Abstract
Background
Kinematic patterns after TKA can vary considerably from those of the native knee. It is unknown, however, if there is a relationship between a given kinematic pattern and patient satisfaction after TKA.
Questions/purposes
Is there an association between kinematic patterns as measured by AP translation during open kinetic chain flexion-extension and closed kinetic chain exercises (rising from a chair and squatting) and a custom aggregate of patient-reported outcome measures (PROMs) that targeted symptoms, pain, activities of daily living (ADL), sports, quality of life (QOL), and patient satisfaction after TKA?
Methods
Thirty patients who underwent TKA between 2014 and 2016 were tested at a minimum follow-up of 6 months. As three different implants were used, per implant the first 10 patients who presented themselves at the follow-up consultations and were able to bend the knee at least 90°, were recruited. Tibiofemoral kinematics during an open kinetic chain flexion-extension and closed kinetic chain exercises—rising from a chair and squatting—were analyzed using fluoroscopy. A two-step cluster analysis was performed, resulting in two clusters of patients who answered the Knee Injury and Osteoarthritis Outcome Score and the satisfaction subscore of the Knee Society Score questionnaires. Cluster 1 (CL1) consisted of patients with better (good-to-excellent) patient-reported outcome measures scores (high-PROMs cluster); Cluster 2 (CL2) consisted of patients with poorer scores (low-PROMs cluster). Tibiofemoral kinematics were compared between patients in these clusters by performing a Mann-Whitney U test with Bonferroni correction.
Results
Concerning open kinetic chain flexion-extension, there was no difference in kinematic patterns between the patients in the high-PROMs cluster and those in the low-PROMs cluster, with the numbers available. However, during the closed-chain kinetic exercises, medially, initial anterior translation (femur relative to tibia) was found in patients in Cluster 1 during early flexion, but in those in Cluster 2, translation was steeper and ran more anteriorly (CL1 -1.5 ± 7.3%; CL2 -8.5 ± 4.4%); mean difference 7.0% [95% CI 0.1 to 13.8]; p = 0.046). In midflexion, the femur did not translate anterior nor posterior in relation to the tibia, resulting in a stable medial compartment in Cluster 1, whereas Cluster 2 had already started translating posteriorly (CL1 -0.7 ± 3.5%; CL2 3.4 ± 3.6%; mean difference -4.1% [95% CI -7.0 to -1.2]; p = 0.008). There was no difference, with the numbers available, between the two clusters with respect to posterior translation in deep flexion. Laterally, there was small initial anterior translation in early flexion, followed by posterior translation in midflexion that continued in deep flexion. Patients in Cluster 1 demonstrated more pronounced posterior translation in deep flexion laterally than patients in Cluster 2 did (CL1 8.3 ± 5.2%; CL2 3.5 ± 4.5%); mean difference 4.9% [95% CI 0.6 to 9.1]; p = 0.026).
Conclusions
This study of total knee kinematics suggests that during closed kinetic chain movements, patients with poor PROM scores after TKA experience more anterior translation on the medial side followed by a medial mid-flexion instability and less posterior translation on the lateral side in deep flexion than patients with good PROM scores. The relationship of kinematic variations with patient-reported outcomes including satisfaction must be further elaborated and translated into TKA design and position. Reproduction of optimal kinematic patterns during TKA could be instrumental in improving patient satisfaction after total knee replacement. Future expansion of the study group is needed to confirm these findings.
Level of Evidence Level II, therapeutic study.
Introduction
TKA decreases pain and improves function in most patients with severe osteoarthritis who undergo the procedure [2, 20, 23]. But despite the fact that most patients improve after surgery, a substantial proportion—in the range of 10% to 30%—of these patients report some measure of dissatisfaction after TKA [6, 12, 27, 30, 39]. The inability to have a normal-seeming knee and awareness of the artificial joint in everyday life may be regarded as a setback in TKA for some patients [5, 36].
Kinematic patterns after TKA can vary considerably from those of the native knee. Previous kinematic studies have reported that during flexion, knees that have undergone TKA often display sudden anterior translation of the femur relative to the tibia, better known as paradoxical anterior motion [9, 10, 14, 33, 41, 46]. Numerous studies have examined this abnormal pattern [9, 10, 14, 33, 41, 46], but to our knowledge, an association between a given kinematic pattern and patient-reported outcome measures (PROMs) has yet to be explored.
