Highlights
-
•
The ongoing COVID-19 pandemic has resulted in cancellation/postponement of elective surgeries worldwide.
-
•
This has resulted in a major change in the volume and spectrum of neurosurgical cases.
-
•
The number of surgeries performed are decreasing as the number of COVID-19 cases increase.
-
•
Aerosol generating procedures put the neurosurgeons at a high risk of contracting COVID-19 infection.
Keywords: COVID-19 (coronavirus disease of 2019), India, Neurosurgical practice, COVID-19 testing, Elective surgeries, Emergency surgeries
Abstract
Background
There has been a dramatic change in the pattern of patients being seen in hospitals and surgeries performed during the ongoing COVID-19 pandemic. The objective of this study is to study the change in the volume and spectrum of surgeries performed during the ongoing COVID-19 pandemic compared to pre-COVID-19 era.
Methods
Details of all patients who were operated under department of neurosurgery at our institute since the onset of COVID-19 pandemic in India were collected and compared to the same time period last year. The demographic profile, diagnosis, surgery performed, type of surgery (routine/emergency, cranial/spinal and major/minor) in these two groups were compared. They were further categorized into various categories [neuro-oncology (brain and spine tumors), neuro-trauma (head injury and spinal trauma), congenital cases, degenerative spine, neuro-vascular, CSF diversion procedures, etc.] and compared between the two groups.
Results
Our study showed a drastic fall (52.2%) in the number of surgeries performed during the pandemic compared to pre-COVID era. 11.3% of patients operated during COVID-19 pandemic were non-emergent surgeries compared to 57.7% earlier (p = 0.000). There was increase in proportion of minor cases from 28.8% to 41.5% (p = 0.106). The proportion of spinal cases decreased from 27.9% to 11.3% during the COVID-19 pandemic (p = 0.043).
Conclusions
The drastic decrease in the number of surgeries performed will result in large backlog of patients waiting for ‘elective’ surgery. There is a risk of these patients presenting at a later stage with progressed disease and the best way forward would be to resume work with necessary precautions and universal effective COVID-19 testing.
1. Introduction
COVID-19 has spread worldwide since the first case was reported in Wuhan, China, in December 2019 [1]. India reported its first case on Janurary 30th, 2020 [2] while the hilly state of Uttarakhand reported her first case one and a half month later on March 15th, 2020 [3]. The number of confirmed COVID-19 positive patients has been rising since then due to the highly infectious nature of the virus. At the time of writing this article on 21st June 2020, the number of COVID-19 positive patients in India has touched 410,461 with a death toll of 13,254 [4]. In order to contain the spread of COVID-19 pandemic in the country, the Union Government of India took rapid measures like increasing public awareness about COVID-19, advising social distancing and the universal use of masks. Like many other counties of the world, complete national lockdown was announced in India, starting from March 25th, 2020 and was continued till May 31st, 2020 in four phases. This was necessary to contain the spread of COVID-19 and prepare hospitals for the increased number of COVID-19 patients [5].
Hospitals and medical institutions have had to adapt to the ‘new normal’ by doing widespread COVID-19 testing, switching from physical out-patient department (OPD) to telemedicine and rescheduling of ‘non-emergent’ surgeries [6]. However, there has been a concern amongst health-care workers for patients who had their surgeries cancelled/postponed due to the ongoing COVID-19 pandemic. The authors analyzed the volume and spectrum of neurosurgery patients who underwent surgery at their institution during the period of COVID-19 related lockdown and compared with the spectrum of neurosurgery patients operated during the same period last year. This change may be reflection of the patients who could not undergo surgery during the pandemic.
2. Materials and methods
Details of all patients who were operated under the Department of Neurosurgery at our institute since the onset of COVID-19 pandemic in the country were collected (partially retrospectively and partially prospectively). This was studied according to the four phases of national lockdown as declared by the Union Government of India, i.e. phase I from March 25th to April 14th, phase II from April 15th to May 3rd, phase III from May 4th to May 17th, phase IV from May 18th to May 31st. Data on the number of confirmed COVID-19 cases in the state of Uttarakhand was collected from the official website of Ministry of Health and Family welfare [4]. A comparison was made between the number of cases operated in our department with the number of confirmed COVID-19 cases in the state of Uttarakhand.
