Abstract
Objective:
This study tested two family-based interventions designed for delivery in usual care: Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA), containing motivational interventions, homework management and schoolwork organization training, and family–school partnership building; and Medication Integration Protocol (MIP), containing ADHD psychoeducation, medication decision-making, and integrated medication management.
Method:
This study used a cluster randomized design to test CASH-AA + MIP versus CASH-AA Only for adolescents with ADHD in five sites. Therapists (N = 49) were site clinicians randomized to condition. Clients (N = 145) included 72% males; 42% White Non-Hispanic, 37% Hispanic American, 15% African American, and 6% more than one race; average age was 14.8 years. Fidelity data confirmed protocol adherence and between-condition differentiation.
Results:
One-year improvements were observed across conditions in several outcomes. Overall, CASH-AA + MIP produced greater declines in adolescent-report inattentive symptoms and delinquent acts. Similarly, among non-substance users, CASH-AA + MIP clients attended more treatment sessions. In contrast, among substance users, CASH-AA Only clients showed greater declines in caregiver-report hyperactive symptoms and externalizing.
Conclusions:
This study provides initial experimental support for family-based ADHD medication decision-making when coupled with academic training in usual care. The treatment protocols, CASH-AA and MIP, showed positive effects in addressing not only ADHD symptoms but also common co-occurring problems, and youth with substance use problems benefitted along with non-using peers.
Current Treatment Options for ADHD among Adolescents
Attention-Deficit/Hyperactivity Disorder (ADHD) is considered the most common behavioral disorder among adolescents. Recent prevalence data gathered by the National Survey of Children’s Health (Danielson et al., 2018) indicate that 12% of children aged 12–17 years have a current ADHD diagnosis. ADHD is even more prevalent among adolescents receiving behavioral care, affecting between 20-50% of those enrolled in outpatient mental health and substance use treatment (Turner, Muck, Muck, Stephens, & Sukumar, 2004) as well as those receiving behavioral services in nonspecialty settings such as schools, juvenile justice, and child welfare (Jones, Foster & Conduct Problems Prevention Research Group [CPPRG], 2009). And these may be conservative estimates given that ADHD is thought to be underdiagnosed in adolescent clinical populations (Sibley et al., 2012).
Adolescents with ADHD commonly present deficits in attention, behavioral and emotional regulation, self-organization, academic performance, and social competence that significantly impede the achievement of developmental and educational milestones (Chan, Fogler, & Hammerness, 2016). Currently, there are two options for treating ADHD in this age group that have strong empirical support. One is academic training, which includes organizational skills interventions for the adolescent as well as schoolwork management support for the adolescent and/or caregivers (Evans, Owens, Wymbs, & Ray, 2018). Academic training interventions are typically delivered in school settings, either during the academic year via in-school or afterschool programs (e.g., Evans et al., 2016; Langberg et al., 2018) or during summer programs (e.g., Sibley et al., 2018). School-based academic training has demonstrated robust impacts on functional academic outcomes (e.g., note-taking, homework completion) and organizational skills, along with small to moderate impacts on ADHD symptoms and co-occurring problems (Chan et al., 2016; Evans et al., 2018). However, clinic-based academic interventions are in short supply and have a limited evidence base (Ciesielski, Tamm, Vaughn, Cyran, & Epstein, 2019). One clinic-based model (Sibley et al., 2016) provides training in parenting skills, organization skills, homework management, and family problem-solving to youth and caregivers.
The second well-established treatment option for ADHD among adolescents is stimulant medication (American Academy of Pediatrics, 2014). Rapid-acting stimulants such as methylphenidate (e.g., Ritalin), and extended-release formulations such as osmotic-release oral system methylphenidate (OROS-MPH, i.e., Concerta), have proven consistently effective in reducing ADHD symptoms and improving functioning (Chan et al., 2016). Unfortunately, ADHD medications remain underutilized among eligible adolescents: Just over half of teens who may benefit from ADHD medications actually receive them, compared with more than two-thirds of younger children (Visser et al., 2014). There is also a huge gap in services for Hispanic and African American teens, who have significantly lower prescription rates than their White peers (Visser et al., 2014). Several client and provider factors contribute to ADHD medication underutilization among adolescents, especially in behavioral health settings. On the client side, caregivers much prefer behavioral interventions to medication as a primary treatment option (Daley et al., 2018; Smith, 2000). Also, compared to children, adolescents have increased sensitivity to medication stigma (Walker, Coleman, Lee, Squire, & Friesen, 2008), bigger misperceptions about or disregard for medication effects (Pelham et al., 2017), and less parental influence on their daily self-care (Smith, 2000). On the provider side, behavior therapists practicing in usual care rarely possess sufficient knowledge to inform and collaborate with families about choices of available ADHD medications and the risks and benefits of each (Yeh et al., 2014). Moreover, few reliable protocols exist to guide behavior therapists in integrating psychiatric services into treatment planning for teens.
Two Treatment Protocols Designed for Delivery in Outpatient Behavioral Care
Clinicians treating adolescents have few proven options for addressing ADHD as a primary or secondary treatment goal. This study investigated two innovative behavioral protocols designed to fill this resource gap. One is an academic training intervention intended for delivery by community clinicians: Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA; Hogue, Bobek, & Evans, 2016). CASH-AA is a family-based, clinically flexible protocol containing three modules derived from the robust literature on school-based academic training models: family motivational interventions around ADHD and academic performance, homework management and schoolwork organization training, and family–school partnership building. CASH-AA program components were adapted from three sources: (a) research-based family therapy interventions for engaging adolescents and their families in treatment and reframing problem behaviors (e.g., Diamond, Liddle, Hogue, & Dakof, 1999); (b) an empirically validated multimodal school-based program for adolescents with ADHD that targets impairment related to academic and organization skills (Evans et al., 2016); (c) evidence-based principles of family-school collaboration for youth with ADHD (e.g., Power et al., 2012).
