Abstract
Objective:
The Coronavirus disease (COVID-19) outbreak has evolved into a pandemic crisis, with King County in Washington State emerging as the early US epicenter. A literature review revealed few reports providing front-line clinical and research teams guidance related to multilevel, rapidly evolving COVID-19 directives.
Method:
The Rapid Assessment Procedure Informed Clinical Ethnography (RAPICE) method was used to develop a clinical case series and conduct participant observation during an ongoing comparative effectiveness trial of peer-integrated, patient-centered interventions after traumatic injury. Participants were patients enrolled in the intervention arm of the ongoing trial, as well as front-line clinicians, patient peer interventionists and clinical research team members implementing the trial. All participants were exposed to the Washington State COVID-19 outbreak.
Results:
Primary and secondary COVID-19 prevention strategies were feasibly integrated into ongoing care coordination and behavioral interventions for at-risk patients. Beyond the compilation of case studies, as an iterative method, RAPICE data collection naturalistically evolved to include observations of intervention team activity occurring within the larger pandemic epicenter context. A daily clinical research team huddle that flexibly accommodated virtual participation was also feasibly implemented.
Conclusions:
Primary and secondary COVID-19 prevention strategies can be feasibly integrated into ongoing clinical interventions during the pandemic. Routine, proactive clinical and research team communication that transparently addresses ethical tensions and health sustaining activities may promote well-being for providers grappling with rapidly evolving pandemic directives. Proactive assessments of individual provider vulnerabilities for severe COVID-19 related respiratory illness may also be a crucial element of health care system pandemic responses.
Keywords: Coronavirus, pandemic, disaster mental health, trauma care systems, preventive intervention
Introduction
The December 2019 Coronavirus disease (COVID-19) outbreak has evolved into a pandemic, with Washington State, and specifically King County, emerging as the early epicenter of the United States exposure (Coronavirus COVID-19 Global Cases, 2020). The King County outbreak has brought multiple clinical and research teams into the frontlines of the pandemic response. Historically, pandemics have had severe global consequences with physical and mental health impacts equal to other major categories of disaster related health care emergencies, such as war and natural disasters (Brooks et al., 2020; Morganstein et al., 2017). Pandemics can result in a unique constellation of psychological stressors and behavioral issues. Individuals exposed to infectious agents during pandemics may not be aware of their risk until they develop symptoms, possibly days or weeks after the exposure, making public health containment efforts challenging. While multiple United States national and organizational guidances targeting the COVID-19 pandemic response are being disseminated, literature review revealed few current US published reports describing the integration of these guidances by front-line clinical and research teams interacting with at-risk patients (2019 Novel Coronavirus (nCoV) Response Program, 2020; Coronavirus (COVID-19), 2020; COVID-19 (2019 novel coronavirus) resource center for physicians, 2020; Morganstein et al., 2017; Pandemics, 2020).
The Rapid Assessment Procedure Informed Clinical Ethnography (RAPICE) approach has been previously shown to be useful in disaster mental health settings as a method for efficiently capturing and informing front-line responder decision making, referrals and resource allocation (Zatzick et al., 2010). RAPICE methods embed participant observation within front-line clinical providers, who log field notes and jottings during routine activities and regularly present these observations to an external consultant (Palinkas & Zatzick, 2019). Additionally, RAPICE methods have been further developed in non-disaster settings, including acute care pragmatic clinical trials (Palinkas & Zatzick, 2019).
Due to the evolving nature of the COVID-19 pandemic, national and organizational guidances can change and/or become obsolete quickly. Clinical and research teams are simultaneously confronted by multilevel problems and decisions that include exposure risk/benefit appraisals at the individual patient, family, provider, collegial and societal levels. As is typical of mass disaster settings, multiple competing ethical tensions exist in the current pandemic context that may stretch the capacities of front-line providers and clinical research teams (Howe & Newman, 2017). Additionally, in the United States, integration of patient peers into clinical research teams is occurring across disease conditions and health care delivery systems (PCORI, 2017). Although potentially invaluable team members, patient peers frequently have chronic conditions that increase the risk of more severe illness if exposed to COVID-19 (Schreiber et al., 2019). The aim of the current investigation was to apply the RAPICE approach to the rapidly evolving United States pandemic epicenter context to develop case studies and to conduct participant observation with clinical research team members, in order to derive generalizable lessons learned.
Materials and Methods
Design Overview
The investigation was a secondary study that was embedded within a larger randomized comparative effectiveness trial, which was designed to assess the impact of a peer-integrated acute care to primary care and community care coordination intervention. The intervention targeted improvements in patient reported outcomes over the course of the year after injury admission (Scheuer et al., 2020). Patients eligible for the original study were required to have been admitted to the University of Washington’s Harborview Level I Trauma Center (Harborview) emergency department, trauma surgical ward or intensive care units for at least 24 hours. Patients included in the study were English and Spanish speaking, male and female physically injured trauma survivors who were ≥ 18 years of age and residents of Washington, Oregon, Alaska or California. All study procedures were approved by the University of Washington’s Institutional Review Board, and informed consent was obtained from each participant at bedside during their inpatient admission prior to the initiation of study procedures.
