Abstract
Background
Robotic-assisted TKA was introduced to enhance the precision of bone preparation and component alignment with the goal of improving the clinical results and survivorship of TKA. Although numerous reports suggest that bone preparation and knee component alignment may be improved using robotic assistance, no long-term randomized trials of robotic-assisted TKA have shown whether this results in improved clinical function or survivorship of the TKA.
Questions/purposes
In this randomized trial, we compared robotic-assisted TKA to manual-alignment techniques at long-term follow-up in terms of (1) functional results based on Knee Society, WOMAC, and UCLA Activity scores; (2) numerous radiographic parameters, including component and limb alignment; (3) Kaplan-Meier survivorship; and (4) complications specific to robotic-assistance, including pin-tract infection, peroneal nerve palsy, pin-site fracture, or patellar complications.
Methods
This study was a registered prospective, randomized, controlled trial. From January 2002 to February 2008, one surgeon performed 975 robotic-assisted TKAs in 850 patients and 990 conventional TKAs in 849 patients. Among these patients 1406 patients were eligible for participation in this study based on prespecified inclusion criteria. Of those, 100% (1406) patients agreed to participate and were randomized, with 700 patients (750 knees) receiving robotic-assisted TKA and 706 patients (766 knees) receiving conventional TKA. Of those, 96% (674 patients) in the robotic-assisted TKA group and 95% (674 patients) in the conventional TKA group were available for follow-up at a mean of 13 (± 5) years. In both groups, no patient older than 65 years was randomized because we anticipated long-term follow-up. We evaluated 674 patients (724 knees) in each group for clinical and radiographic outcomes, and we examined Kaplan-Meier survivorship for the endpoint of aseptic loosening or revision. Clinical evaluation was performed using the original Knee Society knee score, the WOMAC score, and the UCLA activity score preoperatively and at latest follow-up visit. We also assessed loosening (defined as change in the position of the components) using plain radiographs, osteolysis using CT scans at the latest follow-up visit, and component, and limb alignment on mechanical axis radiographs.
To minimize the chance of type-2 error and increase the power of our study, we assumed the difference in the Knee Society score to be 5 points to match the MCID of the Knee Society with power of 0.99, which revealed that a total of 628 patients would be needed in each group.
Results
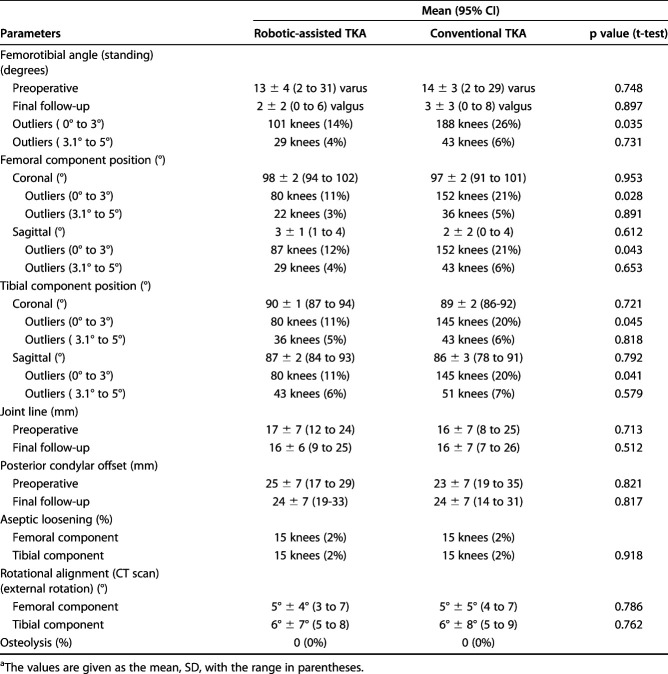
Clinical parameters at the latest follow-up including the Knee Society knee scores (93 ± 5 points in the robotic-assisted TKA group versus 92 ± 6 points in the conventional TKA group [95% confidence interval 90 to 98]; p = 0.321) and Knee Society knee function scores (83 ± 7 points in the robotic-assisted TKA group versus 85 ± 6 points in the conventional TKA group [95% CI 75 to 88]; p = 0.992), WOMAC scores (18 ± 14 points in the robotic-assisted TKA group versus 19 ± 15 points in the conventional TKA group [95% CI 16 to 22]; p = 0.981), range of knee motion (125 ± 6° in the robotic-assisted TKA group versus 128 ± 7° in the conventional TKA group [95% CI 121 to 135]; p = 0.321), and UCLA patient activity scores (7 points versus 7 points in each group [95% CI 5 to 10]; p = 1.000) were not different between the two groups at a mean of 13 years’ follow-up. Radiographic parameters such as the femorotibial angle (mean 2° ± 2° valgus in the robotic-assisted TKA group versus 3° ± 3° valgus in the conventional TKA group [95% CI 1 to 5]; p = 0.897), femoral component position (coronal plane: mean 98° in the robotic-assisted TKA group versus 97° in the conventional TKA group [95% CI 96 to 99]; p = 0.953; sagittal plane: mean 3° in the robotic-assisted TKA group versus 2° in the conventional TKA group [95% CI 1 to 4]; p = 0.612) and tibial component position (coronal plane: mean 90° in the robotic-assisted TKA group versus 89° in the conventional TKA group [95% CI 87 to 92]; p = 0.721; sagittal plane: 87° in the robotic-assisted TKA group versus 86° in the conventional TKA group [95% CI 84 to 89]; p = 