The second protocol is an ADHD medication decision-making intervention, Medication Integration Protocol (MIP: Hogue, Bobek, Tau, & Levin, 2014). MIP is a family-based protocol that features psychoeducation about ADHD and ADHD medication, family-oriented medication decision-making, and integrated medication management. MIP is designed to educate families about the clinical and developmental implications of ADHD among adolescents; elucidate how a given teen’s specific ADHD-related characteristics impact their family, school, and peer functioning; increase opportunities for families to make informed decisions about ADHD medication acceptance; and support active family participation in medication regimens (Hogue et al., 2014). Family ADHD psychoeducation has shown positive effects on ADHD symptom reporting and prosocial functioning in youth (Ferrin et al., 2014). In addition, shared decision-making interventions are linked to improved treatment engagement and planning for youth disorders (Langer & Jensen-Doss, 2018), which in turn promote better outcomes. Broadly speaking, shared decision-making involves jointly deciding on a treatment plan that takes into account clients’ preferences, needs, and values along with provider knowledge and experience. For teens with ADHD in particular, medication selection is directly related to caregiver beliefs about the causes of behavior problems (Yeh et al., 2014). Also, beliefs about ADHD are mutable over time when families engage in shared decision-making with providers (Davis, Claudius, Palinkas, Wong, & Leslie, 2012). MIP pilot study results (Hogue, Lichvar, & Bobek, 2016) support its feasibility and positive impact on ADHD medication utilization (medication evaluation, acceptance, and duration) in routine care.
Main Study Contributions and Specific Aims
The current study examines the long-term impacts of academic training and medication decision-making interventions for adolescents with ADHD. It offers several contributions to the knowledge base for this population. It has practical implications for treatment planning: Families of youth with ADHD invariably prefer behavioral services only, but they need to know whether integrated medication interventions provide a meaningful boost to outcomes most important to them. It took place in existing behavioral health clinics to test protocol effectiveness when delivered by community therapists. It recruited a sample of adolescents with significant ADHD-related impairment, identified via research-administered diagnostic interviews or routine clinical assessment, for whom treating ADHD symptoms was a specific treatment goal. Racial/Ethnic minorities and girls with ADHD are both underserved and under-researched; this study targeted these populations and over half the sample was minority teens, and a quarter was female. Also, the study recruited a sizable subgroup of adolescent substance users, another underserved and high-priority risk group. ADHD and substance use are strongly linked across the adolescent developmental span, accounting for high comorbidity rates and complex clinical presentations (Hogue, Evans, & Levin, 2017). A widespread concern among clinicians and families alike is that ADHD stimulant medications will exacerbate substance use problems and/or create risk for misuse or diversion by substance-involved teens. However, the best available evidence shows consensus that prescribed ADHD medications do not present an additional risk for substance misuse or exacerbate substance use problems (Humphreys, Eng, & Lee, 2013). Moreover, there is evidence that ADHD medication can have additive benefits when combined with behavioral treatment for teens with both ADHD and substance use problems (e.g., Molina et al., 2013).
This study used a cluster randomized design to test CASH-AA + MIP versus CASH-AA Only in routine care for adolescents with ADHD. The main hypothesis was that CASH-AA + MIP would be superior to CASH-AA Only; that is, there would be significant benefits to adding medication decision-making to academic training. Between-condition differences were tested at one-year follow-up for multiple outcomes: behavior problems (ADHD symptoms, internalizing and externalizing problems, delinquency), school functioning (grades, homework problems), and service utilization (treatment attendance, ADHD medication use). Secondary analyses examined the moderating effects of baseline substance use on outcomes. Examination of within-group change across the full sample provided non-experimental evidence of academic training effects; it was not feasible in the community settings to include a no-intervention or waitlist control group.
Method
All activities were approved by the governing Institutional Review Board.
Trial Design
The trial had a cluster randomized longitudinal design. Randomization occurred at the Therapist level: Volunteer therapists at each site were randomly assigned to study condition. It was not possible to randomize also at the Client level because sites were not able to assign clients randomly to study therapists without disrupting routine client management. To enhance the probability of observing a meaningful experiment-wide dose of MIP, we weighted randomization to favor a 2-for-1 proportional assignment to the CASH-AA + MIP condition.
Participants
Therapists and Sites
The study enrolled therapists employed in one of five youth-serving sites: two community-based mental health clinics, one hospital-based youth mental health clinic, one community-based substance use clinic, and one community-based clinic co-licensed in mental health and substance use services. All full-time therapists and clinical trainees at each site who treated adolescent clients and who volunteered to participate were accepted into the study based on site report between 75% and 85% of therapists at each site volunteered, and this percentage did not vary across the site. Therapists at each site managed comparable caseloads, and each site prescribed weekly behavioral sessions and offered in-house psychiatric support.