Recruitment for the study began at Harborview in August of 2018. All patients described in the current report were consented into the study prior to December 2, 2019 and were discharged from the hospital prior to March 1, 2020. The current report derives from patient interactions and clinical research procedures that occurred during the early period of the King County, Washington COVID-19 outbreak, between March 1, 2020 and March 16, 2020.
Patient Recruitment
The population of patients meeting the inclusion criteria above underwent an electronic health record (EHR) posttraumatic stress disorder (PTSD) risk screen. The 10 domain PTSD risk factor items pulled from the EHR were: 1) Gender, 2) Race, 3) Insurance, 4) Treated in the intensive care unit (ICU) during the injury admission, 5) Blood alcohol content positive or any substance disorder international classification of disease (ICD) from EHR, 6) Any psychiatric disorder ICD from EHR, 7) PTSD ICD from EHR, 8) Tobacco use, 9) Injury inflicted by another, and 10) At least one prior hospitalization. Consenting patients with scores ≥ 3 on the initial EHR screen were next screened with the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) PTSD Checklist-Civilian Version (PCL-4). To be included in the study, patients were required to score ≥ 35 on the PCL-4 (Russo et al., 2013) and to have ≥ 1 severe posttraumatic psychosocial concern (Zatzick et al., 2018). Patients were excluded if they required immediate psychiatric intervention (e.g., self-inflicted injury, active psychosis), were cognitively impaired, or were currently incarcerated. After completing the baseline assessment, subjects were randomized to 1 of 2 active comparator conditions, a peer integrated collaborative care intervention or enhanced usual care.
Intervention Activities
The investigation aimed to integrate injured patient peers with front-line acute care providers as part of a multidisciplinary team (Scheuer et al., 2020). In the hours, days and weeks after injury, peers elicit patient post-injury concerns and target these concerns for amelioration, while also working with other members of the intervention team. The peers work with other team members to coordinate care by linking injured patients from inpatient and emergency department settings to primary care and community services. Working with peers, clinical (e.g., MSW, MD) and other study team members deliver evidence-based preventive interventions targeting reductions in recurrent injury risk behaviors (Walton et al., 2010; Zatzick et al., 2014) as well as reductions in the symptoms of posttraumatic stress disorder (PTSD) (Darnell et al., 2017; Zatzick et al., 2013). Psychopharmacologic intervention can also be delivered to injured patients with high levels of PTSD and other symptoms. The clinical team members record all patient encounters in REDCap, and the supervising psychiatric clinician investigator also documents case discussions and summaries in REDCap.
Data Collection and Analyses
The RAPICE approach is designed to be adaptable to diverse real world health service delivery contexts (Palinkas & Zatzick, 2019). Central tenants of the approach include the formation of a multidisciplinary team, use of multiple data sources, iterative data collection and analysis in real time, and rapid completion of the project.
In the current study, the RAPICE approach was implemented with the following context specific adaptations. A senior investigator with prior training in RAPICE methods led the project (Palinkas & Zatzick, 2019; Zatzick et al., 2010; Zatzick et al., 2011). The multidisciplinary clinical research team included patient peer treatment team members, research assistants and coordinators, front-line clinicians, clinician investigators, and external consultants. The RAPICE approach incorporated the use of several data collection methods, including participant observation in clinical settings, the recording of field notes and jottings and the review of primary source documents (e.g., medical records, REDCap research notes).
Clinician and peer team members continued to treat patients who had been previously randomized to the comparative effectiveness trial intervention group and were being followed longitudinally during the King County COVID-19 outbreak. Clinical team members recorded patient progress notes in REDCap; additional logging of field jottings related to unique COVID-19 clinical scenarios also occurred. REDCap notes, electronic medical record review and field jottings were aggregated into brief clinical case vignettes. The vignettes were disguised in order to protect patient identities.
Beyond the compilation of case studies, as an iterative method, RAPICE data collection naturalistically evolved to include observations of intervention team activity occurring within the larger COVID-19 pandemic epicenter context. Prior to the pandemic, the Trauma Survivors Outcomes and Support (TSOS) study team had a daily morning meeting in which clinical research procedures were reviewed and team protocols were established. In the wake of the pandemic, the briefer morning meeting evolved into a more extensive team discussion or “huddle” of pandemic related topics.