Data of patients who underwent surgery under the Department of Neurosurgery during the same period last year, i.e. 25th March 2019 to 31st May 2019 was retrieved retrospectively. The decision to include the patients operated during the same time of the year last year was made in order to remove any seasonal variation in the patient profile. This data was collected from the patient records in neurosurgery operation theatre and patients’ discharge summaries. From May 1st till June 9th 2019, the institute had summer vacation during which, the operation rooms run at only half the strength, while the vacation in 2020 was cancelled in view of the pandemic.
The demographic profile, diagnoses, surgeries performed, type of surger (routine/emergency, cranial/spinal and major/minor) in these two groups were compared. They were further categorized into various categories [i.e. neuro-oncology (brain and spine tumors), neuro-trauma (head injury and spinal trauma), congenital cases, degenerative spine, neuro-vascular, CSF diversion procedures, etc.] and compared between the two groups.
Statistical analysis was performed using IBM Statistical Package for Social Sciences (SPSS version 25.0, SPSS, Inc., Chicago, IL, USA). Continuous variables were expressed as mean and range while categorical variables were expressed as frequencies. Chi square test was used to test for the association between groups of categorical variables. To assess the correlation between the number of surgeries performed and the number of COVID-19 cases in the state of Uttarakhand, Spearman's rank correlation coefficient was used.
3. Results
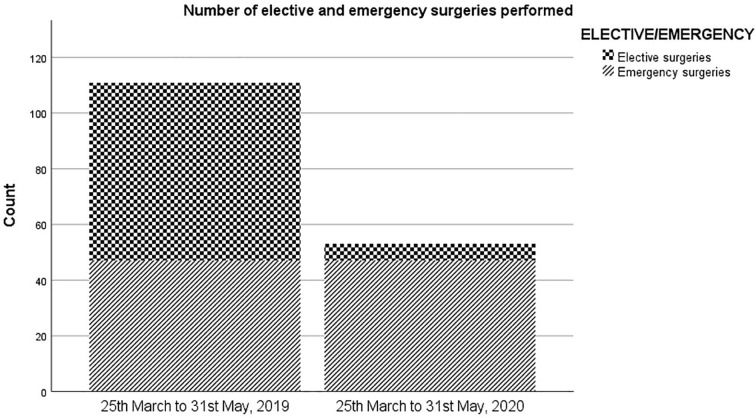
One hundred sixty-four patients were included in the study, of which 53 underwent surgery at our institute during the COVID-19 related lockdown (from March 25th to May 31st 2020). These 53 patients (36 males, 17 females) had a mean age of 38.46 years (range 1–80 years). Forty-seven (88.7%) cases were operated as emergency while six (11.3%) underwent surgery as elective cases. During the same period in 2019, 111 patients (69 males, 42 females) with mean age of 33.86 years (range 2 months – 72 years) underwent surgery. Of these, 47 (42.3%) were emergencies and 64 (57.7%) were done as routine cases (Table 1 ). Thus, during the ongoing pandemic, the total number of surgeries at our department decreased by 52.2% as compared to last year. The proportion of non-emergent cases decreased from 57.7% in pre-COVID era to 11.3% during the COVID-19 pandemic. This change was found to be statistically significant (p value = 0.000) (Fig. 1 ).
Table 1.