Clients
All study clients were recruited from existing site referral streams or active caseloads of study therapists. Research staff contacted the primary caregiver of referred families by phone to administer an ADHD screening tool (Swanson, Nolan, & Pelham, 1992). Eligible families were immediately recruited to schedule a home-based baseline assessment. Caregivers and teens were interviewed separately. Caregiver assessments were administered in the preferred language: 81% English, 19% Spanish. Each family member received an honorarium in gift cards for completing the baseline assessment. Families were then scheduled for home-based follow-up assessments at 3, 6, and 12 months post-baseline. Assessors were unaware of the study condition.
Study inclusion criteria were (1) Adolescent age 12–18; (2) Primary caregiver able to participate in treatment; (3) Adolescent met DSM-5 (American Psychiatric Association, 2013) diagnostic criteria for ADHD at baseline (based on either caregiver or adolescent report), or, the assigned therapist reported that their clinical assessment of the adolescent revealed the presence of ADHD symptoms that were primary targets of treatment planning; (4) Adolescent was not enrolled in behavioral counseling at any other site; (5) Caregiver expressed desire, and adolescent expressed willingness, to participate in treatment; (6) Family had health benefits that met the requirements of the given sites (all sites accepted a broad range of insurance plans including Medicaid); (7) Family completed at least one intake interview at the site and was assigned to a study therapist. Exclusion criteria were intellectual disability or autism spectrum disorder; psychiatric or other medical illness requiring hospitalization; current psychotic symptoms; active suicidal ideation; severe substance use problems that require immediate relief (detox or residential placement). There were no eligibility criteria related to medication status: Youth were permitted to be either on or off medications of any kind at any time during the study.
Interventions
Both CASH-AA and MIP are clinically flexible protocols that do not prescribe a fixed number of sessions or intervention sequences. Both protocols were integrated into existing service delivery for study clients; existing services featured eclectic treatment practices across diverse treatment sites (described above), and ADHD was not a common focus of treatment planning for teens at any site. There were no standardized “pull out” sessions devoted exclusively to either protocol. Per routine clinic practices, there was no pre-specified number of overall treatment sessions or treatment duration for any client.
Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA)
CASH-AA is a three-module protocol that utilizes family and individual sessions to improve school performance (Hogue et al., 2016). Module 1: Motivation and Preparation engage adolescents as active participants in improving academic achievement, assesses home environment characteristics that support or impede school success, and determines family readiness to make changes in the home academic setting. Module 2: Behavior Change contains family-centered interventions designed to boost school attendance, collaboratively develops a homework management plan to increase the amount of distraction-free time spent nightly on school assignments, and helps teens create efficient systems for organizing school assignments and materials. Module 3: Family–School Partnership provides family education and advocacy training on school-based services and assists families in solidifying partnerships with in-school advocates to monitor education plans and academic progress.
Medication Integration Protocol (MIP)
MIP is a family-based protocol designed to integrate medication services into behavioral treatment planning for adolescents with ADHD (Hogue et al., 2014). Importantly, it is not designed to endorse medication use per se, but rather, promote client education about available medications and guide client-therapist collaborative inquiry about their potential therapeutic fit. MIP contains five modular tasks. ADHD Assessment & Medication Consult: Therapists help families understand the results of psychiatric evaluation. ADHD Psychoeducation & Client Acceptance: Therapists and families review ADHD educational materials to prompt interactive discussions about key ADHD-related behavioral and executive functioning issues, promote basic acceptance of ADHD-related characteristics and practical expectations for change, and complete checklists of ADHD-related characteristics and common impairments to generate each teen’s unique “ADHD profile.” ADHD Symptoms & Family Relations: Therapists address negative attributions about ADHD-related behavior by highlighting mislabeled causes (“relabeling”), redefine treatment referral issues as family problems with family solutions (“reframing”), and gauge family readiness for change. ADHD Medication & Family Decision-Making: Therapists educate families about potential benefits and side effects of ADHD medications, raise issues regarding stigma and medication misuse, and collaborate with families to process key factors that inform decisions about medication fit. Medication Management & Integration Planning: For families that initiate medication, therapists play a lead role in case coordination for medication management tailored to each family.
Fidelity Procedures and Evaluation
Throughout the study, two monthly fidelity consultation meetings were convened at each site. Consultation meetings were moderated by developers of the two protocols. To guard against crossover effects, one meeting was attended by CASH-AA Only therapists condition and a separate meeting by CASH-AA + MIP therapists. Meetings supported integration protocols into routine treatment planning for cases, focusing on adapting the timing, sequencing, and dosage of protocol components for individual clients.
Therapists completed brief post-session checklists for every study case to estimate the number of minutes spent discussing ADHD and ADHD medications and delivering interventions specified in the CASH-AA and MIP protocols. Research has shown that therapists can accurately self-report on minutes spent in session discussing protocol-based content (Hogue, Dauber, Lichvar, Bobek, & Henderson, 2015). Checklists were submitted for 99 of the 145 study cases (68%); there was no correlation between number of sessions attended and number of checklists submitted. A total of 1,042 checklists were submitted, averaging 10.5 per case (range = 1– 45). These data indicated that CASH-AA + MIP therapists (M = 18.0; SD = 19.2) spent more time focused on ADHD than CASH-AA Only therapists (M = 14.2; SD = 16.7; t = 3.15, p < .01). In contrast, CASH-AA + MIP therapists (M = 3.0; SD = 6.9) did not spend more time focused on ADHD medication issues than CASH-AA Only therapists (M = 2.3; SD = 4.9; t = 1.69, p = .09). As expected, CASH-AA + MIP therapists devoted more time delivering interventions associated with MIP (M = 2.0; SD = 6.8) than did CASH-AA Only therapists (M = 0.7; SD = 4.2; t = 2.53, p < .05); also as expected, the time they devoted to interventions associated with CASH-AA (M = 6.1; SD = 13.1) was equivalent to their counterparts (M = 6.5; SD = 10.1; t = 0.49, p = .63). In CASH-AA + MIP, 15% of sessions contained some MIP content, and these averaged 12.3 (SD = 12.5) minutes apiece; 26% contained some CASH-AA content, and these averaged 22.2 (SD = 16.5) minutes apiece. In CASH-AA, 49% of sessions contained some CASH-AA content, and these averaged 12.4 (SD = 10.9) minutes apiece.