Notes and jottings derived from daily huddle discussions were subjected to thematic coding. Thematic coding in RAPICE can incorporate different analytic methods that vary markedly in resource and adjudication intensity (Palinkas & Zatzick, 2019). In the current COVID-19 pandemic context, with minimal multidisciplinary team resources allocated to primary data analysis, less time-intensive crystallization immersion coding procedures were employed (Miller & Crabtree, 1992).
Data presentation derived from RAPICE observation can take multiple forms, including case series, presentations, summary diagrams and figures, and descriptive text (Palinkas & Zatzick, 2019). The current investigation first presents a series of clinical cases exemplifying the types of preventive interventions that can be introduced to target COVID-19 exposures. Next, a narrative summary of the team huddle experience is presented and huddle discussion themes explicated.
Results
Clinical Case Series
Case 1
The patient is a 63-year-old Caucasian female with a history of coronary artery disease who was in a head-on motor vehicle crash that resulted in multiple extremity fractures and a laceration to her right lung and subsequent pneumonia. The patient was transported from a rural location to Harborview Medical Center in Seattle. As is typical of acute care, the patient had a series of orthopedic visits scheduled as follow-up at Harborview. However, during a follow-up phone discussion with the peer interventionist, the patient wondered about the wisdom of attending future visits at the Harborview due to the recent outbreak of COVID-19 and the patient’s underlying health conditions that placed her at risk for developing a severe case of COVID-19 if she were to contract the virus. The peer referred the patient to study team clinicians, who worked with the patient and the patient’s primary care provider to find a local, non-Harborview orthopedic referral.
Case 2
The patient is an 85-year-old Caucasian female with a history of diabetes and hypertension who was struck by a car as a pedestrian, resulting in a left femur fracture. The patient has had an extended injury recovery and was recently re-hospitalized with complications from the original injury. During a follow-up telephone conversation with the peer interventionist, the intervention team learned that the patient and her husband, as part of a faith-based charity effort, had allowed an individual who lacked permanent housing to reside with their family. The house guest had subsequently developed a flu-like syndrome characterized by fever and cough. Upon learning of this potential exposure, the study team reviewed the physical health symptoms of the patient; per the patient’s husband, the patient had been experiencing extreme fatigue and potentially other symptoms. The patient’s husband reported he had also been feeling ill. When it was determined that all 3 individuals in the household had experienced flu-like symptoms that could potentially be linked to COVID-19 exposure, members of the clinical research team proceeded to ensure the appropriate medical providers were contacted. With the patient’s permission, the study contacted the patient’s primary care provider and recommended that the provider evaluate the patient for a possible COVID-19 exposure.
Case 3
The patient is an 18-year-old Asian male who was shot in the head, resulting in a cervical spinal cord injury and initial quadriplegia. At the time of his initial injury admission, the patient was hospitalized in the intensive care unit and intubated for approximately 24 hours. The patient has since recovered some upper extremity strength but remains wheelchair bound. The patient currently resides in a skilled nursing facility, as he needs extensive rehabilitative care. The patient has received ongoing intervention from the study team that has focused on peer violence prevention (Dicker, 2016) and motivational interviewing targeting multiple recurrent injury risk behaviors (Walton et al., 2010; Zatzick et al., 2014). The study team members, including the peer interventionist, had attended the patient’s hospital-based outpatient appointments during the coronavirus outbreak. The patient’s ongoing physical vulnerability, when combined with his residence in a Washington State nursing facility (Kamp, 2020), were judged by the study team to place the patient at high risk for a challenging clinical course if exposed to COVID-19. The study team is using a motivational interviewing intervention to weigh with the patient potential risk mitigation strategies, including the pros and cons of potentially moving out of the nursing home environment into a relative’s home.
Clinical and Research Team “Huddle”
Prior to the pandemic, the TSOS study team had a daily (Monday through Friday) 8 a.m. morning meeting in which clinical research procedures were reviewed and team protocols were established. The COVID-19 outbreak impacted the clinical research team at a number of levels, including considerations of individual provider and family member, collegial and community level health risk and exposure assessments. Each morning, clinical team discussions lengthened to incorporate these novel COVID-19 related discussion topics. Participant observation with associated field notes and jottings documented the diverse multilevel COVID-19 clinical research team discussions that occurred as previously briefer team meetings evolved into more extensive COVID-19 focused team huddles.
The overarching goal of the huddle became to raise and transparently discuss the multilevel issues derived from the COVID-19 pandemic. The huddle aimed to address the observation that information evolved rapidly, and multiple information sources did not frequently cover the full range of scenarios encountered by the front-line clinical research team members. The study team huddle had the following characteristics.
The huddle was an open discussion with a moderator that focused on individual stabilization and individual physical and emotional regulation for team members.
Updated guidances released by the University of Washington and/or CDC were discussed. The team also reviewed the unfolding clinical situation at Harborview and other King County hospitals.