0.792), joint line (16 mm in the robotic-assisted TKA group versus 16 mm in the conventional TKA group [95% CI 14 to 18]; p = 0.512), and posterior femoral condylar offset (24 mm in the robotic-assisted TKA group versus 24 mm in the conventional TKA group [95% CI 21 to 27 ]; p = 0.817) also were not different between the two groups (p > 0.05). The aseptic loosening rate was 2% in each group, and this was not different between the two groups. With the endpoint of revision or aseptic loosening of the components, Kaplan-Meier survivorship of the TKA components was 98% in both groups (95% CI 94 to 100) at 15 years (p = 0.972). There were no between-group differences in terms of the frequency with which complications occurred. In each group, 2% of knees (15) had a superficial infection treated with intravenous antibiotics for 2 weeks. No deep infection occurred in these knees. In the conventional TKA group, 0.8% of knees (six) had a motion limitation (< 60°).
Conclusions
At a minimum follow-up of 10 years, we found no differences between robotic-assisted TKA and conventional TKA in terms of functional outcome scores, aseptic loosening, overall survivorship, and complications. Considering the additional time and expense associated with robotic-assisted TKA, we cannot recommend its widespread use.
Level of Evidence
Level I, therapeutic study.
Introduction
Although good long-term results of conventional TKA have been obtained in younger patients with osteoarthritis or rheumatoid arthritis [4, 5, 7-9, 11, 15, 16, 19, 28, 37, 38], robotic-assisted TKA was introduced with the goal of improving implant alignment, particularly in younger patients [3, 6, 13, 23-26, 30, 36]. Several comparative studies of conventional and robotic-assisted TKA have demonstrated that improved component alignment was obtained by using a robotic-assistance compared with conventional TKA instrumentation [22, 30, 35, 36, 39].
To our knowledge, no long-term randomized trial has compared robotic-assisted TKA and conventional TKA, particularly in younger patients. It is crucial to determine whether any potential implant-alignment improvements (or reductions in numbers of alignment outliers) associated with robotic-assisted TKA results in improved long-term outcomes scores or implant survivorship.
We conducted a large randomized, controlled trial of robotic-assisted versus conventional TKA with long-term (10-year minimum) follow-up, to determine whether robotic-assisted TKA was superior to traditional TKA in terms of (1) functional results based on Knee Society, WOMAC and UCLA Activity scores; (2) numerous radiographic parameters, including component and limb alignment, (3) Kaplan-Meier survivorship, and (4) complications specific to robotic-assistance, including pin tract infection, peroneal nerve palsy, pin-site fracture, or patellar complications.
Patients and Methods
This study was a registered, prospective, randomized controlled trial. From January 2002 to February 2008, one surgeon (S-HY) performed 975 robotic-assisted TKAs in 850 patients and 990 conventional TKAs in 849 patients. Among these patients, 1406 were eligible for participation in this study based on prespecified inclusion criteria. Patients younger than 65 years who had an end-stage of osteoarthritis of both knees were included. No patients older than 65 years were randomized because we anticipated long-term follow-up. Patients were excluded if they had inflammatory arthritis, or they had a foot or ankle disorder that limited walking. Of those 100% (1406) patients agreed and were randomized, with 700 patients (750 knees) receiving robotic-assisted TKA and 706 patients (766 knees) receiving conventional TKA. Of those 96% (674 patients) in the robotic-assisted TKA group and 95% (674 patients) in the conventional TKA group were available for follow-up at a mean of 13 (± 5) years. Consequently, the authors evaluated 674 patients (724 knees) in each group for clinical, radiographic, and CT scan evaluation at a mean (range) of 13 years (10 to 15 years) follow-up (Fig. 1). The study was registered in the Clinical Trials.gov Protocol Registration System (Trial number, NCT 03659318). We obtained institutional review board approval for the study, and we acquired informed consent from each patient.
Fig. 1.
