Abstract
Background:
The network approach to psychopathology has become increasingly popular. Little research has examined the dynamic network structure of mental disorders, and, to date, no study has investigated the network dynamics of positive affect, negative affect, and physical activity in bipolar disorder. This represents the first study to estimate the dynamic network structure of affect and physical activity in individuals with and without bipolar I disorder.
Methods:
An intensive longitudinal design was used to assess positive affect, negative affect, and actigraphy-based estimates of physical activity. The overall sample consisted of 32 adults with bipolar I disorder and 36 healthy control participants. Eligible participants underwent an 8-week assessment period, in which once-per-day ratings of affect and actigraphy estimates were obtained. Participants were re-assessed on baseline measures afterwards. Dynamic network analysis was used to examine the network structure of affect and physical activity over time. Multilevel models were used to examine the relationship between autocorrelation and changes in depression symptoms among participants with bipolar disorder.
Limitations:
The network analyses assume stationarity. Future research should consider time-varying multilevel network models to better account for time trends.
Results:
The results of the temporal networks indicated that the directed edges between positive and negative affect were mostly positive among individuals with bipolar I disorder. Among healthy control participants, the directed edges between positive and negative affect were mostly negative in direction. Physical activity, as assessed by daily actigraphy indices, was more densely connected in the healthy control network than the bipolar disorder network. Furthermore, the results indicated that critical slowing down predicted worsening of mood symptoms in the bipolar I disorder group.
Conclusions:
This study suggests that certain dynamic patterns of affect may be an underlying process that contributes to the maintenance of bipolar disorder. These results have both theoretical and practical implications.
Keywords: Bipolar disorder, Network analysis, Actigraphy, Time series
1. Introduction
According to traditional perspectives of psychopathology, affective disorders are often presumed to be the result of latent disease mechanisms that are responsible for the covariance of observable symptoms (Borsboom and Cramer, 2013). Much psychopathology research relies on the assumption that affective disorders resemble taxonic entities that are relatively stable across time. Recently, there has been increasing interest in alternative accounts of mental disorders. One prominent approach is the network perspective, which emphasizes the direct connections between features of psychopathology and does not require the assumption that a latent disease mechanism is responsible for their co-occurrence (Borsboom and Cramer, 2013; Hofmann et al., 2016). To date, much network research on mental disorders, such as affective disorders, has largely been circumscribed to cross-sectional designs and the examination of traditional symptoms and impairment (Fried et al., 2016; Curtiss and Klemanski, 2016; Curtiss et al., 2018). Although disturbances in affect are core features of many psychiatric disorders, affect itself is rarely a static state that remains invariant across time. Instead, presentations of affect in mental disorders exhibit dynamic patterns that fluctuate in accordance with life experiences and stressors (Koval et al., 2013). Little is known about the temporal network dynamics of affect in clinical samples, which has relevance to psychiatric disorders that are characterized by dysregulated and pathological expressions of affect such as in bipolar I disorder.
Specifically, the study of bipolar I disorder allows for insights gained into the temporal dynamics of affect, given that clinical presentations of this condition involve shifts in affect ranging between episodes of mania (i.e., abnormally elevated or irritable mood) and depression (i.e., persistently low mood and/or anhedonia) (APA, 2000). Even in individuals with remitted bipolar disorder who experienced subsyndromal depression, large shifts in the dynamics of negative affect were experienced in response to life stressors (Havermans et al., 2010). To date, no research has been undertaken to investigate affect in bipolar disorder from a dynamic network perspective. Understanding the network dynamics of affect in bipolar disorder can afford valuable insight into dynamic processes that contribute to affective psychopathology.
1.1. Theories of positive affect and negative affect
One of the most researched and well-characterized attributes of affect is valence—the general experience of pleasantness (positive) or unpleasantness (negative) of stimuli or situations (Lerner and Keltner, 2000; Mauss and Robinson, 2009). Despite the inherent complexity of affect, the broad dimensions of positive and negative valence have provided an overarching framework for understanding its phenomenology. The relationship between these positive and negative dimensions is regarded as clinically important for understanding the functional significance of affect, how it is regulated, and the circumstances under which pathological expressions of affect arise. A large literature has examined the role of valence in adaptive and maladaptive patterns of affect (Barlow et al., 2004; Hofmann et al., 2012). For instance, depressive episodes are characterized by pronounced deficits in positive affect and persistent, chronic negative affect (Brown et al., 1998; Beck, 2008), and manic episodes are characterized by persistent positive affect that remain invariant to context (Gruber, 2011; Johnson and Fulford, 2009).
Our understanding of affective psychopathology has been augmented by prominent models of affect valence. The traditional conceptualization of affect valence has been formalized as the circumplex model (CM) (Russell, 1980), which posits that positive affect and negative affect occupy opposite positions with respect to valence. Thus, savoring feelings of happiness or joy at a particular moment should be incompatible with the presence of sadness. According to this approach, affective states occupy a discrete position around a perimeter of space characterized by two cardinal dimensions: valence and arousal. At any given time, one can experience a single affective state distinguished by a specific valence and level of arousal. By contrast, the evaluative space model (ESM), an alternative model of affect, does not impose such restrictions on the compatibility of positive and negative affective states during an affective experience (Cacioppo et al., 1999; Larsen et al., 2001). The ESM permits several modes of affective activation, including co-activation and co-inhibition (Larsen et al., 2001). That is, co-activation would permit positive affect (e.g., happy) and negative affect (e.g., sad) to be simultaneously activated, whereas co-inhibition would require that positive affect inhibits the activation of negative affect and vice versa.
1.2. Network dynamics of affect and physical activity
Of note, the principal research program adopted by affective science has largely focused on affect as a static phenomenon (Houben et al., 2015). However, it is not well understood whether positive and negative affect co-activate each other or whether they are co-inhibitory. Little research has endeavored to understand temporal aspects of affect valence (Houben et al., 2015; Stavrakakis et al., 2015; Bodner et al., 2018) and, moreover, no research has delineated the dynamic network structure of individual facets of positive and negative affect over time. A dynamic network approach to affect valence can elucidate whether dynamic patterns of co-activation, co-inhibition or both emerge over time. Furthermore, the network dynamics of affect valence may have important implications in distinguishing health and psychopathology through differential dynamic patterns (e.g., co-activation versus co-inhibition) (Fisher, 2015; Hofmann et al., 2016; Nelson et al., 2017).