Table comparing the data between the years 2019 and 2020 for the time period March 25th to May 31st. A reduction in the number of surgeries performed is observed, across all specialities.
| 2019 (25th March to 31st May) |
2020 (25th March to 31st May) |
|
|---|---|---|
| Total cases operated | 111 | 53 |
| Male:Female | 69:42 | 36:17 |
| Mean age of patients in years | 33.86 | 38.46 |
| Age range | 2 mths- 72 yrs | 1–80 yrs |
| Elective surgeries | 64 (57.7%) | 6 (11.3%) |
| Emergency surgeries | 47 (42.3%) | 47 (88.7%) |
| Major surgeries | 79 (71.2%) | 31 (58.5%) |
| Minor surgeries | 32 (28.8%) | 22 (41.5%) |
| Cranial cases | 79 (71.2%) | 47 (88.7%) |
| Spinal cases | 31 (27.9%) | 6 (11.3%) |
| Peripheral nerves | 1 (0.9%) | 0 (0%) |
| Brain tumour | 30 (27%) | 12 (22.6%) |
| Congenital | 7 (6.3%) | 0 (0%) |
| Cranial infection | 0 (0%) | 1 (1.9%) |
| CSF diversion procedures | 18 (16.2%) | 16 (30.2%) |
| Degenerative spine | 9 (8.1%) | 0 (0%) |
| Head injury | 21 (18.9%) | 12 (22.6%) |
| Neurovascular (ruptured aneurysms) | 5 (4.5%) | 2 (3.8%) |
| Spinal infection | 0 (0%) | 1 (1.9%) |
| Spinal trauma | 6 (5.4%) | 3 (5.7%) |
| Spinal tumour | 6 (5.4%) | 2 (3.8%) |
| Stroke | 2 (1.8%) | 2 (3.8%) |
| Miscellaneous | 6 (5.4%) | 2 (3.8%) |
Fig. 1.
Vertical stacked bar graph depicting the number of elective and emergency surgeries performed between 25th March and 31st May, in 2019 and 2020. The total number of surgeries at our department decreased by 52.2% as compared to last year. The proportion of non-emergent cases decreased from 57.7% in 2019 to 11.3% in 2020. This change was found to be statistically significant (p value = 0.000).
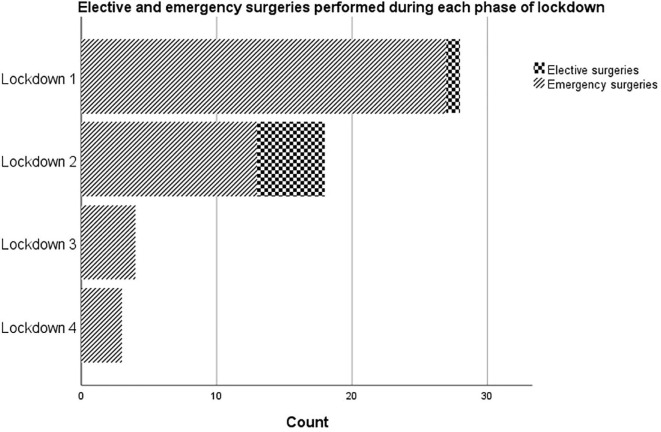
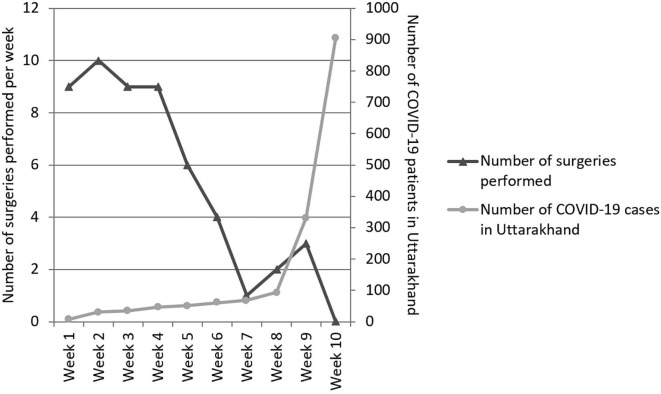
When the number of cases done during the COVID-19 related lockdown was analyzed according to the four phases of lockdown, 28 (52.8%) surgeries were performed during Phase I, 20 (37.7%) during Phase II, 2 (3.7%) during Phase III and 3 (5.6%) during Phase IV. No elective cases were done during lockdown III and IV (Fig. 2 ). When this data was correlated with the number of COVID-19 positive patients in the state, it was found that at the end of Phase I, there were 37 COVID-19 positive cases in Uttarakhand, 60 at the end of Phase 2, 92 at the end of Phase 3 and 907 at the end of Phase 4. When the number of COVID-19 cases in the state were compared with the number of surgeries performed per week, it was observed that the number of surgeries performed declined steadily as the number of COVID-19 cases rose in the state. This finding was found to be statistically significant (p value = 0.000, correlation coefficient = −0.914) (Fig. 3 ).
