Abstract
Background/Purpose:
The U.S. has an alarming rate of firearm injuries. Racial disparities among victims and predictors of outcomes are not well established. Our objective was to assess costs, length of stay (LOS), and inpatient mortality among nonfatal and fatal pediatric firearm injuries that required hospitalization.
Methods:
Pediatric (≤ 18 years of age) hospitalizations with a firearm injury discharge diagnosis were identified from the national Kids’ Inpatient Databases (KID) for 2006 through 2012. Firearm injury intent, weapon type, and hospitalization rates by racial groups were examined. Inpatient mortality, costs, and length of stay were examined using regression models.
Results:
Of 15,211 hospitalizations, the majority of injuries were due to assault (60%) and the intentions of firearm injury differed by race (p < 0.001). The median cost per hospitalization was $10,159 (interquartile range: $5,071 to $20,565), totaling more than a quarter of a billion dollars. On regression analysis, Black (OR: 0.41; CI: 0.30–0.55) and Hispanic (OR: 0.47; CI: 0.34–0.66) patients were less likely to die than White patients.
Conclusion:
Pediatric firearm injury circumstances and survival vary by race with Whites being more likely to experience unintentional injury and suicide, while Blacks and Hispanics are more likely to experience inflicted injury.
Keywords: Firearm Violence, Pediatric Trauma, Racial Disparities, Costs
INTRODUCTION
Globally, the United States has the highest pediatric firearm injury rate among developed countries [1]. In 2013, 4.2% of children under 18 years of age witnessed firearm violence [2]. Further, firearm fatalities ranked in the top 5 causes of unintentional injuries for children aged 1–18 in 2016. For every child killed, a substantially greater number are seriously injured, and approximately half of children hospitalized with a firearm-related injury are discharged from the hospital with a disability [3]. Such disabilities have been defined as any degree of limitation in vision, hearing, speech, activities of daily living, cognition, behavior, or bladder/bowel control.
Prior pediatric trauma research centered on motor vehicle collisions, drownings, and fires have successfully decreased death rates from these causes as a result of translatable research [4]. Due to the high incidence and serious injuries associated with firearm injuries in the pediatric population of the U.S., other authors have suggested a similar public health approach for firearm prevention [5–8]. The current literature on pediatric firearm injuries demonstrate that boys, older children, and minorities are disproportionately affected [5, 8]. Approximately 3% of children with firearm injuries died in the emergency department (ED), and 48% of powder-related firearm injuries were admitted to the hospital [5, 6]. Firearm homicides of younger children often occurred in multi-victim events and involved family conflict, while older children more often died in the context of crime [9]. Children and adolescents have similar firearm-related mortality rates in urban and rural settings, although homicides were twice as likely among urban youth and suicides were twice as likely among rural youth [10]. Suicide in adolescents results in more than 1,000 deaths annually and has markedly increased between 1999 and 2014 [11].
While several firearm injury studies have analyzed costs, the majority investigated both adults and children [12–15]. Further, none of the studies have implemented multivariable analyses which assess predictors that determine important outcomes, such as mortality, length of stay (LOS), and drivers of costs. Moreover, only one study has focused solely on children and adolescents, but their multivariable analysis was constructed to derive information on those most at-risk for firearm injuries [14].
While other studies have focused on firearm injury intent, our objective was to understand the predictors of costs, LOS, and inpatient mortality in nonfatal and fatal firearm injuries in the pediatric population.
1. MATERIAL AND METHODS
1.1. Study Design and Data Source
This was a retrospective cross-sectional study of pediatric firearm injuries that resulted in an inpatient hospitalization at U.S. hospitals. We used the Kids’ Inpatient Database (KID) from 2006, 2009, and 2012 [16]. The KID database was developed for the Healthcare Cost and Utilization Project (HCUP) by the Agency for Healthcare Research and Quality (AHRQ), and it was the largest deidentified all-payer pediatric inpatient dataset available for investigation. The dataset excludes ED visits, outpatient visits, or pre-hospital deaths. Since 1997, the database has been updated and released every 3 years with national estimates containing demographic, clinical, and hospital discharge data. The discharge data was weighted to obtain national estimates.
1.2. Study Cohort