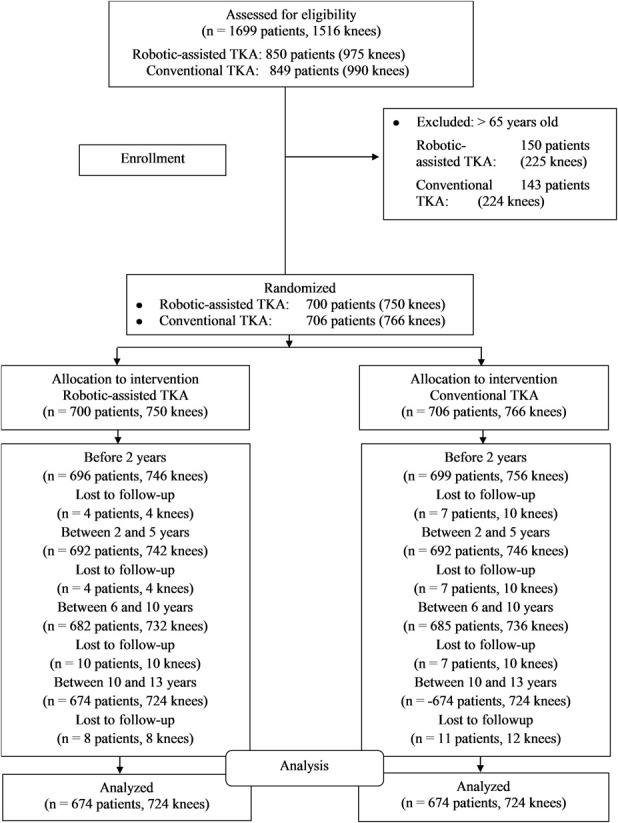
A Consolidated Standard of Reporting Trials (CONSORT) flow diagram is shown. In all, 724 knees in 674 patients were treated with robotic-assisted TKA and another 724 knees in 674 patients were treated with conventional TKA.
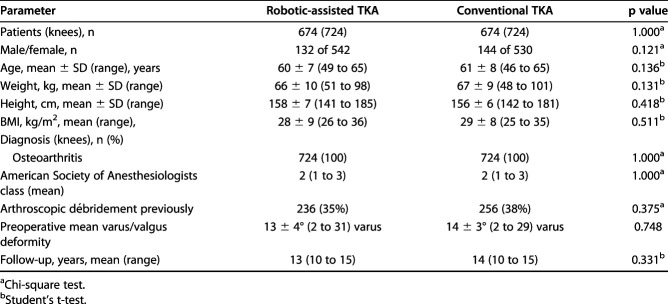
Although the learning curve with this ROBODOC® system (Integrated Surgical Systems Inc, Davis, CA, USA) was not addressed in this study, the surgeon (S-HY) who performed the procedures in this report performed 30 robotic-assisted TKAs using the system before the first patient was enrolled in this study. The robotic-assisted TKA cohort consisted of 542 women and 132 men with a mean (range) age of 60 ± 7 years (49 to 65 years), and mean (range) BMI of 28 ± 9 kg/m2 (26 to 36 kg/m2). Ninety percent of patients (609) had varus knees and 10% of patients (65) had valgus knees. The conventional TKA group consisted of 530 women and 144 men with a mean (range) age of 61 ± 8 years (46 to 65 years) and a mean (range) BMI of 29 ± 8 kg/m2 (25 to 35kg/m2). In all 93% (627) of patients had varus knees and 7% (47) of patients had valgus knees. Other demographic variables including preoperative deformity (mean, 13° varus in the robotic-assisted TKA group and 14° varus in the conventional TKA group), history of prior arthroscopic procedures and The American Society of Anesthesiologists (ASA) physical status classification system, which was used to measure the overall health status of each patient, did not differ between the groups (Table 1).
Table 1.
Patient demographics
Randomization to a robotic-assisted or conventional manual jig-based TKA was done by the allocation ratio 1:1 between the two groups using a computer program, and patients were not blinded to the procedure performed. All operations were performed by one surgeon (S-HY) who was experienced in both conventional TKA and robotic-assisted TKA. The measured resection technique was used in both groups. In the conventional TKA group, 10 mm of tibial bone was resected from the less-deficient side with a 7° posterior tibial slope. Anterior cortical reference was used for the AP cut of the distal part of the femur. Femoral component rotation was determined with use of three reference axes: (1) the transepicondylar axis, (2) the medial trochlear line (Whiteside line [1]), and (3) 3° of external rotation relative to the posterior aspect of the femoral condyles. Tibial component rotation was aligned with the medial one third of the tibial tubercle. Ligamentous balance was established first in knee extension and then in knee flexion with the use of a tensor in both groups.