Beyond the network structure of positive and negative affect, it is of theoretical importance to determine the dynamic relationships occurring between affect valence and physical activity. A core feature of contemporary models of affective states is that they poise individuals to engage in affect-appropriate behaviors (e.g., withdraw when sad or engage when happy) (Scherer, 2005). Therefore, dynamic networks of positive and negative affect will also include daily actigraphy-based activity levels as a feature.
1.3. Critical slowing down in affect and physical activity
In addition to understanding the network dynamics of affect in bipolar disorder, it would be important to examine whether specific dynamic indices are predictive of sudden transitions in clinical severity. There has been a recent call to characterize psychopathology as a complex system, which possess certain dynamic characteristics that can predict the system’s behavior. A principal characteristic of complex systems is that they exhibit ‘tipping points’, which are critical transitions or sudden changes to a qualitatively different state. Critical slowing down has been explored as an important property of complex systems in other disciplines (e.g., aquatic food-web resources in ecology, chronic diseases in medicine, etc.) (Gsell et al., 2016; Rikkert et al., 2016). In accordance with the complex dynamic systems framework, system dynamics should recover more slowly from small perturbations when approaching an impending tipping point (Meisel et al., 2015). In affective science, critical slowing down might provide a framework for identifying tipping points in affective health (e.g., slower recovery time from a negative affective state after a significant life stressor may predict transitions in clinical status or severity). Indices of critical slowing down can be investigated by modeling temporal autocorrelation (van de Leemput et al., 2014). This is the first study to determine whether affect valence functions as an index of critical slowing down among individuals with bipolar I disorder.
1.4. Current study
In the current study, a dynamic network approach was employed to delineate the network structure of positive and negative affect, as well as physical activity. Furthermore, we examined whether critical transitions in severity of depression among participants with bipolar disorder can be predicted by indices of critical slowing down, which have been theoretically linked to sudden transitions or ‘tipping points’ in complex dynamic systems. Using an intensive longitudinal design, we evaluated the temporal dynamics of positive and negative affect in two groups: participants with no lifetime history of psychiatric disorders and a clinical group consisting of participants diagnosed with bipolar I disorder.
2. Methods
2.1. Participants
As part of a larger study (Gershon et al., 2012), we recruited 32 adults (ages 18–64) diagnosed with bipolar I disorder who were currently inter-episode and 36 healthy adults with no history of Axis-I psychiatric disorders. The two groups were matched on age and gender. Demographic characteristics are detailed in Supplementary Table 1.
The following eligibility criteria were required for individuals in the bipolar group: (a) DSM-IV-TR criteria (APA, 2000) for a diagnosis of bipolar I disorder and (b) no diagnosis of substance or alcohol abuse or dependence in the past six months based on DSM-IV-TR criteria. In addition, at study entry, participants in the clinical group were required to have achieved inter-episode status based on (1) the absence of a current (past month) depression, mania/hypomania, or mixed episode based on DSM criteria, and (2) scoring below established thresholds on two clinician-administered symptom scales: a score of less than 24 on the Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) (Rush et al., 1996) and a score of less than 12 on the Young Mania Rating Scale (YMRS) (Young et al., 1978). Participants were excluded for the presence of serious medical or neurological conditions known to influence daily activity patterns (e.g., Alzheimer’s disease, history of head trauma), an unstable living arrangement, or a primary sleep disorder.
A more detailed account of the procedures is discussed elsewhere (Gershon et al., 2012). The University of California, Berkeley Institutional Review Board approved all study procedures. In brief, after participants provided informed consent, completed a baseline assessment including in-person structured clinical interviews to establish lifetime history of Axis-I psychiatric disorders and, for participants in the bipolar disorder group, current inter-episode status. Eligible participants underwent an 8-week assessment period in which they provided once-per-day ratings of positive and negative affect using the PANAS, and completed continuous actigraphy. Participants were re-assessed for inter-episode status using clinical interviews at two time points: one month and two months following baseline.
2.2. Measures
2.2.1. Psychiatric disorders and symptom severity
To determine the presence of Axis-I psychiatric disorders, the Structured Clinical Interview for DSM-IV (SCID) (First et al., 2002) was administered. Diagnostic non-rater reliability for a randomly chosen subset of participants (n = 17) in the current study was excellent (k = 1.00). Two additional clinician administered instruments were used to assess current (past month) depression and mania symptom severity. The IDS-C is a 30-item instrument that measures current (past month) depression severity. Scores range from 0 to 84 (Rush et al., 1996). The YMRS contains 11-items to assesses current (past month) mania severity. Scores range from 0 to 60. Intra-class correlations between the original interviewer and an independent rater for a randomly chosen subset of participants (n = 42) were strong (r = 0.90 for IDS-C and r = 0.84 for YMRS). Only the IDS-C was employed for the primary analyses; the SCID and IDS-C were used to establish eligibility.
2.2.2. International positive and negative affect schedule-short form (I-PANAS-SF)
The I-PANAS-SF is a brief self-report measure that assesses positive and negative affect (Thompson, 2007). This instrument comprises of a set of non-redundant items that measure well-characterized domains of positive and negative affect. Of the ten items, five are indicators of positive affect (i.e., ‘active’, ‘alert’, ‘inspired’, ‘determined’, and ‘attentive’), and five measure negative affect (i.e., ‘ashamed’, ‘upset’, ‘hostile’, ‘nervous’, and ‘afraid’). Prior research has demonstrated that the I-PANAS-SF evidenced good reliability and validity (Thompson, 2007).
