Abstract
Background
Successful brace treatment entails good control of scoliosis with avoidance of surgery. However, achieving curve regression may be an even better radiological result than prevention of curve progression for patients with adolescent idiopathic scoliosis. Vertebral remodeling may occur with well-fitted braces. Better in-brace curve correction may influence the likelihood of vertebral remodeling and the chance of curve regression. Only a few reports have evaluated curve regression with brace treatment, and the factors associated with these events are unknown.
Questions/purposes
(1) What changes in curvature are observed with brace treatment for adolescent idiopathic scoliosis? (2) What factors are associated with curve improvement? (3) What factors are associated with curve deterioration? (4) Is curve regression associated with improvements in patient-reported objective outcome scores?
Methods
Between September 2008 and December 2013, 666 patients with adolescent idiopathic scoliosis underwent underarm brace treatment and were followed until skeletal maturity at 18 years old. Among these patients, 80 were excluded because of early discontinuation of brace treatment (n = 66) and loss to follow-up (n = 14). Hence, 586 patients were included in this study, with a mean brace-wear duration of 3.8 ± 1.5 years and post-weaning follow-up duration of 2.0 ± 1.1 years. The mean age at baseline was 12.6 ± 1.2 years. Most patients were female (87%, 507 of 586) and up to 53% (267 of 507) of females were post-menarche. Bracing outcomes were based on changes in the Cobb angle measured out of brace. These included curve regression, as indicated by at least a 5° reduction in the Cobb angle, curve progression, as indicated by at least a 5° increase in the Cobb angle, and unchanged, as indicated by a change in the Cobb angle of less than 5°. We studied the pre-brace and supine Cobb angles, curve flexibility (pre-brace Cobb angle – supine Cobb angle / pre-brace Cobb angle x 100%), correction rate (pre-brace Cobb angle – in-brace Cobb angle / pre-brace Cobb angle x 100%), location of apical vertebrae, apical ratio (convex vertebral height/concave vertebral height), change in the major curve Cobb angle, and apical ratio post-bracing. The refined 22-item Scoliosis Research Society questionnaire was used for patient-reported outcomes and is composed of five domains (function, pain, appearance, mental health and satisfaction with treatment). Its minimum clinically important difference, based on a scale from 0 to 5, has been quoted as 0.2 for pain, 0.08 for activity and 0.98 for appearance domains. Mental health has no quoted minimum clinically important difference for the adolescent idiopathic scoliosis population. Satisfaction with treatment is described based on improvement or deterioration in domain scores. Intergroup differences between bracing outcomes were evaluated with the Kruskal Wallis test. Univariate analyses of bracing outcomes were performed with a point-biserial correlation coefficient for continuous variables and Pearson’s chi-square test for categorical variables. Multivariate logistic regression models were created for improved and deteriorated outcomes. P values < 0.05 were considered significant.
Results
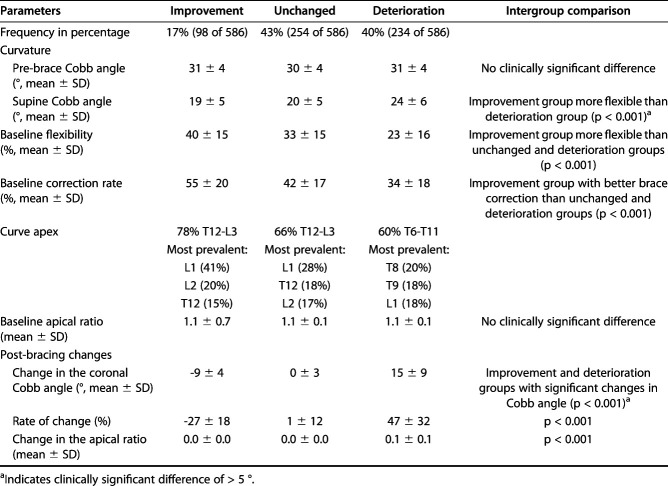
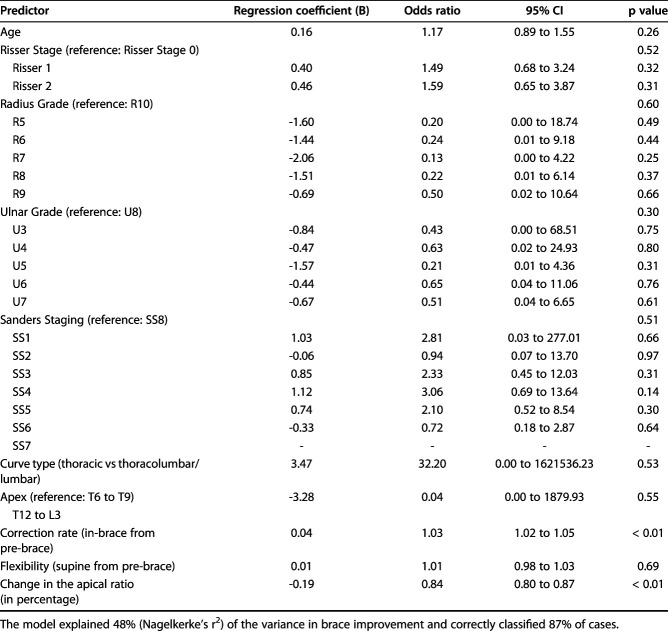
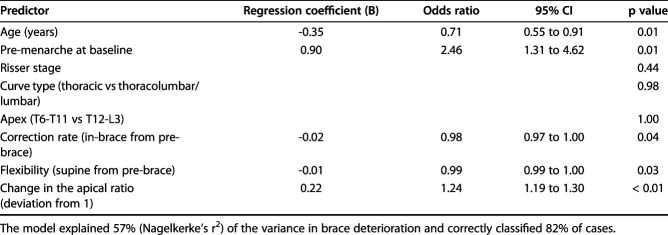
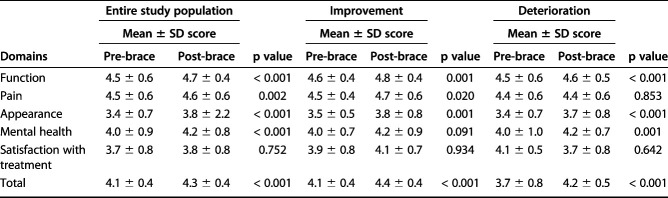
In all, 17% of patients (98 of 586) had an improved angle and 40% of patients (234 of 586) had curve deterioration. In patients who improved, the mean reduction in the Cobb angle was 9 ± 4°, while in patients who deteriorated, the mean increase in the Cobb angle was 15 ± 9°, and this was maintained at the latest post-brace weaning follow-up. Despite a trend for patients with curve regression to have higher baseline flexibility and correction rate, after controlling for age, Risser staging, radius and ulnar grading, and Sanders staging, we found no clinically important differences with increased correction rate or flexibility. We did find that improvement in the Cobb angle after bracing was associated with reduced apical ratio (odds ratio [OR] 0.84 [95% CI 0.80 to 0.87]; p < 0.001). Curve progression was associated with younger age (OR 0.71 [95% CI 0.55 to 0.91]; p = 0.008), pre-menarche status (OR 2.46 [95% CI 1.31 to 4.62]; p = 0.005), and increased apical ratio (OR 1.24 [95% CI 1.19 to 1.30]; p < 0.001) but no clinically important differences were observed with less flexible curves and reduced correction rate. Improvements in scores of the refined 22-item Scoliosis Research Society domains of function (mean difference on a scale from 0 to 5: 0.2; p = 0.001 versus 0.1; p < 0.001) and pain (mean difference on a scale from 0 to 5: 0.2; p = 0.020 versus 0.0; p = 0.853) were greater in the post-brace improvement group than in the deterioration group and fulfilled the minimum clinically important difference threshold. The appearance domain did not fulfill the minimum clinically important difference. Satisfaction with treatment domain score minimally improved with the curve regression group (mean difference on a scale from 0 to 5: 0.2) but deteriorated in the curve progression group (mean difference on a scale from 0 to 5: -0.4).
