Abstract
Background
With recent Medicare payment changes, older adults are increasingly likely to be discharged home instead of to extended care facilities after total joint arthroplasty (TJA), and may therefore be at increased risk for readmissions. Identifying risk factors for readmission could help re-align care pathways for vulnerable patients; recent research has suggested preoperative dependency in activities of daily living (ADL) may increase perioperative and postoperative surgical complications. However, the proportion of older surgical patients with ADL dependence before TJA, and the impact of ADL dependency on the frequency and timing of hospital readmissions is unknown.
Questions/purposes
(1) What proportion of older adults discharged home after TJA have preoperative ADL dependency? (2) Is preoperative ADL dependency associated with increased risk of hospital readmissions at 30 days or 90 days for older adults discharged home after TJA?
Methods
This was a retrospective cohort analysis of 6270 Medicare fee-for-service claims from 2012 from a 5% national Medicare sample for older adults (older than 65 years) receiving home health care after being discharged to the community after elective TJA. Medicare home health claims were used for two reasons: (1) the primary population of interest was older adults and (2) the accompanying patient-level assessment data included an assessment of prior dependency on four ADL tasks. Activities of daily living dependency was dichotomized as severe (requiring human assistance with all four assessed tasks) or partial/none (needing assistance with three or fewer ADLs); this cutoff has been used in prior research to evaluate readmission risk. Multivariable logistic regression models, clustered at the hospital level and adjusted for known readmission risk factors (such as comorbidity status or age), were used to model the odds of 30- and 90- day and readmission for patients with severe ADL dependence.
Results
Overall, 411 patients were hospitalized during the study period. Of all readmissions, 64% (262 of 411) occurred within the first 30 days, with a median (interquartile range [IQR]) time to readmission of 17 days (5 to 46). Severe ADL dependency before surgery was common for older home health recipients recovering from TJA, affecting 17% (1066 of 6270) of our sample population. After adjusting for clinical covariates, severe ADL dependency was not associated with readmissions at 90 days (adjusted odds ratio = 1.20 [95% CI 0.93 to 1.55]; p = 0.15). However, severe preoperative ADL dependency was associated with higher odds of readmission at 30 days (adjusted OR = 1.45 [95% CI 1.11 to 1.99]; p = 0.008).
Conclusions
Severe preoperative ADL dependency is modestly associated with early but not late hospital readmission after TJA. This work demonstrates that it may important to apply a simple screening of ADL dependency preoperatively so that surgeons can guide changes in care planning for older adults undergoing TJA, which may include participation in preoperative rehabilitation (pre-habilitation) or more aggressive follow-up in the 30 days after surgery. Further research is needed to determine whether severe ADL dependence can be modified before surgery, and whether these changes in dependency can reduce readmission risk after TJA.
Level of Evidence
Level III, therapeutic study.
Introduction
Total joint arthroplasty (TJA) is one of the most common surgical procedures in the United States [12]. To address rising costs related to these procedures, Medicare has introduced care bundling to incentivize hospital systems and post-acute care providers to better coordinate and streamline care for patients who undergo TJA [3]. Almost immediately after the initiation of care bundling, hospital systems responded by discharging more patients to home with home health therapy and reducing the use of more costly skilled nursing facilities or rehabilitation hospitals [5, 10]. However, sending these borderline patients home after TJA may increase hospital readmission risk [19]. Therefore, identifying modifiable risk factors for readmission before surgery may be beneficial in tailoring preoperative and postoperative care for older adults (older than 65 years) with higher vulnerability who are planning to discharge home after TJA.