2.2.3. Actigraphy
Estimates of daily physical activity levels were obtained with Actiwatches (AW64, Respironics Inc., Bend OR) worn continuously on the wrist of the non-dominant hand (Sadeh et al., 1995). Physical movement data were sampled at 60 s intervals. Data derived from the watch’s accelerometer were downloaded and pre-processed using Respironics Actiware Version 5.5. Movement data were analyzed using functional principal components analysis (fPCA), which extracts orthogonal components from semi-continuous data (Ramsay et al., 2009). Four components were derived from this analysis, which together accounted for 80.1% of the variance in the movement data. The fPCA analysis and resulting components from this sample are described elsewhere (Gershon et al., 2016). In the current study, we used the first component of the fPCA analysis, which provides an overall index of daily activity.
2.3. Data analytic strategy
To interrogate the dynamic network structure, items from the PANAS and actigraphy-based activity levels (derived from fPCA analysis) were used to model the relationship between positive affect, negative affect, and physical activity data using the R package mlVAR (Epskamp et al., 2016). Each item on the PANAS, as well as the daily actigraphy-derived fPCA scores, was a node. Edges between nodes reflected directed partial regression coefficients. That is, each directed edge reflects a unique association between two nodes controlling for all other relationships in the network. Two network structures were modeled in the clinical and non-clinical group: (1) a dynamic network of positive and negative affect, and (2) a dynamic network of positive affect, negative affect, and daily actigraphy-derived fPCA scores.
Specifically, dynamic networks were constructed using multilevel vector autoregressive (VAR) analyses (Bringmann et al., 2013). In these models, a given node at time t was regressed onto all other time lagged t − 1 independent variables. All models were analyzed using fixed estimates procedure of mlVAR, whereby only the intercept is random. Thus, the fixed effect coefficients produced a weighted directed network, in which the temporal connections can be construed as an approximation of causality, akin to Granger causality (Granger, 1969; Bringmann et al., 2015). Visualizations of each network omitted non-significant edges in the interest of removing superfluous detail.
Node centrality was determined by computing three centrality indices: in-strength, out-strength, and betweenness. A node’s in-strength parameter denotes the sum of all weighted edges that are directed toward it, whereas a node’s out-strength parameter denotes the sum off all weighted edges that proceed from it to another node. The betweenness centrality parameter indicates the number of times that a node lies on the shortest path between any other pair of nodes. The principal centrality parameter emphasized in the current study is out-strength, which best reflects a node’s influence on other nodes in the network. Generally, node strength is more stable than other centrality parameters (e.g., betweenness, closeness, etc.) and, thus, serves as a good metric to quantify network stability (Fried et al., 2016).
In accordance with the complex dynamic systems framework, indices of critical slowing down were investigated by modeling temporal autocorrelation (van de Leemput et al., 2014). Multilevel models were specified such that a given affect variable at time t (e.g., rating of ashamed at time t) was regressed on its t − 1 score (e.g., rating of ashamed at time t − 1). This autoregression coefficient can be specified to have an interaction effect with pre-post changes in depression symptom severity scores (i.e., depression t1 – depression t2). A significant interaction effect would determine whether changes in depression symptom severity are associated with indices of critical slowing down (i.e., the temporal autocorrelation of a given affect variable). Multilevel models permit decomposition of within- and between-person effects (Krull and MacKinnon, 2001), whereby fixed effect and random effect components may be estimated. Person-mean centering was employed for all level 1 predictors, which provided unambiguous decomposition of within- and between-person effects (Curran and Bauer, 2011). Random effect components of the slope and intercept reflect individual differences.
Two-sided permutation tests were conducted to determine whether node out-strength differed between positive affect and negative affect nodes within each network (i.e., clinical and non-clinical), which would illuminate whether a certain affect cluster is more central in each network. In addition, differences in the out-strength centrality for positive and negative affect were compared across clinical and non-clinical networks.
3. Results
3.1. Dynamic network structure of PA and NA
Among individuals in the clinical group, results of the mlVAR network analyses demonstrated robust, positive associations both within and between nodes of a particular valence (Fig. 1a). For instance, the negative affect items formed a directed pathway proceeding from ‘hostile’ to ‘ashamed’ (β = 0.07, p < 0.01) and from ‘ashamed to ‘afraid’ (β = 0.01, p < 0.05), and the positive affect node ‘attentive’ was prospectively predictive of other positive affect items (i.e., ‘alert’ (β = 0.09, p < 0.01) and ‘determined’ (β = 0.09, p < 0.01)). Between-valence directed edges also emerged, as evidenced by the positive pathways from ‘ashamed’ to ‘alert’ (β = 0.04, p < 0.05) and ‘active’ (β = 0.06, p < 0.05), as well as from ‘afraid’ to ‘attentive’ (β = 0.04, p < 0.05).
Fig. 1. Dynamic network structure of PA and NA.