Conclusions
Curve regression occurs after underarm bracing and is associated with superior patient-reported outcome scores. This possible change in Cobb angle should be explained to patients before and during bracing. Whether this may help improve patients’ duration of brace-wear should be addressed in future studies. Patients with well-fitting braces may experience curve improvement and possible vertebral remodeling. Those braced at a younger age and with increased vertebral wedging are more likely to have curve progression.
Level of Evidence
Level III, therapeutic study.
Introduction
Bracing is the only commonly accepted treatment option with the potential to stop curve progression in patients with adolescent idiopathic scoliosis [47]. However, patients frequently have a poorer quality of life during brace treatment. Prolonged bracing can reduce spinal mobility, leading to poor body image and self-esteem and worse self-perceived function, pain, appearance, and mental health [13, 34, 35, 44, 46]. The Scoliosis Research Society proposed that bracing should only be considered to avoid progression and not to reduce the curve’s magnitude [38], Similarly, most studies only discussed the use of brace treatment to avoid curve progression [16, 17, 22, 23, 28, 29]. However, recent Society on Scoliosis Orthopaedic and Rehabilitation (SOSORT) guidelines suggested that bracing is both effective for preventing progression and improving curves at skeletal maturity [31]. Only a few studies with small study populations have suggested curve improvement during brace treatment of large curves [27, 32]. The prevalence of curve improvement with brace treatment and its determinants are currently unknown.
Spinal flexibility is a key factor for planning the treatment of adolescent idiopathic scoliosis. It provides useful information regarding the surgical strategy and outcome prediction [37, 40, 48]. Flexibility assessments can also help predict in-brace correction [12, 18]. Spines that are more flexible are likely to have better correction with orthotic treatment. Better in-brace curve correction may influence the end-of-treatment Cobb angle [45] and the Cobb angle at long-term follow-up [14]. However, this relationship and the factors associated with changes after brace treatment are not well understood. Well-fitting braces may induce vertebral remodeling, as evidenced by changes in the curve pattern [49]. Based on the Hueter-Volkman’s law, we suspect that patients with good in-brace correction may have improved curvature [42].
Thus, we asked, (1) What changes in curvature are observed with brace treatment for adolescent idiopathic scoliosis? (2) What factors are associated with curve improvement? (3) What factors are associated with curve deterioration? (4) Is curve regression associated with improvements in patient-reported objective outcome scores?
Patients and Methods
Study Design
Between September 2008 and December 2013, 666 patients with adolescent idiopathic scoliosis underwent custom molded underarm thoraco-lumbo-sacral orthosis (underarm brace) treatment and were followed until skeletal maturity at 18 years old. The study was approved by our institutional review board. All patients were referred for bracing according to the Scoliosis Research Society criteria: age between 10 years and 14 years, major curve magnitude of 25° to 40°, Risser Stage 0 to 2, less than 1 year post-menarche, and no previous treatment. Among 666 patients with a brace during this period, 80 (12%) were excluded (Fig. 1), 10% because of early brace discontinuation (66 of 666) and 2% because of loss to follow-up (14 of 666). Of these 80 patients, 44 had thoracic major curves and 36 had thoracolumbar/lumbar major curves. After exclusion, 586 patients were included for analysis, with a mean ± SD brace-wear duration of 3.8 ± 1.5 years and post-weaning follow-up duration of 2.0 ± 1.1 years.
Fig. 1.
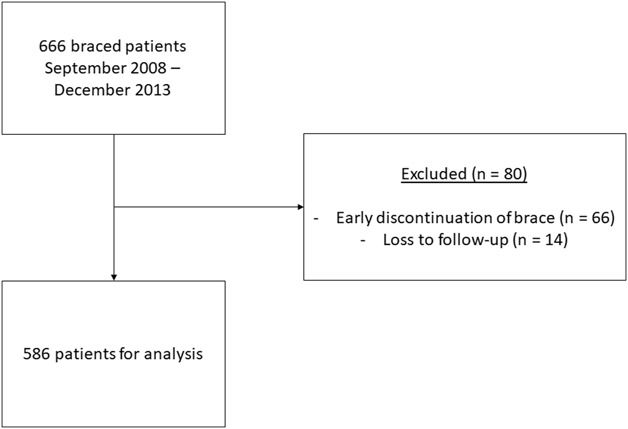
Flowchart of patients included the study.