One candidate variable that has been used to identify elevated risk for readmissions is pre-hospitalization dependency (requirement for human assistance) in activities of daily living (ADLs) such as bathing, ambulation, and transfers. Multiple studies have found links between impairments in preoperative physical and mental function and poor outcomes after TJA [1, 11]; however, these studies have not exclusively studied older adults (older than 65 years old), have only evaluated the early 30-day readmission time period, and have not focused exclusively on the growing population of older adults who discharge directly home after surgery versus to an extended care facility. Understanding the prevalence of preoperative ADL dependency among older surgical candidates and determining the association between levels of preoperative ADL dependency and 30- and 90-day readmissions would be a highly valuable tool for surgeons to plan pre- and postoperative care pathways for vulnerable older patients who are planning to discharge home after TJA.
Therefore, we asked: (1) What proportion of older adults discharged home after TJA have preoperative ADL dependency? (2) Is preoperative ADL dependency associated with increased risk of hospital readmissions at 30 days or 90 days for older adults discharged home after TJA?
Patients and Methods
This was a retrospective analysis of the 5% national sample of 2012 Medicare administrative and claims data for patients undergoing TJA and discharged home with home health care (instead of to a nursing home or rehabilitation hospital). The year 2012 was the latest available data when this analysis began and represents the last full year of data before the initiation of the Medicare Comprehensive Care for Total Joint Replacement model. Patients receiving home health care after TJA are homebound but generally only receive two to three visits per week from clinical staff [7]—therefore, patients who go home after TJA have substantially less medical supervision compared with those who discharge to extended care rehabilitation facilities.
Briefly, the Medicare research identifiable files used in this study are available under a data use agreement with the Centers for Medicare & Medicaid Services (CMS). The files that were provided by CMS for this study were all paid provider claims for care received by all Medicare fee-for-service beneficiaries in home health care, linked with a patient-level assessment file called the Medicare Outcome and Assessment Information Set [OASIS]. These assessment files include granular detail on pre- and postsurgical ADL status, making them a unique and valuable information source. Medicare information has a high degree of accuracy, and the datasets are well-maintained, making these files a valuable source of information for healthcare utilization and outcomes for older adults [9]. Medicare makes these files available for researchers as 5% or 100% samples—the data use agreement used to acquire data for this study stipulated use of the 5% data for answering the research questions. Medicare data has an advantage over other orthopaedic cohort datasets for this project (such as the National Surgical Quality Improvement Project) for older adults because it allows researchers to follow patients longer than 30 days.
The 5% sample of Medicare home health users was linked to the Medicare Provider and Analysis Review (MEDPAR) file to identify Medicare fee-for-service beneficiaries who were discharged from a short-stay hospital in 2012 after their first elective TKA (ICD-9 procedure code 81.54) or THA (ICD-9 procedure code 81.51) in 2012 (Fig. 1). We excluded those who underwent arthroplasty after having a hip fracture. We limited the sample to patients who started home health care within 7 days after hospitalization to accurately characterize posthospitalization disability levels. Lastly, the Medicare Master Beneficiary Summary File was linked to the surgical cohort by a common Medicare identification number to determine Medicare and Medicaid enrollment, patient race, and death dates for patients in the study sample. To be consistent with Medicare readmission metrics, we excluded beneficiaries who left the hospital against medical advice or those who died within 90 days after surgery.
Fig. 1.
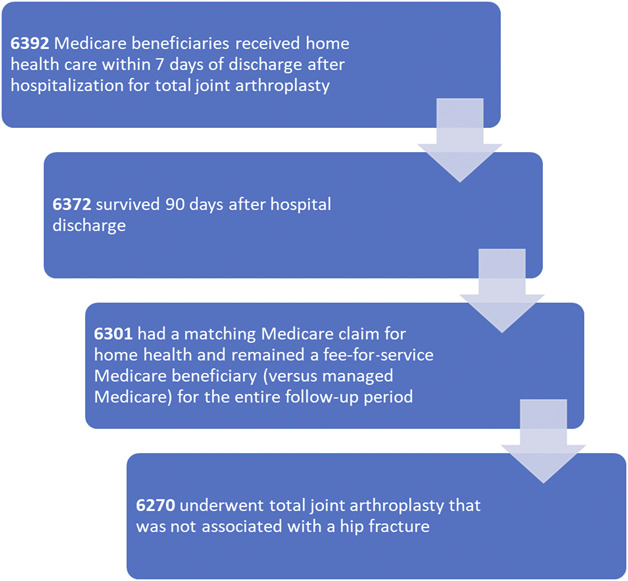
The development of the analytic sample is depicted in the figure.