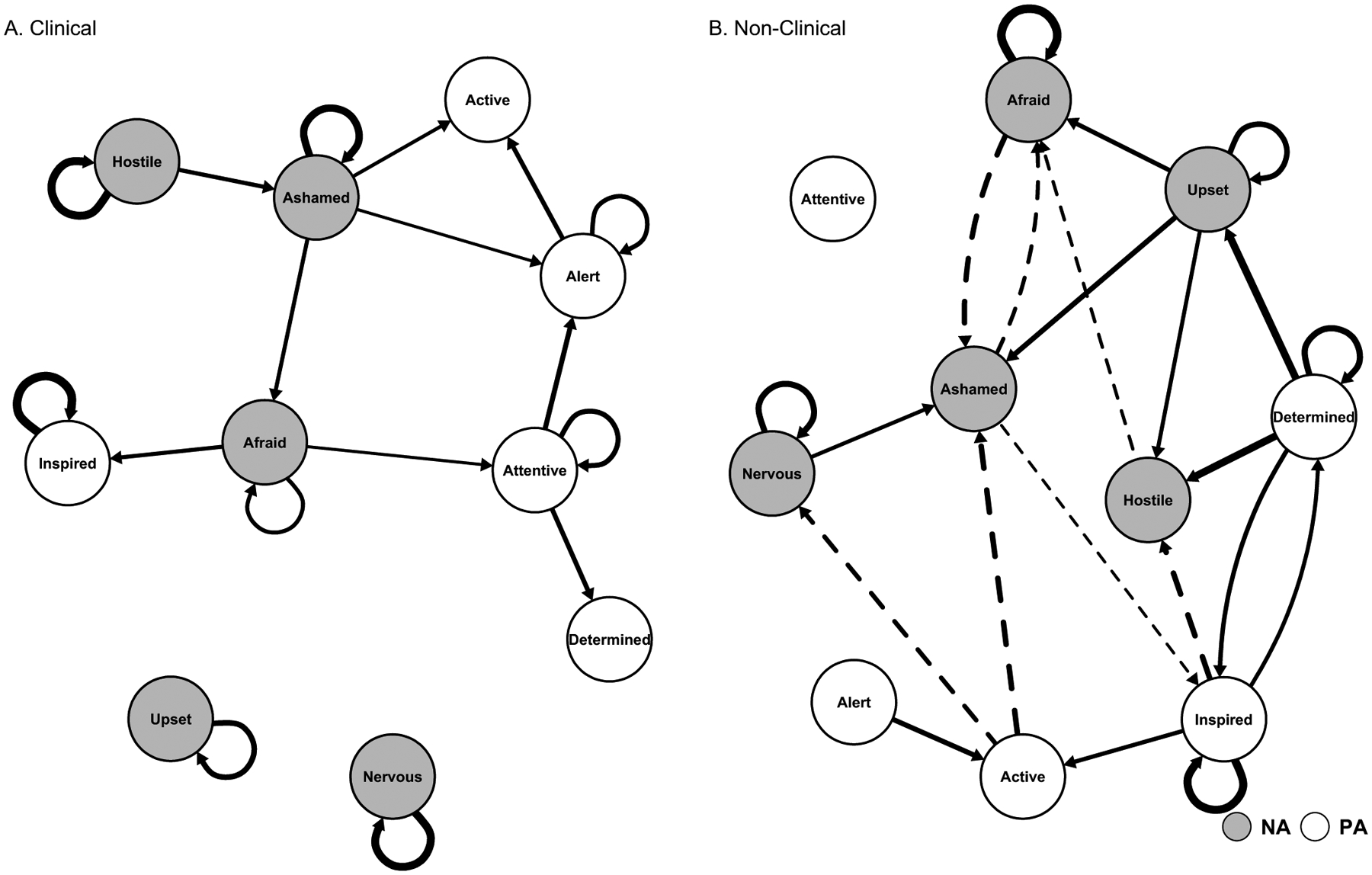
Note: In Figure 1A, positive directed edges emerged both within and between positive and negative affect nodes, suggesting temporal co-activation patterns characterize affective pathology. Fig. 1B reveals that positive directed edges are more frequent within nodes of a single valence than between oppositely valenced nodes. Thickness of arrow reflects strength of association. Solid arrows denote positive associations, whereas dashed arrows denote negative associations.
Although the dynamic network among individuals in the non-clinical group exhibited positive associations across nodes of the same valence, it also featured negative edges between nodes of opposite valence (Fig. 1b). That is, the majority of the directed edges were positive within nodes of positive affect (e.g., ‘inspired’ to ‘determined’ (β = 0.06, p < 0.05)) and negative affect (e.g., ‘upset’ to ‘ashamed’ (β = 0.08, p < 0.01)), whereas the majority of the between-valence directed edges were negative (e.g., ‘active’ to ‘ashamed’ (β = −0.09, p < 0.05)). Comparison of the clinical and non-clinical dynamic networks suggests that the clinical network comprises a significantly greater proportion of positive directed edges (100%) than the non-clinical network (58%, χ2 = 5.07, p < 0.05). This indicates that co-inhibition may be preserved in the non-clinical but not in the clinical sample.
3.2. Out-strength centrality comparisons
The centrality indices for the clinical and non-clinical dynamic networks are depicted in Supplementary Figs. 1 and 2, respectively. In the clinical dynamic network, ‘attentive’ and ‘ashamed’ were especially influential, possessing the highest out-strength centrality parameters (i.e., OS = 1.56 and OS = 1.50, respectively). In the non-clinical dynamic network, ‘determined’ and ‘upset’ exhibited the largest out-strength centrality parameters (i.e., OS = 2.01 and OS = 0.86, respectively).
Several permutation tests were conducted to facilitate comparisons of node centrality across positive and negative affect and across clinical and non-clinical groups. In the clinical dynamic network (Fig. 1a), no significant differences in out-strength emerged between positive affect nodes (M = 0.05) and negative affect nodes (M = 0.07) (z = 0.46, p = 0.64). Likewise, a similar pattern of results was revealed in the non- clinical network (Fig. 1b) across positive affect (M = 0.16) and negative affect (M = 0.10) (z = −0.91, p = 0.36).
Comparisons of the overall clinical (M = 0.06) and non-clinical (M = 0.13) dynamic networks revealed no significant differences in out-strength (z = −1.57, p = 0.11). For comparisons with only positive affect nodes, no significant differences in centrality were found between clinical (M = 0.05) and non-clinical networks (M = 0.16) (z = −1.46, p = 0.14). A similar pattern of results emerged for the negative affect nodes across the clinical (M = 0.07) and non-clinical networks (M = 0.10) (z = −0.57, p = 0.56).
3.3. Dynamic network structure of PA, NA, and actigraphy-derived daily activity
The inclusion of actigraphy-derived daily activity as a node yielded differential dynamic network structures between the clinical group and non-clinical group. Specifically, modeling activity levels resulted in the formation of an isolated community of nodes in the clinical group (Fig. 2a). In one community, physical activity formed a positive feed-back pathway with the positive affect node ‘active’ (actigraphy-based daily activity levels → ‘active’ β = 0.08, p < 0.01; ‘active’→ actigraphy-based daily activity levels β = 0.14, p < 0.01). Higher levels of ‘ashamed’ prospectively predicted lower levels of physical activity in the clinical group (β = −0.06, p < 0.05). In the larger community of nodes, the directed edges across individual nodes of positive and negative affect were positive in direction, similar to Fig. 1a.