Robotic-assisted TKA was carried out in two steps. CT-based preoperative planning using ORTHODOC (Integrated Surgical Technology Corp, Davis, CA, USA) (Fig. 2) was performed in the first step before the day of surgery, and robotic-assisted surgery using the ROBODOC surgical assistance was performed in the second step. The operating surgeon carried out preoperative ORTHODOC planning for the femoral and tibial components [15, 34,36]. The size and position of the femoral and tibial component was selected in 3-D using the ORTHODOC workstation [15, 33].
Fig. 2.

This photograph depicts the robotic set up.
While the surgery was performed, the knee was flexed to approximately 70° to 80° using a special leg holder. The leg was fixed to the ROBODOC base using two Steinman and Hoffman fixation systems (Stryker Osteosynthesis, Geneva, Switzerland), one each for the femur and tibia. Two recovery markers and one bone motion monitor were installed into the femur and tibia. Surface registration and verification were performed using the ROBODOC Digi Match registration system. Next, under direct control with surgeon supervision, the ROBODOC milled the distal femur and proximal tibia according to the plan generated in ORTHODOC. The soft tissues were protected carefully in the ROBODOC workspace. Once cutting was complete, the ROBODOC device was removed from the operative field.
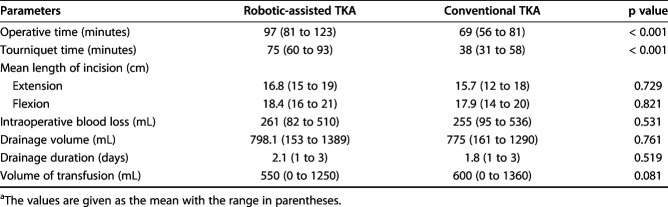
A Duracon® posterior cruciate-substituting total knee prosthesis (Stryker Orthopedics, Mahawh, NJ, USA) was used in each knee. The patella was resurfaced in 10 knees in each group and was not resurfaced in the remaining knees. In the beginning of these study, we had planned to resurface the patella. After the 10 knees in each group were resurfaced patella, we felt that resurfacing patella would not influence the results of robotic or conventional TKA. Therefore, we did not resurface the remaining patellae. All implants were cemented after pulsed lavage irrigation, drying, and pressurization of vacuum-mixed cement. As would be expected, operative and tourniquet times were longer in the robotic-assisted TKA group than those in the conventional TKA (Table 2).
Table 2.
Operative dataa
Prophylactic antibiotics were administered for 24 hours. A mechanical compression device was applied for 14 days for thromboprophylaxis in all patients who were hospitalized for this time period. On the second postoperative day, patients in both groups started walking with full weightbearing using crutches or a walker. All patients were discharged home from the hospital. All patients were advised to use crutches or a walker for 4 to 6 weeks to prevent a fall and a cane thereafter as needed.
Follow-up patient examinations were conducted at 3 months and 1 year postoperatively and every 2 to 3 years thereafter. A research associate (J-WP) who was not part of the surgical team recorded patient’s study outcomes. The Knee Society knee [12] and WOMAC scores [2] were assessed preoperatively and at the latest follow-up visit. Degree of pain with activity was scored on a 10-point VAS, with 0 meaning no pain and 10 meaning severe pain. The UCLA activity score assessed activity level at the latest follow-up visit [40]. To measure the range of knee motion preoperatively and at each follow-up, a standard (60-cm) goniometer was used. A research associate (J-WP ) who was not part of the surgical team recorded these data.
Standing AP hip-to-ankle radiographs, supine AP and lateral radiographs, and skyline patellar radiographic were made preoperatively and at each follow-up. The radiographs were evaluated by one observer (J-WP ), who was not a member of operating team, to determine the limb anatomic axis, component alignment, joint line, posterior femoral condylar offset, and the presence and location of radiolucent lines with use of Knee Society guidelines [12]. All radiographs were made under fluoroscopic guidance to control knee rotation. One observer (J-WP) who was not part of the operative team analyzed and recorded radiographic data at the latest follow-up visit. We assessed loosening (defined as change in the position of the components) using plain radiographs, osteolysis using CT scans at the latest follow-up visit, and component and limb alignment on mechanical axis radiographs.
All patients underwent a CT scan between 10 and 15 years with use of a multislice scanner (General Electric Light Speed Plus; GE Medical System, Milwaukee, WI, USA) to determine the rotational alignment of the components and evidence of osteolysis. The CT scan sequence was between 10 cm proximal to the superior pole of the patella and 10 cm distal to the tibial tuberosity and was made in contiguous 2.5-mm slices. The rotational alignment of the femoral and tibial components was measured as noted in previous studies [15-18]. Osteolysis was defined as a nonlinear region of periprosthetic cancellous bone loss with definable margins. One author (J-WP), who was not part of the surgical team, examined all CT scans.