Depending on the topic and the latest public health or organizational guidances, the huddle lasted between 30–60 minutes.
A key theme that emerged from these huddles was the convergence of individual and/or family commitments with team organizational and collegial commitments. Specific attention was given to the way that these obligations could be at odds with one another, and how to weigh the benefits and risks associated with a particular course of action in regard to these competing demands. This was drawn into sharp relief during an early team huddle discussion of a critically ill frontline provider (Green & Clarridge, 2020). On March 16, 2020, the team became aware of an emergency room physician in his mid-40s who was intubated and in the intensive care unit (ICU) after triaging an influx of COVID-19-positive patients at a neighboring King County hospital. The team discussion focused on the risks inherent in working at an acute-care facility triaging and treating potential COVID-19 patients. The team had been evaluating each member’s COVID-19 exposure risk and developing plans to mitigate that risk while carrying out research and clinical obligations. As a result, the team decided that while essential clinical research staff (e.g., MDs, MSWs) would remain at the hospital to triage clinical emergencies, all other team members, including patient peers, would work from home.
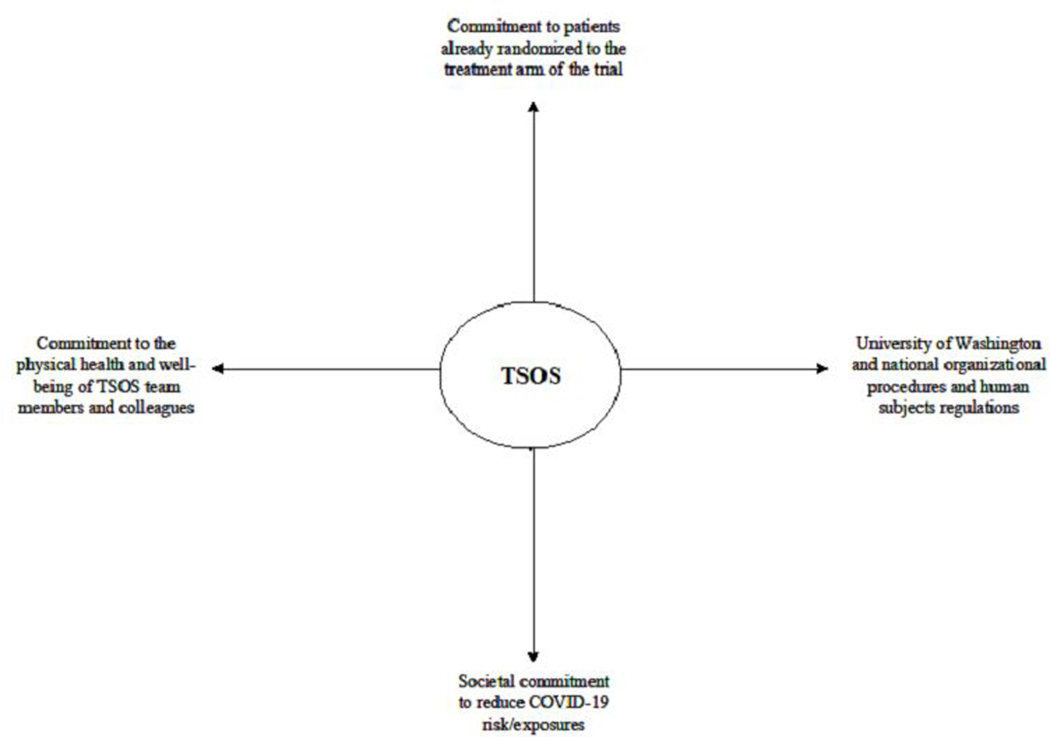
The decision to have the patient peers work from home culminated an approximately 2-week disaster-focused ethical analysis and deliberation (Howe & Newman, 2017). The study team considered the risks and benefits of each individual team member’s physical presence at Harborview. For instance, a core element of the intervention being tested in the original comparative effectiveness trial was whether or not previously injured patient peers could be integrated into a collaborative care team. However, previously injured peers may have chronic disease risk factors (e.g., histories of intensive care unit intubation/pulmonary infections in the wake of traumatic injury exposure) that increase the risk of more severe complications if subsequently exposed to COVID-19. These discussions regarding the potential for patient peer exposure to COVID-19 that could lead to serious morbidity elucidated the ethical tensions between providing the highest quality peer intervention for patients already randomized into the trial and the societal imperative to reduce COVID-19 risks and exposures (Figure 1) (Emanuel & Emanuel, 1992; Howe & Newman, 2017).
Figure 1.