Study Parameters
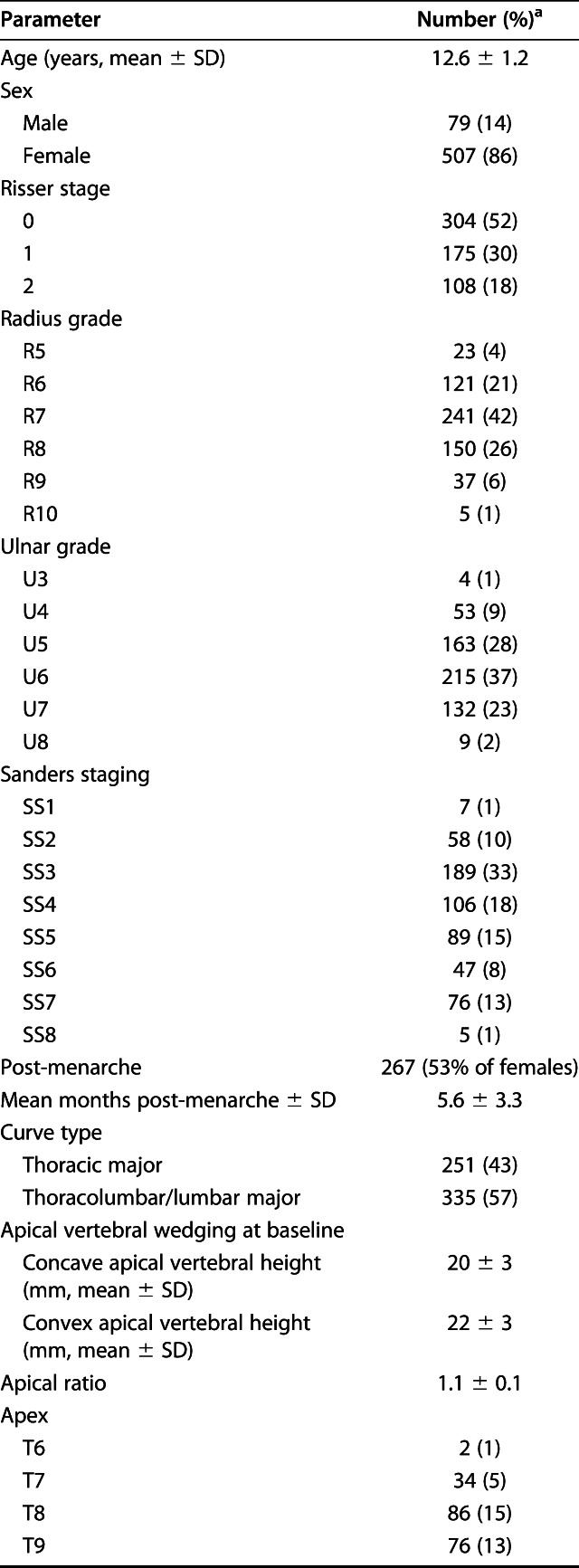
Baseline demographic data included chronological age, sex, and age at the time of menarche (Table 1). The mean age at baseline was 12.6 ± 1.2 years. Most patients were female (87%, 507 of 586) and up to 53% (267 of 507) of females were post-menarche. At baseline, before brace-wear, we obtained the following radiographs: a pre-brace standing whole-spine posteroanterior radiograph, supine whole-spine radiograph, and immediate in-brace standing whole-spine posteroanterior radiograph. On the pre-brace standing radiograph, the Risser stage, major curve Cobb angle, major curve apex, and the curve type were identified. Left-hand radiographs were also obtained at baseline to determine the skeletal age parameters of the distal radius and ulna classification and Sanders staging. The distal radius and ulna classifications were graded from radius grades 1 to 11 and ulnar grades 1 to 9 with increasing maturity status as the grades increased [6, 7]. Sanders staging is graded from 1 to 8 with increasing maturity status [39]. The curve type was classified as thoracic major curve (apex from T6 to 11) and thoracolumbar/lumbar major curve (apex from T12 to L3). The major curve Cobb angle was also measured on whole-spine radiographs to assess curve flexibility (pre-brace Cobb angle – supine Cobb angle / pre-brace Cobb angle x 100%). This angle was also measured on the first in-brace radiograph to calculate the correction rate (pre-brace Cobb angle – in-brace Cobb angle / pre-brace Cobb angle x 100%). In addition, to represent curve remodeling, the convex and concave apical vertebral body heights were measured, and the apical ratio (convex height/concave height) was calculated. An increased ratio suggested more wedging between the convex and concave sides of the apical vertebra. Also, we measured the vertebral body height and the major curve Cobb angle on the final radiographs to determine any changes that occurred during bracing. Two post-brace weaning radiographs were analyzed, one at 6 months post-brace weaning and a final radiograph (a standing posteroanterior view) obtained either at the time of skeletal maturity (age of 18 years or Risser Stage 4, no growth in body height for the past 6 months, and 2 years post-menarche) or immediately before surgery in patients with curve deterioration of 50° or more during brace treatment. All patients were recommended to follow a gradual weaning protocol over 6 months from the day of brace weaning. The mean pre-brace Cobb angle was 31 ± 4°, mean supine Cobb angle was 22 ± 6° and mean in-brace Cobb angle was 18 ± 6°. The mean flexibility was 30 ± 17% and mean correction rate was 41 ± 19%. All radiographs were taken without the brace on for at least 24 hours except for the in-brace radiograph. The refined 22-item Scoliosis Research Society questionnaire was used to determine patient-reported quality of life outcomes and is comprised of five domains (function, pain, appearance, mental health and satisfaction with treatment). Its minimum clinically important difference, based on a scale from 0 to 5, has been quoted as 0.2 for pain, 0.08 for activity and 0.98 for appearance domains [4]. Mental health has no quoted minimum clinically important difference for the adolescent idiopathic scoliosis population. Satisfaction with treatment is described and based on improvement or deterioration in domain scores. These scores were obtained immediately before seeing the clinician at the consultation room.
Table 1.
