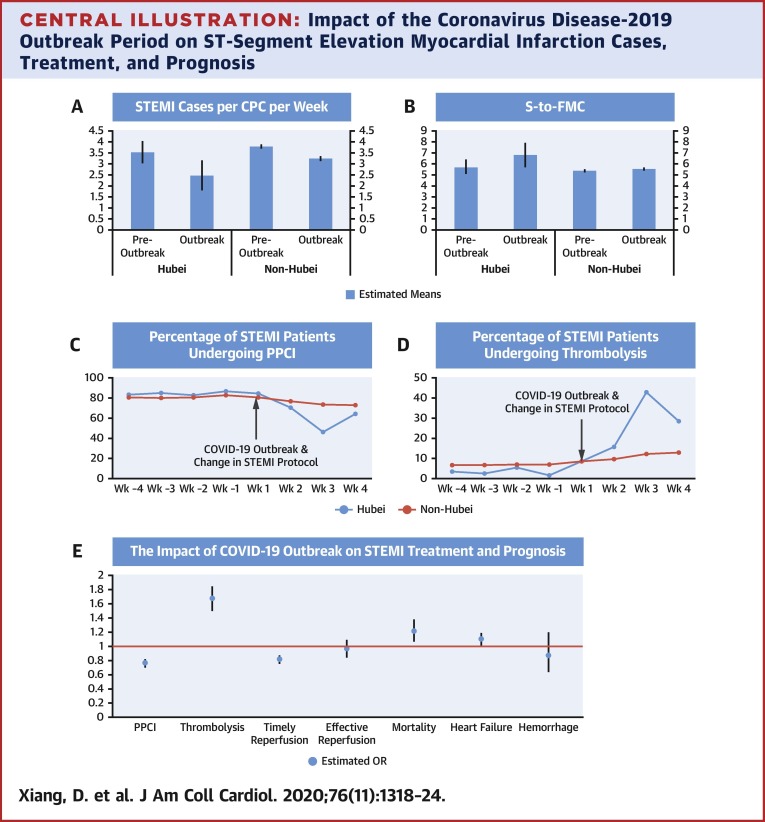
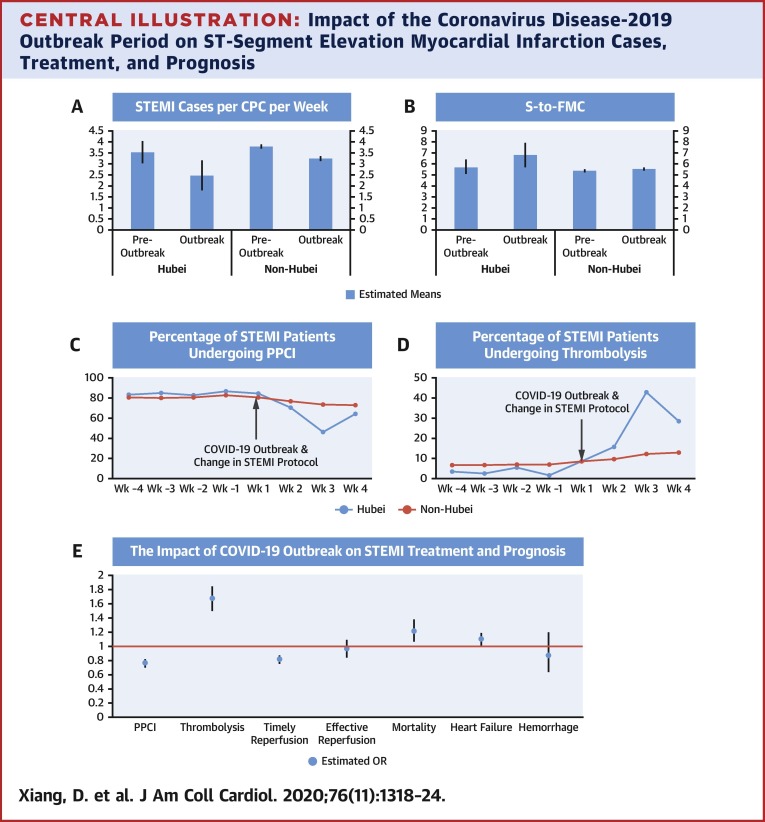
There was an approximately 26% drop in the weekly total number of hospitalized STEMI cases during the COVID-19 outbreak nationwide, and an approximately 62% drop in Hubei (Table 1). Regression analysis (Table 2 ) confirmed the negative and significant effect of the COVID-19 outbreak on the number of cases reported by each CCPC each week (coefficient: –0.55; 95% confidence interval [CI]: –0.71 to –0.40; p < 0.001), but the interaction term was not statistically significant (coefficient: –0.50; 95% CI: –1.37 to 0.37; p = 0.25). Our model estimated that each CCPC admitted 2.47 patients (95% CI: 1.78 to 3.16 patients) (Hubei) and 3.24 patients (95% CI: 3.12 to 3.36 patients) (non-Hubei) each week during the COVID-19 outbreak period, in contrast to 3.53 patients (95% CI: 3.02 to 4.04 patients) (Hubei) and 3.79 patients (95% CI: 3.69 to 3.89 patients) (non-Hubei) per center per week before the outbreak (Central Illustration ).