Fig. 2. Dynamic network structure of PA, NA, and physical activity.
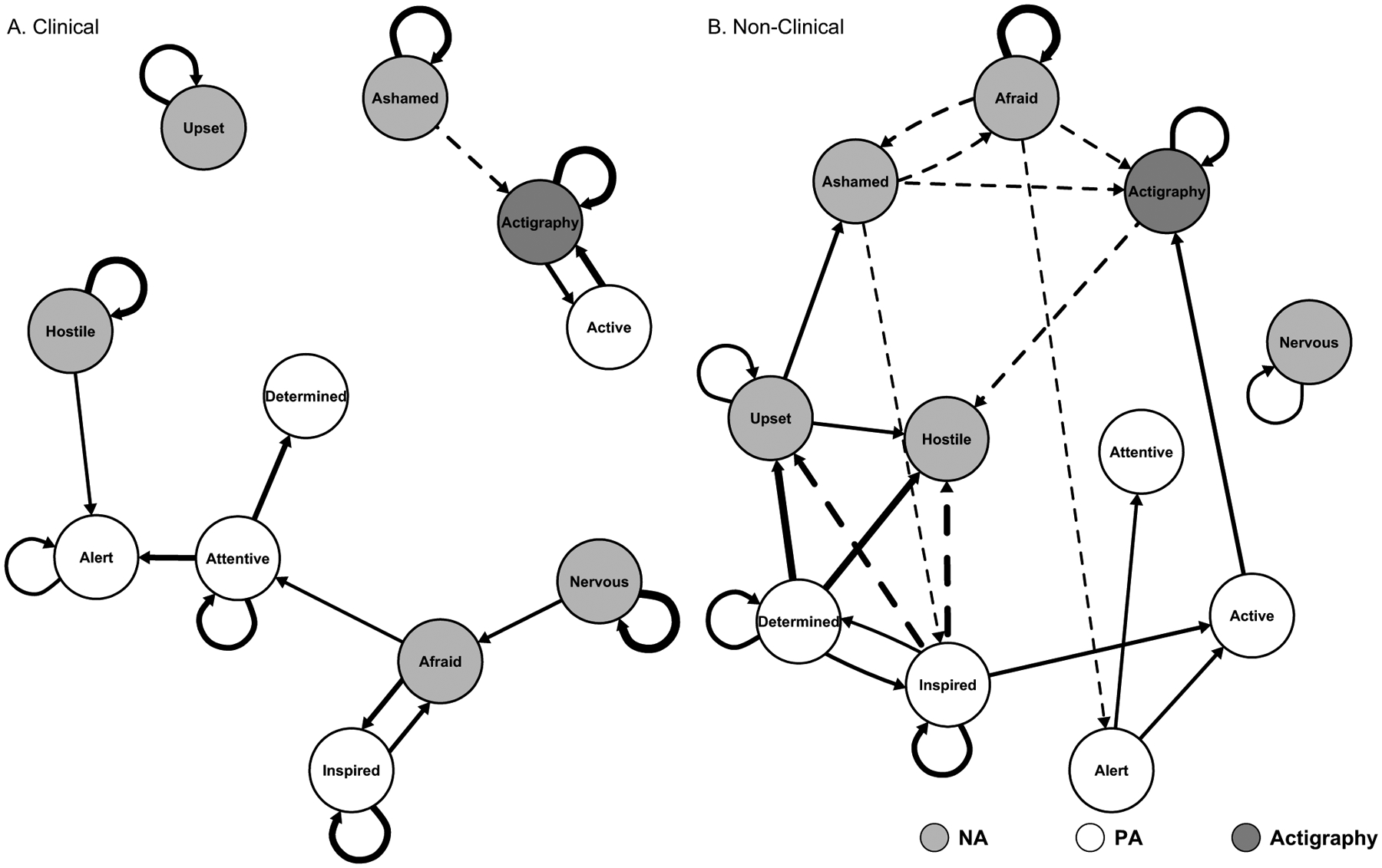
Note: In Fig. 2A, higher levels of being ‘ashamed’ prospectively predicted less physical activity, whereas ‘active’ predicted more physical activity. As revealed in Fig. 2B, physical activity is connected to a more diverse set of positive and negative affect nodes in non-clinical individuals. Thickness of arrow reflects strength of association. Solid arrows denote positive associations, whereas dashed arrows denote negative associations.
Among the individuals in the non-clinical group, activity levels were prospectively predicted by the negative affect nodes ‘ashamed’ (β = −0.05, p < 0.01) and ‘afraid’ (β = −0.05, p < 0.01) (Fig. 2b). Moreover, higher levels of the positive affect node ‘active’ prospectively predicted greater actigraphy-based daily activity levels (β = 0.08, p < 0.01). Akin to Fig. 1b, the within-valence directed edges were primarily positive, whereas the between-valence directed edges were largely negative.
3.4. Indices of critical slowing down
Several multilevel models were pursued to determine whether critical slowing down in positive affect, negative affect, or actigraphy-based daily activity levels predicted significant changes in depression symptoms in the clinical group. Results revealed significant interaction effects between the autocorrelation coefficient and depression change for two affect variables: ‘alert’ (β = −0.01, p < 0.05) and ‘inspired’ (β = −0.01, p < 0.05) (Table 1). As demonstrated in Supplementary Fig. 3, worsening of depression was associated with larger autocorrelation coefficients for these two affect variables. That is, critical slowing down in temporal dynamics of ‘alert’ and ‘inspired’ is predictive of greater transitions in depression symptoms over time.
Table 1.