All radiographic and CT parameters were measured three times (with a 3-day interval between measurements). To determine intraobserver agreement for measurements for all radiographic and CT scan parameters, the chance-corrected kappa coefficient [20] was calculated as previously reported [17]. Intraobserver agreement ranged from 0.95 to 0.97.
We identified the complications that might be specifically related to robotic assistance, including soft tissue damage, deep infection, pin-site fracture, pin tract infection, patellar tendon disruption, patellar dislocation, patellar fracture, supracondylar fracture, or peroneal nerve palsy.
Statistical Analysis
Lee et al. [21], in 2017, found the minimum clinically important difference (MCID) for Knee Society function score to be between 6.1 and 6.4 and for Knee Society knee score to be between 5.3 and 5.9 after TKR. Our study was carried out before 2017 and MCID was not used for the study. An a priori power calculation was performed with use of a clinically relevant difference in the Knee Society score to be 5 points and a SD of 5 points to match the MCID of the Knee Society with a power of 0.99 (α = 0.05 and β = 0.99) which revealed that a total of 628 patients would be needed in each group. To evaluate whether the axial alignment followed a normal (Gaussian) distribution, we used the Kolmogorov-Smirnov test [32, 33]. To assess the homogeneity of variance (constant variance), we used the Levine test [29]. We used an unpaired Student’s t-test, with the assumption of homogeneity of variance used as appropriate, to compare the limb alignment and surgery duration. We assessed the differences between the two groups with regard to the Knee Society, WOMAC and UCLA activity scores with the Student’s paired t-test and the Pearson nonparametric chi-square test. The knee ROM was compared between the two groups with use of a two-way repeated-measures ANOVA. We used nonparametric chi-square tests to compare complication rates, radiographic, and CT scan data between the two groups.
The level of significance was set at p < 0.05. Kapan-Meier survivorship analysis was carried out to determine the cumulative rate of survival of the implant during the period of the study with revision for any reason or aseptic loosening as the endpoint [14]; the 95% CI at certain times was calculated with the formula of Greenwood [10].
Results
Functional Outcomes
There was no difference in any clinical outcome measure at the latest follow-up for patients who received robotic-assisted TKAs compared with those who received conventional TKAs. There was no difference in mean total Knee Society knee scores (93 ± 5 points versus 92 ± 6 points, respectively; mean difference 1 point [95% confidence interval 0.8 to 2.4 points]; p = 0.321). There were no differences between the groups in terms of the proportions of patients with residual pain; in the robotic-assisted TKA group, 85% of patients (573 of 674) had no pain, 13% of patients (88) had mild pain, and 2% of patients (13) had severe pain at latest follow-up. In the conventional TKA group, 82% of patients (553 of 674 patients) had no pain, 16% (108) had mild pain, and 2% (13) had severe pain at latest follow-up (p = 0.598). There was no difference (95% CI 16 to 22; p = 0.981) in the mean WOMAC scores (18 ± 14 points and 19 ± 15 points) between the two groups at latest follow-up. The knee ROM in the robotic-assisted TKA group and conventional TKA group was not different preoperatively (128° ± 6° versus 129° ± 8°; p = 0.725) or at latest follow-up (125 ± 6° versus 128 ± 7°; p = 0.321). Mean UCLA activity scores in the robotic-assisted TKA group and conventional TKA group were not different preoperatively (2 points versus 2 points, 95% CI 1 to 4) or at latest follow-up (7 points versus 7 points, 95% CI 5 to 10; p = 1.000). Using the Bonferroni method for multiple comparison correction, the mean operation and tourniquet times were longer in the robotic-assisted TKA group than in the conventional TKA group (Table 2).
Radiographic Outcomes
There were no differences between the two groups at latest follow-up with regard to any radiographic parameters measured, including limb alignment, component alignment, or aseptic loosening (Table 3). If one presumes that it is desirable to align the knee to within ± 3° of a neutral mechanical axis, the prevalence of outliers was 14% in the robotic-assisted TKA group and 26% in the conventional TKA group (p = 0.035). However, if one assumes a tolerance level of ± 5° from a neutral mechanical axis, the prevalence of outliers was 4% in the robotic-assisted TKA group and 6% in the conventional TKA group (p = 0.731). There was also no difference in rotational alignment of the femoral component from transepicondylar axis (5° ± 4° versus 5° ± 5° external rotation [95% CI 4 to 7]; p = 0.786) or tibial component (6° ± 7° versus 6° ± 8° external rotation [95% CI 4 to 10]; p = 0.762) in the CT scans analyzed between the two groups at latest follow-up. No knee in either group had evidence of osteolysis on either plain radiographs or CT scans. In each group, 2% of knees (15) had aseptic loosening of the femoral and/or tibial component.
Table 3.