Fig. 2.
Horizontal stacked bar graph depicting the number of elective and emergency surgeries performed in each phase of lockdown. 28 (52.8%) surgeries were performed during Phase I, 20 (37.7%) during Phase II, 2 (3.7%) during Phase III and 3 (5.6%) during Phase IV. No elective cases were done during lockdown III and IV.
Fig. 3.
Frequency polygon depicting the number of surgeries performed in relation to the rising trend of COVID-19 cases in Uttarakhand from March 25th to May 31st 2020. The number of surgeries performed decreased as the number of COVID-19 cases rose (p value = 0.000, correlation coefficient = −0.914).
During the COVID-19 pandemic in 2020, twenty-two cases (41.5%) were minor cases (burr hole tapping of abscess/chronic subdural hemorrhage, ventriculoperitoneal shunt, external ventricular drainage, endoscopic third ventriculostomy, lumbar discectomy), while 31 (58.5%) were major cases. During the same duration in 2019, 32 (28.8%) were minor cases and 79 (71.2%) were major cases. This showed an increase in proportion of minor cases from 28.8% to 41.5%. However, this result could not reach statistical significance (p = 0.106) (Table 1).
3.1. Speciality-wise distribution
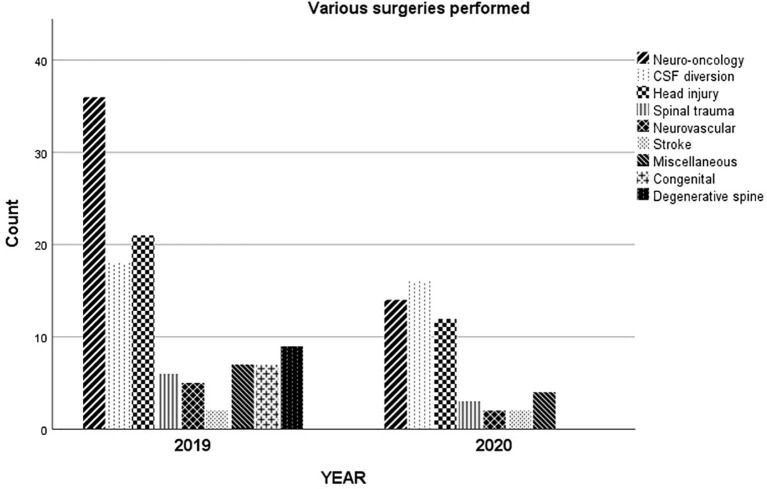
The proportion of cranial cases increased from 71.2% in pre-COVID-19 era to 88.7% during the COVID-19 pandemic. The proportion of spinal cases decreased from 27.9% to 11.3%. This finding was found to be statistically significant (p value = 0.043) (Table 1). Overall, majority of cases in the study were of neuro-oncology (30.5%), neuro-trauma (25.6%) and CSF diversion procedures (20.7%). The number of neuro-oncology decreased from 36 (30 cranial, 6 spinal) in pre-COVID-19 era to 14 (12 cranial, 2 spinal) during the COVID-19 lockdown. Overall, four cases of brain tumor were operated by the trans-sphenoidal route (three in pre-COVID-19 era and one during COVID-19 era). Neuro-trauma cases also reduced from 27 (21 head injuries, 6 spinal injuries) in this duration in 2019 to 15 (12 head injuries, 3 spinal injuries) during the pandemic. Two cases underwent surgical clipping of intra-cranial aneurysms during COVID-19-related lockdown as compared to five cases during the same duration last year. Similarly, no patient underwent surgery for congenital condition or degenerative spinal disorders during the lockdown period, whereas seven congenital conditions and nine degenerative spine cases were operated during the same duration last year. The number of cases for CSF diversion did not change much (18 in pre-COVID-19 times while 16 in COVID-19 times) (Fig. 4 ).