Autoregression multilevel models.
| Parameter PA fixed effects | Active Estimate | SE | Alert Estimate | SE | Inspired Estimate | SE | Determined Estimate | SE | Attentive Estimate | SE |
|---|---|---|---|---|---|---|---|---|---|---|
| Intercept (γ00) | 2.35*** | 0.13 | 2.59*** | 0.15 | 2.28*** | 0.17 | 2.78*** | 0.18 | 2.69*** | 0.16 |
| Affect t − 1 (γ10) | 0.08* | 0.03 | 0.11** | 0.03 | 0.16*** | 0.03 | 0.12** | 0.03 | 0.13*** | 0.03 |
| Depression Δ (γ01) | −0.01 | 0.02 | 0.01 | 0.02 | −0.05 | 0.03 | −0.02 | 0.03 | 0.002 | 0.03 |
| Affect t − 1 × Depression Δ (γ11) | −0.003 | 0.01 | −0.01* | 0.01 | −0.01* | 0.005 | 0.003 | 0.006 | −0.01 | 0.01 |
| NA Fixed Effects | Ashamed Estimate | SE | Upset Estimate | SE | Hostile Estimate | SE | Nervous Estimate | SE | Afraid Estimate | SE |
| Intercept (γ00) | 1.29*** | 0.07 | 1.65*** | 0.09 | 1.34*** | 0.07 | 1.54*** | 0.11 | 1.32*** | 0.09 |
| Affect t − 1 (γ10) | 0.15 | 0.05 | 0.15*** | 0.03 | 0.12** | 0.04 | 0.14*** | 0.03 | 0.10 | 0.05 |
| Depression Δ (γ01) | −0.005 | 0.01 | −0.03 | 0.02 | 0.01 | 0.01 | −0.03 | 0.02 | −0.03 | 0.02 |
| Affect t − 1 × Depression Δ (γ11) | 0.006 | 0.01 | −0.001 | 0.01 | −0.009 | 0.01 | −0.01 | 0.01 | −0.01 | 0.01 |
| Act. Fixed Effects | Actigraphy Estimate | SE | ||||||||
| Intercept (γ00) | −32.57*** | 3.69 | ||||||||
| Act. t − 1 (γ10) | 0.15** | 0.05 | ||||||||
| Depression Δ (γ01) | −0.64 | 0.67 | ||||||||
| Act. t − 11 × Depression Δ (γ11) | −0.002 | 0.01 |
Note. SE = standard error; Δ = change; PA= positive affect; NA = negative affect; Act = actigraphy. Random effect components are omitted for ease of presentation.
p < 0.05;
p < 0.01;
p < 0.001.
4. Discussion
Collectively, the results provide evidence that individuals with bipolar disorder can be distinguished from healthy controls based on differences in their dynamic network structure of positive and negative affect. Specifically, these results reveal that directed edges between nodes of opposite affect valence are largely positive in direction among individuals with bipolar disorder, whereas they are more varied in direction among healthy controls. This suggests that for individuals in the bipolar disorder group, once one affective state is activated it is more likely that any other affective state will be activated irrespective of valence. This finding comports with prior research that suggests that impoverished emotion differentiation (i.e., the ability to distinguish between various discrete positive and negative emotions) is related to poorer mental health and emotion regulation deficits (Barrett et al., 2001).
Furthermore, these results have important implications when considered in light of contemporary theories of affect by potentially reconciling discrepancies between models. The traditional CM posits that the simultaneous activation of positive and negative affect is prohibited, as individual positive and negative affective states occupy opposing positions on the valence-activation circumplex grid. For example, an affective state characterized by moderate activation and moderate positive valence, such as elation, would be diametrically opposite to an affective state characterized by moderate inactivation and moderate negative valence, such as depression. Revised versions of the CM posit that this bipolarity of affective experience occurs not only at a single time point, but also across short time-frames (e.g., a period of a day) (Remington et al., 2000). Thus, affective states of opposite valence would interact in a co-inhibitory fashion according to the CM. In contrast, the ESM permits multiple forms of affective activation, including co-activation and co-inhibition, but it does not specify the exact conditions under which they are likely to occur.
The results of the current study substantiate that both co-activation and co-inhibition are possible for opposite-valenced affective states; however, these activation patterns are differentially associated with clinical outcomes. The tenets of the CM may hold for individuals without a psychiatric condition, as their dynamic networks revealed a co-inhibitory relationship between affective states of opposite-valence. The CM does not, however, adequately account for affect dynamics of individuals with bipolar disorder. The presence of co-activation across positive and negative affect in the clinical dynamic networks provides support for ESM, which is more permissive. Thus, this study offers important context to account for the existence of both co-inhibition and co-activation of opposite-valenced affect states. These findings are corroborated by prior research, suggesting that experiences of simultaneous positive and negative affect in response to complex emotional situations may have deleterious health consequences (Larsen et al., 2001). Thus, these results provide important evidence attesting to the empirical possibility of two theoretically distinct activation patterns (i.e., co-inhibition and co-activation) and specifies one potential condition under which co-activation emerges (i.e., the presence of bipolar disorder).
Beyond the broader level of affect valence, the dynamic characteristics of individual states of positive and negative affect were also of clinical importance. Specifically, critical slowing down in ‘alert’ and ‘inspired’ were associated with changes in depression symptoms. That is, these results indicate that as the levels of certain nodes become progressively more similar across time, the more likely it is that an individual with bipolar disorder will experience an increase in depression symptoms. Identifying indicators of critical slowing down can provide crucial insight into the dynamic processes that contribute to maintenance and pathogenesis of affective disorders. The clinical significance of critical slowing down is consistent with research identifying emotional inertia as a predictor of worsening depression (Houben et al., 2015; Wichers et al., 2016). Furthermore, prior research has suggested that dynamic network characteristics of depression may provide insight into the high relapse rates that occur subsequent to treatment (Snippe et al., 2017).
It is important to acknowledge certain limitations of this study that bear on interpretation of the results. First, although the current study used an intensive longitudinal design to address questions about the dynamics of affect and physical activity, it should be noted that ratings of affect were collected once per day across the study period. To further our knowledge of momentary experiences of affect, it would be beneficial to examine the network dynamics of affect in clinical samples using affect ratings that are collected numerous times each day. Second, participants in the bipolar group were required to maintain inter-episode status throughout the study period. Our focus on the inter-episode period by definition precluded examination of predictors of episode relapse. Although the inter-episode period allows for identification of factors that sustain impairment outside of acute episodes and maintain vulnerability, it will be important for the present results to be replicated with participants who have more variable symptom profiles to identify indicators of critical slowing down that lead to relapse. Third, the current study did not collect data on neurocognitive deficits or social cognition domains such as theory of mind or social perception. Future research may benefit from examining how the dynamics of affect valence interact with social cognition. Fourth, prior research has suggested the possibility of gender differences in negative affect (Fujita et al., 1991). The sample size of the current study is not large enough to further divide the bipolar and healthy control participants into each gender category to examine between group network differences. However, future research on affect dynamics should consider the role of gender.