Radiographic results at final follow-up (15 years)a
Component Survivorship
There were no between-group differences in terms of survivorship. Kaplan-Meier survivorship [14] analysis, with revision or aseptic loosening defined as the endpoint, showed no differences between the groups with a 98% implant survival proportion for both groups (95% CI 94 to 100) at 15 years after the operation (p = 0.972). A deviation between 3° to 5° from the mechanical axis of the lower limb did not increase the rate of aseptic loosening.
Complications
There were no between-group differences in terms of the frequency with which complications occurred. In all, 0.6% of knees (four) in each group had a superficial infection, and they were treated with intravenous antibiotics for 2 weeks. No deep infection occurred in these knees. In the conventional TKA group, 0.6% of knees (four) had motion limitation (< 60°). No knee in either group had a pin site fracture, pin tract infection, patellar dislocation, patellar fracture, supracondylar fracture, or peroneal nerve palsy.
Discussion
Robotic-assisted TKA has the potential to improve the alignment of the TKA components, and as a result could lead to improved patient functional outcome and survivorship of TKA implants [3, 6, 13, 22-26, 31]. To our knowledge, no long-term randomized trial has compared robotic-assisted TKA and conventional TKA. In this large, randomized trial with analysis at a minimum of 10-years after surgery, we found no differences between the robotic-assisted and conventional approach to TKA alignment in terms of outcomes scores, mean implant or limb alignment, survivorship, or complications. Although we found a small reduction in the proportion of knees aligned more than of 3° away from neutral when robotic assistance was used, we found no between-group difference if the outlier cutoff was 5°, and no reduction in aseptic loosening in the robotic-assisted group.
There are several limitations of this study. First, it should be noted that current studies on function and survivorship with robotic-assisted TKA are analyses of one particular autonomous robotic system. This particular system is geared exclusively to modulating bone cuts and has no algorithm for balancing soft tissues within the knee. It is possible that functional outcomes would differ if the robotic device reported on was also able to quantify soft tissue balance. Second, there were few obese patients. Eleven percent of patients (74 of 674) in the robotic-assisted TKA group and 12% (81 of 674) in the conventional TKA group had > 30 kg/m2 BMI; no patients had morbid obesity (> 40 kg/m2 BMI), a group that may benefit more from robotic assistance given the difficulties associated with identifying anatomic landmarks for accurate component position. However, even if robotic assistance is shown to improve the radiographic alignment of the components in patients with morbid obesity, the question still remains whether it will improve long-term clinical outcome or survivorship of the TKA. Our study does not address this. Third, our study population has a preponderance of women with low body weight and good preoperative knee ROM, which is typical of the Korean population; these factors might limit general applicability to other patients or practice settings. On the other hand, the patients in this series engaged in high-level activities, such as farming, squatting, and lifting. Fourth, we performed no interobserver comparisons of the radiologic and CT measurements to confirm the measurements by one observer, and this can lead to bias in interpreting loosening and osteolysis, leading to either underestimation or overestimation. However, intraobserver agreements for the radiographic and CT measurements were 0.95 to 0.98, indicating excellent reproducibility. Fifth, the preoperative deformities included greater varus deformities than in most non-Asian studies and few valgus deformities, possibly limiting general applicability to other patients or practice settings. Finally, there may be differences that we did not account for between the patients with un-resurfaced patellae and those few that were resurfaced, but we found no differences overall and did not perform a separate analysis on these 20 patients.
The findings of our study suggest that there were no differences in Knee Society knee and function scores, WOMAC scores, UCLA activity scores, or range of knee motion between the two groups at mean of 13 years follow-up. Given the relative novelty of robotic technology and limited market penetration, there are few studies addressing the impact of robotic-assistance on such functional outcome parameters. Song et al. [36] found no difference in original Knee Society knee scores between robotic-assisted TKAs and conventional TKAs. Likewise, Yang et al. [39] reported no differences in the functional outcomes of WOMAC score, Hospital for Special Surgery knee score, knee ROM, or VAS scores between robotic-assisted TKA and conventional TKA. Liow et al. [22] also observed no differences with the Knee Society knee and functional scores between robotic-assisted and conventional TKA. These studies are not dissimilar to studies of computer navigation assistance in TKA. Kim et al. [17, 18] found no differences between the navigated and conventional TKA in knee ROM, Knee Society knee function scores, WOMAC, or UCLA activity scores at 15 years follow-up. It seems important that any technique that adds cost (or risks associated with novelty) should deliver results that patients can perceive as improvements; that goal was not achieved in this study with robotic-assisted TKA.