Fig. 4.
Clustered bar graph depicting the speciality-wise distribution of surgeries performed between March 25th to May 31st in 2019 and 2020. A reduction in all specialities is observed. No surgeries for congenital conditions and degenerative spinal conditions were performed during the period of the lockdown.
COVID-19 testing was made available in our institute from March 30th, 2020 while from April 25th, 2020 onwards, it was made a pre-requisite for those undergoing any surgery. Following that, 12 surgeries were performed of which seven were done with pre-operative COVID-19 testing. Five cases were taken up as emergency without pre-operative testing. In these five cases, testing was done following the surgery. Test results of all cases were negative. Repeat testing was done for a patient of cervical Potts’ spine who continued to have fever post-operatively. The repeat test for this patient was also negative.
4. Discussion
The COVID-19 pandemic has taken the world by storm. It has shaken up the lives of almost everyone, medical professionals being the worst affected. It has put healthcare workers in the tough situation of protecting themselves from the very patients they are trying to protect. Recognizing the potential tsunami of COVID-19 cases to come, the following changes were made in our institution in mid-to-late March: 1) out-station leaves of all physicians and health-care workers (HCWs) were cancelled to prevent the community spread of COVID-19 as well as to keep maximum work-force available at the hospitals; 2) the surgical workflow including neurosurgery was changed dramatically by the cancellation of elective surgery cases in order to increase hospital capacity for future COVID-19 patients; 3) all non-emergency outpatient visits were attended to via tele-medicine; 4) decreased staffing in all departments to preserve work-force and prevent fatigue; 5) all physical meetings in the hospital were either cancelled or replaced by virtual meetings; 6) authorized and implemented remote work for clinical, resident, and support staff; 7) restricted all visitors to our facilities; 8) requirement of every employee on-site to wear face-mask protection and to attest daily to symptom-free status; 9) created new virtual COVID-19 related educational programs for HCWs.
Subsequently, the hospital was divided into COVID-19 and non-COVID-19 areas. A screening OPD was developed where every incoming patient was screened for COVID-19-related symptoms and travel history, thermal screening was made available and subsequently COVID-19 testing was started at our institution on March 30th, 2020. A large section of the hospital was prepared for testing and admitting COVID-19 confirmed/suspected patients. These areas had designated areas for donning at entry and doffing at exit. The bio-medical waste management protocols were re-defined according to the latest scientific literature. Faculty, residents, nurses and support-staff from various clinical departments were re-deployed in these COVID-19 related areas. The non-COVID-19 part of the hospital deals with the patients who have been tested COVID-19 negative and are planned for further management related to their condition.
At our centre, all patients getting admitted to the hospital for elective surgery now require COVID-19 testing. Surgery for those who test positive for COVID-19 should be postponed until test results are negative, where possible. This is supported by evidence from a seminal article where it was shown that in patients with peri-operative COVID-19 infection, 30-day mortality of elective surgery was 23.8% and pulmonary complications were seen in 51.2% cases [6], [7], [8]. Once a patient tests negative for COVID-19, he is shifted to the non-COVID-19 area and undergoes surgery in the designated non-COVID-19 operation room. For patients who do require urgent surgery, they are assumed to be COVID-19 positive until proven otherwise, and managed accordingly in the operation room in the COVID-19 area. In accordance with this, a level-III personal protective equipment (PPE) is worn by all those in the operation room (OR). This is to mitigate the possible risk of operating on asymptomatic COVID-19-positive patients, which will increase as community prevalence increases, and in the absence of preoperative COVID-19 testing. Such patients undergo COVID-19 testing in the post-operative period and are shifted to the non-COVID-19 area only after testing negative for COVID-19. Twelve of our cases done during COVID-19 pandemic underwent COVID-19 testing. Five of these were operated in COVID-19 ORs, with HCWs wearing level-III PPE as they required urgent surgery and could not wait for COVID-19 testing.