Baseline characteristics
Arrangement of Brace Fabrication and Fitting
Supine radiographs were obtained on the day of brace casting, within 1 month of the pre-brace radiograph. Patients underwent negative casting in the supine position with traction and counter-traction along the long axis of the curve. The amount of traction depended on the patient’s tolerance. A molded cast was used to manufacture the underarm brace. After the brace was fitted, the patient wore the brace for 2 weeks before an in-brace radiograph was obtained. Patients were advised to wear the brace for 20 hours per day and were followed up regularly at our scoliosis clinic every 4 months to 6 months. Simultaneously, patients were monitored by an orthotist for any need to change or revise the brace as well as a clinical psychologist for regular counseling. Patients also had a designated physiotherapist to provide postural training and maintenance exercises.
Imaging Method and Measurements
Radiographs were obtained with the patient standing upright in a relaxed position with the arms raised and slightly fisted hands resting on the clavicle. For the supine radiographs, patients lay comfortably on a radiolucent table. The film focus distance was 180 cm and the exposure factors were 77 kilovoltage peak and 20 miliamperage seconds. Two 35 cm x 35 cm cassettes were used to capture C7 to the hips. For in-brace radiographs, the images were taken at least 2 hours after the patient donned the brace to reflect the true correction achieved [24]. All parameters were collected on radiographs using the DICOM-based Radworks 5.1 computer software program (Applicare Medical Imaging BV, Zeist, the Netherlands). All radiographs were measured by two independent observers (JPYC, LCKC) who were blinded to the patients’ details. When the difference in the measurements between the two assessors was less than 5° and 1 mm, the mean of the two measurements was reported. When the discrepancy was more than 5° or 1 mm, a consensus between the assessors was determined.
Statistical Analysis
Data are presented as the mean ± SD. All analyses were performed with SPSS version 24.0 (IBM SPSS Inc, Chicago, IL, USA). Outcomes were based on changes in the Cobb angle. These included “improvement” or curve regression, as indicated by at least 5° reduction in the Cobb angle; “deterioration” or curve progression, as indicated by at least 5° increase in the Cobb angle; and “unchanged,” indicated by a change in the Cobb angle of less than 5°. Normality tests were performed using Shapiro-Wilk’s test with Q-Q probability plots. Intergroup comparisons of any differences between the study parameters and bracing outcomes were made with the Kruskal Wallis test. The studied parameters were the pre-brace and supine Cobb angles, flexibility and correction rates, apical vertebrae, apical ratio, and change in the major curve Cobb angle and apical ratio post-bracing. A univariate analysis for associations between these variables and bracing outcomes was performed using a point-biserial correlation coefficient for continuous variables (age, Risser stage, apical ratio, curve flexibility, and correction rate), and Pearson’s chi-square test was used to determine any association between the outcomes and categorical variables (sex, whether the patient had a brace post-menarche, Lenke curve type, and location of the apical vertebrae).
Multivariate logistic regression models were created for improved and deteriorated outcomes based on statistically significant factors in the univariate analyses. P values less than 0.05 were considered significant. Odds ratios are reported for statistically significant parameters. The 95% confidence intervals are listed, where applicable.
Results
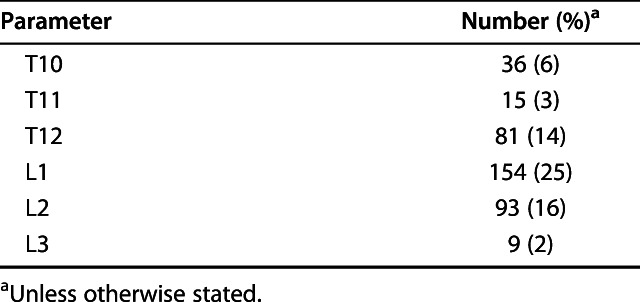
In all, 17% of patients (98 of 586) had curve regression (Fig. 2A-B) and 40% (234 of 586) had curve deterioration (Table 2). Among patients with improvement, the mean ± SD reduction in the Cobb angle was 9 ± 4° while in those with deterioration, the mean ± SD increase in the Cobb angle was 15 ± 9°, which fulfilled our criteria of a 5° change in Cobb angle. At the final follow-up, there were no further changes compared with brace-weaning. The mean change in Cobb angle was 0 ± 4° at mean 2 ± 1 year post-brace weaning follow-up for the curve regression group. The mean change in Cobb angle was 1 ± 3° at mean 2 ± 1 year post-brace weaning follow-up for the unchanged group. The mean change in Cobb angle was 1 ± 4° at mean 2 ± 1 year post-brace weaning follow-up for the curve progression group. There were no differences in the pre-brace Cobb angle between patients with an improved angle and those with a deteriorated angle. However, patients with improvement had a smaller supine Cobb angle (19 ± 5° versus 24 ± 6°; p < 0.001) and higher flexibility (80 ± 76% versus 38 ± 43%; p < 0.001) and correction rate (54 ± 21% versus 34 ± 18%; p < 0.001) than those in the deterioration group. There was an increased apical ratio in the deteriorated group (0.1 ± 0.1).
Fig. 2A-B.

These radiographs are of a patient with improved curve magnitude, with (A) a pre-brace standing radiograph showing a T10 to L3 curve of 30° and (B) a post-brace standing radiograph showing curve regression of 15°.
Table 2.
Outcomes of bracing
After controlling for potential confounders including age, Risser staging, radius and ulnar grading, Sanders staging, curve type, and curve apex, improvement in the Cobb angle after bracing was found to be associated with reduced apical ratio of 1:1 (OR 0.84 [95% CI 0.80 to 0.87]; p < 0.001), and increased correction rate (OR 1.03 [95% CI 1.02 to 1.05]; p < 0.001) (Table 3). However, this association with correction rate was not clinically significant. There was no association with flexibility.
Table 3.
Multivariate logistic regression model of post-bracing curve regression
Deterioration in the Cobb angle after bracing was associated with younger age, pre-menarche status at baseline, and increased apical ratio, correction rate, and flexibility (Table 4). For every year of increase in chronological age, there was a reduced likelihood of curve progression (OR 0.71 [95% CI 0.55 to 0.91]; p = 0.008). Patients who were pre-menarche had a higher likelihood of deterioration than those who were post-menarche (OR 2.46 [95% CI 1.31 to 4.62]; p = 0.005). The association of curve deterioration with less flexible curves (OR 0.99 [95% CI 0.99 to 1.00]; p = 0.030) and a reduced correction rate during bracing (OR 0.98 [95% CI 0.97 to 1.00]; p = 0.042) were not clinically significant. An increased apical ratio was also associated with curve progression (OR 1.24 [95% CI 1.19 to 1.30]; p < 0.001). The curve type and location were not associated with curve progression.