Measures
Baseline Characteristics
The Comprehensive Addiction Severity Index for Adolescents (CASI-A; Meyers, McLellan, Jaeger, & Pettinati, 1995) is a semi-structured interview that collects information on high-risk adolescents and their families and also assesses risk factors in family relations, legal involvement, and substance use during the past 30 days. It has shown reliability and validity for teens receiving psychiatric or substance abuse treatment. The Mini-International Neuropsychiatric Interview (MINI Version 5.0; Sheehan et al., 1998) is a structured diagnostic interview validated in adult samples (e.g., Lecrubier et al., 1997) and previously used with adolescent samples (e.g., Hogue & Dauber, 2013); we updated the ADHD questions to match DSM-5 criteria. The MINI has demonstrated interrater and test-retest reliability on international samples of adult psychiatric and non-psychiatric patients and is designed to be administered by lay interviewers. An adolescent was categorized as “substance user” if they (1) met DSM-5 criteria for substance use disorder at baseline or (2) were enrolled in treatment at the substance use treatment site. Baseline SU data were used to dichotomize the sample in this manner to capture the clinically salient factor of being a “substance use case.” Of the 145 study cases, 46 (32%) were substance users (SU+) and the rest SU−.
Behavior Problems
To assess ADHD symptoms, two adolescent-report and two caregiver-report variables were calculated using data from the ADHD diagnostic scale of the MINI: total number of symptoms endorsed (out of 9) on the Inattentive/Disorganized (I/D) subscale, and total (out of 9) on the Hyperactive/Impulsive (H/I) subscale. Co-occurring behavior problems were measured with raw scores from the Child Behavior Checklist (caregiver report; Achenbach, 1991a) and Youth Self-Report (Achenbach, 1991b), which are parallel measures of youth behavior problems supported by extensive evidence of reliability, validity, and clinical utility. Each contains a summary scale of Externalizing (delinquent and aggressive) and Internalizing (anxious/depressed, withdrawn, somatic complaints) problems. Delinquency was assessed using the National Youth Survey Self-Report Delinquency Scale (Elliot, Ageton, Huizinga, Knowles, & Cantor, 1983), a well-validated self-report scale used to assess adolescent criminal behavior. Adolescents reported on the number of times they engaged in various overt and covert delinquent acts.
School Functioning
School grades were captured via adolescent report of class grades (i.e., all or mostly A’s; mostly A’s and B’s; etc.). Self-report of grade point average by teens is an often used and reasonably valid substitute for objective grade data (e.g., Crockett, Schulenberg, & Petersen, 1987). Homework problems were measured with the parent-report Homework Problems Checklist (Anesko, Schoiock, Ramirez, & Levine, 1987), which documents inattention/avoidance (e.g., complaining, messy homework) over the past 2 weeks.
Service Utilization
Treatment Attendance data were collected from the site clinical records. Medication use, coded as “on” or “off’ medication at baseline and at each follow-up timepoint, was captured with a module adapted from the CASI-A (described above).
Randomization
All consenting therapists at each site convened for a 90-minute on-site training in the CASH-AA protocol. At the end of the training, therapists were randomized to condition. Those randomized to CASH-AA + MIP were invited to attend a 90-minute on-site training in the MIP protocol. These training and randomization procedures were followed whenever new therapists were hired at each site. In a few instances, when the number of active therapists in a study condition at a given site dipped below three due to staff turnover, the next therapist to volunteer at that site was assigned directly to the low-member condition in order to maintain critical mass for fidelity consultation meetings. Of the 49 study therapists, less than 10% inherited group membership in this fashion; this proportion did not differ among sites.
Plan of Analysis
Analytic Strategy for Nesting Effects and Missing Data
In this study, clients were nested within therapists, and therapists nested within sites. We used the sandwich estimator to adjust parameter estimates and standard errors to account for clients nested in therapists (Asparouhov, 2005). This approach is used to analyze nested data when the goal is to examine outcomes at the individual level (i.e., client), and the hierarchical data structure (i.e., client nesting at therapist level) is akin to a nuisance factor to be accounted for, but inference about the degree of between-therapist variability is not of central concern. Because this study had only five sites, smaller than the 10–20 sites needed for stable estimates of random effects (Kreft & de Leeuw, 1998), we used the alternative of modeling site as a fixed effect included as a nuisance covariate in analyses. Because the site was not significant in any analyses, final results do not report it. Analyses used full information maximum likelihood estimation, which produces unbiased parameter estimates under the assumption that data are missing at random (MAR; Schafer & Graham, 2002). Although MAR cannot be directly evaluated, we examined the missingness mechanism via correlations between main study variables (see Table 1) and a binary variable representing missingness. All correlations were non-significant, favoring the MAR assumption.
Table 1.