Even now, in the steep part of the COVID-19 incidence curve, we are continuously mobilizing more space, including converting our regular wards to intensive care units and mobilizing more provider staff to join COVID-19 care teams as necessary. Similar measures have been taken by various institutions and hospitals around the world. Most hospitals in the USA have restricted all non-essential elective surgeries and procedures in accordance with recommendations from the American College of Surgeons (ACS) and Centres for Medicare and Medicaid Services [10], [11]. Many hospitals around the world have reported a drastic drop in non-emergent surgeries [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24]. In our study, the total number of surgeries since the onset of COVID-19 pandemic decreased by about half. This can be attributed to the national lockdown, transition of physical OPD to tele-medicine and as per recommendations of the various surgical bodies as mentioned above. During normal times, an average number of 11.1 neurosurgery cases are done every week at our department as shown by data of last year. At our institute, 58 less neurosurgery cases were done during the 10 weeks of COVID-19 pandemic as compared to pre-COVID times. In simple terms, this means that if we increase our surgical volume by 20% after the pandemic is over, it will take us 26.4 weeks to clear these 58 cases.
According to an estimate, 28,404,603 operations would be cancelled or postponed globally during the peak 12 weeks of disruption due to the COVID-19 pandemic, accounting for 72.3% cancellation rates overall. It was calculated that a median of 45 weeks will be required to clear the backlog of operations resulting from this disruption if the normal surgical volume was increased by 20% post-pandemic [18]. Moreover, this decrease in surgical volume does not appear to be normalizing anytime soon as large sections of the hospitals are now being dedicated for isolation of COVID-19 suspect and positive patients, thereby limiting the beds available for routine neurosurgery work.
In a national survey conducted by the authors on neurosurgeons, there was a 70% decrease in the number of surgeries performed as well decrease in the proportion of elective surgeries from 72% to 42% during the COVID-19 era all over the country [6]. In our study, the proportion of elective surgeries performed has decreased to 11.3% during the COVID-19 pandemic as compared to 57.7% during the same time-frame in 2019.
As per ACS guidelines, elective, non-urgent spine surgery has a Tier 2 rating with a recommendation to postpone the procedure, if possible [9], [25]. Similar trend has been seen in the present study, where the proportion of spinal surgeries has decreased from 27.9% to 11.3% during the COVID-19 pandemic. In various neurosurgical centers, functional neurosurgery, unruptured aneurysm surgery, spine surgery, benign tumors, and other less urgent surgical cases have been postponed [14]. In our study, the number of CSF diversion procedures and procedures for stroke and abscesses were largely unchanged, while there was a reduction in all other cases, including neuro-oncology, congenital and degenerative spine cases. In general, the postponement of surgeries considered ‘elective’ is likely to result in the progression of the disease, hence rendering patients more difficult to manage. Interestingly, the number of neuro-trauma and neuro-vascular cases also decreased in our study in spite of being emergency procedures. The decrease in neuro-trauma case-load can be attributed to decreased road traffic accidents during the national lockdown. However, decrease in number of ruptured aneurysm surgeries raises the possibility that some patients requiring urgent intervention could not reach the hospital.