Table 2.
Results of Regression Models
| Model | Outcome Variable | n | Outbreak | Outbreak × Hubei |
|---|---|---|---|---|
| 1 | Hospitalized STEMI cases (per CPC per week) | 7,145 | –0.55 (–0.71 to –0.40)∗ | –0.50 (–1.37 to 0.37) |
| 2 | S-to-FMC, h | 23,133 | 0.12 (–0.10 to 0.33) | 0.88 (–0.48 to 2.24) |
| 3 | Primary PCI | 21,205 | 0.76 (0.71 to 0.81)∗ | 0.58 (0.38 to 0.89)† |
| 4 | Thrombolysis | 21,205 | 1.67 (1.50 to 1.84)∗ | 4.78 (2.45 to 9.34)∗ |
| 5 | Timely reperfusion | 17,107 | 0.81 (0.76 to 0.86)∗ | 0.90 (0.60 to 1.36) |
| 6 | Effective reperfusion | 16,759 | 0.96 (0.85 to 1.08) | 1.03 (0.49 to 2.13) |
| 7 | Total ischemic time, h | 16,525 | 0.09 (–0.12 to 0.29) | –0.06 (–1.45 to 1.32) |
| 8 | FMC-to-W, min | 15,280 | 4.44 (0.43 to 8.44)† | 16.20 (–11.76 to 44.17) |
| 9 | FMC-to-N, min | 2,602 | 4.54 (0.72 to 8.36)† | 17.56 (–6.01 to 41.12) |
| 10 | In-hospital mortality | 25,118 | 1.21 (1.07 to 1.37)‡ | 1.42 (0.73 to 2.76) |
| 11 | In-hospital heart failure | 24,342 | 1.10 (1.02 to 1.18)† | 1.30 (0.85 to 2.00) |
| 12 | In-hospital hemorrhage | 18,031 | 0.87 (0.64 to 1.19) | 2.93 (0.70 to 12.27) |
Values are n or odds ratio/coefficient (95% confidence interval). Each row in the table represents a regression model. Models 2–12 included age and sex as control variables.
CPC = Chest Pain Center; PCI = percutaneous coronary intervention; other abbreviations as in Table 1.
p < 0.001.
p < 0.05.
p < 0.01.
Central Illustration.
Impact of the Coronavirus Disease-2019 Outbreak Period on ST-Segment Elevation Myocardial Infarction Cases, Treatment, and Prognosis
(A, B) The estimated means of number of ST-segment elevation myocardial infarction (STEMI) cases per Chest Pain Center (CPC) per week and the estimated means of time from symptom onset to first medical contact (S-to-FMC) (in hours) before and during the outbreak, in Hubei and in other provinces. (C, D) The decrease of proportion of STEMI cases undergoing primary percutaneous coronary intervention (PPCI) and the increase of those undergoing thrombolysis during the coronavirus disease-2019 (COVID-19) outbreak. (E) The estimated odds ratios of the independent variable “COVID-19 Outbreak Period” (January 24, 2020 to February 20, 2020) and corresponding confidence intervals in logistic regression models with 8 intermediate and endpoint outcome variables. OR = odds ratio; Wk = week.
Time from symptom onset to first medical contact
During the COVID-19 outbreak, the percentage of reported STEMI cases with FMC within 12 h of symptom onset dropped slightly in Hubei (Table 1), but this trend was not statistically significant in our regression analysis (Table 2). Our model estimated that mean S-to-FMC during the COVID-19 outbreak period was 6.75 h (IQR: 5.61 to 7.89 h) (Hubei) and 5.48 h (IQR: 5.30 to 5.66 h) (non-Hubei), in contrast to 5.66 h (IQR: 4.99 to 6.32 h) (Hubei) and 5.32 h (IQR: 5.16 to 5.48 h) (non-Hubei) before the outbreak.