Children and adolescents (≤ 18 years) who experienced an inpatient hospital admission secondary to a firearm injury were included in the study (Figure 1). Both nonfatal and fatal injuries were included. We utilized the external cause of injury codes (E-codes) from the International Classification of Diseases Ninth Revision (ICD09) for inpatient hospitalizations secondary to firearm injuries. The E-codes specify the intent of injury as well as the type of gun used, if known. Intent was categorized as Assault (E965.0–965.4, E968.6), Suicide (E955.0–955.4, E955.6), Unintentional (E922.0–922.4, E922.8–922.9, E928.7), and Undetermined (E985.0–985.4, E985.6).
Figure 1.
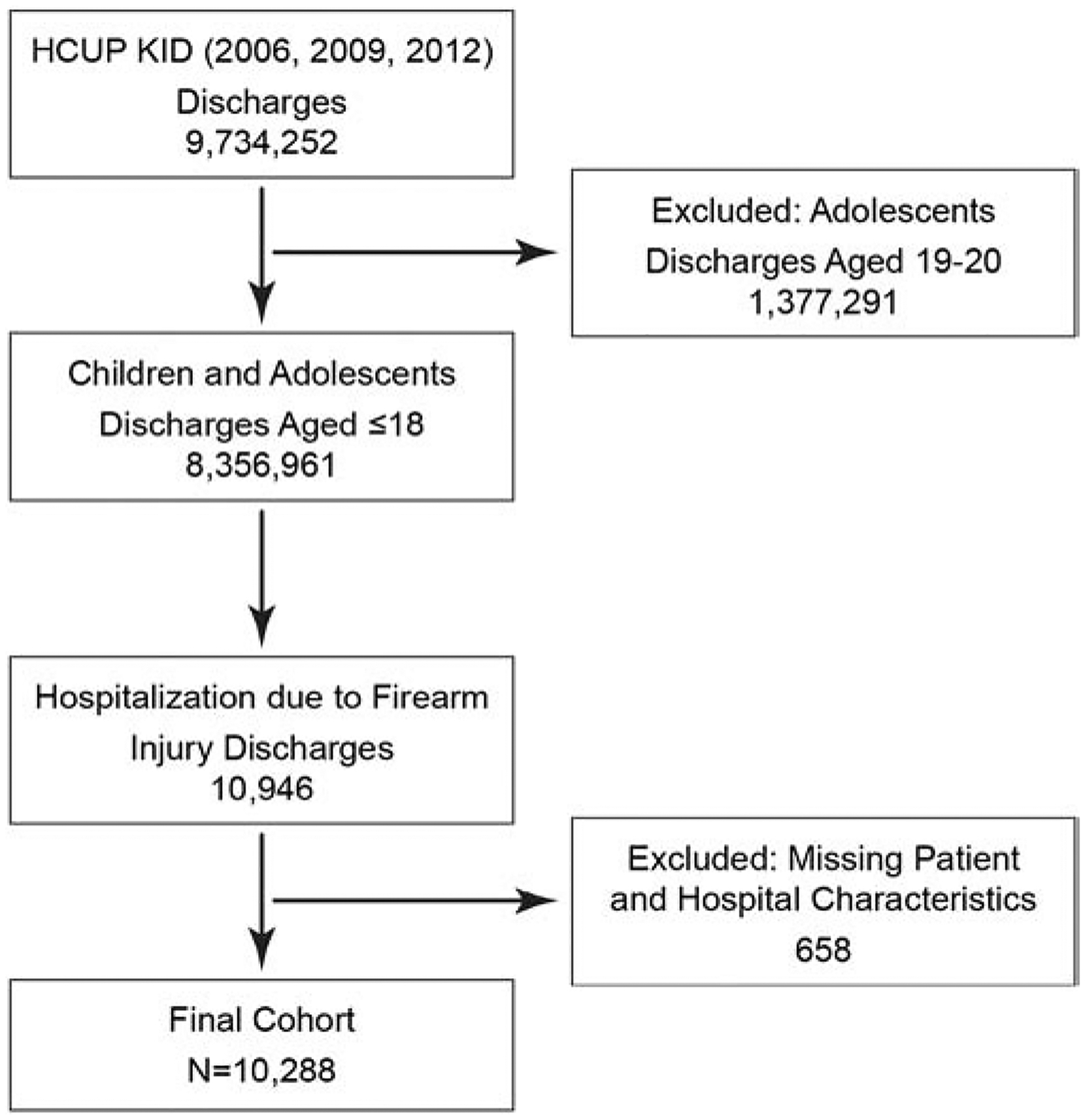
Unweighted Cohort Development
1.3. Patient Characteristics
Patient characteristics included Age (at the time of hospitalization), Sex, Race, Socioeconomic status, Insurance payer status, Admission day, and Severity of illness and Risk of mortality by the All-Patient Refined Diagnosis-Related Group (APR-DRG) elements (Mild loss of function; Moderate loss of function; Major loss of function; Extreme loss of function). Age was categorized as 0–4, 5–9, 10–14, and 15–18 years of age based on a classification system used by the Centers for Disease Control and Prevention (CDC) [17]. Race was defined as Black, Hispanic, Other, or White, as reported by KID. Those coded as unknown for race were excluded. Socioeconomic status was derived by using the median household income of each patient as a proxy based on their home zip code. Median household income was defined by quartiles by KID (2012: quartile 1: $1–$38,999; quartile 2: $39,000–$47,999; quartile 3: $48,000–$62,999; quartile 4: ≥ $63,000) encompassing the poorest to the wealthiest families. The calculations are done so that the maximum for quartile 1 level of income represented 150% of the poverty level, and the margin between the second and third quartiles approximated the nation’s median household income [16]. The expected primary insurance payer was divided into Private, Self-pay, Other, and Medicaid/Medicare. Of note, if a readily identified category for payer source was not available, it was categorized as Other in the dataset. Patients with missing data were excluded.
1.4. Hospital Characteristics
Hospital characteristics included were Bed size, Region of the U.S., Hospital teaching status, and Children’s hospital status. Bed size was categorized as Small, Medium, and Large based on the number of hospital beds specific to the region of the hospital and teaching status. U.S. hospital census regions were defined as West, Northeast, South, and Midwest, according to the U.S. Census Bureau. Hospital teaching status was reported as Rural, Urban non-teaching, and Urban teaching. Children hospitals were defined according to the American Hospital Association (AHA) Annual Survey and data obtained from the National Association of Children’s Hospitals and Related Institutions, which included only freestanding children’s hospitals.
1.5. Outcome Variables
Primary outcome measures were Total hospital charges, LOS, and Inpatient mortality. Total hospitals costs were calculated using the HCUP Cost-to-Charge Ratio files and converted to the 2012 U.S. dollar amount to adjust for the rate of inflation. All costs were adjusted using the Consumer Price Index.
1.6. Statistical Analysis
Descriptive statistics were used to characterize the study cohort. Unadjusted categorical and continuous variables were analyzed using chi-square and t-test, respectively. A multivariable logistic regression was constructed to determine the association of patient and hospital characteristics with mortality. Multivariable linear regression was used to determine the association of patient and hospital characteristics with Total hospital costs and LOS. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina). This study was deemed exempt by the Institutional Review Board at the University of Texas Medical Branch.
2. RESULTS
2.1. Patient and Hospital Characteristics
A weighted total of 15,211 (unweighted n = 10,288) children and adolescents were included in this study. There were 1,076 patients excluded for missing data. Of the included patients, the majority were male (89%) and aged 15–18 (79%) (Table 1). The majority of firearm hospitalizations involved Blacks (44%), followed by Other race (20%), Hispanic (19%), and White (16%). The majority of children were covered by Medicaid/Medicare (55%) and their family income placed them in the poorest quartile (52%). While most admissions occurred on weekdays (61%), weekend admissions (Saturday-Sunday) were disproportionately represented (39%). A larger number of injuries (68%) were classified as Not Severe (APR-DRG severity of illness: Mild (36%) and Moderate (28%) loss of function). The majority of hospitals were Large (72%), Urban teaching hospitals (83%), and Adult hospitals (92%). The most represented geographical area was the Midwest (34%), followed by the West (26%), the South (24%), and the Northeast (15%) regions.
Table 1.
