Abstract
Study Objective
To present a series of robotic laparoendoscopic single-site surgery (LESS) and reduced-port hysterectomy cases and discuss the surgical technique required for successful use on this new platform.
Design
Retrospective case series.
Setting
Academic medical center.
Patients
All patients undergoing robotic LESS or reduced-port hysterectomy with the SP1098 da Vinci SP Surgical System (Intuitive Surgical, Sunnyvale, CA) from December 2019 to March 2020.
Interventions
Robotic LESS or reduced-port hysterectomy.
Measurements and Main Results
A total of 8 cases of hysterectomy were performed successfully. Four cases included concomitant resection of endometriosis. Five cases required placement of an additional port. The average uterine weight was 136.1 g ± 61.5 g (range 87–246). The average estimated blood loss was 37.5 mL ± 27 mL (range 20–100). The average operative time was 86.5 minutes ± 27.1 minutes (range 60–132). The time required for vaginal cuff closure was available for patients 5 to 8, and ranged from 10 minutes to 13 minutes. All patients had same-day discharge. There were no conversions to alternative surgical modality, complications, or readmissions.
Conclusion
Our preliminary experience with the SP1098 da Vinci SP Surgical System demonstrated the technical feasibility and safety of this surgical modality for gynecologic surgery. Additional studies examining postoperative outcomes and prospective studies comparing this modality with traditional robotic surgery are indicated.
Keywords: Single-incision surgery, R-LESS, Single site
Minimally invasive surgery has been shown to have significant benefits for patients in gynecology [1]. Multiple studies show that endoscopic approaches to gynecologic procedures have comparable or improved outcomes when compared with laparotomic approaches. Multiport approaches to laparoscopy and robotic surgery are currently most common in the United States. Laparoendoscopic single-site surgery (LESS) has emerged as a potentially less invasive alternative to multiport laparoscopy. LESS refers to a spectrum of surgical techniques that allow the performance of laparoscopic surgery through consolidation of all ports into 1 surgical incision [2]. LESS has been shown to be comparable to traditional laparoscopy in terms of efficacy and safety in gynecologic surgery [3], although the approach does require alteration in surgical technique and may be more challenging to adopt.
In the last decade, as robotics became more popular in gynecologic surgery, single-site robotic platforms were developed. Multiple studies show that robotic LESS is a safe and effective platform, comparable to traditional robotics with respect to operative time, complications, and postoperative pain [4,5]. However, this surgical modality also has challenges, including reduced extracorporeal triangulation and a limited array of nonarticulating instruments. Significant alteration in surgical technique is required for successful use of the system [6].
The SP1098 da Vinci SP Surgical System (Intuitive Surgical, Sunnyvale, CA) is a newer robotic system, with articulating instruments and camera that allow for intracorporeal triangulation, which may circumvent some of the weaknesses of previous single-site robotic systems. It was approved for urologic procedures and transoral otolaryngology by the Food and Drug Administration (FDA) in March 2019 [7]. However, it is not currently FDA-approved for gynecologic surgery. Thus far, 1 Korean group has published their experience with gynecologic surgery with this platform [8]. They found that the use of the da Vinci SP1098 platform was feasible for a variety of gynecologic surgeries, including hysterectomy, myomectomy, and sacrocolpopexy without conversion to alternative surgical modality. The objective of this case series is to present our surgical technique and discuss the feasibility of performing robotic LESS hysterectomy using the SP1098 da Vinci SP Surgical System.
Materials and Methods
From December 2019 to March 2020, 8 patients underwent robotic LESS or reduced-port hysterectomy at Mayo Clinic Arizona in Phoenix, AZ. All patients were counseled that the SP1098 da Vinci SP Surgical System is not FDA-approved for gynecologic surgery. In addition to the standard discussion of surgical risks, the patients were counseled that off-label use of the da Vinci SP1098 may incur additional risks such as intraoperative conversion to multiport robotics or laparotomy. All patients were offered performance of their surgery through a standard multiport robotic approach. Furthermore, all patients were aware that their surgeon had minimal direct experience with the da Vinci SP1098 platform.