COVID-19 and changes in reperfusion strategies and efficiency for STEMI patients
Reperfusion strategies
The percentage of STEMI patients undergoing primary PCI dropped by one-half, whereas the percentage of thrombolysis increased sharply in Hubei during the COVID-19 outbreak (Central Illustration). There were similar but more moderate trends in the non-Hubei sample. Regression analysis (Table 2) confirmed these trends. The COVID-19 outbreak significantly reduced the probability of primary PCI (odds ratio [OR]: 0.76; 95% CI: 0.71 to 0.81; p < 0.001), with a much larger effect in Hubei province (interaction term OR: 0.57; 95% CI: 0.37 to 0.88; p < 0.001). In contrast, the COVID-19 outbreak had a substantial positive effect on the probability of thrombolysis (OR: 1.66; 95% CI: 1.50 to 1.84; p < 0.001), particularly in Hubei (interaction term OR: 4.78; 95% CI: 2.45 to 9.33; p < 0.001). These results are consistent with the modified CCPC STEMI protocol that recommended prioritizing thrombolysis.
Timely reperfusion
The proportion of STEMI patients receiving timely reperfusion therapy dropped from 59.44% to 51.56% in Hubei during the COVID-19 outbreak and from 65.13% to 60.10% in other provinces. Regression analysis confirmed the negative impact of being admitted during the COVID-19 outbreak period (OR: 0.80; 95% CI: 0.76 to 0.86; p < 0.001), but the interaction term between the COVID-19 outbreak period and Hubei province was not statistically significant (Table 2).
Further analysis of FMC-to-W and FMC-to-N revealed that the COVID-19 outbreak delayed primary PCI for 20.82 min in Hubei and 4.43 min in other provinces; the delay for thrombolytic treatment was 22.60 min in Hubei and 4.49 min in other provinces (Table 2). Overall, the impact of the COVID-19 outbreak on total ischemic time was not statistically significant in Hubei or in other provinces.
Effective reperfusion
Being admitted during the COVID-19 impact period had no significant effect on the probability of receiving effective reperfusion (defined as successful thrombolysis or reaching TIMI flow grade 3 after primary PCI), in Hubei or in other provinces (Table 2).
In-hospital mortality and heart failure rates
The rates of in-hospital mortality and in-hospital heart failure increased from 4.6% to 7.3% and from 14.2% to 18.4% in Hubei during the outbreak period (Table 1), while the increase for other provinces was much smaller. Regression analysis confirmed that being admitted during the COVID-19 outbreak period was associated with higher likelihood of in-hospital mortality (OR: 1.21; 95% CI: 1.07 to 1.37; p = 0.003) and in-hospital heart failure (OR: 1.10; 95% CI: 1.02 to 1.18; p = 0.020), but the interaction term between the COVID-19 outbreak period and Hubei province was not statistically significant (Table 2). The COVID-19 outbreak did not have an impact on the rate of in-hospital hemorrhage, in Hubei or in other parts of the country (Table 2).
Discussion
The decline in hospitalized STEMI cases and the slight-to-moderate increases in S-to-FMC, FMC-to-N and FMC-to-W during the COVID-19 outbreak suggest that the outbreak reduced STEMI patients’ probability of accessing care and receiving timely reperfusion. These changes were more pronounced in Hubei province, the epicenter of the outbreak in China. Consistent with CCPC’s modified STEMI protocol, there was an increase in the proportion of STEMI cases undergoing thrombolysis and a decrease in that of primary PCI during the outbreak, with no significant change in the proportion of STEMI cases receiving effective reperfusion therapy. The in-hospital mortality and in-hospital heart failure rate of STEMI patients increased during the COVID-19 outbreak in China, while the rate of in-hospital hemorrhage remained stable in Hubei as well as in other parts of the country.
Our findings provide much needed empirical evidence for health care professionals searching for a balance between optimizing timely treatment for STEMI patients and protecting health care workers and vulnerable cardiovascular patients from the risk of nosocomial COVID-19 infection. Despite the inevitable delays in treatment timeline due to mandatory infection control procedures and changes in reperfusion strategies during the outbreak, the proportion of patients receiving effective reperfusion remained stable.
Study limitations
Our study has 3 important limitations. First and foremost, because there was little time lag between the start of China’s response to the COVID-19 outbreak and the release of CCPC’s modified STEMI protocol, this observational study cannot fully dissociate the effects of the CCPC’s modified protocol from the other aspects of the COVID-19 outbreak. In other words, we cannot conclude the extent to which the switch to prioritizing thrombolysis for patients with unclear COVID status contributed to the deterioration of STEMI prognosis or attenuated the negative impact of other factors during the outbreak. Because most unobserved factors—such as mild patients delaying or avoiding hospital visits during the outbreak—tend to worsen the prognosis of hospitalized patients entering our sample, the results that we currently observe is likely an overestimation of the overall negative impact of the COVID-19 outbreak.