Patient and hospital characteristics
| (Weighted N) | (15,211) |
| Age | |
| 0–4 | 466 (3%) |
| 5–9 | 627 (4%) |
| 10–14 | 2,106 (14%) |
| 15–18 | 12,012 (79%) |
| Race | |
| Black | 6,752 (44%) |
| Hispanic | 2,881 (19%) |
| Other | 3,098 (20%) |
| White | 2,480 (16%) |
| Gender | |
| Male | 13, 495 (89%) |
| Female | 1,715 (11%) |
| Firearm Type | |
| Air Gun | 1,346 (9%) |
| Handgun | 3,986 (26%) |
| Other | 8,516 (56%) |
| Rifle/Military Firearm | 313 (2%) |
| Shotgun | 1,049 (7%) |
| Intent of Firearm Injury | |
| Assault | 9,122 (60%) |
| Suicide | 490 (3%) |
| Undetermined | 847 (6%) |
| Unintentional | 4,751 (31%) |
| Payer Source | |
| Medicare/Medicaid | 8,358 (55%) |
| Self-pay + Other | 2,663 (17%) |
| Private | 4,189 (28%) |
| Median Household Income | |
| Quartile 1 | 7,970 (52%) |
| Quartile 2 | 3,717 (24%) |
| Quartile 3 | 2,349 (15%) |
| Quartile 4 | 1,225 (8%) |
| Admission Day | |
| Weekday (Monday-Friday) |
9,298 (61%) |
| Weekend (Saturday-Sunday) |
5,912 (39%) |
| Severity of Illness by APRDRG | |
| 1 | 5,507 (36%) |
| 2 | 4,266 (28%) |
| 3 | 2,855 (19%) |
| 4 | 2,582 (17%) |
| Hospital Bed Size | |
| Small | 1,168 (8%) |
| Medium | 3,170 (21%) |
| Large | 10,872 (72%) |
| Hospital Teaching Status | |
| Rural | 417 (3%) |
| Urban Non-teaching | 2,225 (15%) |
| Urban Teaching | 12,569 (82%) |
| Hospital Region | |
| Northeast | 2,272 (15%) |
| South | 3,683 (24%) |
| Midwest | 5,237 (34%) |
| West | 4,018 (27%) |
| Children’s Hospital | |
| No | 14,042 (92%) |
| Yes | 1,169 (8%) |
2.2. Race, gun type, and intent
The most common type of gun used are classified as Other (56%), followed by Handguns (26%) (Figure 2A). When stratified by race, Other gun type remains the most common for all groups (p < 0.001). However, of the identifiable weapon type, Handgun was the most common overall (60%) and was the most common regardless of race. Air guns disproportionately impacted Whites more. Air guns represented only 9% of total firearm injuries, but 22% of injuries in Whites. The percentage of Other gun injuries in Whites was also markedly lower than other races, representing only 32% of injuries. Rifle and Shotgun injuries were more common in Whites than the other race cohorts.
Figure 2.
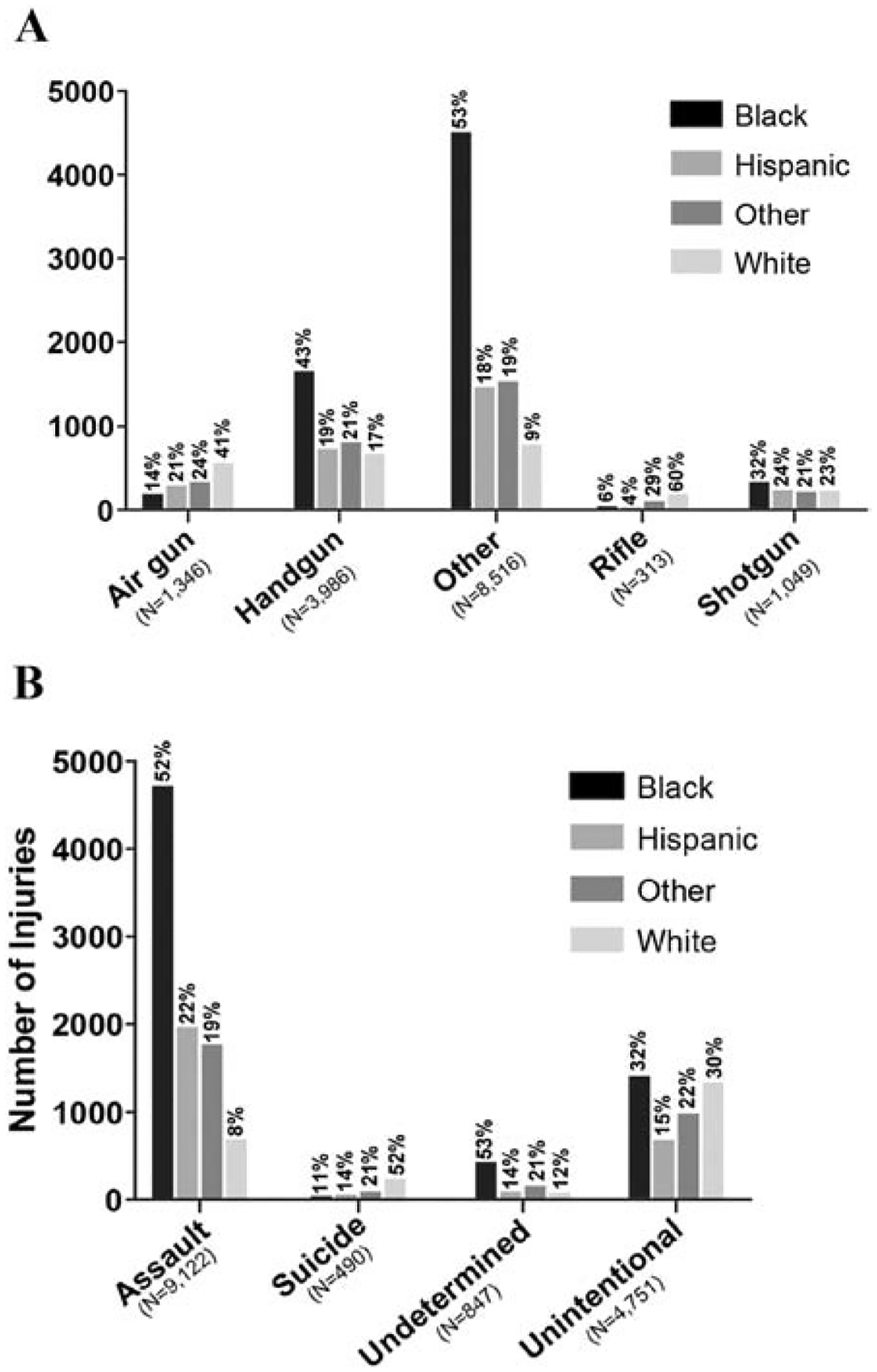
A) Gun type stratified by race. B) Intent stratified by race.
Most commonly, firearm injury hospitalizations were due to Assaults (60%), followed by Unintentional intent (31%) (Figure 2B). When stratified by race, assaults remained the most common form of firearm injury for Blacks (52%), followed by Hispanics (22%). For White patients, Unintentional intent (58%) was the most common type of firearm injury, followed by Assault (28%), Suicide (10%), and Undetermined (4%). Among those hospitalized for suicide (n = 490), the majority of patients were White (52%) when compared to Other (22%), Hispanic (14%), and Black (11%). Of those who committed suicide, Handguns (43%) were commonly used, followed by Other gun (38%), Shotgun (11%), and Air gun (8%).
2.3. Mortality analysis
The overall inpatient mortality for children after firearm injury was 6.5% (Age: 0–4: 5.6%; 5–9: 2.6%; 10–14: 6.4%; 15–18: 6.3%; p = 0.02). Of the total deaths (n = 632) among hospitalized children, Blacks had a slightly higher number of deaths (n = 243; 38%) compared to patients identified as White (n = 150; 24%), Other (n = 126; 20%), or Hispanic (n = 113; 18%). Males represented the majority of children who suffered inpatient mortality (male 88%; female 12%), but when further analyzed using logistic regression, the inpatient mortality rates between males and females were not significantly different. When the gun type was known among those that experience inpatient mortality (n = 237), Handgun accounted for the majority (n = 206; 87%), followed by Shotgun (n = 23; 10%), Rifle/Military weapon (n = 7; 3%), and Air gun (n = 1; 0.4%).