All patient records were reviewed to identify demographics and preoperative comorbidities. The primary outcomes reported included operative time (defined as the time between incision start and closure) and perioperative outcomes, including emergency room visits and readmissions. Data collection also included estimated blood loss, conversion to multiport robotic surgery or laparotomy, pathology, uterine weight, length of hospital stay, and perioperative complications. The time required to complete vaginal cuff closure was also noted if the procedure was recorded. This retrospective case series was deemed exempt by the Mayo Clinic Arizona Institutional Review Board (approval number: 20-000440).
Single-Port System
The SP1098 da Vinci SP Surgical System consists of the surgeon console, vision cart, and patient cart, which are the same as in the previous da Vinci surgical platforms. A single instrument arm is attached to the patient cart. This contains 4 instrument drives that control the articulating camera and up to 3 robotic instruments, which are inserted into the abdomen through a 25-mm SP multichannel port. The surgeon can control up to 3 6-mm fully wristed, elbowed instruments that have between 20 and 25 lives. The instruments most likely to be used in gynecologic surgery include the monopolar curved scissors, Maryland bipolar forceps, fenestrated bipolar forceps, needle driver, Cadiere forceps, and monopolar scissors. The elbow joints allow the surgeon to maintain intracorporeal triangulation. The 10-mm oval EndoWrist SP camera has a 73° field of view and has 12 lives. The camera can be moved in a traditional fashion, or the cobra mode can be used. When the cobra function is used, the camera retracts and moves above or below the instruments, which can help prevent instrument collision and optimize visualization. An instrument guidance system displays the locations of the camera and instruments within the operative field.
Surgeons
The cases were performed by 2 surgeons. The participating physicians (a urogynecologic surgeon and a gynecologic oncology surgeon) had extensive standard multiport robotic experience, minimal robotic LESS experience (<10 cases), and were naive to the da Vinci SP1098 single-port platform. Minimally invasive gynecologic surgery fellows assisted the surgeons at the bedside in all cases.
Surgical Technique
The patients underwent surgery through a single 2.5-cm vertical umbilical incision (as measured by a sterile ruler) performed through an open Hasson approach. The fascia was tagged with an interrupted 0-Vicryl suture (Ethicon, Somerville, NJ) on each side of the incision to provide upward countertraction on the incision. The single-port trocar was placed directly through the incision. The CO2 tubing was attached to the insufflation adapter, and the abdomen was insufflated to 15 mmHg. The patient was placed in a steep Trendelenburg position, and the single-port robot was subsequently docked on the patient's left side (Fig. 1 ). The fenestrated bipolar grasper was placed in the first aperture of the trocar and the monopolar scissors in the third aperture (Fig. 2 ). Two robotic instruments were found to be sufficient. Hysterectomy was performed through the standard surgical procedure (see Supplemental Video). In 5 of the 8 cases, an additional assistant port was placed in the left lower quadrant to assist with traction and suction/irrigation as needed. Vaginal cuff closure was performed with unidirectional barbed suture in 1 layer. Universal cystoscopy was performed. After completion of the surgery, the fascial defect was closed with a delayed absorbable suture in a running fashion. The skin was closed with an absorbable suture in a subcuticular fashion.
Fig. 1.
Robot arm docked to SP cannula without instruments.