Table 4.
Multivariate logistic regression model for curve progression post-bracing
The refined 22-item Scoliosis Research Society questionnaire scores generally improved in all domains, regardless of the outcome of Cobb angle (Table 5). Importantly, the scores for function (mean difference on a scale from 0 to 5: 0.2; p = 0.001 versus 0.1; p < 0.001) and pain (mean difference on a scale from 0 to 5: 0.2; p = 0.020 versus 0.0; p = 0.853) fulfilled the minimum clinically important difference and were better in the post-brace improvement group than in the deterioration group. There were no clinically meaningful differences in appearance (mean difference on a scale from 0 to 5: 0.3; p = 0.001 versus 0.2; p < 0.001). Patients in the improved group appeared to have minimal increase in satisfaction with treatment (mean difference on a scale from 0 to 5: 0.2), while those in the deteriorated group had worse satisfaction scores (mean difference on a scale from 0 to 5: -0.4).
Table 5.
Changes in baseline pre-brace and post-brace Scoliosis Research Society-22r domain and total scores
Discussion
Bracing has well-accepted benefits: potentially stopping curve progression and avoiding surgery in patients with adolescent idiopathic scoliosis [47]. However, some patients may have curve regression with brace treatment [27, 32]. The prevalence of such phenomena and their associated factors are unknown. In this study, 17% (98 of 586) of individuals had an improved Cobb angle after bracing. Curve regression was associated with less vertebral wedging while curve progression was associated with younger age. Patients with curve regression had greater refined 22-item Scoliosis Research Society scores compared with patients with curve progression, especially in the domains of pain, appearance, and satisfaction with treatment.
There are several limitations to this study. This was a retrospective radiographic study; hence, it was not possible to consistently report the duration of brace-wear. Compliance data were based on patient self-reporting only, rather than an objective measure such as thermal sensors, which have not been available in our unit until recently. Patients with stiffer curves may also have poorer compliance. Hence, this may introduce bias into the study. The duration of brace-wear may influence the likelihood of remodeling observed in vertebral bodies. This suggests that we underestimated the true prevalence of curve regression because the information regarding the in-brace duration further supports the chance of curve regression. Conversely, there is also potential overestimation of curve regression due to the selection and transfer bias of excluding 80 patients from the analysis. Early discontinuation of brace treatment may have been related to curve deterioration and discomfort with the brace. Those lost to follow-up may also have had poor results with the brace and may have lost faith in our management. This group may have inherently stiffer curves which do not respond well to bracing. Hence, the actual prevalence of patients with curve progression may be higher than reported. Nevertheless, it is interesting to note that our noncompliance and drop-out rate (12%; 88 of 666) is far below what has been reported by Katz et al. [22], in which only 17% were compliant. There were also similar numbers of thoracic and thoracolumbar/lumbar curves; curve type related stiffness is unlikely a factor resulting in noncompliance. Our unit also provides regular clinical psychologist visits as required and this may have improved overall compliance. Karol et al. [21] showed that with counseling, there was only a 14% rate of inadequate brace-wear or refusal. There may also be cultural issues at play that should be explored in future multiethnic multicultural studies. Despite blinded assessment of the imaging by two independent investigators (JPYC, LCKC), introducing a consensus approach for large data variances is inherently biased. Another limitation is the lack of a 3-D assessment; we only assessed changes in the coronal plane. Whether changes occur in the sagittal and axial planes requires further study. The apical ratio was determined based on only one image, which may not represent vertebral wedging because deformities occur in three dimensions. In addition, the differences are small and may be subject to potential measurement errors due to the vertebral morphology. A ratio was used rather than absolute measurements to try and lessen the related bias. Our findings are also only relevant to underarm bracing, and the effect of different brace types should also be explored. The method for brace weaning should also be studied in future work. Although we adopted a gradual weaning protocol, there may be variations such as only nocturnal use for 6 months or a gradual step-wise reduction in brace-wear. This may not have a significant effect on the overall results with the large sample size but a dedicated study should be performed to verify this. Our brace weaning criteria—Risser stage 4, no growth in body height for the past 6 months, and 2 years post-menarche—may not be sufficient because curve progression after brace-weaning has been reported due to inadequacies of conventional maturity parameters [8].
We found that nearly 1 in 5 patients experienced curve regression with underarm bracing. However, most patients (43%) had an unchanged Cobb angle and more patients (40%) had curve deterioration. In all three outcome groups of curve regression, unchanged, and curve progression, the mean Cobb angle at baseline was similar. This suggests that factors other than the initial curve magnitude are responsible for the changes in post-bracing outcomes. One such factor is the location of the major curve. Patients with thoracolumbar/lumbar curves may have a better prognosis with a higher likelihood of an unchanged or improved Cobb angle, while those with thoracic curves are more likely to have a deteriorated angle. This was supported by Thompson et al. [43], who found that patients with thoracic curves had a higher risk of brace failure that ultimately led to surgery. This may be due to reduced effectiveness of the underarm brace to impart enough correction forces on the apex of the thoracic curve. Compared with other brace types, the underarm brace is unable to maintain an adequate longitudinal traction and mostly relies on transverse or bending forces for correction. Furthermore, additional padding posteriorly for pressure on the apical rib is less effective with the brace opening at the back. Similarly, flexibility is associated with bracing outcomes. In patients with curve progression, there is a clear trend of increasing stiffness during flexibility assessments with supine radiographs and less satisfactory in-brace correction than in those with curve regression. Curve flexibility and in-brace correction are inter-related. The flexibility of the curve has been shown to predict the immediate correction likely obtained with bracing [12, 36]. It is important to consider that our population, especially that of the curve regression group, are predominantly thoracolumbar/lumbar major curves, which are inherently more flexible and fare better than thoracic curves [43]. This is different from other reports [22, 43, 47]. With this large study population, we were also able to test for male sex with 79 boys included in the analysis unlike other studies on bracing outcomes with inadequate male sample sizes [22, 43, 47]. However, sex is unlikely an important factor as we found no association with post-brace outcomes in our univariate analyses. The data appears to show trends in increased flexibility and correction rate with curve regression.