Trauma Survivors Outcomes & Support (TSOS) Individual, Familial, Collegial and Societal Tensions for Clinician-Provider Decision Making
Other team huddle discussion topics elucidated additional ethical tensions. For example, a provider on the team had an aging parent who resided in an eldercare group living home, and she was considering moving the parent back into her home. Most COVID-19 fatalities in King County occurred at another such facility when the virus spread rapidly among residents, indicating that the parent’s current living situation might put them at high risk for exposure (Kamp, 2020; McMichael et al., 2020). However, the provider was also at risk for exposure due to her work at Harborview, and since she was asymptomatic, she did not meet the current guidelines to receive a COVID-19 test. The team entered into a disaster focused ethical analysis and deliberation (Howe & Newman, 2017). The deliberation focused on the ethical tension between complying with organizational directives regarding testing protocols, the societal impetus to reduce exposures, and the provider’s familial obligation to protect her parent from COVID-19 exposure (Figure 1).
Team huddle discussions extended beyond transparent deliberation of ethical tensions occurring as a result of the COVID-19 outbreak to include physical and emotional health supportive principles adapted for the pandemic context (Table 1). These supportive principles included activities that promoted physical health, such as awareness of hand washing routines, and activities targeting emotional well-being, such as the monitoring of social media use.
Table 1.
Activities Promoting Clinician-Provider Physical & Emotional Health and Community Well-Being in the Pandemic Context
| Clinician-Provider Activity | Example |
|---|---|
| Individual awareness of and reflection on daily routines | Reflecting on hygienic activities, such as hand washing, and incorporating of new behaviors, such as frequent 20 second cleansings |
| Taking stock of individual, familial, collegial and community commitments and exposure risks | Consideration of familial exposure risks, such as the risks and benefits of housing elderly parents in nursing facilities/elderly group living situations |
| Monitoring of social media use | Selective use of social media sites, as well as considering the timing/daily sequencing of social media contacts |
| Prioritizing stress reduction activities | Ensuring breaks in daily activities for exercise/calming activities |
| Extending support to family, friends, colleagues and community as time and energy allows | Connecting with individuals who are preventing COVID-19 exposure by practicing social distancing |
Finally, during the course of these extended huddles, it became clear that the expertise required to answer the evolving questions related to individual and family illness exposure and organizational and national policy would require consultation beyond the investigative team. The RAPICE approach flexibly integrates external consultants (Palinkas & Zatzick, 2019; Zatzick et al., 2011), and appropriate individuals were sought out within the organization and nationally in order to answer questions that arose in the rapidly fluctuating pandemic context. The team began to cultivate a series of relationships with expert consultants, including Harborview emergency preparedness directors and national disaster mental health leadership within the ASPR Western Regional Alliance for Pediatric Emergency Management (Schreiber, 2020). These consultants were often able to provide on-the-ground knowledge and updates more rapidly than the information released from official sources.
Discussion
The current investigation adds to the emerging literature on the United States’ COVID-19 outbreak by demonstrating that in the pandemic context, during which local and national guidances struggle to keep up with the rapidly evolving conditions, clinical and research teams can benefit from approaches that allow them to rapidly assess on-the-ground experiences and update team procedures accordingly. The examination of a clinical case series combined with review of provider experiences can yield early, important lessons learned. For instance, a review of the case studies suggests that both primary and secondary intervention strategies can be integrated into ongoing care coordination interventions. Primary intervention strategies can include redirecting patients away from high COVID-19 density clinical settings to settings with less risk of exposure to the virus. Secondary prevention strategies include evaluating the COVID-19 exposure risk of patients with chronic conditions, and then proactively acting to ameliorate exposure risks. Additionally, the results suggest that patient-centered motivational interviewing interventions, which can be embedded within care coordination, may be an optimal approach to weighing the pros and cons of COVID-19 prevention strategies. The case series suggests the potential for novel preventive intervention development for other challenges raised by the pandemic, such as maintaining social distancing while still receiving necessary medical care.
Beyond patient-focused issues, a key theme for clinicians, peers and research staff on the team was that of front-line provider vulnerability to severe COVID-19 respiratory illness. The March 16, 2020 huddle discussion, in which the team reviewed the recent announcement that an emergency room physician at a King County hospital was critically ill and being treated in the ICU, led the team to definitively withdraw all non-key clinical personnel from the hospital setting. The team also reflected on the possibility that a member of their own team could potentially become critically ill and require care at the facility in which they worked. This concern shed light on the ethical tension between the preservation of team-member physical and emotional well-being and the need to continue study-related activities, particularly those that served patients already randomized to the study’s intervention arm. A key observation derived from the current investigation is reflecting on each team member’s individual vulnerability to severe respiratory illness in the wake of COVID-19 exposure. As recent developments in US health care system research have encouraged the incorporation of patient peers into front-line teams delivering clinical interventions, this observation could help inform other clinical and research teams’ decisions regarding the safety of patient peers as the pandemic evolves (PCORI, 2017).