Table 2 reports adjusted odds ratios for patient and hospital characteristics for mortality. By age, with 0–4 as the referent group, there were no statistically significant differences. Compared to White children, Black (OR 0.41, 95% CI 0.30–0.55), Hispanic (OR 0.47, 95% CI 0.34–0.66), and Other race (OR 0.61, 95% CI 0.44–0.87) had lower odds of mortality. Handgun injuries were the most lethal, with a mortality rate of 7.5%, and were 34 times more likely to result in inpatient mortality than an Air gun. Similarly, Other (OR 31, 95% CI 4.11–242.94), Rifle/Military firearms (OR 18.41, 95% CI 2.02–167.88), and Shotgun (OR 20.20, 95% CI 2.37–172.14) had higher odds of resulting in death than an Air gun. As expected, higher severity of illness increased the risk of mortality. When compared to the inpatient mortality for Mild loss of function (0.4%), all other APR-DRG severities had significantly increased mortality rates (loss of function: Moderate = 2.2%, OR 9.72, 95% CI 4.83–19.55; Major = 10.6%, OR 98.07, 95% CI 48.07–200.07; and Extreme = 19.8%, OR 591.30 (289.62 – > 999.99)). Rural hospitals had a significantly lower mortality rate than Urban non-teaching hospitals (0.6% vs. 5.8%). No other hospital characteristics were significant in the model. Although Children’s hospital status had a lower mortality rate than adult centers, statistical significance was not achieved (OR 0.72, 95% CI 0.38–1.38).
Table 2.
Inpatient mortality analysis
| Characteristics | Mortality Rate (%) | Adjusted Odds Ratio (95% CI) |
|---|---|---|
| Age | ||
| 0–4 (Ref.) | 5.6% | |
| 5–9 | 2.6% | 0.36 (0.12–1.12) |
| 10–14 | 6.4% | 1.50 (0.70–3.19) |
| 15–18 | 6.3% | 1.02 (0.51–2.04) |
| Race | ||
| White (Ref.) | 8.8% | |
| Black | 5.4% | 0.41 (0.30–0.55) |
| Hispanic | 5.7% | 0.47 (0.34–0.66) |
| Other | 6.0% | 0.61 (0.44–0.87) |
| Gender | ||
| Male (Ref.) | 6.0% | |
| Female | 6.6% | 1.18 (0.81–1.70) |
| Firearm Type | ||
| Air Gun (Ref.) | 0.1% | |
| Handgun | 7.5% | 34.60 (4.48–267.24) |
| Other | 6.8% | 31.60 (4.11–242.94) |
| Rifle/Military Firearm | 3.1% | 18.41 (2.02–167.68) |
| Shotgun | 3.2% | 20.20 (2.37–172.14) |
| Payer Source | ||
| Medicare/Medicaid (Ref.) | 5.1% | |
| Self-pay + Other | 8.7% | 1.46 (1.13–1.90) |
| Private | 6.4% | 1.05 (0.80–1.37) |
| Median Household Income | ||
| Quartile 1 (Ref.) | 6.2% | |
| Quartile 2 | 6.3% | 1.02 (0.79–1.32) |
| Quartile 3 | 5.3% | 0.87 (0.64–1.17) |
| Quartile 4 | 6.4% | 1.02 (0.63–1.65) |
| Admission Day | ||
| Weekday (Ref.) | 6.3% | |
| Weekend | 5.8% | 0.84 (0.68–1.04) |
| Severity of Illness by APRDRG | ||
| 1 (Ref.) | 0.4% | |
| 2 | 2.2% | 9.72 (4.83–19.55) |
| 3 | 10.6% | 98.07 (48.07–200.07) |
| 4 (Ref.) | 19.8% | 591.30 (280.62–999.99) |
| Hospital Bed Size | ||
| Small (Ref.) | 4.8% | |
| Medium | 5.4% | 0.89 (0.54–1.49) |
| Large | 6.4% | 0.88 (0.526–1.45) |
| Hospital Teaching Status | ||
| Urban Non-teaching (Ref.) | 5.8% | |
| Urban Teaching | 6.3% | 1.22 (0.90–1.65) |
| Rural | 0.6% | 0.05 (0.01–0.22) |
| Hospital Region | ||
| South (Ref.) | 6.3% | |
| Northeast | 5.4% | 0.99 (0.69–1.44) |
| West | 5.9% | 0.83 (0.61–1.12) |
| Midwest | 6.4% | 0.83 (0.60–1.13) |
| Children’s Hospital | ||
| No (Ref.) | 6.3% | |
| Yes | 3.3% | 0.72 (0.38–1.38) |
2.4. Treatment cost analysis
The total treatment cost of all pediatric firearm injuries in 2006, 2009, and 2012 was $261,144,691 with a median treatment cost per admission of $10,159 (interquartile range: $5,071 to $20,565). Table 3 reports linear regression results for total cost. No difference was observed among White, Black, and Hispanic children for total cost. Compared to Air gun injuries, all weapon types resulted in significantly more hospitalization cost, although Shotgun did not reach statistical significance (Table 3). Self-pay patients had lower hospitalization cost than patients with Medicaid/Medicare healthcare coverage (−$1,646.85, p = 0.02). Severity of illness was a major influencer of treatment costs. Compared to the cost of a child with a Mild loss of function APR-DRG severity of illness, all other severities had significantly higher treatment costs (Moderate = $1,381.75, p < 0.01; Major = $4,098.92, p = 0.004; and Extreme = $14,729.84, p < 0.0001).
Table 3.