Therefore, in this study, we asked: (1) Is there an association between kinematic patterns as measured by AP translation during open kinetic chain flexion-extension and closed kinetic chain exercises (rising from a chair and squatting) and custom aggregate of PROMs that targeted symptoms, pain, activities of daily living (ADL), sports, quality of life (QOL), and patient satisfaction after TKA?
Patients and Methods
We conducted a prospective, single-institution study at Ghent University Hospital, Belgium, to evaluate the influence of total knee kinematics on PROMs. We obtained institutional ethics committee approval, and all patients participating in this study provided informed consent. Thirty patients (20 women and 10 men) who underwent TKA between 2014 and 2016 and who were at least 6 months postoperative were recruited and participated in this study. As three different implants are used in our group, per implant, the first 10 patients who presented themselves at the follow-up consultation and who were able to bend their knee at least 90° were recruited. The patients had a mean age of 64 ± 9 years and a mean BMI of 27 ± 5 kg/m2. The diagnosis was osteoarthritis in all patients, and the procedures were performed by four senior surgeons (JV, NA, GVD, PD) using a similar standardized, adapted, measured resection technique as published earlier [21]. Three different posterior-stabilized TKA designs were used in this study: the Journey™ II Bi-Cruciate Stabilized knee system (Smith & Nephew, Memphis, TN, USA), Persona® knee system (Zimmer-Biomet, Warsaw, IN, USA), and the Unity™ knee system (Corin Ltd, Cirencester, UK). All patients received the same postoperative rehabilitation protocol for outpatient rehabilitation. Standard follow-up consultations were planned at 6 weeks, 3 months, 6 months, 12 months and 24 months after surgery.
Evaluation of Total Knee Kinematics
Fluoroscopic videos of each of the patients were captured in the sagittal plane using a static fluoroscopy machine (Siemens Axiom Luminos dRF, Erlangen, Germany).
Patients performed the following activities: for the open kinetic chain flexion-extension of the knee, the patient sat on a chair that was set at a height so his or her legs were off the ground. The patient was asked to extend and flex the knee as far as possible. For the closed kinetic chain exercises, patients performed weightbearing flexion-extension exercises in which they stood up from a chair with the knee initially in 90° of flexion and then sat down. If necessary, patients were allowed to support themselves by use of a handrail, though only limited support was allowed. Then, the patient squatted to maximum flexion without external support.
The patients were asked to perform each exercise three times, and the best sequence was selected. The best sequence was defined as the best-performed exercise that had a clear beginning and ending (that is, that the start and the end of the movement was captured by the fluoroscope).
Three flexion zones were defined: early flexion (0° to 30°), midflexion (30° to 60°), and deep flexion (60° to 90°). AP translations in each flexion zone were defined as the difference between the lowest and highest flexion angles.
The fluoroscopic videos were then cropped into relevant frames of interest. Kinematics were analyzed using the fluoroscopic images with a standard 2-D to 3-D image registration technique (open source software package Jointtrack, https://sourceforge.net/projects/jointtrack/, University of Florida, Gainesville, FL, USA).
In this technique, computer-aided design models are overlaid on the fluoroscopic images based on their silhouette to obtain transformation matrices of the computer-aided design models in the image space. This process was validated at our center and displayed errors of < 0.5° mm and 0.5 mm for in-plane rotations and translations, respectively [7].
Because the polyethylene tibial insert was radiolucent on fluoroscopic images and the implants used in this study were fixed-bearing, we assumed that the insert was rigidly connected to the tibial component.
We defined landmarks on the femoral and tibial components. Then we identified bearing surfaces of the femoral component and fit the spheres through the medial and lateral condyle. The centers of these spheres represented the medial and lateral centers, which we used as the origin for the description of medial and lateral translations. We defined the mediolateral and distal proximal directions of the femoral component based on the implant’s geometry as the dimensions perpendicular to the femoral intercondylar box geometry [7].
For the tibia, the proximal-distal direction was derived from the axis perpendicular to the tibial baseplate. Point 0 in the AP direction was defined as the posterior-most point of the tibial tray.