After controlling for multiple confounders like skeletal age, the main factor associated with curve regression was a reduced apical ratio of 1:1. Ample evidence suggests that the risk of curve progression is near or slightly above the peak height velocity [5, 9-11]; thus, a more skeletally mature patient may be less likely to have marked spine growth and the potential for curve progression. However, Risser staging has inherent limitations for predicting growth spurts in adolescents [3, 15, 19, 25, 41]. All children have a Risser Stage of 0 before the growth acceleration curve, which provides limited information about whether the patient has had a growth spurt. The baseline characteristics clearly illustrated the problem with using Risser staging for brace indications. Although patients fulfilled the brace criteria of Risser 0 to 2, there are some that reached the later skeletal maturity stages like radius grade 10, ulna grade 8, and Sanders stage 8. This mismatch [8, 10] between Risser staging and other more accurate maturity parameters may be associated with some unnecessary braces. Nevertheless, according to our results, changes in the curve pattern caused by vertebral remodeling occur with bracing independent of skeletal age. Change in the apical ratio is a good visual representation of vertebral remodeling. With a reduced apical ratio, the concave height becomes more closely matched with the convex height, indicating less vertebral wedging (Fig. 3A-B). Similar to the concept of vertebral body stapling or tethering [2, 33], the brace may alter spinal growth with potential correction of a scoliosis deformity. Potential curve correction is supported by the initial rate of correction with the brace. Well-fitted braces that correct approximately 50% of the deformity and maintain a balanced spine have been shown to cause changes in the curve pattern, and this has been considered evidence of vertebral remodeling [49]. Better initial correction with the brace will more likely act according to Hueter-Volkman’s law [42], and we suspect that these patients may have improvement in their curvature because of altered vertebral growth and remodeling. It is important to note that we use the supine radiograph to predict what is achievable with bracing. The supine radiograph has been shown to be predictive of in-brace correction [12] and has the benefits of being a passive modality that produces the similar alignment as is expected with the patient standing. Nevertheless, our custom molding technique relies on the orthotist’s experience and is a factor not easily standardized or assessed objectively. Subtle technical determinants of a good brace-fit include patient tolerance to traction during molding and the degree of strap tightness.
Fig. 3.
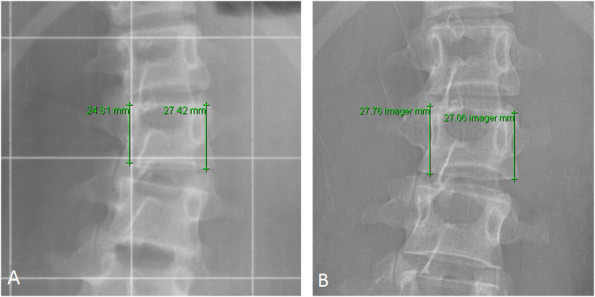
These radiographs are of a patient with improved curve magnitude with remodeling as shown by (A) a pre-brace L2 apical ratio of 1:1 (convex height of 27 mm and concave height of 25 mm) and (B) a post-brace L2 apical ratio of 1:0 (convex height of 27 mm and concave height of 28 mm).
The parameters associated with curve progression were younger age (pre-menarche and younger chronological age) and increased apical ratio. Younger patients, especially those who are pre-menarche, are expected to have larger growth potential and risk of curve progression [26]. No clinical differences were observed with reduced curve flexibility nor reduced correction rate. Poor brace outcomes are expected if the brace cannot correct the deformity, and difficulties with brace-fitting may be owing to an inherently stiff curve [43]. Our results do not support this. Even patients with less flexible curves may not behave poorly. Besides growth potential, another factor associated with curve progression is increased vertebral wedging as seen by an increased apical ratio (Fig. 4A-B). Our brace may be unable to alter vertebral growth adequately to prevent increased wedging. Vertebral wedging and increased rotational deformity have been suggested to be risk factors of curve progression [30]. These are early prognostic factors for poor bracing outcomes.
Fig. 4.
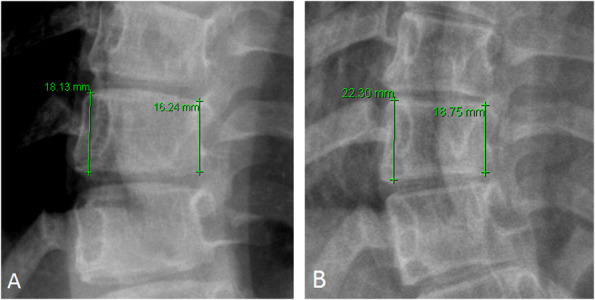
These radiographs are of a patient with curve progression and increased vertebral wedging as shown by (A) a pre-brace T10 apical ratio of 1:1 (convex height of 18 mm and concave height of 16 mm) and (B) a post-brace T10 apical ratio of 1:2 (convex height of 22 mm and concave height of 19 mm).
Beyond the radiological findings, curve regression has an additional benefit of better patient-reported quality-of-life outcome scores. Our reported scores for the overall population are similar to those reported in other studies [1, 20]. However, greater improvements in all domains, particularly function and pain, were observed with intergroup comparisons between patients in the improved group and those in the deteriorated group fulfilling the minimum clinically important differences as reported by Carreon et al. [4]. Although there was a difference in the appearance domain scores between the groups, this did not reach clinical significance. Interestingly, patients in the curve regression group reported having mildly improved satisfaction with treatment while patients with curve deterioration had a worse satisfaction of treatment after bracing. As our scores were obtained before the consultation, there are likely improved external features apparent to the patient before seeing the radiograph. Our findings further stress the importance of achieving these outcomes because there are obvious benefits in terms of patient-reported outcome measures.