Multiple rapidly shifting clinical guidances and protocols are now being developed to address the COVID-19 pandemic (2019 Novel Coronavirus (nCoV) Response Program, 2020; Coronavirus (COVID-19), 2020; COVID-19 (2019 novel coronavirus) resource center for physicians, 2020; Pandemics, 2020). Providers face multiple individual, collegial and organizational competing demands and ethical tensions that are likely to fluctuate as new COVID-19 guidances emerge. The approximately 2-week study period revealed multiple examples of clinical research team members grappling with competing ethical tensions. As members of their local community, the team members had an overarching commitment to diminish opportunities for COVID-19 exposure within King County. However, this key directive often conflicted with study team’s obligation to provide on-going care to patients already randomized to the intervention in the comparative effectiveness trial, which often involved meeting patients at outpatient clinics, the emergency department and the hospital.
A daily morning team huddle facilitated reflection on these competing directives and obligations. Ethical tensions front-line providers faced had the potential to cause ongoing emotional strain and could contribute to physical and mental health related burnout if not proactively addressed as part of the organizational pandemic response. The huddle also prompted team reflection on daily routines, monitoring of social media use and prioritization of stress reduction activities. Transparently taking stock of multilevel commitments and ultimately the extension of support to family, friends and colleagues were also discussion topics with the potential to enhance team member well-being during the pandemic.
RAPICE may constitute an ideal method for investigation during pandemics and other evolving post-disaster contexts. Five weeks after the 7.0 earthquake in Haiti in January of 2010, a mental health training was developed for 24 doctors, nurses, social workers and psychologists to integrate knowledge about screening and intervention for posttraumatic stress reactions in human immunodeficiency virus (HIV) treatment and general medical settings (Zatzick et al., 2010). The workshop was modified for the Haitian post-disaster context and evaluated using the RAPICE approach. Initially, the workshop facilitators planned to focus on Haitian HIV-positive patients, but upon arrival, the team realized that Haitian providers had also been exposed to familial, collegial and community loss, and were demonstrating a need for acute mental health coping resources. Therefore, based on RAPICE field observations, the study team modified the session to primarily address provider bereavement and posttraumatic stress. Based on RAPICE-derived observations, the study team elected to deliver the patient-focused training at a separate workshop in July of 2010, the 6-month anniversary of the earthquake. Across 2 disaster settings, post-natural disaster in Haiti and in the current pandemic disease outbreak in King County, RAPICE has demonstrated the ability to rapidly integrate multiple data sources and nimbly incorporate iterative data collection and analyses.
The RAPICE approach in the current investigation is limited by the inability to fastidiously apply comparative coding frameworks (Palinkas & Zatzick, 2019). Although challenging to implement in the immediate post-disaster or pandemic context, more in-depth thematic coding could be considered in future studies.
This investigation aimed to provide early insights and lessons learned from a compilation of case studies and participant observation at the early epicenter of the United States coronavirus (COVID-19) pandemic. Emerging observations from case studies suggested that primary and secondary prevention strategies can be incorporated into ongoing treatment provided to vulnerable patients who are at risk for COVID-19 exposure. Procedures, such as a daily team huddle, that can flexibly accommodate virtual participation and transparently incorporate discussion of ethical tensions and supportive principles may lead to increased clarity for providers grappling with multilevel and rapidly evolving individual, organizational and societal directives. Proactive assessments of individual provider vulnerabilities to severe respiratory illness in the wake of COVID-19 exposure may also be a crucial element of health care system pandemic responses.
Acknowledgements
The authors wish to acknowledge Heather Kelly-Hendrick, M.D., for her open communication and dedicated commitment to her patients and colleagues during the King County COVID-19 outbreak.
Funding
This study was supported in part by the Patient-Centered Outcomes Research Institute (PCORI) Award (IHS-2017C1–6151). This research was also supported within the National Institutes of Health (NIH) Health Care Systems Research Collaboratory by cooperative agreement 1UH2MH106338–01/4UH3MH106338–02 from the National Institute of Mental Health. Support was also provided by the NIH Common Fund through cooperative agreement U24AT009676 from the Office of Strategic Coordination within the Office of the NIH Director. The content is solely the responsibility of the authors and does not necessarily represent the official views of PCORI, its Board of Governors or Methodology Committee, or the NIH.
Biography
Kathleen Moloney is a Research Coordinator at the Department of Psychiatry and Behavioral Sciences at the University of Washington where she coordinates data analysis and care management for early intervention studies for PTSD in trauma survivors. She received her bachelor’s degree in Neuroscience from the University of Southern California.