Based on the tibial and femoral component coordinate systems, we subsequently defined a joint coordinate system in accordance with the mathematical description of Grood and Suntay [15]. The fixed axes were represented by the mediolateral axis of the femoral component and the proximal-distal axis of the tibial component.
For AP translations, the relative positions of the medial and lateral femoral condyles were plotted on a tibial baseplate reference frame in terms of percentage locations of the AP length (0% and 100% correspond to the most-posterior and most-anterior locations, respectively) (Fig. 1).
Fig. 1.

The AP dimension of the tibial insert is shown; 0% and 100% correspond to the most-posterior and most-anterior locations, respectively.
During all three movements (open chain flexion/extension, closed chain chair rising and squat), the knee passes the same flexion angle twice. Therefore, we calculated the average of the flexion and extension phases.
Evaluation of PROMs
We used two PROM tools. The Knee Injury and Osteoarthritis Outcome Score [31] consists of 42 knee-related items, and each item is scored from 0 to 4. Five subscales of symptoms, pain, activities of daily living, sports, and quality of life were evaluated. A normalized score (100 indicating no symptoms and 0 indicating extreme symptoms) was calculated for each subscale. The 2011 Knee Society Score [28] consists of 34 questions divided into five subscales, which are rated separately; we used only the Satisfaction subscale (five items; 40 points) in this study. The higher the score, the better the satisfaction. Dutch translations of both scales have been validated for use in Dutch-speaking countries or regions including Flanders, where this study was conducted [8, 38].
To create a single differentiator, we grouped the patients into two clusters based on the PROM scores: Cluster 1 (CL1) consisted of patients (n = 21) with good-to-excellent PROM scores and Cluster 2 (CL2) consisted of patients (n = 9) with low-to-medium PROM scores (based on a cluster analysis and silhouette coefficient of 0.6, see below).
With the numbers available, there were no differences in age or gender between patients in the two clusters (Table 1). The BMI of patients in Cluster 1 was higher than that of patients in Cluster 2 (CL1: 30 ± 5 kg/m2; CL2: 25 ± 4 kg/m2), mean difference 4 [95% CI 0.60 to 7.74]; p = 0.024). When we compared the Knee Injury and Osteoarthritis Outcome Score and Knee Society Score subscales between the clusters, we found that patients in Cluster 1 had higher scores for all subscales than patients in Cluster 2 (Table 2). Therefore, for interpretation purposes, Cluster 1 was called the “high-PROMs cluster” and Cluster 2 was called the “low-PROMs cluster.”
Table 1.
Cluster-specific demographics
Table 2.
PROMs per cluster
Statistical Analysis
We performed the statistical analysis by using SAS 9.4 (SAS Institute Inc, Cary, NC, USA) and SPSS version 22 (IBM Corp, Armonk, NY, USA), with a 95% CI (α = 0.05).
We applied a uniform cluster method using an agglomerative two-step cluster analysis of the subscales of the Knee Injury and Osteoarthritis Outcome Score (Pain, Symptoms, Activities of Daily Life, Sports, and Quality of Life) and Knee Society Score (Satisfaction). The overall goodness-of-fit of the clusters was evaluated using the silhouette coefficient. A silhouette measure of less than 0.2 was classified as poor solution quality, between 0.2 and 0.5 as fair, and more than 0.5 as good; a good solution quality (0.6) was found in this study [32]. No power analysis was performed due to the lack of similar studies and the inability to predict how many patients will end up in each cluster.
After defining the clusters, we used Mann-Whitney U tests to compare between-group differences. To evaluate within-group differences, we constructed a mixed-effect model to evaluate the values of interest (difference in the AP position between movements and between certain flexion angles). A Bonferroni correction was applied for all tests. A chi-square test was used to compare categorical variables.
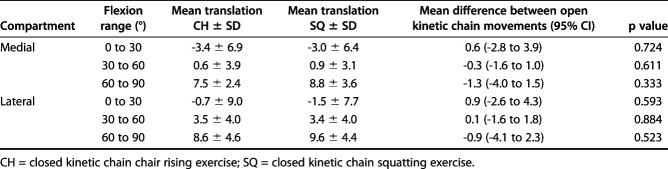
When evaluating the kinematics of the chair-rising exercise and the squatting movement, we found no difference in kinematics within the evaluated flexion range. Therefore, these movements were combined and reported as closed kinetic chain movements (Table 3).