In neurosurgery, highest risk for COVID-19 is posed by aerosol-generating procedures (AGPs) such as endonasal surgeries and surgeries requiring extensive drilling like skull base surgeries [26]. Endonasal AGPs theoretically present a higher risk of viral exposure than intubation due to the aggressive disruption of potentially virus-containing mucosa and longer duration of exposure in these procedures than during intubation [27]. Viral shedding has been found to be higher in the upper respiratory tract and, once aerosolized, virus particles remain airborne for more than 3 hours [28], [29]. In the survey conducted by the authors, almost 80% neurosurgeons were against doing endo-nasal procedures during the COVID-19 pandemic [6]. At our centre, endo-nasal surgeries are being avoided largely. These procedures, if need to be done, should be performed only after testing negative for COVID-19 and with full personal protective equipment (PPE) in a negative pressure operation room. Informal UK and US advisories have recommended the use of powered, air-purifying respirators (PAPRs) for all operating room staff during conduct of high-risk AGPs, and have suggested that an N95 mask and eye protection may not offer full protection. This was based on reports from Wuhan, China, that there was a high infection rate among ENT surgeons, and that the use of PAPRs anecdotally reduced the rate of transmission [27]. Similarly, prolonged surgeries with extensive bone drilling increase the exposure to those present in the operation rooms. In our institute, major surgeries have decreased and a large proportion of surgeries performed comprised of minor cases. This is another major change during the ongoing pandemic.
The decreased volume and limited spectrum of neurosurgery cases has affected neurosurgery training adversely. The reduction in clinical and surgical exposure is likely to hamper their operative and clinical skills [30], [31]. Departments must take it upon themselves to ensure that each surgery is utilised to its maximum teaching capacity. Videos of previously operated cases may be re-visited via video-conferencing to overcome this draught in surgical exposure.
5. Conclusions
With restricted public movement during the ongoing COVID-19 pandemic and re-delegation of resources and personnels to deal with COVID-19, there has been a major drop in the number of non-emergent surgeries performed. There is a risk of these patients presenting at a later stage with progressed disease and therefore, an alternative to postponing elective surgeries should be found. The best way forward would be to resume work with necessary precautions and universal effective COVID-19 testing.
Source of support
Nil.
Disclosures
None.
Conflict of interest
None.
References
- 1.Kim K.H., Choi E.H., Kim S.-K. Editorial. COVID-19 outbreak and its countermeasures in the Republic of Korea. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reid D. India confirms its first coronavirus case. CNBC 2020. https://www.cnbc.com/2020/01/30/india-confirms-first-case-of-the-coronavirus.html (accessed June 21, 2020).
- 3.DehradunMarch 15 PT of I, March 15 2020UPDATED: Ist 2020 23:04. Uttarakhand reports first coronavirus case. India Today n.d. https://www.indiatoday.in/india/story/uttarakhand-reports-first-coronavirus-case-1655825-2020-03-15 (accessed June 21, 2020).
- 4.MoHFW | Home n.d. https://www.mohfw.gov.in/ (accessed June 21, 2020).
- 5.Over 8 lakh case count if no lockdown, MEA cites ICMR; Health says no such report. The Indian Express 2020. https://indianexpress.com/article/coronavirus/over-8-lakh-case-count-if-no-lockdown-mea-cites-icmr-health-says-no-such-report-6357154/ (accessed June 21, 2020).
- 6.Venkataram T, Goyal N, Dash C, Chandra PP, Chaturvedi J, Raheja A. Impact of the COVID-19 Pandemic on Neurosurgical Practice in India: Results of an anonymized national survey. Neurol. India. 2020;68(3):595. doi: 10.4103/0028-3886.289004. [DOI] [PubMed] [Google Scholar]
- 7.Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020. https://doi.org/10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed]
- 8.Shelar J. Why it’s safer to postpone elective surgery. The Hindu. 2020 [Google Scholar]
- 9.COVID-19: Elective Case Triage Guidelines for Surgical Care n.d. https://www.facs.org/covid-19/clinical-guidance/elective-case. (accessed June 12, 2020).
- 10.CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures during COVID-19 Response | CMS. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental (accessed June 12, 2020).