Client demographics.
| Full Sample N = 145 |
|
|---|---|
| M (SD) or n (%) | |
| Adolescent age | 14.80 (1.95) |
| Adolescent race/ethnicity | |
| Black or African American | 22 (15%) |
| White | 61 (42%) |
| Hispanic | 53 (37%) |
| More than one race | 9 (6%) |
| Family composition | |
| Single parent | 74 (51%) |
| Two parents | 60 (41%) |
| Grandparent | 5 (3%) |
| Other | 6 (4%) |
| Caregiver post-high school education | 102 (70%) |
| Caregiver currently employed | 108 (75%) |
| Household income greater than $30K | 103 (74%) |
| Substance use case | 46 (32%) |
| DSM-V Diagnoses (from research interviews) | |
| ADHD | 111 (77%) |
| Oppositional defiant disorder | 94 (65%) |
| Conduct disorder | 45 (31%) |
| Substance use disorder | 34 (24%) |
| Generalized anxiety disorder | 35 (24%) |
| Major depressive disorder | 42 (29%) |
| Met criteria for more than one disorder | 112 (77%) |
| On ADHD medication at baseline | 61 (42%) |
Behavioral Outcomes
We used latent growth curve modeling (LGC; Duncan, Duncan, & Strycker, 2006) to examine the impact of treatment condition on change in main outcomes. Analyses used a 2 (condition) by 4 (time) repeated measures intent-to-treat design. First, we tested a series of growth curve models for each outcome, using chi-square difference tests of nested models to determine the overall shape of the individual change trajectories (linear or quadratic). Second, we tested unconditional models to obtain the average effect for change over time, without including treatment condition or other covariates; this provides the clearest test of full-sample time effects. Third, we added Condition (CASH-AA + MIP vs. CASH-AA Only) to the models to test its impact on initial status and change over time. These models controlled for covariates: sex (male vs. female); age (<15 years vs. 15+); race (non-Hispanic White vs. Other); baseline substance use (SU+ vs. SU−). Treatment effects for any given outcome were shown by a significant slope parameter, as tested by the pseudo z test – calculated by dividing the coefficient by its standard error – associated with Condition. For the one outcome that deviated substantially from normality (delinquency), we used two-part growth curve models (Brown, Catalano, Fleming, Haggerty, & Abbott, 2005), which allow for simultaneous estimation of separate but correlated continuous and categorical LGC models. In the categorical part, a binary indicator variable is created to indicate Any versus None of the given outcome; the continuous part models the frequency of occurrence of the outcome given any positive occurrence. Effect size estimates for significant Condition effects were calculated using Cohen’s d (Cohen, 1988) based on Feingold’s (2009) procedures for calculating effect sizes for LGC analyses; an effect size of d = .20 is considered small, d = .50 medium, and d = .80 large. To enhance interpretation of clinical meaningfulness (Evans et al., 2018), for all significant findings we also reported estimated mean differences between groups in the original scale using the following formula (Feingold, 2009): B(intercept) + B(linear slope)*3 + B(quadratic slope)*9. Only significant effects are reported; for cases in which the linear effect was not significant but the quadratic effect was, both models were tested although only quadratic effect statistics are reported.
We tested the moderating effects of substance use status as follows: First, we tested an LGC model per above including Condition, baseline SU status (SU+ vs. SU−), and their interaction. Note that Condition and SU status were grand mean centered prior to computing interaction terms. If the interaction was significant, post-hoc analyses examined condition effects within SU status subgroups; if not, the interaction term was removed to test for SU status main effects. For all analyses of behavioral outcomes, we relied on the results of the unconditional models to determine whether to include a quadratic effect. For models that included quadratic effects, if these effects were statistically significant (p < .05), we do not interpret the companion linear effects, as the interpretation of linear effects in the presence of significant quadratic effects is misleading. If the quadratic effect was not significant, we re-ran the model without the quadratic effect to test the linear effect.
Service Utilization
Linear regression was used to examine condition effects on treatment attendance, controlling for covariates per above. We examined condition effects on medication use in two ways. First, we used LGC as described above to examine whether clients in the CASH-AA + MIP condition were more likely to be on ADHD medication across the follow-up period. Second, we conducted a chi-square test to determine whether CASH-AA + MIP clients were more likely to start medication at some point during follow-up.
Results
Participant Flow
Study enrollment began in April 2015 and concluded in August 2018. The CONSORT diagram (Figure 1) depicts therapist and client flow into the study and interview completion rates. Of the 82 therapists who were randomized across the five sites, 49 (60%) were assigned a study case. There were no differences between therapists who were assigned versus not assigned a study case on any demographic variable (sex, race/ethnicity, years of experience). Of the 257 families who participated in the initial phone screen, 58 (23%) were not invited to a baseline interview (45 did not meet ADHD screening eligibility, eight left the site before a baseline interview was completed, two moved out of state, and three for miscellaneous other reasons). In addition, 23 families (9%) refused to participate in the baseline after being screened eligible (caregivers feeling overwhelmed; caregivers and/or adolescents not having time to participate in follow-up interviews; caregivers not wanting ADHD to be a treatment focus). Of the 176 families who completed baseline, 31 (18%) did not meet eligibility criteria: 22 did not meet ADHD diagnostic criteria, three exhibited serious suicidal risk, two were assigned non-study therapists, and four for other reasons. This resulted in a final sample of 145 families. Follow-up interview rates were excellent: 94% at 3 months, 95% at 6 months, and 96% at 12 months (discounting 16 truncated cases yet to be interviewed at study termination). Of the 145 families enrolled, 143 (99%) completed at least one follow-up and thus were included in all outcome analyses. Follow-up completion rates did not differ between conditions at any timepoint.