Table 3.
Differences (percentage points) in AP translation during early (0° to 30°), mid (30° to 60°) and deep flexion (60° to 90°) between the chair rising and the squatting exercise
Results
Open Kinetic Chain Movements
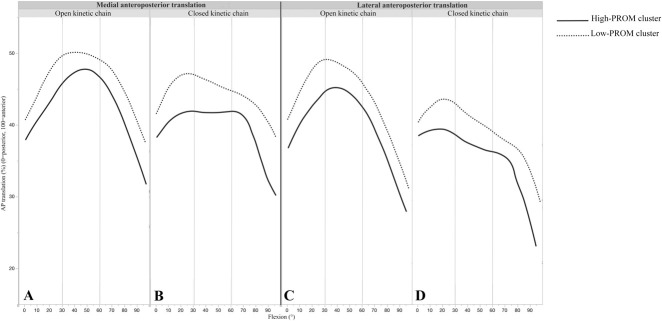
With the numbers available, we found that during open kinetic chain movements, there was no difference in kinematic patterns between the high-PROMs and low-PROMs clusters at each of the three flexion ranges for either the medial (Table 4) or lateral side (Table 5). Both clusters followed a similar pattern (Fig 2A-D).
Table 4.
Differences (percentage points) in medial translation during early (0° to 30°), mid (30° to 60°) and deep flexion (60° to 90°) between clusters 1 and 2 for open and closed kinetic chain movements
Table 5.
Differences (percentage points) in lateral translation during early (0° to 30°), mid (30° to 60°) and deep flexion (60° to 90°) between clusters 1 and 2 for open and closed kinetic chain movements
Fig. 2 A-D.
This graph shows the AP position of each flexion angle for (A) the medial compartment during the open kinetic chain movement, (B) the medial compartment during the closed kinetic chain movements, (C) the lateral compartment during the open kinetic chain movment and (D) the lateral compartment during the closed kinetic chain movements. The solid lines represent the high-PROMs cluster, dotted lines represent the low-PROMs cluster.
Closed Kinetic Chain Movements
From 0° to 30° of flexion, greater medial anterior translation was found in the low-PROMs cluster during the closed kinetic chain exercises than in the high-PROMs cluster (CL1 -1.5 ± 7.3; CL2 -8.5 ± 4.4); mean difference 7.0 [95% CI 0.1 to 13.8]; p = 0.046, Table 4). From 30° to 60° of flexion, there was a stable medial compartment in patients in the high-PROMs cluster, hence almost no translation, whereas there was posterior translation in patients in the low-PROMs cluster (CL1 -0.7 ± 3.5; CL2 3.4 ± 3.6; mean difference -4.1 [95% CI -7.0 to -1.2]; p = 0.008) (Table 4). From 60° to 90° of flexion, the high-PROMs cluster had more pronounced posterior translation laterally than the low-PROMs cluster (CL1 8.3 ± 5.2; CL2 3.5 ± 4.5; mean difference 4.9 [95% CI 0.6 to 9.1]; p = 0.026) (Table 5).
Discussion
Although numerous studies have investigated the kinematic patterns of the knee before and after TKA [4, 9–11, 14, 19, 22, 25, 33, 41, 46], to our knowledge none has evaluated the relationship between patient-reported outcomes and total knee kinematics. Therefore, this study sought to determine if there is an association between in vivo kinematics during open and closed kinetic chain movements in patients who underwent TKA and PROM subscales of symptoms, pain, activities of daily living, sports, quality of life, and patient satisfaction. We did not find an association between open kinetic chain kinematics and these PROM subscales; however, only one type of open kinetic chain movement was evaluated. Conversely, during closed kinetic chain movements, patients with poor PROM scores had a more pronounced anterior motion medially followed by a less stable medial compartment in midflexion and less posterior translation in deep flexion laterally during than patients with better PROM scores.
This study has some limitations. First, the numbers of surgeons and implants are possible confounders. As there are differences reported in kinematic patterns between different implants and surgeons [9, 41], this should be further evaluated. Unfortunately, in the current study, the number of patients with each implant type was too small to determine if implant type or surgeon affects the kinematic pattern. Also, other possible influencing factors such as implant alignment and coronal stability were not included in the evaluation; further analyses will be conducted to determine the influence of these factors. Although there were differences between patients in the clusters, the number of patients in the study was small, and more substantial comparisons might be drawn from larger patient groups. However, the nature of these intensive studies generally leads to study groups that are relatively small. The sizes of the groups in this study are comparable to those of other published studies using similar methods [10, 12, 13, 47].