Hannah Scheuer is a Social Worker at the Department of Psychiatry and Behavioral Sciences at the University of Washington where she coordinates care management and regulatory procedures for an early intervention study for PTSD in trauma survivors. She received her bachelor’s degree in Psychology from Reed College and her Master of Social Work from Portland State University.
Allison Engstrom is a Research Coordinator at the Department of Psychiatry and Behavioral Sciences at the University of Washington where she coordinates the regulatory procedures, data analysis and care management for early intervention studies for PTSD and related comorbidities. She received her bachelor’s degree in Psychology from the University of Houston.
Merritt Schreiber is a Professor of Clinical Pediatrics at the David Geffen School of Medicine at UCLA as well as an Investigator at The Lundquist Institute. Dr. Schreiber’s research interests focus on disaster mental health, the management of acute psychological trauma in children and adults and the management of psychological casualties in Emergency Medicine and Trauma Care.
Lauren Whiteside is an Assistant Professor in the Department of Emergency Medicine at the University of Washington and an Emergency Medicine Physician at Harborview Medical Center. Dr. Whiteside’s research interests focus on the intersection of emergency medicine, substance use, mental health and injury.
Deepika Nehra is an Assistant Professor in the Department of Surgery at the University of Washington and a Trauma and Acute Care Surgeon at Harborview Medical Center. Dr. Nehra’s research interests focus on understanding the long-term impact of injury and emergency surgery with a particular interest in the psychosocial aspects of injury impact and recovery.
Mary Lou Walen is a Peer Interventionist at the Department of Psychiatry and Behavioral Sciences at the University of Washington where she provides psychosocial and care coordination support to patients randomized into an early intervention study for PTSD in trauma survivors.
Frederick Rivara is a Professor in the Department of Pediatrics at the University of Washington as well as a member of the Core Research Faculty at the Harborview Injury Prevention and Research Center. Dr. Rivara’s research interests focus on long term disability after traumatic brain injury in children, interventions to reduce the prevalence of PTSD after traumatic injury in adolescents and the genetic factors associated with poor recovery from trauma.
Douglas Zatzick is a Professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington as well as a member of the Core Research Faculty at the Harborview Injury Prevention and Research Center. Dr. Zatzick’s research interests focus on pragmatically focused clinical trials targeting PTSD and related comorbidities in traumatically injured populations.
Footnotes
Declaration of Interests
The authors declare no conflicts of interest.
References
- 2019 Novel Coronavirus (nCoV) Response Program. (2020, March 16). University of Washington; Retrieved March 16 from https://one.uwmedicine.org/coronavirus [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020, February 26, 2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronavirus (COVID-19). (2020). Centers for Disease Control and Prevention. Retrieved March 16 from https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Coronavirus COVID-19 Global Cases. (2020, March 13). Center for Systems Science and Engineering at Johns Hopkins University. https://coronavirus.jhu.edu/map.html
- COVID-19 (2019 novel coronavirus) resource center for physicians. (2020). American Medical Association. Retrieved March 16 from https://www.ama-assn.org/delivering-care/public-health/covid-19-2019-novel-coronavirus-resource-center-physicians
- Darnell D, O’Connor S, Wagner A, Russo J, Wang J, Ingraham L, Sandgren K, & Zatzick D (2017, March 1). Enhancing the Reach of Cognitive-Behavioral Therapy Targeting Posttraumatic Stress in Acute Care Medical Settings. Psychiatric Services, 68(3), 258–263. 10.1176/appi.ps.201500458 [DOI] [PubMed] [Google Scholar]
- Dicker RA (2016). Hospital-based violence intervention: An emerging practice based on public health principles. Trauma Surgery & Acute Care Open, 1(1), e000050. 10.1136/tsaco-2016-000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel EJ, & Emanuel LL (1992). Four models of the patient-physician relationship. JAMA, 267, 2221–2226. [PubMed] [Google Scholar]
- Green SJ, & Clarridge C (2020, March 15). EvergreenHealth doctor tests positive for coronavirus, in critical condition The Seattle Times; https://www.seattletimes.com/seattle-news/health/evergreenhealth-doctor-tests-positive-for-coronavirus-in-critical-condition/ [Google Scholar]
- Howe EG, & Newman E (2017). Ethical Issues in Disaster Psychiatry In Raphael B, Fullerton CS, Weisaeth L, & Ursano RJ (Eds.), Textbook of Disaster Psychiatry (2 ed., pp. 314–324). Cambridge University Press; 10.1017/9781316481424.022 [DOI] [Google Scholar]