Figure 1.
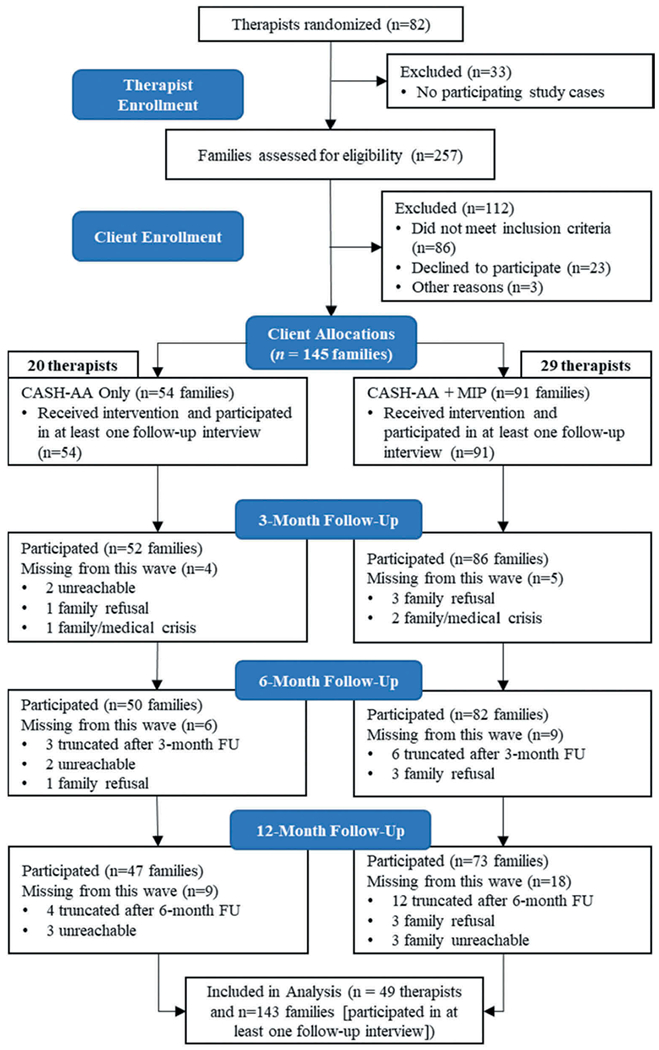
CONSORT diagram showing the number of therapists and clients enrolled.
Baseline Data
Therapist participants (N = 49:29 in CASH-AA + MIP, 20 in CASH-AA Only) included 82% females; 63% White Non-Hispanic, 29% Hispanic American, and 8% some other race/ethnicity. A total of 77% were full-time staff and the remaining were trainees; their average amount of postgraduate experience was 5.1 years. A total of 72% had a terminal Master’s-level degree, 10% Bachelor’s-level, 8% PhD-level, and 6% MD-level; 4% were unknown. There were no between-condition differences in therapist characteristics. Demographic and clinical characteristics of the client sample (N = 145:91 in CASH-AA + MIP, 54 in CASH-AA Only) are presented in Table 1 for the whole sample and separately by the condition. There were no significant differences between conditions on any of the measured demographic and clinical characteristics. Of note, only 77% of the sample met full diagnostic criteria for ADHD based on research-administered interviews; per the study eligibility criteria detailed above, the remaining 23% were enrolled in the study based on routine clinical assessment of ADHD symptoms during the initial stage of treatment and subsequent inclusion of ADHD-related intervention goals in client treatment plans. At treatment initiation 42% of adolescents had a current prescription for ADHD medication; 15% had a current prescription for anxiety or depression, and 4% for some other behavioral disorder.
Main Treatment Outcomes
Testing Shape of Change in the Full Sample
A significant linear decline was found for caregiver-report I/D [B(SE) = −.31(.07); pseudo-z = −4.23, p < .001]. Significant quadratic slopes were found for adolescent-report I/D [B(SE) = .21(.07); pseudo-z = 2.92, p = .003] and H/I [B(SE) = .21(.05); pseudo-z = 3.37, p = .001] and caregiver-report H/I [B(SE) = .13(.06); pseudo-z = 2.28, p = .023]; both results indicate an uptick in ADHD symptoms following the initial linear decline. A similar pattern of significant quadratic effects was found for adolescent-report internalizing [B(SE) = .56(.20); pseudo-z = 2.83, p = .005] and externalizing [B(SE) = .51 (. 18); pseudo-z = 2.84, p = .004]. Caregiver-report internalizing [B(SE) = −1.13(.31); pseudo-z = −3.65, p < .001] and externalizing [B(SE) = −.72 (.36); pseudo-z = −2.00, p = .045] showed significant linear declines. Significant linear improvement was also found in homework problems [B(SE) = −1.44(.29); pseudo-z = −5.04, p < .001]. There was no overall change in delinquency or school grades.