Another remark should be made for a better understanding of the effect size of the presented data. It was reported that a difference of 2% points and 5% points resulted in a difference between the two clusters. However, as the total AP translation ranges between a maximum anterior point of about 50% (center of the tibia, due to the post-cam engagement) and a maximum posterior point of about 30%, this makes that this translation happens on about 20% of the tibial surface. In that way, this difference of 5% points and 2% points means that this is actually about 25% and 10% difference on the total AP translation. The use of a uniform cluster method using an agglomerative two-step cluster analysis of the subscales of the Knee Injury and Osteoarthritis Outcome Score (Pain, Symptoms, Activities of Daily Life, Sports, and Quality of Life) and Knee Society Score (Satisfaction) is something that is not yet commonly used in the orthopaedic evidence. However, this analysis method makes it straightforward to compare two (or more) groups of individuals that are more similar to each other than to patients in the other cluster without the need for hard cut-off points [29, 40].
Another limitation was that although there was a difference in BMI between patients in the two clusters, and patients with good-to-excellent PROM scores had a higher BMI than those with poorer scores, the study design did not allow us to make conclusions regarding the clinical relevance of this finding. Patients in both groups had a mean BMI between 25 and 30 kg/m2, which means they both can be classified in the overweight category. Furthermore, to our knowledge, no published studies have evaluated the influence of BMI on patient satisfaction or kinematic patterns. Lastly, the postoperative testing occurred during a relatively short period; however, published studies have shown that 6 months is a sufficient amount of time for postoperative recovery [14, 46]. Furthermore, studies conducted on implants at various timepoints after surgery have shown that in vivo kinematics do not change with time, especially during longer postoperative periods [19, 47].
When evaluating open kinetic chain movement, we did not see a difference in kinematic patterns between patients in the high-PROMs cluster and those in the low-PROMs cluster. However, there was a difference in kinematic patterns between open- and closed-kinetic chain movements. This implies that muscular activity and weightbearing conditions may be associated with the kinetic and kinematic patterns of the knee. This is in accordance with the findings of Horiuchi et al. [17] and Yoshiya et al. [44]. However, Zambianchi et al. [45] recently demonstrated that open- and closed-chain exercises do not show a different kinematic pattern. The authors attributed this to a design feature of their investigated total knee implant, implying that implant design strongly influences open kinetic chain movements.
Given that there was no difference in kinematic patterns during the open-chain exercises between patients in the two clusters in the current study and that our results are inconsistent with those of previous studies, our findings suggest that open-chain movements may not be as closely associated with patient-reported outcomes. This could possibly be due to the fact that most of our activities of daily living occur during weightbearing, closed kinetic chain, conditions.
In closed kinetic chain, weightbearing movements, the femur was located more anteriorly relative to the tibia during complete ROM in patients with low-PROM scores than in patients with high-PROM scores. Biomechanically, a more-anteriorly located femur leads to decreased lever arm mechanisms for knee extension. Because patients who undergo TKA have diminished quadriceps force [1, 13, 24, 35, 43], a decreased lever arm leads to reduced quadriceps efficiency. According to Furu et al. [13], there is a close relationship among quadriceps strength, physical function, and patient satisfaction, and we must acknowledge that reduced quadriceps efficiency may be associated with decreased PROM scores. Secondly, there was steeper and more pronounced paradoxical anterior motion on the medial side in patients in the low-PROMs clusters than in patients in the high-PROMs cluster. Although patients in both clusters had initial anterior translation, which is also found in the native knee, this was more pronounced and ran more anterior in patients with poor-PROM scores than in patients with high-PROM scores.