Curve regression occurs in patients undergoing brace treatment, and the Cobb angle is maintained even after brace weaning. Vertebral remodeling may also occur with less vertebral wedging at weaning compared with brace initiation. Curve regression is likely a better outcome for patients undergoing brace treatment because the deformity is less severe. This is also reflected by better patient-perceived quality of life scores. Although we perceive no deterioration of the deformity and avoiding surgery as success with brace treatment, we should push the boundaries further because achieving curve regression is more impactful. This study has shown that 17% of patients may experience curve regression with satisfactory duration of brace-wear. The possible improvement in the Cobb angle should be disclosed to patients before and during bracing. Positive reinforcement may encourage patients and their families to be more compliant with bracing protocols. This perceived effect, along with the influence of using better skeletal maturity parameters than Risser staging for initiating bracing, and using more objective compliance data should be verified in future prospective studies. Physicians should also advocate that braces should be made with the curve reduced as much as possible; often the molded brace can achieve similar correction to that predicted with pre-bracing supine radiographs. A well-fitting brace provides the best chance of a positive outcome and the potential of vertebral remodeling to a more normal spine.
Acknowledgments
None.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. This study was supported by the General Research Fund of the Research Grants Council, grant #17156416.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedics & Traumatology, The University of Hong Kong.
References
- 1.Asher M, Min Lai S, Burton D, Manna B. Discrimination validity of the Scoliosis Research Society-22 patient questionnaire: relationship to idiopathic scoliosis curve pattern and curve size. Spine (Phila Pa 1976) . 2003;28:74-78. [DOI] [PubMed] [Google Scholar]
- 2.Betz RR, Ranade A, Samdani AF, Chafetz R, D'Andrea LP, Gaughan JP, Asghar J, Grewal H, Mulcahey MJ. Vertebral body stapling: a fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine (Phila Pa 1976). 2010;35:169-176. [DOI] [PubMed] [Google Scholar]
- 3.Biondi J, Weiner DS, Bethem D, Reed JF., 3rd Correlation of Risser sign and bone age determination in adolescent idiopathic scoliosis. J Pediatr Orthop . 1985;5:697-701. [DOI] [PubMed] [Google Scholar]
- 4.Carreon LY, Sanders JO, Diab M, Sucato DJ, Sturm PF, Glassman SD, Spinal Deformity Study G. The minimum clinically important difference in Scoliosis Research Society-22 Appearance, Activity, And Pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2010;35:2079-2083. [DOI] [PubMed] [Google Scholar]
- 5.Cheung JP, Cheung PW, Samartzis D, Cheung KM, Luk KD. The use of the distal radius and ulna classification for the prediction of growth: peak growth spurt and growth cessation. Bone Joint J. 2016;98-B:1689-1696. [DOI] [PubMed] [Google Scholar]
- 6.Cheung JP, Samartzis D, Cheung PW, Cheung KM, Luk KD. Reliability analysis of the distal radius and ulna classification for assessing skeletal maturity for patients with adolescent idiopathic scoliosis. Global Spine J . 2016;6:164-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung JP, Samartzis D, Cheung PW, Leung KH, Cheung KM, Luk KD. The distal radius and ulna classification in assessing skeletal maturity: a simplified scheme and reliability analysis. J Pediatr Orthop B . 2015;24:546-551. [DOI] [PubMed] [Google Scholar]
- 8.Cheung JPY, Cheung PWH, Luk KD. When should we wean bracing for adolescent idiopathic scoliosis? Clin Orthop Relat Res . 2019;477:2145-2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung JPY, Cheung PWH, Samartzis D, Luk KD. APSS-ASJ Best Clinical Research Award: Predictability of curve progression in adolescent idiopathic scoliosis using the distal radius and ulna classification. Asian Spine J . 2018;12:202-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung JPY, Cheung PWH, Samartzis D, Luk KD. Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res . 2018;476:429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung JPY, Luk KD. Managing the pediatric spine: growth assessment. Asian Spine J . 2017;11:804-816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung JPY, Yiu KKL, Vidyadhara S, Chan PPY, Cheung PWH, Mak KC. Predictability of supine radiographs for determining in-brace correction for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) . 2018;43:971-976. [DOI] [PubMed] [Google Scholar]
- 13.Cheung PWH, Wong CKH, Cheung JPY. An insight into the health-related quality of life of adolescent idiopathic scoliosis patients who are braced, observed, and previously braced. Spine (Phila Pa 1976) . 2019;44:E596-E605. [DOI] [PubMed] [Google Scholar]
- 14.Clin J, Aubin CE, Sangole A, Labelle H, Parent S. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) . 2010;35:1706-1713. [DOI] [PubMed] [Google Scholar]
- 15.Dhar S, Dangerfield PH, Dorgan JC, Klenerman L. Correlation between bone age and Risser's sign in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) . 1993;18:14-19. [DOI] [PubMed] [Google Scholar]
- 16.Gepstein R, Leitner Y, Zohar E, Angel I, Shabat S, Pekarsky I, Friesem T, Folman Y, Katz A, Fredman B. Effectiveness of the Charleston bending brace in the treatment of single-curve idiopathic scoliosis. J Pediatr Orthop . 2002;22:84-87. [PubMed] [Google Scholar]
- 17.Gutman G, Benoit M, Joncas J, Beausejour M, Barchi S, Labelle H, Parent S, Mac-Thiong JM. The effectiveness of the SpineCor brace for the conservative treatment of adolescent idiopathic scoliosis. Comparison with the Boston brace. Spine J . 2016;16:626-631. [DOI] [PubMed] [Google Scholar]
- 18.He C, To MK, Cheung JP, Cheung KM, Chan CK, Jiang WW, Zhou GQ, Lai KK, Zheng YP, Wong MS. An effective assessment method of spinal flexibility to predict the initial in-orthosis correction on the patients with adolescent idiopathic scoliosis (AIS). PLoS One . 2017;12:e0190141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoppenfeld S, Lonner B, Murthy V, Gu Y. The rib epiphysis and other growth centers as indicators of the end of spinal growth. Spine (Phila Pa 1976) . 2004;29:47-50. [DOI] [PubMed] [Google Scholar]