We found that there were also no differences between the two groups in terms of various radiographic parameters, including tibiofemoral alignment, femoral and tibial component position, posterior femoral condylar offset, joint line level, and osteolysis. Bellemans et al. [3] and Decking et al. [6] found that robotic-assisted TKA demonstrated promising Knee Society knee functional results with low rates of component malalignment. Park and Lee [30] demonstrated that overall knee alignment was not different between robotic-assisted TKA and conventional TKA. Song et al. [35, 36] demonstrated a more precise mean neutral mechanical axis for robotic-assisted TKA of 0.2° compared with 1.2° for conventional TKA. However, they observed no difference between the two groups regarding coronal alignment of either the tibial or femoral components. Among three clinical randomized trials [22, 35, 36], the studies revealed no outliers (+/- 3° from mechanical axis) with the use of robotic-assisted TKA while conventional TKA had outlier rates of between 19% and 24%. In the present study, the prevalence of outliers was higher in the conventional TKA group than in robotic-assisted TKA, if outliers were judged as ± 3° from a neutral mechanical axis but was not different between the two groups if the tolerance level was ± 5°. Although ± 3° mechanical axis is generally considered the optimum target, controversy over this goal exists [17, 18]. Paratte et al. [31] found no difference in 15-year implant survival rates between “aligned” and “malaligned” groups using ± 3° outliers as the standard. In the current series, we also found no difference in clinical outcomes and the survivorship of the implants between aligned (< 3°) and “malaligned” (> 3°) group. A key stated goal of robotic-assisted TKA is improvement in radiographic parameters [3, 22, 25, 35, 36, 39]; this was not achieved here.
In the current series, we noted excellent survivorship of TKAs in both groups at 15 years, which we attribute to appropriate surgical technique in both groups. There is limited evidence whether long-term survivorship of robotic-assisted TKA is better than conventional TKA in patients 65 years and younger. In the retrospective study by Yang et al. [39], there was no difference in the survivorship between the robotic-assisted and conventional TKAs in patients younger than 65 years old. However, several authors [5, 7, 8, 15, 16, 19, 27, 38] have reported good results with conventional TKA in younger patients with osteoarthritis at long-term follow-up. Others have suggested that the alignment improvements anticipated with robotic-assisted TKA might be associated with improved survivorship [3, 22, 24, 25, 35, 36]. This benefit was not observed in our large, randomized trial, and so this calls into serious question the value of this new technology, which is associated with greater cost.
In the current study, the frequency of complications directly attributable to differences in surgical technique was low in both groups, and there were no differences between the two groups. Park and Lee [30] reported a high incidence of complications (six of 32 knees), including superficial infection, patellar tendon rupture, patellar dislocation, supracondylar fracture, patellar fracture, and peroneal nerve injury, during the learning curve for robotic-assisted TKA. However, no major adverse results were observed after the learning curve of (30 cases). Song et al. [36] also reported that there were no differences in complications between the robotic-assisted and conventional TKAs.
At a minimum follow-up of 10 years, we found no differences between robotic-assisted TKA and conventional TKA in terms of functional outcome scores, aseptic loosening, overall survivorship, and complications. Although we observed a small improvement in the proportion of knees with ± 3° deviation from a neutral mechanical axis in the robotic TKA group, there was no such difference if the definition of an outlier was taken to be ± 5° as is commonly done [27], and, importantly, there was no between-group difference in terms of aseptic loosening or overall survival. In addition, functional outcomes and the frequency of complications did not differ between the robotic TKA and conventional TKA groups. Considering the additional time and expense associated with robotic-assisted TKA, we cannot recommend its widespread use.
Acknowledgments
We thank Ms DooRi Kim for her recording of clinical, radiographic, and CT scan findings.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am. 1995;77:1331-1334. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1998;15:1833-1840. [PubMed] [Google Scholar]
- 3.Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. 2007;464:111-116. [DOI] [PubMed] [Google Scholar]
- 4.Crowder AR, Duffy GP, Trousdale RT. Long-term results of total knee arthroplasty in young patients with rheumatoid arthritis. J Arthroplasty. 2005;20(Suppl 3):12-16. [DOI] [PubMed] [Google Scholar]
- 5.Dalury DF, Barrett WP, Mason JB, Goldstein WW, Murphy JA, Roche MW. Midterm survival of a contemporary modular total knee replacement: a multi-centre study of 1970 knees. J Bone Joint Surg Br. 2008;90:1594-1596. [DOI] [PubMed] [Google Scholar]
- 6.Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand. 2004;75:573-579. [DOI] [PubMed] [Google Scholar]