Subsequently, in midflexion, patients in the low-PROMs cluster demonstrated sudden posterior translation, whereas the cluster of patients with high-PROMs scores had almost no change and a stable medial compartment in midflexion. Sudden posterior translation might be caused by abrupt post-cam engagement, but further research should confirm this assumption. Because larger translation is seen during midflexion, this might be linked to midflexion instability. Instability was the third-leading cause of revision TKA in several studies [7, 18, 37]. Because the number of revision procedures is growing, reasons for revision such as instability demand greater attention from the orthopaedic community. Because satisfactory improvement in patient-reported outcomes was noted after revision surgery for instability and 70% of patients in one study reported perceptible improvement [18], a relationship between stability and satisfaction is not surprising. Future studies could evaluate preoperative stability at different flexion angles and determine if there is a correlation with the postoperative kinematic pattern.
Patients in the high-PROMs cluster had posterior translation greater than 50° to 60°. This finding can be explained by the engagement of the post-cam mechanism, which has been described to be approximately this value for used implants [3]. In the native knee, the posterior cruciate ligament is functional at greater than 50° of flexion, which forces the femoral condyles to run posteriorly [37]. Our findings support the thinking that patients whose knees mimic this native-knee kinematic rollback pattern on the medial side appear to have higher PROM scores than patients whose knees do not exhibit this pattern.
Lastly, there was more pronounced posterior translation in the lateral compartment in patients in the high-PROMs cluster than in patients in the low-PROMs cluster. In the native knee, posterior femoral rollback during knee bending occurs regularly [16, 42]. Implant kinematics that mimic those of the normal knee might induce an improved quadriceps lever arm in deep flexion that allows for better function. More-posterior femoral rollback delays posterior impingement between the femur and posterior aspect of the tibial component, allowing increased knee flexion to occur [9].
Although understanding kinematics is important, our knowledge of the correlation between kinematics and patient satisfaction is still in its infancy. The few studies that have addressed this topic evaluated the intraoperative kinematics of the knees of patients under anesthesia and during passive motion and incomplete closure during arthrotomy [26, 42]. This might be the cause of the inconsistent results. One of these studies [28] found that functional activities, knee flexion angle, and patient satisfaction were better in patients with a medial pivot pattern. Another study [42] stated that a medial pivot pattern may not be a substantial indicator of clinical success. With our study of total knee kinematics, we have demonstrated that during the closed kinetic chain movements, patients with low PROM scores after TKA experience more pronounced anterior motion on the medial side followed by a medial mid-flexion instability and less posterior translation on the lateral side in deep flexion than patients with high PROM scores. The relationship of kinematic variations with patient-reported outcomes including satisfaction needs to be further elaborated and translated into TKA design and position. Reproduction of optimal kinematic patterns during TKA could be instrumental in improving patient satisfaction.
Acknowledgments
We thank Mr. G. Byttebier for his assistance with the statistical analysis. Nele Arnout MD, Geert Van Damme MD, and Patrick Deprez MD, for their cooperation as senior surgeons. We also thank Delphine Lambrecht MD for her help during the organization of the study.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Ghent University Hospital, Ghent, Belgium.
The first two authors contributed equally to this manuscript.
References
- 1.Alnahdi AH, Zeni JA, Snyder-Mackler L. Quadriceps strength asymmetry predicts loading asymmetry during sit-to-stand task in patients with unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2587–2594. [DOI] [PubMed] [Google Scholar]
- 2.Arden N, Nevitt MC. Osteoarthritis: Epidemiology. Best Pract Res Clin Rheumatol . 2006;20:3–25. [DOI] [PubMed] [Google Scholar]