Fifth, the temporal networks assume stationarity, which requires that the properties of the network are constant over time. Because stationarity may not always apply to dynamic properties of psychological constructs, it will be beneficial to develop time-varying multilevel network models that may better account for time trends. Finally, there has been some discussion about the utility of estimating temporal autocorrelation to identify critical slowing down in multilevel models, with some critiques contending that such an approach conflates between-subject and within-subject variability (Bos and De Jonge, 2014). In response to this critique, Wichers and colleagues (2014) asserted that person-mean centering unambiguously disaggregates between-subject and within-subject effects, and they argued that the group-based approach of using multilevel models to investigate critical slowing down is still consistent with the principles of dynamic systems. That not-withstanding, it would still be advantageous for future research to examine concepts such as critical slowing down in a more intra-individual approach whereby increased autocorrelation in a single person could predict changes in disorder state.
Despite these limitations, an important implication of this work is that differential dynamic network properties can distinguish clinical and non-clinical participants through distinct activation patterns of affect and physical activity (i.e., co-activation and co-inhibition). Because affective disorders such as bipolar disorder are heterogeneous in terms of presentation and etiology (Kessler et al., 2005), it is necessary to adopt a precision medicine approach to ascertain which individual differences confer risk for increases in disorder severity. The dynamic systems approach represents a potential framework that permits the identification of individual differences in the temporal course of affect (Kuppens et al., 2010). In the current study, we elucidated general dynamic markers of affective health and pathology in relation to positive and negative affect (i.e., lack of between valence co-inhibition and critical slowing down). The dynamic network approach can be extended to examine idiosyncratic features of a single person’s affect over time to predict clinically significant changes in emotional health. As intensive longitudinal designs (e.g., ecological momentary assessment) become more readily implementable with available smartphone technology, it will be possible to develop tools that monitor affect over time to identify dynamic network signatures of emotional health and pathology.
Supplementary Material
Funding
This research was supported by the National Institute of Mental Health (NIMH) Research Scientist Development Award K01MH100433 and an NIMH Ruth L. Kirschstein National Research Service Award Postdoctoral Fellowship F32MH76339 to Dr. Anda Gershon. Dr. Stefan G. Hofmann receives support from National Institutes of Health/ National Center for Complementary and Integrative Health, National Institutes of Health/National Institute of Mental Health, the James S. McDonnell Foundation 21st Century Science Initiative in Understanding Human Cognition-Special Initiative, and the Department of the Army for work unrelated to the studies reported in this article. He receives compensation for his work as an advisor from the Palo Alto Health Sciences and Otsuka Digital Health, Inc., and for his work as a subject matter expert from John Wiley & Sons, Inc., and SilverCloud Health, Inc. He also receives royalties and payments for his editorial work from various publishers.
Footnotes
Competing interests
None of the authors declare any conflicts of interest with respect to the authorship or publication of this article.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2019.02.017.
References
- APA, 2000. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR). American Psychiatric Press, Washington, DC. [Google Scholar]
- Barlow DH, Allen LB, Choate ML, 2004. Toward a unified treatment for emotional disorders. Behav. Ther 35, 205–230. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Gross J, Christensen TC, Benvenuto M, 2001. Knowing what you’re feeling and knowing what to do about it: mapping the relation between emotion differentiation and emotion regulation. Cognit. Emot 15, 713–724. [Google Scholar]
- Beck AT, 2008. The evolution of the cognitive model of depression and its neurobiological correlates. Am. J. Psychiatry 165, 969–977. [DOI] [PubMed] [Google Scholar]
- Bodner N, Kuppens P, Allen NB, Sheeber LB, Ceulemans E, 2018. Affective family interactions and their associations with adolescent depression: a dynamic network approach. Dev. Psychopathol 30, 1459–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO, 2013. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Bos EH, De Jonge P, 2014. “Critical slowing down in depression” is a great idea that still needs empirical proof. Proc. Natl. Acad. Sc 111, E878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Lemmens LHJM, Huibers MJH, Borsboom D, Tuerlinckx F, 2015. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol. Med 45, 747–757. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, Tuerlinckx F, 2013. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One 8, e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH, 1998. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J. Abnorm. Psychol 107, 179–192. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Gardner WL, Berntson GG, 1999. The affect system has parallel and integrative processing components. J. Pers. Soc. Psychol 76, 839–855. [Google Scholar]
- Curran PJ, Bauer DJ, 2011. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu. Rev. Clin 62, 583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtiss J, Klemanski DH, 2016. Taxonicity and network structure of generalized anxiety disorder and major depressive disorder: an admixture analysis and complex network analysis. J. Affect. Disord 199, 99–105. [DOI] [PubMed] [Google Scholar]
- Curtiss J, Ito M, Takebayashi Y, Hofmann SG, 2018. Longitudinal network stability of the functional impairment of anxiety and depression. Clin. Psychol. Sci 6, 325–334. [Google Scholar]
- Epskamp S, Waldorp LJ, Mõttus R, Borsboom D, 2016. Discovering psychological dynamics: the Gaussian graphical model in cross-sectional and time-series data. arXiv preprint arXiv:1609.04156. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient ed. Biometrics Research, New York. [Google Scholar]