Treatment Effects: Behavioral Outcomes
As seen in Table 2, a significant condition effect was found on the quadratic slope for adolescent-report I/D [B(SE) = −.31(.14); pseudo-z = −2.24, p = .025, d = 1.17, estimated mean difference = −.66]. These results are graphed in Figure 2, which depicts that whereas both conditions showed initial declines in I/D symptoms, CASH-AA + MIP clients maintained improvement across follow-up, whereas CASH-AA Only clients evidenced a return toward elevated baseline levels. The effect size indicates this represents a large difference between groups; the estimated mean difference suggests that CASH-AA + MIP clients showed improvement that was about half-a-symptom better than CASH-AA Only clients. A significant condition effect on the linear slope was found for the continuous part of two-part delinquency growth model [B(SE) = −.20(.10); pseudo-z = −2.03, p = .042, d = .58, estimated mean difference = −.08]. That is, among adolescents who engaged in any delinquency, CASH-AA + MIP clients showed greater declines in delinquent acts than CASH-AA Only clients. The effect size indicates this was a moderate difference between groups.
Table 2.
Condition effects on outcomes controlling for baseline covariates (sex, age, race, baseline substance use).
| Intercept |
Linear Slope |
Quadratic Slope |
||||
|---|---|---|---|---|---|---|
| B(SE) [95% CI]a |
Pseudo-z | B(SE) [95% CI]a |
Pseudo-z | B(SE) [95% CI]a |
Pseudo-z | |
| ADHD Symptoms | ||||||
| Inattentive symptoms – AD report (Q) | −0.30 (0.39) | −0.77 | 0.81 (0.48) | 1.69 |
−0.31 (0.14)
[−0.59, −0.03] |
−2.24 * |
| Hyperactive symptoms – AD report (Q) | 0.55 (0.34) | 1.60 | 0.31 (0.39) | 0.79 | −0.14 (0.13) | −1.11 |
| Inattentive symptoms – CG report (L) | 0.14 (0.21) | 0.66 | 0.13 (0.14) | 0.94 | – | – |
| Hyperactive symptoms – CG report (Q) | 0.26 0(.43) | 0.62 | −0.14 (0.40) | −0.35 | 0.11 (0.14) | 0.78 |
| Comorbid Problems | ||||||
| Internalizing problems – AD report (Q) | −1.15 (1.44) | −0.80 | −0.44 (1.06) | −0.41 | 0.07 (0.36) | 0.21 |
| Externalizing problems – AD report (Q) | −0.87 (1.44) | −0.60 | −1.01 (1.22) | −0.83 | 0.39 (0.37) | 1.05 |
| Internalizing problems – CG report (L) |
−4.56 (1.94)
[−8.44, −0.68] |
−2.36 * | 0.50 (0.57) | 0.87 | – | – |
| Externalizing problems – CG report (L) | −0.23 (1.73) | −0.14 | 1.09 (0.58) | 1.87 | – | – |
| Delinquency-binary part (L) | 0.30 (0.51) | 0.58 | 0.12 (0.28) | 0.42 | – | – |
| Delinquency-continuous part (L) |
0.52 (0.20)
[0.12, 0.92] |
2.67 ** |
−0.20 (0.10)
[−0.40, 0.00] |
−2.03 * | – | – |
| School Functioning | ||||||
| School grades (L) | 0.26 (.32) | 0.80 | 0.03 (0.12) | 0.27 | – | – |
| Academic self-efficacy (L) | −0.10 (.14) | −0.66 | −0.01 (0.05) | −0.11 | – | – |
| Homework problems (L) | −0.81 (1.33) | −0.61 | 0.47 (0.54) | 0.87 | – | – |
| Minutes doing homework (L) | 2.50 (7.01) | 0.36 | 0.99 (2.26) | 0.44 | – | – |
| ADHD Medication | ||||||
| Medication use (L) | −1.31 (.85) | −1.54 | 0.28 (0.29) | 0.96 | – | – |
p < .05
p < .01.
95% confidence intervals are only shown where the effect of study condition was significant.
Figure 2.
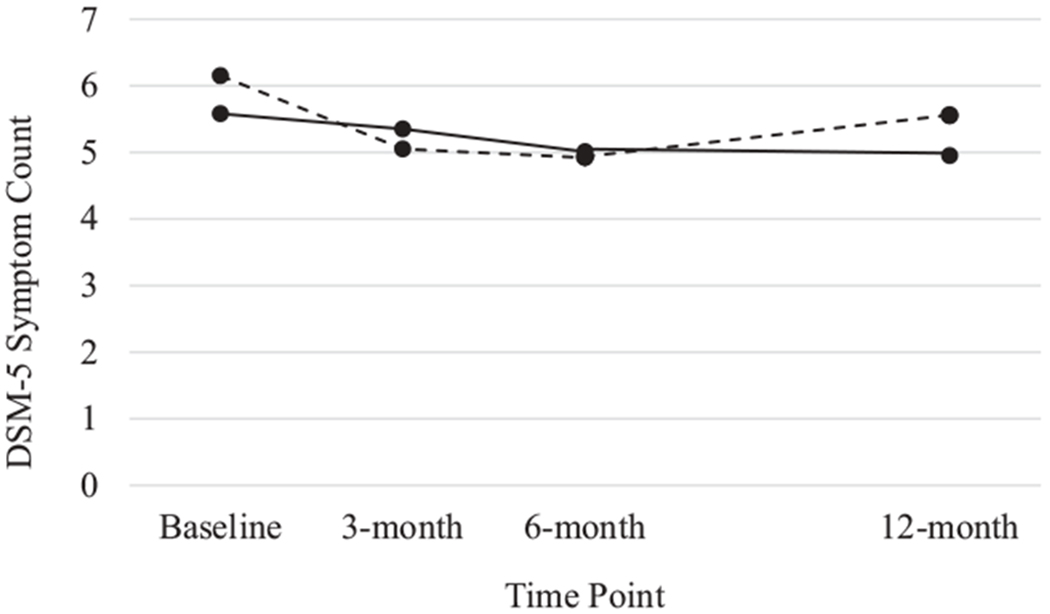
Quadratic treatment effects for adolescent-reported ADHD Inattentive/Disorganized symptoms. CASH-AA only clients are presented by the dotted line and CASH-AA + MIP clients are represented by the solid line.