- 3.Arnout N, Vanlommel L, Vanlommel J, Luyckx JP, Labey L, Innocenti B, Victor J, Bellemans J. Post-cam mechanics and tibiofemoral kinematics: a dynamic in vitro analysis of eight posterior-stabilized total knee designs. Knee Surg Sports Traumatol Arthrosc . 2015;23:3343–3353. [DOI] [PubMed] [Google Scholar]
- 4.Banks SA, Harman MK, Bellemans J, Hodge WA. Making sense of knee arthroplasty kinematics: news you can use. J Bone Joint Surg Am . 2003;85-A Suppl:64–72. [DOI] [PubMed] [Google Scholar]
- 5.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The ‘Forgotten Joint’ as the Ultimate Goal in Joint Arthroplasty. Validation of a New Patient-Reported Outcome Measure. J Arthroplasty. 2012;27:430-436.e1. [DOI] [PubMed] [Google Scholar]
- 6.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res . 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daems R, Victor J, De Baets P, Van Onsem S, Verstraete M. Validation of three-dimensional total knee replacement kinematics measurement using single-plane fluoroscopy. Sustain Constr Des . 2016;7:1–14. [Google Scholar]
- 8.De Groot IB, Favejee MM, Reijman M, Verhaar JAN, Terwee CB. The dutch version of the knee injury and osteoarthritis outcome score: A validation study. Health Qual Life Outcomes . 2008;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Conventry Award Paper: Multicenter Determination of In Vivo Kinematics After Total Knee Arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. [DOI] [PubMed] [Google Scholar]
- 10.Dennis DA, Komistek RD, Stiehl JB, Walker SA, Dennis KN. Range of motion after total knee arthroplasty: The effect of implant design and weight-bearing conditions. J Arthroplasty. 1998;13:748–752. [DOI] [PubMed] [Google Scholar]
- 11.Digennaro V, Zambianchi F, Marcovigi A, Mugnai R, Fiacchi F, Catani F. Design and kinematics in total knee arthroplasty. Int Orthop . 2014;38:227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunbar MJ, Richardson G, Robertsson O. I can’t get no satisfaction after my total knee replacement: rhymes and reasons. Bone Joint J. 2013;95 B:148–152. [DOI] [PubMed] [Google Scholar]
- 13.Furu M, Ito H, Nishikawa T, Nankaku M, Kuriyama S, Ishikawa M, Nakamura S, Azukizawa M, Hamamoto Y, Matsuda S. Quadriceps strength affects patient satisfaction after total knee arthroplasty. J Orthop Sci . 2016;21:38–43. [DOI] [PubMed] [Google Scholar]
- 14.Grieco TF, Sharma A, Komistek RD, Cates HE. Single Versus Multiple-Radii Cruciate-Retaining Total Knee Arthroplasty: An In Vivo Mobile Fluoroscopy Study. J Arthroplasty . 2016;31:694–701. [DOI] [PubMed] [Google Scholar]
- 15.Grood ES, Suntay WJ. A Joint Coordinate System for the Clinical Description of Three-Dimensional Motions: Application to the Knee. J Biomech Eng . 1983;105:136. [DOI] [PubMed] [Google Scholar]
- 16.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MAR. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br . 2000;82:1196–1198. [DOI] [PubMed] [Google Scholar]
- 17.Horiuchi H, Akizuki S, Tomita T, Sugamoto K, Yamazaki T, Shimizu N. In Vivo Kinematic Analysis of Cruciate-Retaining Total Knee Arthroplasty During Weight-Bearing and Non-Weight-Bearing Deep Knee Bending. J Arthroplasty. 2012. [DOI] [PubMed] [Google Scholar]
- 18.Kannan A, O’Connell RS, Kalore N, Curtin BM, Hull JR, Jiranek WA. Revision TKA for flexion instability improves patient reported outcomes. J Arthroplasty. 2015;30:818–821. [DOI] [PubMed] [Google Scholar]
- 19.LaCour MT, Sharma A, Carr CB, Komistek RD, Dennis DA. Confirmation of long-term in vivo bearing mobility in eight rotating-platform TKAs. Clin Orthop Relat Res . 2014;472:2766–2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liddle AD, Pegg EC, Pandit H. Knee replacement for osteoarthritis. Maturitas . 2013;75:131–136. [DOI] [PubMed] [Google Scholar]
- 21.Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? Bone Joint J . 2012;94-B:1271–1276. [DOI] [PubMed] [Google Scholar]
- 22.Meccia B, Komistek RD, Mahfouz M, Dennis D. Abnormal axial rotations in TKA contribute to reduced weightbearing flexion knee. Clin Orthop Relat Res . 2014;472:248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michael JW, Schluter-Brust KU, Eysel P. The Epidemiology, Etiology, Diagnosis, and Treatment of Osteoarthritis of the Knee. Dtsch Arztebl Int . 2010;107:152–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mizner RL, Billing S. Quadriceps Strength and the Time Course. 2003. [Google Scholar]