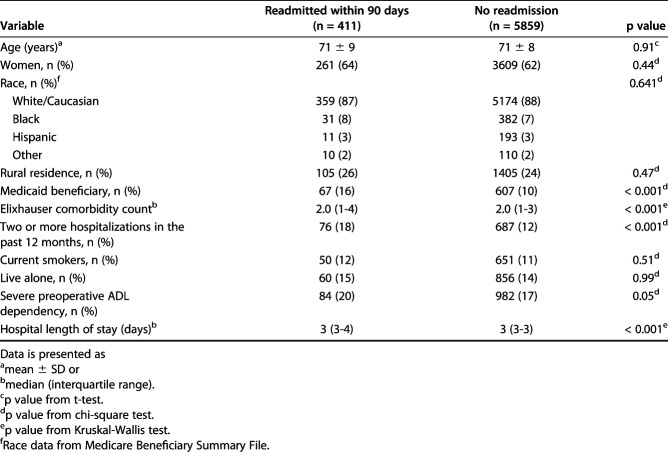
Overall, 6270 patients were included in the analysis; 68% (4285) underwent TKA and 32% (1985) underwent THA. Most were older than 70 years, female, and identified as Caucasian (Table 1). Patient started home health care a median (IQR) of 4 days (4 to 5) after surgery, which did not differ across readmission status.
Table 1.
Demographics of the patients in the study sample
Outcomes
The primary study outcome was the proportion of older adults discharged home who had ADL dependence before surgery. The secondary outcomes were to evaluate the relationship between ADL dependency and hospital readmissions at 30 and 90 days postoperatively.
A hospital readmission was defined a priori as readmission to a short-stay hospital (versus transfer to an extended care facility after home discharge). The 30- and 90-day periods align with Medicare periods of interest for readmission rates after elective TJA. We also categorized the top three diagnosis-related groups (DRGs) coded for readmissions from the MEDPAR file.
Primary Explanatory Variable
We assessed presurgical ADL disability using patient self-report data recorded on the Outcome and Assessment Information Set. The measure assessed three basic ADL categories: (1) general self-care (for example, dressing, bathing, and grooming), (2) ambulation, and (3) transfers, and a single instrumental activity of daily living question: (4) the ability to perform household tasks (for example, laundry and meal preparation). Requiring human assistance with four or more basic and instrumental ADLs assessed is generally considered to be representative of severe disability [8]; severe disability has previously been used to evaluate patients at risk for hospital readmissions [13]. Therefore, we dichotomized disability as severe (dependency with all four ADLs) or partial/none (requiring human assistance with three or fewer ADLs).
Clinical Characteristics
Data on patient birthdate, gender, and clinician-assessed hospitalization history were extracted from the Outcome and Assessment Information Set. Data on race and dual eligibility for Medicaid were extracted from the Master Beneficiary Summary File. We used the 31-item Elixhauser Comorbidity Index to characterize multimorbidity in the sample population. Elixhauser comorbidities were extracted from the ICD-9 diagnosis codes in the Medicare Provider and Analysis Review file and coded using a validated algorithm [6, 16]. Hospital length of stay was also extracted from the MEDPAR file.