The second limitation is that we were unable to assess the extent to which CCPC’s modified protocol protected health care workers and other vulnerable cardiovascular patients from COVID-19 infection due to the lack of complete data on nosocomial infection. Nonetheless, the information that we do have suggest that the protocol was likely effective in this regard. As of April 27, 2020, the CPCs in our network had reported only 2 cases of nosocomial infection related to procedures of primary PCI or thrombolysis during this pandemic, both occurring in catheterization labs during primary PCI in Wuhan, Hubei, before we released the modified protocol on January 23, 2020.
Last, but not least, the analysis presented in this paper did not account for the influence of the spring festival holiday, a major 2-week festival that coincided with the first 2 weeks of the COVID-19 outbreak period. The spring festival significantly influences patient behavior, public transportation, and hospital operation. Because this study did not include a spring festival period control group, it cannot dissociate the impacts of the spring festival on STEMI treatment and prognosis from those of the COVID-19 outbreak in China.
Conclusions
The COVID-19 outbreak led to a substantial drop in the number of admitted STEMI cases as well as delays in patients’ access to care. Consistent with CCPC’s recommendations, the proportion of patients undergoing primary PCI decreased and that of thrombolysis increased, but the proportion of patients receiving effective reperfusion therapy remained stable. The outbreak was associated with moderately increased in-hospital mortality and in-hospital heart failure, while the probability of in-hospital hemorrhage did not change.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: The COVID-19 outbreak negatively affected STEMI patient’s access to care, treatment timeline, and prognosis.
TRANSLATIONAL OUTLOOK: Future studies should compare the treatment and prognosis of STEMI patients in countries implementing different pandemic STEMI protocols to further evaluate the effects of different strategies.
Acknowledgments
The authors thank the staff members of all the CPCs in China for their hard work in caring for STEMI patients, and the staff of CCPC Headquarters for their full support in promoting the modified the STEMI protocol and in collecting data for this analysis. The authors are particularly grateful for Wei Sun for providing invaluable advice for the statistical analysis process.
Footnotes
This study is supported by Ministry of Science and Technology of the People’s Republic of China (2016YFC1301201). The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Zhang Y., Yu B., Han Y. Protocol of the China ST-segment elevation myocardial infarction (STEMI) Care Project (CSCAP): a 10-year project to improve quality of care by building up a regional STEMI care network. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiang D., Yi S. Chest pain centers in China: Current status and prospects. Cardiol Plus. 2017;2:18–21. doi: 10.4103/cp.cp_5_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ibanez B., James S., Agewall S. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Leor O., Cid-Alvarez B. STEMI care during COVID-19: losing sight of the forest for the trees. J Am Coll Cardiol Case Rep. 2020 Apr 23 doi: 10.1016/j.jaccas.2020.04.011. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ardati A.K., Mena Lora A.J. Be prepared. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam C.-C.F., Cheung K.-S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daniels M.J., Cohen M.G., Bavry A.A., Kumbhani D.J. Reperfusion of STEMI in the COVID-19 era - business as usual? Circulation. 2020;141:1948–1950. doi: 10.1161/CIRCULATIONAHA.120.047122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szerlip M., Anwaruddin S., Aronow H.D. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic. Catheter Cardiovasc Interv. 2020 Mar 25 doi: 10.1002/ccd.28887. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Zaman S., MacIsaac A.I., Jennings G.L. Cardiovascular disease and COVID-19: Australian and New Zealand consensus statement. Med J Aust. 2020 Jul 31 doi: 10.5694/mja2.50714. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Uccio F.S.D., Valente S., Colivicchi F. ANMCO position paper: the network organization for the management of patients with acute coronary syndrome during the COVID-19 pandemic. G Ital Cardiol. 2020;21:332–335. doi: 10.1714/3343.33129. [DOI] [PubMed] [Google Scholar]
- 13.Mahmud E., Dauerman H.L., Welt F.G. Management of acute myocardial infarction during the COVID-19 pandemic: a position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) J Am Coll Cardiol. 2020;76:1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daralammouri Y., Azamtta M., Hamayel H. Recommendations for safe and effective practice of interventional cardiology during COVID-19 pandemic: expert opinion from Jordan and Palestine. Palest Med Pharm J. 2020;5:65–73. [Google Scholar]
- 15.Xiang D., Huo Y., Ge J. Expert consensus on operating procedures at chest pain centers in China during the coronavirus infectious disease-19 epidemic. Cardiol Plus. 2020;5:21–32. doi: 10.4103/cp.cp_5_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadeghipour P., Talasaz A.H., Eslami V. Management of ST-segment-elevation myocardial infarction during the coronavirus disease 2019 (COVID-19) outbreak: Iranian“247” National Committee’s position paper on primary percutaneous coronary intervention. Catheter Cardiovasc Interv. 2020 Apr 22 doi: 10.1002/ccd.28889. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S. The impact of the COVID-19 pandemic on healthcare activities in interventional cardiology units in Spain. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]