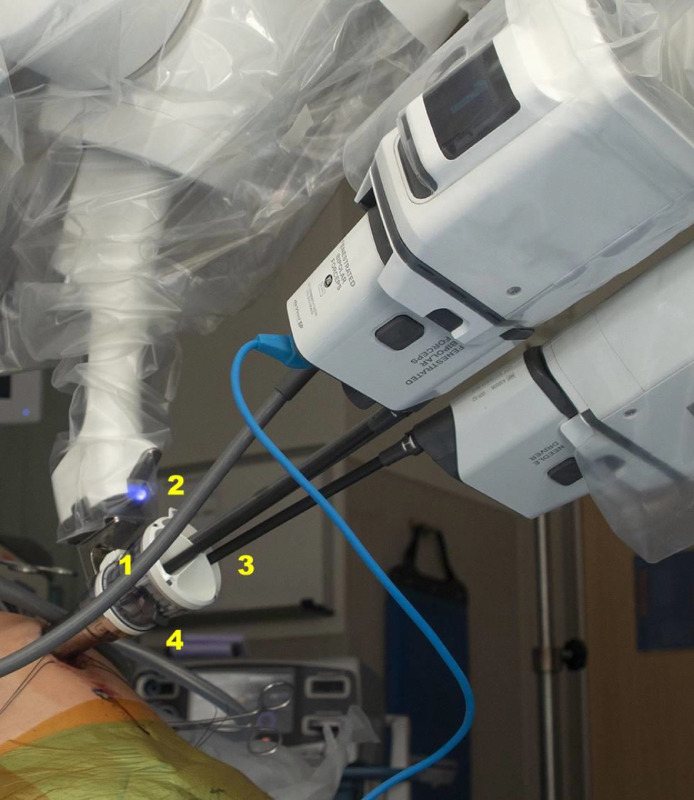
Fig. 2.
Instruments and camera docked through SP cannula. (1) The fenestrated bipolar. (2) Camera. (3) Monopolar scissors. (4) The fourth aperture is empty and can be used in a limited fashion by the bedside assistant.
Results
A total of 8 cases with a mean age of 46.3 years ± 13.6 years and body mass index of 27.8 kg/m2 ± 7.5 kg/m2 (range 22.2–40) were included (Table 1 ). With respect to comorbidities, none of the patients in this series was a smoker or had a diagnosis of diabetes. One patient had a diagnosis of asthma. The indication for surgery for all cases was benign, and included abnormal uterine bleeding (n = 5, 62.5%), postmenopausal bleeding (n = 2, 25%), and risk reduction (n = 1, 12.5%). Five of the women had a history of abdominal surgery, including cesarean section, ablation of endometriosis, salpingectomy for sterilization and ectopic pregnancy, and uterine artery embolization for fibroids. The patients’ clinical characteristics are summarized in Table 1. The operative characteristics are displayed in Table 2 . Seven cases were robot-assisted total laparoscopic hysterectomy. Four cases included concomitant resection of endometriosis. Owing to the presence of endometriosis and adhesions, 1 case was performed as a robot-assisted modified radical hysterectomy, with resection of parametrium and mobilization of the ureters. A 5-mm assist port was placed in the first 5 cases, which included the 4 cases with concomitant resection of endometriosis. The average uterine weight was 136.1 g ± 61.5 g (range 87–246). The average estimated blood loss was 37.5 mL ± 27 mL (range: 20–100). The average operative time was 86.5 minutes ± 27.1 minutes (range 60–132). The time required for vaginal cuff closure was recorded for patients 5 to 8, and ranged from 10 minutes to 13 minutes.
Table 1.
Clinical characteristics
| Patient | Age, yr | BMI (kg/m2) | Number of prior abdominal surgeries | Indication | Pathology |
|---|---|---|---|---|---|
| 1 | 33 | 37.7 | 1 | AUB | Leiomyoma |
| 2 | 38 | 40.4 | 1 | AUB | Adenomyosis + endometriosis |
| 3 | 31 | 30.9 | 3 | AUB | Adenomyosis |
| 4 | 47 | 24.5 | 0 | AUB | Adenomyosis + endometriosis |
| 5 | 38 | 22.5 | 0 | AUB | Leiomyoma + endometriosis |
| 6 | 67 | 22.2 | 2 | PMB | Benign |
| 7 | 56 | 22.4 | 0 | PMB | Grade 1 endometrioid adenocarcinoma |
| 8 | 61 | 22.2 | 1 | Risk reduction | Leiomyoma + paratubal cysts |
AUB = abnormal uterine bleeding; BMI = body mass index; PMB = postmenopausal bleeding.
Table 2.