- Fisher AJ, 2015. Toward a dynamic model of psychological assessment: implications for personalized care. J. Consult. Clin. Psychol 83, 825–836. [DOI] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D, 2016. What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord 189, 314–320. [DOI] [PubMed] [Google Scholar]
- Fujita F, Diener E, Sandvik E, 1991. Gender differences in negative affect and well-being: the case for emotional intensity. J. Personal. Soc. Psychol 61, 427–434. [DOI] [PubMed] [Google Scholar]
- Gershon A, Ram N, Johnson SL, Harvey AG, Zeitzer J, 2016. Daily actigraphy profiles distinguish depressive and well periods in bipolar disorder. Clin. Psychol. Sci 4, 641–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon A, Thompson WK, Eidelman P, McGlinchey EL, Kaplan KA, Harvey A.G.m, 2012. Restless pillow, ruffled mind: sleep and affect coupling in inter-episode bipolar disorder. J. Abnorm. Psychol 121, 863–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granger CW, 1969. Investigating causal relations by econometric models and cross-spectral methods. Econometrica 37, 424–438. [Google Scholar]
- Gruber J, 2011. Can feeling too good be bad? Positive emotion persistence (PEP) in bipolar disorder. Curr. Dir. Psychol. Sci 20, 217–221. [Google Scholar]
- Gsell AS, Scharfenberger U, Özkundakci D, Walters A, Hansson LA, Janssen AB, Dakos V, 2016. Evaluating early-warning indicators of critical transitions in natural aquatic ecosystems. Proc. Natl. Acad. Sci 113, E8089–E8095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havermans R, Nicolson NA, Berkhof J, 2010. Mood reactivity to daily events in patients with remitted bipolar disorder. Psychiatry Res. 179, 47–52. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J, McNally RJ, 2016. A complex network perspective on clinical science. Perspect. Psychol. Sci 11, 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A, 2012. Emotion dysregulation model of mood and anxiety disorders. Depress. Anxiety 29, 409–416. [DOI] [PubMed] [Google Scholar]
- Houben M, Van Den Noortgate W, Kuppens P, 2015. The relation between short-term emotion dynamics and psychological well-being: a meta-analysis. Psychol. Bull 141, 901–930. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Fulford D, 2009. Preventing mania: a preliminary examination of the GOALS program. Behav. Ther 40, 103–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE, 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Koval P, Madeline LP, Meers K, Kuppens P, 2013. Affect dynamics in relation to depressive symptoms: variable, unstable or inert? Emotion 13, 1132–1141. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP, 2001. Multilevel modeling of individual and group level mediated effects. Multivariate Behav. Res 36, 249–277. [DOI] [PubMed] [Google Scholar]
- Kuppens P, Oravecz Z, Tuerlinckx F, 2010. Feelings change: accounting for individual differences in the temporal dynamics of affect. J. Pers. Soc. Psychol 99 (6), 1042–1060. [DOI] [PubMed] [Google Scholar]
- Larsen JT, Mcgraw AP, Cacioppo JT, 2001. Can people feel happy and sad at the same time? J. Pers. Soc. Psychol 81, 684–696. [PubMed] [Google Scholar]
- Lerner JS, Keltner D, 2000. Beyond valence: toward a model of emotion-specific influences on judgement and choice. Cognit. Emot 14, 473–493. [Google Scholar]
- Mauss IB, Robinson MD, 2009. Measures of emotion: a review. Cognit. Emot 23, 209–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel C, Klaus A, Kuehn C, Plenz D, 2015. Critical slowing down governs the transition to neuron spiking. PLoS Comput. Biol 11, e1004097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson B, McGorry PD, Wichers M, Wigman JT, Hartmann JA, 2017. Moving from static to dynamic models of the onset of mental disorder: a review. JAMA Psychiatry 74, 528–534. [DOI] [PubMed] [Google Scholar]
- Ramsay JO, Hooker G, Graves S, 2009. Functional Data Analysis with R and Matlab. Springer, New York. [Google Scholar]
- Remington NA, Fabrigar LR, Visser PS, 2000. Reexamining the circumplex model of affect. J. Pers. Soc. Psychol 79, 286–300. [DOI] [PubMed] [Google Scholar]
- Rikkert MGO, Dakos V, Buchman TG, de Boer R, Glass L, Cramer AO, Tolner EA, 2016. Slowing down of recovery as generic risk marker for acute severity transitions in chronic diseases. Crit. Care Med 44, 601–606. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH, 1996. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol. Med 26, 477–486. [DOI] [PubMed] [Google Scholar]
- Russell JA, 1980. A circumplex model of affect. J. Pers. Soc. Psychol 39, 1161–1178. [Google Scholar]
- Sadeh A, Hauri PJ, Kripke DF, Lavie P, 1995. The role of actigraphy in the evaluation of sleep disorders. Sleep 18, 288–302. [DOI] [PubMed] [Google Scholar]
- Scherer KR, 2005. What are emotions? And how can they be measured? Soc. Sci. Inf 44, 695–729. [Google Scholar]
- Snippe E, Viechtbauer W, Geschwind N, Klippel A, de Jonge P, Wichers M, 2017. The impact of treatments for depression on the dynamic network structure of mental states. Sci. Rep 7, 46523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavrakakis N, Booij SH, Roest AM, de Jonge P, Oldehinkel AJ, Bos EH, 2015. Temporal dynamics of physical activity and affect in depressed and nondepressed individuals. J. Health Psychol 34, 1268–1277. [DOI] [PubMed] [Google Scholar]
- Thompson ER, 2007. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). J. Cross Cult. Psychol 38, 227–242. [Google Scholar]
- van de Leemput IA, Wichers M, Cramer AO, Borsboom D, Tuerlinckx F, Kuppens P, Derom C, 2014. Critical slowing down as early warning for the onset and termination of depression. Proc. Natl. Acad. Sci 111, 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M, Borsboom D, Tuerlinckx F, Kuppens P, Viechtbauer W, van de Leemput IA, …, Scheffer M, 2014. Reply to Bos and De Jonge: Between-subject data do provide first empirical support for critical slowing down in depression. Proc. Natl. Acad. Sc 111, E879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M, Groot PC, Psychosystems ESM., EWS Group., 2016. Critical slowing down as a personalized early warning signal for depression. Psychother. Psychosom 85, 114–116. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA, 1978. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