- 7.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriquez D. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79:575-582. [DOI] [PubMed] [Google Scholar]
- 8.Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87:598-603. [DOI] [PubMed] [Google Scholar]
- 9.Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(Suppl 2):67-70. [DOI] [PubMed] [Google Scholar]
- 10.Greenwood M. The Natural Duration of Cancer. Reports on Public Health and Medical Subjects . London, UK: Her Majesty’s Stationery Office; 1926:1-26. [Google Scholar]
- 11.Hofmann AA, Heithoff SM, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res. 2002;404:102-107. [DOI] [PubMed] [Google Scholar]
- 12.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society Clinical Rating system. Clin Orthop Relat Res. 1989;248:13-14. [PubMed] [Google Scholar]
- 13.Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31:2353-2363. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan EL, Meier P. Nonparametric estimation from incomplete observation. J Am Stat Assoc. 1958;53:457-481. [Google Scholar]
- 15.Kim Y-H, Choi Y, Kim J-S. Osteolysis in well-functioning fixed-and mobile-bearing TKAs in younger patients. Clin Orthop Relat Res. 2010;468:3084-3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y-H, Kim J-S, Choe J-W, Kim H-J. Long-term comparison of fixed-bearing and mobile-bearing total knee replacements in patients younger than fifty-one years of age with osteoarthritis. J Bone Joint Surg Am. 2012;94:866-873. [DOI] [PubMed] [Google Scholar]
- 17.Kim Y-H, Park J-W, Kim J-S. Computer-navigated versus conventional total knee arthroplasty. A prospective randomized trial. J Bone Joint Surg Am. 2012;94:2017-2024. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y-H, Park J-W, Kim J-S., Chitranjan S. Ranawat Award: Does computer navigation in knee arthroplasty improve functional outcomes in young patients? Clin Orthop Relat Res. 2018;476:6-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krackow KA, Pepe CL, Galloway EJ. A mathematical analysis of the effect of flexion and rotation on apparent varus/valgus alignment at the knee. Orthopedics. 1990;13:861-868. [DOI] [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] [Google Scholar]
- 21.Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sport Traumatol Arthrosc. 2017; 25: 3354-3359 [DOI] [PubMed] [Google Scholar]
- 22.Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014;29:2373-2377. [DOI] [PubMed] [Google Scholar]
- 23.Lonner JH. Indications for unicompartmental knee arthroplasty and rationale for robotic arm-assisted technology. Am J Orthop. 2009;38(2 Suppl):3-6. [PubMed] [Google Scholar]
- 24.Lonner JH. Robotic arm-assisted unicompartmental arthroplasty. Seminars in Arthroplasty. 2009;20:15-22. [PubMed] [Google Scholar]
- 25.Lonner JH, Hershman S, Mont M, Lotke PA. Total knee arthroplasty in patients 40 years of age and younger with osteoarthritis. Clin Orthop Relat Res. 2000;380:85-90. [DOI] [PubMed] [Google Scholar]
- 26.Lonner JH, Moretti VM. Evolution of image-free robotic assistance in unicompartmental knee arthroplasty. Am J Orthop (Belle Meade NJ). 2016;45:249-254. [PubMed] [Google Scholar]
- 27.Matziolis G, Krocher D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007; 89: 236-243. [DOI] [PubMed] [Google Scholar]
- 28.Mont MA, Lee CW, Sheldon M, Lennon WC, Hungerford DS. Total knee arthroplasty in patients </=50 years old. J Arthroplasty. 2002;17:538-543. [DOI] [PubMed] [Google Scholar]
- 29.National Institute of Standards and Technology. Statistical Engineering Division. Levene test. Dataplot. Available at: https://www.itl.nist.gov/div898/software/dataplot/refman1/auxillar/levetest.htm. September 12, 2008.
- 30.Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. 2007;22:1054-1059. [DOI] [PubMed] [Google Scholar]
- 31.Paratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen year survival of modern cemented knee replacements. J Bone Joint Surg Am. 2010;92:2143-2149. [DOI] [PubMed] [Google Scholar]
- 32.Riffenburgh RH. Tests on the distribution shape of continuous data. In: Riffenburgh RH, ed. Statistics in Medicine. Amsterdam: Elsevier; 2006:370-380. [Google Scholar]
- 33.Rosner B. Fundamentals of Biostatistics. 5th ed. Pacific Grove, CA: Duxbury Press; 2000:527-530. [Google Scholar]
- 34.Shepherd DE, Seedhom BB. Thickness of human articular cartilage in joints of the lower limb. Ann Rheum Dis. 1999; 58:27-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2011;19:1069-1076. [DOI] [PubMed] [Google Scholar]
- 36.Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471:118-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stern SH, Bowen MK, Insall JN, Scuderi GR. Cemented total knee arthroplasty for gonarthrosis in patients 55 years old or younger. Clin Orthop Relat Res. 1990;260:124-129. [PubMed] [Google Scholar]
- 38.Tai CC, Cross MJ. Five-to 12-years follow-up of a hydroxyapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg Br. 2006;88:1158-1163. [DOI] [PubMed] [Google Scholar]
- 39.Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic total knee arthroplasty with a cruciate-retaining implant: A 10-year follow-up study. Clin Orthop Surg. 2017;9:169-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890-895. [DOI] [PubMed] [Google Scholar]