Treatment cost analysis (measured in USD)
| Characteristics | Regression Coefficient | Standard Error | P Value |
|---|---|---|---|
| Age | |||
| 0–4 (Ref.) | |||
| 5–9 | −860.35 | 1,695.56 | 0.61 |
| 10–14 | 1,146.99 | 1,356.73 | 0.40 |
| 15–18 | 877.53 | 1,244.78 | 0.48 |
| Race | |||
| White (Ref.) | White (Ref.) | ||
| Black | −336.72 | 723.91 | 0.64 |
| Hispanic | −1,228.28 | 965.68 | 0.20 |
| Other | −1,669.41 | 738.75 | 0.02 |
| Gender | |||
| Male (ref.) | |||
| Female | −256.79 | 710.93 | 0.72 |
| Firearm Type | |||
| Air Gun (Ref.) | |||
| Handgun | 1,764.10 | 807.35 | 0.03 |
| Other | 2,012.78 | 741.13 | 0.0007 |
| Rifle/Military Firearm | 4,101.73 | 1,958.57 | 0.04 |
| Shotgun | 1,117.10 | 1,352.86 | 0.41 |
| Payer Source | |||
| Medicare/Medicaid (Ref.) | |||
| Self-pay + Other | −1646.85 | 700.66 | 0.019 |
| Private | −930.68 | 694.72 | 0.18 |
| Median Household Income | |||
| Quartile 1 (Ref.) | |||
| Quartile 2 | −322.52 | 580.62 | 0.58 |
| Quartile 3 | 148.01 | 760.43 | 0.85 |
| Quartile 4 | −913.49 | 968.51 | 0.35 |
| Admission Day | |||
| Weekday (Ref.) | |||
| Weekend | 227.73 | 500.18 | 0.66 |
| Severity of Illness by APRDRG | |||
| 1 (Ref.) | |||
| 2 | 1,381.75 | 553.42 | 0.01 |
| 3 | 4,098.92 | 1,421.83 | 0.004 |
| 4 | 14,729.84 | 2,683.04 | <0.0001 |
| Hospital Bed Size | |||
| Small (Ref.) | |||
| Medium | −445.71 | 1,625.04 | 0.78 |
| Large | 1,327.22 | 1,538.31 | 0.39 |
| Hospital Teaching Status | |||
| Urban Non-teaching (Ref.) | |||
| Rural | 807.67 | 1,038.82 | 0.44 |
| Urban Teaching | 1,420.25 | 924.90 | 0.12 |
| Hospital Region | |||
| South (Ref.) | |||
| Northeast | 7,577.08 | 2,683.11 | 0.005 |
| Midwest | 1,820.45 | 930.017 | 0.05 |
| West | 8,480.82 | 1,046.32 | <0.0001 |
| Children’s Hospital | |||
| No (Ref.) | |||
| Yes | 9,462.14 | 2,282.74 | <0.0001 |
Hospital location and Children’s hospital status also significantly impacted treatment costs, when controlled for all other variables. Hospitals in the South were significantly less expensive than hospitals in any other region (West: $8,480.82, p < 0.0001; Northeast: $7,577.08, p = 0.005; Midwest $1,820.45, p = 0.05). Additionally, care at Children’s hospitals was significantly more expensive than care at Non-children’s hospitals ($9,462.14, p < 0.0001). The median cost for a firearm injury at a Children’s hospital was $11,144 (interquartile range: $5,251 to $25,041).
2.5. LOS analysis
The total LOS for all pediatric firearm injuries in 2006, 2009, and 2012 was 77,253 days with a median LOS of 2.55 days (interquartile range: 0.81 days −5.95 days). When controlling for all variables, all gun injuries were associated with a significantly longer LOS than the referent air gun (Table 4). Children with Medicaid/Medicare coverage spent a significantly longer amount of time in the hospital than those with Self-pay (−1.28 days, p < 0.0001) and those with Private healthcare (−0.47 days, p = 0.05, respectively). Similar to mortality and cost, APR-DRG severity had the most important influence on LOS. Compared to children with an APR-DRG severity for Mild loss of function, those with more severe injuries were hospitalized longer (Moderate = 1.86 days, p < 0.0001; Major = 4.99, p < 0.0001; Extreme = 12.09 days, p < 0.0001).
Table 4.
LOS analysis (measured in hospital days)
| Characteristics | Regression Coefficient | Standard Error | P Value |
|---|---|---|---|
| Age | |||
| 0–4 (Ref.) | |||
| 5–9 | −0.16 | 0.75 | 0.83 |
| 10–14 | −0.66 | 0.63 | 0.30 |
| 15–18 | −0.40 | 0.65 | 0.53 |
| Race | |||
| White (Ref.) | |||
| Black | −0.10 | 0.28 | 0.71 |
| Hispanic | −0.19 | 0.33 | 0.57 |
| Other | −0.41 | 0.29 | 0.15 |
| Gender | |||
| Male (ref). | |||
| Female | 0.17 | 0.30 | 0.58 |
| Firearm Type | |||
| Air Gun (Ref.) | |||
| Handgun | 0.92 | 0.30 | 0.002 |
| Other | 1.08 | 0.26 | <0.0001 |
| Rifle/Military Firearm | 2.75 | 0.64 | <0.0001 |
| Shotgun | 2.54 | 0.34 | <0.0001 |
| Payer Source | |||
| Medicare/Medicaid (Ref.) | |||
| Self-pay + Other | −1.28 | 0.24 | <0.0001 |
| Private | −0.47 | 0.23 | 0.05 |
| Median Household Income | |||
| Quartile 1 (Ref.) | |||
| Quartile 2 | 0.06 | 0.21 | 0.77 |
| Quartile 3 | −0.01 | 0.23 | 0.97 |
| Quartile 4 | 0.21 | 0.33 | 0.51 |
| Admission Day | |||
| Weekday (Ref.) | |||
| Weekend | −0.12 | 0.21 | 0.58 |
| Severity of Illness by APRDRG | |||
| 1 (Ref.) | |||
| 2 | 1.86 | 0.10 | <0.0001 |
| 3 | 4.99 | 0.22 | <0.0001 |
| 4 | 12.09 | 0.53 | <0.0001 |
| Hospital Bed Size | |||
| Small (Ref.) | |||
| Medium | 1.53 | 0.55 | 0.0005 |
| Large | 1.37 | 0.43 | 0.0013 |
| Hospital Teaching Status | |||
| Urban Non-teaching (Ref.) | |||
| Rural | −0.40 | 0.33 | 0.23 |
| Urban Teaching | 0.56 | 0.23 | 0.02 |
| Hospital Region | |||
| South (Ref.) | |||
| Northeast | −0.24 | 0.38 | 0.53 |
| Midwest | −0.98 | 0.32 | 0.002 |
| West | −0.04 | 0.34 | 0.91 |
| Children’s Hospital | |||
| No (Ref.) | |||
| Yes | 2.57 | 0.91 | 0.005 |
Hospital bed size, Teaching status, Location, and Children’s hospital status all significantly impacted LOS after controlling for all other variables. Medium and Large hospitals had significantly longer LOS than Small hospitals (1.53 days, p = 0.0005; 1.37 days, p = 0.0013, respectively). When compared to Urban non-teaching hospitals, Urban teaching hospitals minimized hospitalization days for pediatric injury victims (0.56 days, p = 0.020). Midwest hospitals had significantly shorter LOS than hospitals in the South (−0.98, p = 0.002). Finally, Children’s hospitals had significantly longer LOS than Non-children’s hospitals (2.57 days, p = 0.005).
3. DISCUSSION
Firearm injuries result in significant morbidity and mortality within the pediatric population and remain a public health concern. Our data revealed that approximately 14 children per day aged 0–18 were hospitalized for a firearm injury. We report five key findings that complement the literature focused on pediatric firearm injuries. First, gender was not a predictive factor for inpatient mortality. Second, the APR-DRG severity of illness variable was an accurate predictor of mortality, LOS, and costs. Third, when all factors are held constant, White patients are less likely to survive than other racial and ethnic groups. Fourth, hospital characteristics, such as teaching status, bed size, and children hospital status, are important for assessing survival and cost differences for firearm injuries in children. Lastly, the substantial burden on health care systems resulted in more than 75,000 hospital days and more than a quarter of a billion dollars for direct hospital costs.