- 25.Mochizuki T, Sato T, Blaha JD, Tanifuji O, Kobayashi K, Yamagiwa H, Watanabe S, Matsueda M, Koga Y, Omori G, Endo N. Kinematics of the knee after unicompartmental arthroplasty is not the same as normal and is similar to the kinematics of the knee with osteoarthritis. Knee Surg Sports Traumatol Arthrosc . 2014;22:1911–1917. [DOI] [PubMed] [Google Scholar]
- 26.Nishio Y, Onodera T, Kasahara Y, Takahashi D, Iwasaki N, Majima T. Intraoperative Medial Pivot Affects Deep Knee Flexion Angle and Patient-Reported Outcomes After Total Knee Arthroplasty. J Arthroplasty. 2014;29:702–706. [DOI] [PubMed] [Google Scholar]
- 27.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res . 2006;452:35–43. [DOI] [PubMed] [Google Scholar]
- 28.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, Chadha P, Daylamani DA, Scott WN, Bourne RB. Development of a new knee society scoring system. Clin Orthop Relat Res . 2012;470:20–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reutter A. TwoStep Cluster Analysis. IBM Software, Bus. Anal. SPSS. 2003:1–5. [Google Scholar]
- 30.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand . 2000;71:262–267. [DOI] [PubMed] [Google Scholar]
- 31.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a Self-Administered Outcome Measure. J Orthop Sport Phys Ther . 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 32.Schutz T. Erik Mooi and Marko Sarstedt - A concise guide to market research: the process, data and methods using IBM SPSS statistics. Int J Mark Res . 2011;53:563. [Google Scholar]
- 33.Scott G, Imam MA, Eifert A, Freeman MAR, Pinskerova V, Field RE, Skinner J, Banks SA. Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilised?A pulsed fluoroscopic investigation. Bone Joint Res . 2016;5:80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res . 2002:7–13. [DOI] [PubMed] [Google Scholar]
- 35.Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG. Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res . 2010;468:2460–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thienpont E, Opsomer G, Koninckx A, Houssiau F. Joint awareness in different types of knee arthroplasty evaluated with the forgotten joint score. J Arthroplasty . 2014;29:48–51. [DOI] [PubMed] [Google Scholar]
- 37.Toutoungi DE, Lu TW, Leardini A, Catani F, O’Connor JJ. Cruciate ligament forces in the human knee during rehabilitation exercises. Clin Biomech . 2000;15:176–187. [DOI] [PubMed] [Google Scholar]
- 38.Van Der Straeten C, Witvrouw E, Willems T, Bellemans J, Victor J. Translation and validation of the Dutch New Knee Society Scoring System©. Clin Orthop Relat Res . 2013;471:3565–3571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Onsem S, Van Der Straeten C, Arnout N, Deprez P, Van Damme G, Victor J. A New Prediction Model for Patient Satisfaction After Total Knee Arthroplasty. J Arthroplasty. 2016;31:2660-2667.e1. [DOI] [PubMed] [Google Scholar]
- 40.Van Onsem S, Verstraete M, Dhont S, Zwaenepoel B, Van Der Straeten C, Victor J. Improved walking distance and range of motion predict patient satisfaction after TKA. Knee Surg Sport Traumatol Arthrosc . 2018:1–8. [DOI] [PubMed] [Google Scholar]
- 41.Victor J, Mueller JKP, Komistek RD, Sharma A, Nadaud MC, Bellemans J. In vivo kinematics after a cruciate-substituting TKA. Clin Orthop Relat Res . 2010;468:807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM. Do Medial Pivot Kinematics Correlate With Patient-Reported Outcomes After Total Knee Arthroplasty? J Arthroplasty. 2017;32:2411–2416. [DOI] [PubMed] [Google Scholar]
- 43.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech . 2008;23:320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M. In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty. 2005. [DOI] [PubMed] [Google Scholar]
- 45.Zambianchi F, Fiacchi F, Lombari V, Venturelli L, Marcovigi A, Giorgini A, Catani F. Changes in total knee arthroplasty design affect in-vivo kinematics in a redesigned total knee system: A fluoroscopy study. Clin Biomech . 2018;54:92–102. [DOI] [PubMed] [Google Scholar]
- 46.Zeller IM, Sharma A, Kurtz WB, Anderle MR, Komistek RD. Customized versus patient-sized cruciate-retaining total knee arthroplasty: an in vivo kinematics study using mobile fluoroscopy. J Arthroplasty. 2017;32:1344–1350. [DOI] [PubMed] [Google Scholar]