- Kamp J (2020, March 10). Coronavirus Spreads to More Elder Facilities in Seattle Area. The Wall Street Journal. https://www.wsj.com/articles/coronavirus-spreads-to-more-elder-facilities-in-seattle-area-11583884557 [Google Scholar]
- McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Lewis J, Baer A, Kawakami V, Lukoff MD, Ferro J, Brostrom-Smith C, Rea TD, Sayre MR, Riedo FX, Russell D, Hiatt B, Montgomery P, Rao AK, Chow EJ, Tobolowsky F, Hughes MJ, Bardossy AC, Oakley LP, Jacobs JR, Stone ND, Reddy SC, Jernigan JA, Honein MA, Clark TA, & Duchin JS (2020). Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. New England Journal of Medicine. 10.1056/NEJMoa2005412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WL, & Crabtree BF (1992). Primary care research: A multimethod typology and qualitative road map In Doing qualitative research. (pp. 3–28). Sage Publications, Inc. [Google Scholar]
- Morganstein JC, Fullerton CS, Ursano RJ, Donato D, & Holloway HC (2017). Pandemics: Health Care Emergencies In Raphael B, Fullerton CS, Weisaeth L, & Ursano RJ (Eds.), Textbook of Disaster Psychiatry (2 ed., pp. 270–284). Cambridge University Press; 10.1017/9781316481424.019 [DOI] [Google Scholar]
- Palinkas LA, & Zatzick D (2019). Rapid assessment procedure informed clinical ethnography (RAPICE) in pragmatic clinical trials of mental health services implementation: Methods and applied case study. Administration and Policy in Mental Health and Mental Health Services Research, 46(2), 255–270. 10.1007/s10488-018-0909-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandemics. (2020). American Psychological Association. Retrieved March 16 from https://www.apa.org/practice/programs/dmhi/research-information/pandemics
- PCORI. (2017). Improving Healthcare Systems - Cycle 1 2017. Patient-Centered Outcomes Research Institute; https://www.pcori.org/funding-opportunities/improving-healthcare-systems-cycle-1-2017 [Google Scholar]
- Russo J, Katon W, & Zatzick D (2013, September-October). The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry, 35(5), 485–491. 10.1016/j.genhosppsych.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheuer H, Engstrom A, Thomas P, Moodliar R, Moloney K, Walen ML, Johnson P, Seo S, Vaziri N, Martinez A, Maier R, Russo J, Sieber S, Anziano P, Anderson K, Bulger E, Whiteside L, Heagerty P, Palinkas L, & Zatzick D (2020). A comparative effectiveness trial of an information technology enhanced peer-integrated collaborative care intervention versus enhanced usual care for US trauma care systems: Clinical study protocol. Contemporary clinical trials, 105970–105970. 10.1016/j.cct.2020.105970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber M, Cates DS, Formanski S, & King M (2019, Mar 1). Maximizing the Resilience of Healthcare Workers in Multi-hazard Events: Lessons from the 2014–2015 Ebola Response in Africa. Mil Med, 184(Suppl 1), 114–120. 10.1093/milmed/usy400 [DOI] [PubMed] [Google Scholar]
- Schreiber MD (2020). Model State Level Infectious Disease Behavioral Health Response Plan [Draft Model State Level EID BH Response]. Lundquist Institute, Harbor-UCLA Medical Center, David Geffen School of Medicine at UCLA. [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, & Cunningham RM. (2010). Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA, 304(5), 527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Coq N, Frederic J, Pierre-Louis M, Robinson E, Chery J, Bijou S, Wilhelm S, Barnhart S, & Hahn L (2010). Psychosocial support training for HIV health care providers in response to the Haitian earthquake Consortium of Universities for Global Health Annual Meeting,, University of Washington. [Google Scholar]
- Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Dunn C, Lord SP, Petrie M, O’Connor SS, & Katon W (2013). A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery, 257(3), 390–399. 10.1097/SLA.0b013e31826bc313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Rivara F, Jurkovich G, Russo J, Trusz SG, Wang J, Wagner A, Stephens K, Dunn C, Uehara E, Petrie M, Engel C, Davydow D, & Katon W (2011, March-April). Enhancing the population impact of collaborative care interventions: Mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. Gen Hosp Psychiatry, 33(2), 123–134. https://doi.org/S0163-8343(11)00002-8[pii] 10.1016/j.genhosppsych.2011.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Russo J, Lord SP, Varley C, Wang J, Berliner L, Jurkovich G, Whiteside LK, O’Connor S, & Rivara FP (2014). Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial. JAMA Pediatr, 168. [DOI] [PubMed] [Google Scholar]
- Zatzick D, Russo J, Thomas P, Darnell D, Teter H, Ingraham L, Whiteside LK, Wang J, Guiney R, Parker L, Sandgren K, Kelly Hedrick M, Van Eaton EG, & Jurkovich G (2018, March 13). Patient-Centered Care Transitions After Injury Hospitalization: A Comparative Effectiveness Trial. Psychiatry, 1–17. 10.1080/00332747.2017.1354621 [DOI] [PubMed] [Google Scholar]