As demonstrated in prior studies focused on pediatric firearm injuries [9, 12, 18–22], we also observed a similar pattern of firearm violence in that the larger burden of injuries lie with male victims (89%), older adolescents (15–18 years of age), racial minority groups, those living at or below 150% of the poverty line (52%), and patients insured by Medicaid/Medicare. Additionally, similar to Leventhal et al. [21], our study showed that Black children and adolescents accounted for the majority of hospitalizations for each age group regardless of gender; although, males had a higher incidence in each age cohort. However, on regression analysis, we found that gender was not a predictive variable of inpatient mortality. Though other studies have commented on the gender discrepancy in pediatric firearm injuries [9, 15, 21], ours is the first study to demonstrate that gender may not play a significant role in mortality using regression analysis. In addition, there were no significant differences between costs or LOS; possibly indicating that gender alone does not influence these variables. Moreover, there may be other variables that could influence these outcomes, but were not measured in our study. Hence, these findings are important because it enhances our understanding into the relationship and directionality between firearm injury and gender, specifically, as it relates to inpatient mortality, costs, and LOS in the pediatric population. Therefore, severity of illness and age of the victims may be as relevant as gender for injuries that result in hospitalization.
APR-DRG severity of illness is a tool utilized to help appropriately categorize patients based on their admission diagnosis, severity of their disease processes, and risk of mortality. This system was primarily designed to quantify resource consumption using patient features. Among all outcome variables, there was a difference between APR-DRG severity of illness ranging from moderate to extreme and the referent APR-DRG severity of illness for mild loss of function. The highest severity class (extreme loss of function) was more likely to result in higher costs, longer LOS, and inpatient mortality. Our study is the first to look at the predictive quality of APR-DRG classification in firearm injuries in the adult or pediatric population. It provides the baseline knowledge and reveals the importance of APR-DRG as measurement of resource consumption among pediatric firearm injury victims, which has the potential to be clinically important. Assessment of the APR-DRG components in future studies will aid in better understanding this finding. Several other studies available have analyzed APR-DRG, but only in the context of its ability to capture and stratify trauma cases in comparison to other methods, such as a trauma registry and other severity classification systems [23, 24]. Therefore, we propose APR-DRG as a potential marker for the identification of injury severity and resource consumption in future pediatric violence studies.
Prior studies have highlighted that unintentional injuries have accounted for the majority of pediatric firearm injuries [15, 18]. Our study differs in that intentional firearm injuries, such as assault and suicide, are disproportionally responsible for hospitalization and mortality when compared to unintentional injuries. In our dataset, the majority of hospitalizations were secondary to assault, which is consistent with other studies [14]. Despite this, we found, suicide was much more likely to result in inpatient mortality than assault or unintentional injury. This is corroborated with recent national suicide data demonstrating an upward trend among children and adolescents aged 10–14 years old, with the majority of patients identified as White victims [11]. Correspondingly, our study demonstrated a similar finding among patients aged 10–14 years old who had the highest mortality rate (6.4%) among firearm victims. These findings may explain the increased rate of death among White firearm victims in our analysis.
Further, White victims were more likely to die during admission than Black and Non-white Hispanic victims. To the authors’ knowledge, these findings are novel to this study. However, this association was not demonstrated between races for LOS or costs. We believe this is important because race has long been documented as a risk factor for firearm injury intent; assaults were more common among minorities and suicide among nonminority victims. One study evaluating these injuries found that families with White children were more likely to employ unsafe gun storage practices than families with Black children [25]. Unintentional injuries are most commonly the result of a child playing with a firearm or presenting it to other children, resulting in accidental discharge of the weapon [2].Our study reveals that of all unintentional firearm discharges, Black children accounted for the majority of cases; however, when firearm intent was analyzed separately by race, unintentional firearm discharge accounted for the majority of firearm cases, not suicide, in White children and adolescents. Our finding is supported by Peek-Asa et al. [15], although their study included both children and adults analyzed by age. Interestingly, other KID database studies reported a higher percentage of suicide in comparison to unintentional injuries in White children and adolescents [14, 21]. Such findings could be largely attributable to cohort development; these studies used 0–20 years of age, whereas we primarily used 0–18 years of age based on trauma clinical experiences at stand-alone children hospitals. The authors believe that while suicide was not a leading cause of injury in our study, it remains a national priority that requires gender-specific interventions to prevent and curtail the injury and death rates [26]. One method to begin this process comes from The Committee on Adolescence from the American Academy of Pediatrics, who identified screening methodology for risk factors during care visits using validated questionnaires [27].
When analyzing by weapon type, the predominate firearm type was Other, which likely reflects the lack of information at the time of injury regarding the actual firearm used. Further, there was a significant difference for inpatient mortality for all gun types when compared to air gun. However, it is important to highlight that, while viewed as a “toy,” air guns have been documented to result in both severe injury and hospitalizations [28–30]. Our study further demonstrates that firearm type was a good predictor of mortality, LOS, and cost.
Our cost analysis showed pediatric firearm injuries resulted in an “excess” of 75,000 hospital days and more than a quarter of a billion dollars ($261 million) for hospital services. In addition, we found that most hospitalizations occurred in large-bed hospitals (72%) and at hospitals designated as urban teaching hospitals (83%). This was in concordance with another study analyzing ED visits secondary to firearm injury in which the majority of patients were treated at an urban teaching hospital [18]. Hospitals geographically designated as rural centers had a statistically significant lower mortality compared to larger urban non-teaching hospitals. LOS stay was also less at rural hospitals but did not reach statistical significance. These findings may suggest that less severe injuries were more likely to be treated at rural and smaller hospitals; however, our data does not definitively support this supposition.
In addition to where a hospital was located, further delineation between adult and children hospitals made a difference. Overall, more children were treated at adult hospitals. While the mortality percentages differed between Children’s and Adult hospitals, this did not reach statistical significance. Another study focused on the outcomes of children and adult centers after gun injuries had the same result as our study—there was a trend toward a lower mortality in pediatric centers but no real statistical difference was appreciated [31]. Miyata et al. further demonstrated that, although mortality was no different, functionality was better for those injured patients when treated at pediatric trauma centers. Improved functionality, although unable to specifically be analyzed within our dataset, may explain and support our findings, which demonstrated that care at a children’s hospital was more expensive and the LOS was longer. Thus, the pediatric specialty care of these institutions may possibly explain these differences.