Operative characteristics
| Patient | Procedures performed | Estimated blood loss (mL) | Operative time (min) | Cuff closure time (min) | Uterine weight (g) |
|---|---|---|---|---|---|
| 1 | TH + BS* | 25 | 102 | NR | 101 |
| 2 | MRH + BS + E* | 50 | 116 | NR | 213 |
| 3 | TH + BS + E* | 20 | 68 | NR | 108 |
| 4 | TH + BSO + E* | 25 | 80 | NR | 246 |
| 5 | TH + BS + E*† | 100 | 132 | 10 | 143 |
| 6 | TH + BS | 30 | 60 | 13 | 95 |
| 7 | TH + BS | 30 | 75 | 12 | 87 |
| 8 | TH + BSO | 20 | 59 | 12 | 88 |
BS = bilateral salpingectomy; BSO = bilateral salpingo-oophorectomy; E = resection of endometriosis; MRH = modified radical hysterectomy; NR = not recorded; TH = total hysterectomy.
5-mm assist port placed.
Uterine manipulator used.
All patients had same-day discharge. Six patients experienced a completely benign postoperative course. One patient developed upper abdominal pain, and a computed tomography scan of the abdomen and pelvis was obtained for workup. This revealed moderate inflammatory changes within the pelvis with thickened loops of ileum. The patient was managed expectantly, and her symptoms resolved; her upper abdominal pain was felt to be unrelated to surgery. Another patient reported vaginal bleeding in postoperative week 3, which did not require any intervention. At her subsequent 6-week postoperative examination, she was found to have granulation tissue of the vaginal cuff, which was cauterized with silver nitrate.
There were no emergency room visits during the 6-week postoperative period and no readmissions. Six patients had an in-person 6-week postoperative evaluation. There were no clinical or physical examination findings suggestive of hernia or concern for delayed wound healing at the umbilicus. Because all nonurgent in-person care was deferred during coronavirus disease social distancing protocols, the last 2 patients included in this series had video postoperative visits. They reported no concerns.
Discussion
Interest in single-incision laparoendoscopic surgery continues to grow. Previously established robotic LESS platforms faced several obstacles to widespread adoption because of technical challenges. The newer single-port systems enjoy several advantages, including increased dexterity and range of motion, camera mobility, and intracorporeal instrument triangulation. The additional benefits of robotic LESS can be preserved, including a single scar with improved cosmesis and the potential for decreased pain.
Our preliminary experience with the SP1098 da Vinci SP Surgical System demonstrated the technical feasibility of this surgical modality for gynecologic surgery. The mean operative time of 86.5 minutes and low estimated blood loss are consistent with our practice experience with standard multiport robotic hysterectomy. Vaginal cuff closure times ranged from 10 minutes to 13 minutes, which is also consistent with the times achieved on a multiport robotics platform. These results suggest that standard robotic skills are highly transferrable to the robotic single-port platform. However, at this point, little can be concluded about the surgeon learning curve with this platform. Although operative times did decrease between case 1 and case 8, the surgeries performed were heterogeneous and difficult to compare directly. Further information regarding the surgeon learning curve will be collected as our institution's experience with this surgical platform progresses.
Hysterectomy with the single-port platform seems to be safe as well. None of the patients experienced a conversion to alternative surgical modality, surgical complication, or required readmission. Only 1 patient required an unscheduled office visit for evaluation of vaginal bleeding, but no intervention or treatment was indicated.
Despite several advantages of the da Vinci SP1098 system compared with previous robotic single-site systems, some alteration to surgical technique is required. For example, obtaining traction of tissue is limited with the da Vinci SP1098. Medial traction and cephalad traction along the axis of the trocar are not restricted; however, adequate lateral or anterior traction is more challenging to obtain. Second, the bedside assistant can play a very limited role. Although a laparoscopic instrument can be inserted through the fourth aperture of the trocar if not in use, movement is restricted to the axis of the single-port trocar. Thus, the bedside assistant is best used to retrieve specimens and operate a suction irrigator. In the first 5 of the 8 cases, an additional 5-mm port was placed in the left lower quadrant. Of note, 4 of these 5 cases included resection of endometriosis. The 5-mm assist port was placed owing to difficulty obtaining adequate tissue traction during ureterolysis. Our practice does not routinely use an intrauterine manipulator with standard multiport robotics. However, an intrauterine manipulator with a colpotomy cup was used in 1 case and was very helpful with anteversion, lateral traction, and colpotomy. It is likely that the routine use of a uterine manipulator may eliminate the need for an additional assistant port for traction purposes. Another option, as described by Shin et al [8], is to use a GelPass One-port System (Meden, Seoul, South Korea) or a similar product at the umbilicus. The SP cannula as well as an additional assistant trocar can be inserted through the GelSeal cap (Applied Medical, Rancho Santa Margarita, CA). The use of this method likely allows for additional intraoperative flexibility, but also adds to the total surgical cost. In future cases, optimal surgical technique at our institution will continue to be refined.