Statistical Methods
We calculated descriptive statistics to compare patients who were readmitted with those who were not. Continuous variables were compared using two sample t-tests, categorical variable were compared using a chi-square test, and count variables with non-normal distributions were compared using the Kruskal-Wallis test. Then, we used logistic regression using generalized estimating equations to evaluate the association between preoperative ADL dependency and risk for readmission while accounting for potential non-independence of patients treated at the same hospital with similarities between surgical volume and staff, care pathways, and patient characteristics. A compound symmetry correlation structure was used for the model. The model adjusted for the following factors that may influence early hospital readmission rates: age, sex, race, hospitalization history, hospital length of stay, smoking status, social support, Elixhauser Comorbidity Index score, and Medicaid dual eligibility. A two-tailed p-value of 0.05 was used to determine statistical significance. Because claims data and mandatory Medicare home health evaluations were used as primary data sources, there were no missing data for the analyzed variables. All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA). This project received ethical approval from the University of Colorado Multiple Institutional Review Board.
Results
Proportion of Patients Receiving Home Health Care After TJA with Severe Preoperative ADL Dependency
We found that 17% (1066 of 6270) of the patients in this sample were dependent in all four ADLs surveyed and categorized as having severe ADL dependency before surgery. The proportions did not differ meaningfully between patients who underwent THA (16%, 326 of 1985) and those who underwent TKA (17%, 740 of 4285). Of the sample, 58% (3667 of 6270) had no preoperative ADL dependencies, 15% (932 of 6270) had one dependency, 5% (333 of 6270) had two dependencies, and 4% (272 of 6270) had three ADL dependencies before surgery.
Relationship Between ADL Dependency and Odds of Hospital Readmissions After TJA
After controlling for the aforementioned readmission risk factors (such as comorbidity), we found that those patients with severe ADL dependency were no more likely to be readmitted to the hospital within 90 days than those with three or fewer ADL dependencies (adjusted OR = 1.20 [95% CI 0.93 to 1.55]; p = 0.15). However, 30 days after TJA, patients with severe ADL dependency had higher odds of hospital readmission (adjusted OR = 1.45 [95% CI 1.11 to 1.99]; p = 0.008). The median (IQR) time to readmission was 17 days (5 to 46) after hospital discharge, suggesting half of readmissions occurred within the first 2 to 3 weeks post-discharge. Across all 411 readmissions, there were 159 unique DRG codes indicating reasons for readmission; the top three categories were for revision surgery (DRG 467 or 468; 27 of 411 readmissions), cellulitis or surgical site infections (DRG codes 863 and 603; 26 of 411), and for cardiac arrhythmias (DRG 310; 13 of 411). Because of small sample sizes, we were unable to make further subgroup comparisons.
Discussion
The results of this study suggest that nearly 1 in 5 older TJA recipients who discharge directly home from the hospital had severe preoperative ADL dependency, requiring human assistance with self-care, ambulation, transfers, and household tasks before surgery. Dependency in all four ADL tasks before surgery was modestly associated with 30-day but not 90-day hospital readmissions. These findings provide surgeons with an effective screening tool to identify high-risk patient before surgery and to determine for whom preoperative interventions (such as pre-habilitation) may be necessary. These findings also could help surgeons plan postoperative care with greater precision, potentially by increasing the availability of resources and medical follow-up during the initial 30-day postoperative period for patients sent home after acute hospitalization.
This study is not without limitations. First, we only evaluated patients who were discharged directly home from acute hospitalization and excluded those who discharged first to skilled nursing facilities or rehabilitation hospitals. Therefore, our findings should be generalized to only patients who discharge home after surgery. But because an increasing number of patients are being discharged home instead of to nursing facilities as a response to Medicare payment changes, these findings are highly relevant. Second, because retrospective claims data were used in the analysis, we cannot make definite statements about causal relationships between functional status and readmissions; we can only state that a statistical association exists. However, the relative strength of the association after accounting for medical complexity and other known readmission risk factors are indicators that this association is robust. It is also possible that other factors that are not well-assessed in claims data (such as social determinants of health) were not available in our data and may have influenced readmission rates. However, our study did control indirectly for poverty (Medicaid status) so these factors were considered as much as possible in the available data. Additionally, because we only evaluated Medicare fee-for-service beneficiaries, the results may not be generalizable to other payers (such as managed Medicare).