- 11.Tomlinson S.B., Hendricks B.K., Editorial C.-G. Innovations in neurosurgical education during the COVID-19 pandemic: is it time to reexamine our neurosurgical training models? J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.After PM Modi’s Covid-19 appeal, footfall in Delhi hospitals decreases – India News – Hindustan Times n.d. https://www.hindustantimes.com/india-news/after-pm-s-covid-19-appeal-footfall-in-delhi-hospitals-decreases/story-Kl6LjnQcDuPzxvNaProYtK.html (accessed May 31, 2020).
- 13.Amin-Hanjani S., Bambakidis N.C., Barker F.G., Carter B.S., Cockroft K.M., Du R. COVID-19 and neurosurgical practice: an interim report. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bambakidis N.C., Tomei K.L. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.3.JNS20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernstein M. Editorial. Neurosurgical priority setting during a pandemic: COVID-19. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carter B.S., Chiocca E.A. Editorial. COVID-19 and academic neurosurgery. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi B.D. Editorial. A neurosurgery resident’s response to COVID-19: anything but routine. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CovidSurg Collaborative. Nepogodiev D., Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans: Elective surgery during the SARS-CoV-2 pandemic. Br J Surg. 2020 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fontanella M.M., De L., Maria, Zanin L., Saraceno G., Terzi di L., Bergamo, Servadei F. Neurosurgical practice during the SARS-CoV-2 pandemic: a worldwide survey. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghogawala Z., Kurpad S., Falavigna A., Groff M.W., Sciubba D.M., Wu J.-C. COVID-19 and spinal surgery. J Neurosurg: Spine. 2020;1:1–3. doi: 10.3171/2020.4.SPINE20468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee Z.D., Yeu D.L.C., Ang B.T., Ng W.H., Seow W.T. Editorial. COVID-19 and its impact on neurosurgery: our early experience in Singapore. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prall J.A., Davis J.D., Jenkins N.R. Editorial. Community practice in the time of COVID-19. J Neurosurg. 2020;1:1–2. doi: 10.3171/2020.4.JNS201033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robertson F.C., Lippa L., Broekman M.L.D. Editorial. Task shifting and task sharing for neurosurgeons amidst the COVID-19 pandemic. J Neurosurg. 2020;1:1–3. doi: 10.3171/2020.4.JNS201056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiner H.L., Adelson P.D., Brockmeyer D.L., Maher C.O., Gupta N., Smyth M.D. Editorial. Pediatric neurosurgery along with Children’s Hospitals’ innovations are rapid and uniform in response to the COVID-19 pandemic. Journal of Neurosurgery. Pediatrics. 2020;1:1–3. doi: 10.3171/2020.4.PEDS20240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.March 17 O, 2020. COVID-19: Guidance for triage of non-emergent surgical procedures. American College of Surgeons n.d. https://www.facs.org/covid-19/clinical-guidance/triage (accessed May 11, 2020).
- 26.Gupta P., Muthukumar N., Rajshekhar V., Tripathi M., Thomas S., Gupta S.K. Neurosurgery and neurology practices during the Novel COVID-19 pandemic: A consensus statement from India. Neurology India. 2020;68:246. doi: 10.4103/0028-3886.283130. [DOI] [PubMed] [Google Scholar]
- 27.Lo Y.T., Teo N.W.Y., Ang B.T. Editorial. Endonasal neurosurgery during the COVID-19 pandemic: the Singapore perspective. J Neurosurg. 2020;1:1–3. doi: 10.3171/2020.4.JNS201036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van N., Doremalen, Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dash C, Venkataram T, Goyal N, Chaturvedi J, Raheja A, Singla R, et al. Neurosurgery training in India during COVID-19 pandemic: straight from the horse’s mouth. Neurosurgical Focus 2020 (Dec); Focus 20-537 (submitted for publication). [DOI] [PubMed]
- 31.Goyal N, Venkataram T, Dash C, Chandra PP. Letter to the Editor Regarding- Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.07.216. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]