Our study, as have others, has demonstrated that the majority of victims in pediatric firearm injuries are from low-income communities and that those insured by Medicaid represent the major source of reimbursement at the provider and hospital levels [32, 33]. By advocating for violence preventative programs and resources, using social capital within and external of these communities, preventable firearm violence may be eliminated. Surgeons have recently demonstrated that stronger state-level child access prevention (CAP) laws resulted in a reduction in pediatric firearm injuries compared to states with weaker CAP laws [34]. Additionally, surgeons are encouraging healthcare providers to accept the professional and moral obligation to appropriately respond with preventative measures aimed at firearm violence burdening our trauma systems [35]. To this end, members of the Society of Black Academic Surgeons have also responded with a recently published literature review on the impact of gun violence in the Black community, as well as recommendations to improve these conditions [36]. Several other surgical societies including the American College of Surgeons, the American Pediatric Surgical Association, the Pediatric Trauma Society, and the American Academy of Pediatrics have also published firearm safety position statements and recommendations [37–41]. Additionally, hospital-based violence intervention programs have also been implemented across the nation. A recent study from the University of California San Francisco reported longterm recidivism reduction among trauma victims, most of who were from high-risk communities [42]. And as a final point, community-based programs, such as the Safe Streets program based on the Cure Violence model in Baltimore, has reported an improvement in attitudes toward violence intervention programs in the community, as well as a reduction in nonfatal firearm injuries among high-risk adolescents and young adults [43–45]. Therefore, given the findings herein and the emerging data supporting the ability of community-based programs to mitigate firearm violence risk, targeted approaches toward the highest-risk groups and communities may result in significant risk reduction in vulnerable populations.
The study has several limitations. Primarily, the study’s retrospective design was a limitation that prevents our ability to determine a cause-effect relationship. Further, only hospitalized patients and those accurately coded for firearm injuries were assessed. Thus, we are unable to capture ED visits, outpatient visits, or pre-hospital deaths as a result of firearm injuries. Additionally, the HCUP-KID is an administrative database and differs from other national datasets, such as the National Trauma Database, which primarily is derived from patient clinical information. Moreover, the HCUP-KID has inherent limitations, such as coding inaccuracies that may result in sampling biases. Further, the individual components of the APR-DRG classification system are not available within HCUP KID. Further, our results present a unique perspective to advance the understanding of firearm injury in the pediatric population.
4. CONCLUSION
Pediatric firearm injuries continue to be a major source of economic and public health hardship. Therefore, it is important to identify predictors that identify potential areas of intervention within the hospital setting. Our findings further elucidate predictors of inpatient mortality, LOS, and direct hospital costs. Ultimately, focusing on preventative measures, the severity of illness, and treatment locations may improve overall outcomes.
FUNDING
BDH is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (T32DK007639). KBJ is supported by a research career development award (K12HD052023: Building Interdisciplinary Research Careers in Women’s Health Program-BIRCWH; Berenson, PI) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) at the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
ABBREVIATIONS
- ED
Emergency department
- LOS
Length of stay
- KID
Kids’ Inpatient Database
- HCUP
Healthcare Cost and Utilization Project
- AHRQ
Agency for Healthcare Research and Quality
- APR-DRG
All-Patient Refined Diagnosis-Related Group
- CDC
Centers for Disease Control and Prevention
- AHA
American Hospital Association
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: Presented at the 5th Annual Pediatric Trauma Society in Houston, TX, November 8-10, 2018.
CONFLICT OF INTEREST
The authors do not have any conflicts of interests to declare.
REFERENCES
- [1].Grinshteyn E, Hemenway D. Violent Death Rates: The US Compared with Other Highincome OECD Countries, 2010. Am J Med 2016;129(3):266–73. [DOI] [PubMed] [Google Scholar]
- [2].Finkelhor D, Turner HA, Shattuck A, Hamby SL. Prevalence of Childhood Exposure to Violence, Crime, and Abuse: Results From the National Survey of Children’s Exposure to Violence. JAMA Pediatr 2015;169(8):746–54. [DOI] [PubMed] [Google Scholar]
- [3].DiScala C, Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics 2004;113(5):1306–12. [DOI] [PubMed] [Google Scholar]
- [4].Kellermann AL, Rivara FP. Silencing the science on gun research. Jama 2013;309(6):549–50. [DOI] [PubMed] [Google Scholar]
- [5].Allareddy V, Nalliah RP, Rampa S, Kim MK. Firearm related injuries amongst children: estimates from the nationwide emergency department sample. Injury 2012;43(12):2051–4. [DOI] [PubMed] [Google Scholar]
- [6].Powell EC, Jovtis E, Tanz RR. Incidence and circumstances of nonfatal firearm-related injuries among children and adolescents. Arch Pediatr Adolesc Med 2001;155(12):1364–8. [DOI] [PubMed] [Google Scholar]
- [7].Hemenway D The public health approach to motor vehicles, tobacco, and alcohol, with applications to firearms policy. J Public Health Policy 2001;22(4):381–402. [PubMed] [Google Scholar]
- [8].Eber GB, Annest JL, Mercy JA, Ryan GW. Nonfatal and fatal firearm-related injuries among children aged 14 years and younger: United States, 1993–2000. Pediatrics 2004;113(6):1686–92. [DOI] [PubMed] [Google Scholar]
- [9].Fowler KA, Dahlberg LL, Haileyesus T, Gutierrez C, Bacon S. Childhood Firearm Injuries in the United States. Pediatrics 2017;140(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cunningham RM, Walton MA, Carter PM. The Major Causes of Death in Children and Adolescents in the United States. N Engl J Med 2018;379(25):2468–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999–2014. NCHS Data Brief 2016(241):1–8. [PubMed] [Google Scholar]
- [12].Spitzer SA, Staudenmayer KL, Tennakoon L, Spain DA, Weiser TG. Costs and Financial Burden of Initial Hospitalizations for Firearm Injuries in the United States, 2006–2014. Am J Public Health 2017;107(5):770–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gani F, Makary MA, Wick EC, Efron JE, Fang SH, Safar B, et al. Bundled Payments for Surgical Colectomy Among Medicare Enrollees: Potential Savings vs the Need for Further Reform. JAMA Surg 2016;151(5):e160202. [DOI] [PubMed] [Google Scholar]
- [14].Lee J, Moriarty KP, Tashjian DB, Patterson LA. Guns and states: pediatric firearm injury. J Trauma Acute Care Surg 2013;75(1):50–3; discussion 3. [DOI] [PubMed] [Google Scholar]
- [15].Peek-Asa C, Butcher B, Cavanaugh JE. Cost of hospitalization for firearm injuries by firearm type, intent, and payer in the United States. Inj Epidemiol 2017;4(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Quality AfHRa. Overview of the Kids’ Inpatient Database (KID). 2018. [accessed August 1.2018].
- [17].Prevention CfDCa. Nonfatal Injury Data., 2018. [accessed August 3.2018].