In this national sample of patients covered by Medicare and discharged home after TJA, we found that 17% demonstrated severe ADL dependence (requiring human assistance with four key ADLs) before surgery. This is substantially higher than prior estimates for TJA recipients from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, which range from 2% to 4% [4, 15]. However, the NSQIP database assesses preoperative ADL function with a single clinician assessment of whether a patient is independent, partially dependent, or severely dependent with overall functional health status, and includes a wide range of younger surgical patients who may have higher levels of functional independence before surgery. Our study, focusing on adults older than 65 years, assesses four different tasks, whether a patient requires human assistance to complete these tasks, and sums the total number of dependencies. This approach may provide a more comprehensive look at overall physical function and may be easily reproducible and reliable across surgeons assessing older adults before TJA. Quantifying the total number of preoperative ADL dependencies also provides additional valuable information for physicians monitoring postoperative functional recovery—failure to regain these levels early after hospitalization may signal higher risk of postoperative complications or poor patient outcomes [2].
Severe preoperative ADL dependency was not associated with increased odds of readmission within 90 days of TJA, although it was associated with an increased risk of readmission within 30 days of surgery. Older adults with severe ADL dependency before surgery had a relative 45% increase in the probability of 30-day readmission as compared with those with partial or no ADL dependency preoperatively. This study builds on prior research that concluded preoperative ADL dependency or poor physical function is a risk factor for adverse events both perioperatively and in the 30 day postoperative window for patients undergoing TJA [1, 4, 11]. The results from our study and others indicating the relationship between preoperative ADL dependency and early timing of readmissions also have implications for how both preoperative and postoperative care can be redesigned more effectively. Preoperatively, patients identified as having severe ADL dependency could be candidates for pre-habilitation. Prior research has suggested that preoperative rehabilitation improved TJA outcomes [17, 18]. Identifying severe ADL dependency preoperatively also allows surgeons to proactively anticipate and plan elevated postoperative care needs in the early postsurgical period. Because there is substantial flexibility in how Medicare allows postoperative home care to be structured, surgeons could encourage home health agencies to frontload nursing and rehabilitation visits for older adults with severe preoperative ADL dependency by increasing the frequency of combined visits in the early postoperative period and taper these services later in the postoperative course. This is a commonly used readmission reduction intervention for older adults recovering from medical hospitalizations [14] and would be easy to implement after TJA without added resource use or costs. Because at least one of the top reasons for readmission observed in our study may be potentially preventable (infection), increasing supportive services like home nursing care early after surgery may be effective.
In conclusion, our findings suggest that a simple preoperative assessment of four simple ADL tasks may indicate a higher odds of 30-day hospital readmission after surgery. These findings provide orthopaedic surgeons a tool to identify patients at high risk for postoperative readmissions and perhaps refer these patients for preoperative rehabilitation. Surgeons could also use these findings to plan for more intensive postoperative medical follow-up in the first 30 days a patient is home. Future research should evaluate whether more aggressive management of preoperative disability before surgery reduces hospital readmissions; findings from such research could help shape how patients with high preoperative disability levels are cared for before and after surgery.
Acknowledgments
None
Footnotes
The institution of one or more of the authors (JRF, JSL) has received, during the study period, funding from the National Institute on Aging, training grant numbers T32AG000279, F31AG056069, and T32AG019134; the Foundation for Physical Therapy; the Center on Health Services Training and Research (CHSTAR); and the American Physical Therapy Association Home Health Section. Support for VA/CMS data was provided by the Department of Veterans Affairs, VA Health Services Research and Development Services, VA Information Resource Center (Project Numbers SDR-02-237 and 98-004).
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Colorado, Anschutz Medical Campus, Aurora, CO, USA.