This case series included a small number of cases; however, the characteristics of the patients and types of procedures performed are reflective of high-volume gynecology practices. The body mass index of the patients included ranged from normal to class II obese. Of the 8 patients, 5 had a history of previous abdominal procedures. Of note, the previously published case series reported an average patient length of stay of 4.6 days [8]. This difference may be due to different institutional discharge criteria; however, our case series supports the feasibility of same-day discharge for patients undergoing surgery with the robotic single-port modality.
In conclusion, hysterectomy with the SP1098 da Vinci SP Surgical System is technically feasible for the well-selected patient, with minimal alteration in technique. In addition, the da Vinci SP1098 robotic platform seems to be safe for gynecologic surgery. Additional studies examining postoperative outcomes and prospective studies comparing this modality to traditional robotic surgery are indicated.
Footnotes
The authors declare that they have no conflict of interest.
The study design was approved as exempt by the Mayo Clinic Arizona Institutional Review Board (approval number: 20-000440).
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.jmig.2020.08.009.
Appendix. Supplementary materials
Video. Surgical technique for robotic single port surgery.
References
- 1.Nieboer TE, Johnson N, Lethaby A. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;3 doi: 10.1002/14651858.CD003677.pub4. [DOI] [PubMed] [Google Scholar]
- 2.Spana G, Rane A, Kaouk JH. Is robotics the future of laparoendoscopic single-site surgery (LESS) BJU Int. 2011;108:1018–1023. doi: 10.1111/j.1464-410X.2011.10513.x. [DOI] [PubMed] [Google Scholar]
- 3.Song T, Kim ML, Jung YW, Yoon BS, Joo WD, Seong SJ. Laparoendoscopic single-site versus conventional laparoscopic gynecologic surgery: a metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2013;209:317. doi: 10.1016/j.ajog.2013.07.004. e1–317.e9. [DOI] [PubMed] [Google Scholar]
- 4.Bogliolo S, Ferrero S, Cassani C. Single-site versus multiport robotic hysterectomy in benign gynecologic diseases: a retrospective evaluation of surgical outcomes and cost analysis. J Minim Invas Gynecol. 2016;23:603–609. doi: 10.1016/j.jmig.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Paek J, Lee JD, Kong TW, Chang SJ, Ryu HS. Robotic single-site versus laparoendoscopic single-site hysterectomy: a propensity score matching study. Surg Endosc. 2016;30:1043–1050. doi: 10.1007/s00464-015-4292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheib SA, Fader AN. Gynecologic robotic laparoendoscopic single-site surgery: prospective analysis of feasibility, safety, and technique. Am J Obstet Gynecol. 2015;212:179. doi: 10.1016/j.ajog.2014.07.057. e1–179.e8. [DOI] [PubMed] [Google Scholar]
- 7.United States Food and Drug Administration. May 31, 2018. Re: K173906 Trade/Device Name: da Vinci SP Surgical System, EndoWrist SP Instruments, and Accessories. K173906. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf17/K173906.pdf. Accessed August 31, 2020.
- 8.Shin HJ, Yoo HK, Lee JH, Lee SR, Jeong K, Moon HS. Robotic single-port surgery using the da Vinci SP® surgical system for benign gynecologic disease: a preliminary report. Taiwan J Obstet Gynecol. 2020;59:243–247. doi: 10.1016/j.tjog.2020.01.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video. Surgical technique for robotic single port surgery.