- 20.Iwahara T, Imai M, Atsuta Y. Quantification of cosmesis for patients affected by adolescent idiopathic scoliosis. Eur Spine J . 1998;7:12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karol LA, Virostek D, Felton K, Wheeler L. Effect of compliance counseling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am . 2016;98:9-14. [DOI] [PubMed] [Google Scholar]
- 22.Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am . 2010;92:1343-1352. [DOI] [PubMed] [Google Scholar]
- 23.Lee CS, Hwang CJ, Kim DJ, Kim JH, Kim YT, Lee MY, Yoon SJ, Lee DH. Effectiveness of the Charleston night-time bending brace in the treatment of adolescent idiopathic scoliosis. J Pediatr Orthop . 2012;32:368-372. [DOI] [PubMed] [Google Scholar]
- 24.Li M, Wong MS, Luk KD, Wong KW, Cheung KM. Time-dependent response of scoliotic curvature to orthotic intervention: when should a radiograph be obtained after putting on or taking off a spinal orthosis? Spine (Phila Pa 1976) . 2014;39:1408-1416. [DOI] [PubMed] [Google Scholar]
- 25.Little DG, Sussman MD. The Risser sign: a critical analysis. J Pediatr Orthop . 1994;14:569-575. [DOI] [PubMed] [Google Scholar]
- 26.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am . 1984;66:1061-1071. [PubMed] [Google Scholar]
- 27.Lusini M, Donzelli S, Minnella S, Zaina F, Negrini S. Brace treatment is effective in idiopathic scoliosis over 45 degrees : an observational prospective cohort controlled study. Spine J . 2014;14:1951-1656. [DOI] [PubMed] [Google Scholar]
- 28.Maruyama T. Bracing adolescent idiopathic scoliosis: a systematic review of the literature of effective conservative treatment looking for end results 5 years after weaning. Disabil Rehabil . 2008;30:786-791. [DOI] [PubMed] [Google Scholar]
- 29.Minsk MK, Venuti KD, Daumit GL, Sponseller PD. Effectiveness of the Rigo Cheneau versus Boston-style orthoses for adolescent idiopathic scoliosis: a retrospective study. Scoliosis Spinal Disord . 2017;12:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nault ML, Mac-Thiong JM, Roy-Beaudry M, Turgeon I, Deguise J, Labelle H, Parent S. Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine (Phila Pa 1976) . 2014;39:E601-E606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A, Marti C, Maruyama T, O'Brien J, Price N, Parent E, Rigo M, Romano M, Stikeleather L, Wynne J, Zaina F. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord . 2018;13:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Negrini S, Negrini F, Fusco C, Zaina F. Idiopathic scoliosis patients with curves more than 45 Cobb degrees refusing surgery can be effectively treated through bracing with curve improvements. Spine J . 2011;11:369-380. [DOI] [PubMed] [Google Scholar]
- 33.Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP. Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Joint Surg Am . 2018;100:1691-1697. [DOI] [PubMed] [Google Scholar]
- 34.Noonan KJ, Dolan LA, Jacobson WC, Weinstein SL. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J Pediatr Orthop . 1997;17:712-717. [PubMed] [Google Scholar]
- 35.Odermatt D, Mathieu PA, Beausejour M, Labelle H, Aubin CE. Electromyography of scoliotic patients treated with a brace. J Orthop Res . 2003;21:931-936. [DOI] [PubMed] [Google Scholar]
- 36.Ohrt-Nissen S, Hallager DW, Gehrchen M, Dahl B. Supine lateral bending radiographs predict the initial in-brace correction of the providence brace in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2016;41:798-802. [DOI] [PubMed] [Google Scholar]
- 37.Ohrt-Nissen S, Kamath VHD, Samartzis D, Luk KDK, Cheung JPY. Fulcrum flexibility of the main curve predicts postoperative shoulder imbalance in selective thoracic fusion of adolescent idiopathic scoliosis. Eur Spine J . 2018;27:2251-2261. [DOI] [PubMed] [Google Scholar]
- 38.Richards BS, Bernstein RM, D'Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976). 2005;30:2068-2075; discussion 76-77. [DOI] [PubMed] [Google Scholar]
- 39.Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am . 2008;90:540-553. [DOI] [PubMed] [Google Scholar]
- 40.Shigematsu H, Cheung JP, Bruzzone M, Matsumori H, Mak KC, Samartzis D, Luk KD. Preventing fusion mass shift avoids postoperative distal curve adding-on in adolescent idiopathic scoliosis. Clin Orthop Relat Res . 2017;475:1448-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shuren N, Kasser JR, Emans JB, Rand F. Reevaluation of the use of the Risser sign in idiopathic scoliosis. Spine (Phila Pa 1976) . 1992;17:359-361. [DOI] [PubMed] [Google Scholar]
- 42.Stokes IA, Spence H, Aronsson DD, Kilmer N. Mechanical modulation of vertebral body growth. Implications for scoliosis progression. Spine (Phila Pa 1976) . 1996;21:1162-1167. [DOI] [PubMed] [Google Scholar]
- 43.Thompson RM, Hubbard EW, Jo CH, Virostek D, Karol LA. Brace success is related to curve type in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am . 2017;99:923-928. [DOI] [PubMed] [Google Scholar]
- 44.Ugwonali OF, Lomas G, Choe JC, Hyman JE, Lee FY, Vitale MG, Roye DP., Jr Effect of bracing on the quality of life of adolescents with idiopathic scoliosis. Spine J . 2004;4:254-260. [DOI] [PubMed] [Google Scholar]
- 45.Upadhyay SS, Nelson IW, Ho EK, Hsu LC, Leong JC. New prognostic factors to predict the final outcome of brace treatment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) . 1995;20:537-545. [DOI] [PubMed] [Google Scholar]
- 46.Vasiliadis E, Grivas TB, Savvidou O, Triantafyllopoulos G. The influence of brace on quality of life of adolescents with idiopathic scoliosis. Stud Health Technol Inform . 2006;123:352-356. [PubMed] [Google Scholar]
- 47.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med . 2013;369:1512-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yao G, Cheung JPY, Shigematsu H, Ohrt-Nissen S, Cheung KMC, Luk KDK, Samartzis D. Characterization and predictive value of segmental curve flexibility in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976). 2017;42:1622-1628. [DOI] [PubMed] [Google Scholar]
- 49.Zheng X, Sun X, Qian B, Wu T, Mao S, Zhu Z, Wang B, Qiu Y. Evolution of the curve patterns during brace treatment for adolescent idiopathic scoliosis. Eur Spine J . 2012;21:1157-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]