References
- 1.Ayers DC, Fehring TK, Odum SM, Franklin PD. Using joint registry data from FORCE-TJR to improve the accuracy of risk-adjustment prediction models for thirty-day readmission after total hip replacement and total knee replacement. J Bone Joint Surg Am. 2015;97:668-671. [DOI] [PubMed] [Google Scholar]
- 2.Boyd CM, Landefeld CS, Counsell SR, Palmer RM, Fortinsky RH, Kresevic D, Burant C, Covinsky KE. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr So. 2008;56:2171-2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472:188-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curtis GL, Hammad A, Anis HK, Higuera CA, Little BE, Darwiche HF. Dependent functional status is a risk factor for perioperative and postoperative complications after total hip arthroplasty. J Arthroplasty. 2019;34:S348-S351. [DOI] [PubMed] [Google Scholar]
- 5.Dummit LA, Kahvecioglu D, Marrufo G, Rajkumar R, Marshall J, Tan E, Press MJ, Flood S, Muldoon LD, Gu Q. Association between hospital participation in a Medicare bundled payment initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016;316:1267-1278. [DOI] [PubMed] [Google Scholar]
- 6.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36:8-27. [DOI] [PubMed] [Google Scholar]
- 7.Falvey JR, Bade MJ, Forster JE, Burke RE, Jennings JM, Nuccio E, Stevens-Lapsley JE. Home-health-care physical therapy improves early functional recovery of Medicare beneficiaries after total knee arthroplasty. J Bone Joint Surg Am. 2018;100:1728-1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005;161:575-584. [DOI] [PubMed] [Google Scholar]
- 9.Hennessy S, Leonard CE, Palumbo CM, Newcomb C, Bilker WB. Quality of Medicaid and Medicare data obtained through Centers for Medicare and Medicaid Services (CMS). Med Care. 2007;45:1216-1220. [DOI] [PubMed] [Google Scholar]
- 10.Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD. Early results of Medicare's bundled payment initiative for a 90-day total joint arthroplasty episode of care. J Arthroplasty. 2016;31:343-350. [DOI] [PubMed] [Google Scholar]
- 11.Kapoor A, Chew PW, Reisman JI, Berlowitz DR. Low self-reported function predicts adverse postoperative course in Veterans Affairs beneficiaries undergoing total hip and total knee replacement. J Am Geriatr Soc. 2016;64:862-869. [DOI] [PubMed] [Google Scholar]
- 12.Kremers HM, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meddings J, Reichert H, Smith SN, Iwashyna TJ, Langa KM, Hofer TP, McMahon LF. The impact of disability and social determinants of health on condition-specific readmissions beyond Medicare risk adjustments: a cohort study. J Gen Intern Med. 2017;32:71-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Connor M, Bowles KH, Feldman PH, St Pierre M, Jarrin O, Shah S, Murtaugh CM. Frontloading and intensity of skilled home health visits: a state of the science. Home Health Care Serv Q. 2014;33:159-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phruetthiphat O-a, Gao Y, Vasta S, Zampogna B, Piperno A, Noiseux NO. Preoperative risk factors for, and incidence of delayed surgery in elective primary total knee arthroplasty after hospital admission: the ACS-NSQIP. J Arthroplasty. 2016;31:1413-1416. [DOI] [PubMed] [Google Scholar]
- 16.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130-1139. [DOI] [PubMed] [Google Scholar]
- 17.Snow R, Granata J, Ruhil AVS, Vogel K, McShane M, Wasielewski R. Associations between preoperative physical therapy and post-acute care utilization patterns and cost in total joint replacement. J Bone Joint Surg Am. 2014;96:e165. [DOI] [PubMed] [Google Scholar]
- 18.Soeters R, White PB, Murray-Weir M, Koltsov JCB, Alexiades MM, Ranawat AS, Hip Knee, Surgeons Writing Committee , . Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clin Orthop Relat Res. 2018;476:40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Werner RM, Coe NB, Qi M, Konetzka RT. Patient outcomes after hospital discharge to home with home health care vs to a skilled nursing facility. JAMA Intern Med. 2019;179:617-623. [DOI] [PMC free article] [PubMed] [Google Scholar]