- [18].Kalesan B, Dabic S, Vasan S, Stylianos S, Galea S. Racial/Ethnic Specific Trends in Pediatric Firearm-Related Hospitalizations in the United States, 1998–2011. Matern Child Health J 2016;20(5):1082–90. [DOI] [PubMed] [Google Scholar]
- [19].Parikh K, Silver A, Patel SJ, Iqbal SF, Goyal M. Pediatric Firearm-Related Injuries in the United States. Hosp Pediatr 2017;7(6):303–12. [DOI] [PubMed] [Google Scholar]
- [20].Senger C, Keijzer R, Smith G, Muensterer OJ. Pediatric firearm injuries: a 10-year single-center experience of 194 patients. J Pediatr Surg 2011;46(5):927–32. [DOI] [PubMed] [Google Scholar]
- [21].Leventhal JM, Gaither JR, Sege R. Hospitalizations due to firearm injuries in children and adolescents. Pediatrics 2014;133(2):219–25. [DOI] [PubMed] [Google Scholar]
- [22].Freeman JJ, Bachier-Rodriguez M, Staszak J, Feliz A. A comparison between nonpowder gun and powder-gun injuries in a young pediatric population. Injury 2017;48(9):1951–5. [DOI] [PubMed] [Google Scholar]
- [23].Hackworth J, Askegard-Giesmann J, Rouse T, Benneyworth B. The trauma registry compared to All Patient Refined Diagnosis Groups (APR-DRG). Injury 2017;48(5):1063–8. [DOI] [PubMed] [Google Scholar]
- [24].Rutledge R, Osler T. The ICD-9-based illness severity score: a new model that outperforms both DRG and APR-DRG as predictors of survival and resource utilization. J Trauma 1998;45(4):791–9. [DOI] [PubMed] [Google Scholar]
- [25].Schwebel DC, Lewis T, Simon TR, Elliott MN, Toomey SL, Tortolero SR, et al. Prevalence and Correlates of Firearm Ownership in the Homes of Fifth Graders: Birmingham, AL, Houston, TX, and Los Angeles, CA. Health Educ Behav 2014;41(3):299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in Suicide Among Youth Aged 10 to 19 Years in the United States, 1975 to 2016. JAMA Netw Open 2019;2(5):e193886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Shain B. Suicide and Suicide Attempts in Adolescents. Pediatrics 2016;138(1). [DOI] [PubMed] [Google Scholar]
- [28].Lee R, Fredrick D. Pediatric eye injuries due to nonpowder guns in the United States, 2002–2012. J aapos 2015;19(2):163–8.e1. [DOI] [PubMed] [Google Scholar]
- [29].Dandu KV, Carniol ET, Sanghvi S, Baredes S, Eloy JA. A 10-Year Analysis of Head and Neck Injuries Involving Nonpowder Firearms. Otolaryngol Head Neck Surg 2017;156(5):853–6. [DOI] [PubMed] [Google Scholar]
- [30].Veenstra M, Prasad J, Schaewe H, Donoghue L, Langenburg S. Nonpowder firearms cause significant pediatric injuries. J Trauma Acute Care Surg 2015;78(6):1138–42. [DOI] [PubMed] [Google Scholar]
- [31].Miyata S, Cho J, Lebedevskiy O, Matsushima K, Bae E, Bliss DW. Trauma experts versus pediatric experts: comparison of outcomes in pediatric penetrating injuries. J Surg Res 2017;208:173–9. [DOI] [PubMed] [Google Scholar]
- [32].Marcin JP, Schembri MS, He J, Romano PS. A population-based analysis of socioeconomic status and insurance status and their relationship with pediatric trauma hospitalization and mortality rates. Am J Public Health 2003;93(3):461–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kalesan B, Zuo Y, Xuan Z, Siegel MB, Fagan J, Branas C, et al. A multi-decade joinpoint analysis of firearm injury severity. Trauma Surg Acute Care Open 2018;3(1):e000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hamilton EC, Miller CC 3rd, Cox CS Jr., Lally KP, Austin MT. Variability of child access prevention laws and pediatric firearm injuries. J Trauma Acute Care Surg 2018;84(4):613–9. [DOI] [PubMed] [Google Scholar]
- [35].Scarlet S, Rogers SO Jr,. What Is the Institutional Duty of Trauma Systems to Respond to Gun Violence? AMA J Ethics 2018;20(5):483–91. [DOI] [PubMed] [Google Scholar]
- [36].Joseph K, Turner P, Barry L, Cooper C, Danner O, Enumah S, et al. Reducing the impact of violence on the health status of African-Americans: Literature review and recommendations from the Society of Black Academic Surgeons. Am J Surg 2018;216(3):393–400. [DOI] [PubMed] [Google Scholar]
- [37].Talley CL, Campbell BT, Jenkins DH, Barnes SL, Sidwell RA, Timmerman G, et al. Recommendations from the American College of Surgeons Committee on Trauma’s Firearm Strategy Team (FAST) Workgroup: Chicago Consensus I. J Am Coll Surg 2019;228(2):198–206. [DOI] [PubMed] [Google Scholar]
- [38].American Colleg eof Surgeons. Statement on Firearm Injuries, https://www.facs.org/about-acs/statements/12-firearm-injuries; 2013. [accessed December 23.2019].
- [39].Petty JK, Henry MCW, Nance ML, Ford HR. Firearm injuries and children: Position statement of the American Pediatric Surgical Association. J Pediatr Surg 2019;54(7):1269–76. [DOI] [PubMed] [Google Scholar]
- [40].Pediatric Trauma Society. PTS Position Statement on Gun Violence, https://pediatrictraumasociety.org/news/position-statements/Gun-Violence.cgi; 2018. [accessed December 23.2019].
- [41].Dowd MD, Sege RD. Firearm-related injuries affecting the pediatric population. Pediatrics 2012;130(5):e1416–23. [DOI] [PubMed] [Google Scholar]
- [42].Juillard C, Cooperman L, Allen I, Pirracchio R, Henderson T, Marquez R, et al. A decade of hospital-based violence intervention: Benefits and shortcomings. J Trauma Acute Care Surg 2016;81(6):1156–61. [DOI] [PubMed] [Google Scholar]
- [43].Milam AJ, Buggs SA, Furr-Holden CD, Leaf PJ, Bradshaw CP, Webster D. Changes in Attitudes toward Guns and Shootings following Implementation of the Baltimore Safe Streets Intervention. J Urban Health 2016;93(4):609–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Butts JA, Roman CG, Bostwick L, Porter JR. Cure violence: a public health model to reduce gun violence. Annu Rev Public Health 2015;36:39–53. [DOI] [PubMed] [Google Scholar]
- [45].Webster DW, Whitehill JM, Vernick JS, Curriero FC. Effects of Baltimore’s Safe Streets Program on gun violence: a replication of Chicago’s CeaseFire Program. J Urban Health 2013;90(1):27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]