Treatment Effects: Service Utilization
No significant effects were found for treatment attendance; the full sample attended an average of 20.5 (SD = 17.5) sessions. No significant effects were found for medication use (see Table 2). There were 84 adolescents not on ADHD medication at baseline (58% of the sample); of these, 24 (29%) initiated ADHD medication at some point during the follow-up period. Of those who initiated medication, 16 were in CASH-AA + MIP, representing 18% of adolescents assigned to this condition; and 8 were in CASH-AA Only, representing 15% assigned to this condition. There was no significant between-condition difference in the proportion of youth who initiated ADHD medication during the trial.
Subgroup Treatment Outcomes: Moderating Effects of Baseline Substance Use
Behavioral Outcomes
Significant interactions between baseline substance use and treatment condition were found for caregiver-report H/I (linear effect: [B(SE) = .46 (.20); 95% CI (.06, .86); pseudo-z = 2.30, p = .02]) and caregiver-report externalizing (linear effect: [B(SE) = 2.17(1.03); pseudo-z = 2.11, p = .034]). These interactions were probed by testing effects of Condition on outcome separately for SU− versus SU+ teens. Among substance users (n = 46), there were significant condition effects on caregiver-report H/I [linear effect: B(SE) = .52 (.46); 95% CI (−.40, 1.44), pseudo-z = 2.92, p = .004, d = .64, estimated mean difference = 1.6] and caregiver-report externalizing [linear effect: B(SE) = 2.17(.84), pseudo-z = 2.59, p = .010, d = .57, estimated mean difference = 9.3]. For both outcomes, CASH-AA Only clients showed greater problem declines with moderate effect sizes.
Service Utilization
There was a significant moderating effect of baseline substance use on treatment attendance [B(SE) = −17.7 (7.0); β = −2.54, p = .011]. Probing this interaction revealed a significant condition effect [B(SE) = 6.4 (2.9); β = 2.21, p = .027, d = .23], indicating that among non-substance users, CASH-AA + MIP clients attended more treatment sessions on average (M/SD = 19.4/14.3) than did CASH-AA Only clients (12.8/11.4).
Discussion
CASH-AA + MIP was superior to CASH-AA Only for ADHD-related and delinquency-related outcomes at one-year follow-up. CASH-AA + MIP showed greater declines in adolescent-report inattentive/disorganized symptoms that were large in magnitude. It was also superior in reducing delinquency: Among teenagers who engaged in any delinquent acts during follow-up, those who received CASH-AA + MIP showed greater decreases that were moderate in magnitude. There were no overall treatment effects on service utilization or ADHD medication use, but among non-substance users, CASH-AA + MIP clients attended more treatment sessions. In contrast, among substance users, CASH-AA Only showed larger decreases in caregiver-report hyperactive/impulsive symptoms and caregiver-report externalizing problems.
In line with evidence to date (Chan et al., 2016), study findings indicate the potential value of including medication decision-making along with academic skills training for youth with ADHD, including teens with drug use problems (Hogue et al., 2017). They also suggest that the MIP protocol itself had positive effects, with the caveat that MIP was tested in conjunction with academic training and not as a stand-alone intervention. Results supporting the value of the CASH-AA + MIP package are promising in light of the rigorous study design features: It was tested not against waitlist control or treatment-as-usual, but to a CASH-AA condition receiving identical levels of extramural training. Also, ecological validity was strong: Therapists were community clinicians operating with no changes to routine caseloads and the modest supplement of one or two 90-minute training workshops followed by one monthly hour-long consultation. Thus, the experiment set a high bar for CASH-AA + MIP to cross, and it did so with some success.
Analyses of client outcomes across both study conditions revealed improvements in multiple domains. Both adolescents and caregivers reported significant reductions in both dimensions of ADHD: inattention/disorganization and hyperactivity/impulsivity. Both sources also reported reductions in externalizing and internalizing problems, and caregivers noted a decline in homework problems. These clinical gains could be viewed as quasi-experimental support for the effectiveness of CASH-AA, the protocol common to both conditions. Other school-based (Evans et al., 2016; Langberg et al., 2018) and clinic-based (Sibley et al., 2016) studies of academic training have documented similar multidomain effects. CASH-AA by itself also proved superior to CASH-AA + MIP for some ADHD-related and externalizing problems among the small subgroup of substance-using youth. Further work on translating effective academic training protocols from school to clinic settings should be a top priority for youth ADHD intervention developers (Ciesielski et al., 2019).
Fidelity data produced mixed findings with regard to establishing adherence and differentiation for the two treatment conditions. In support of fidelity, CASH-AA + MIP therapists devoted more time delivering MIP interventions, and equivalent time delivering CASH-AA interventions, compared to CASH-AA therapists. CASH-AA + MIP therapists also spent more time focused on ADHD issues; however, they did not spend more time discussing ADHD medication per se. Generally speaking, clients in both conditions received a modest but meaningful dose of the clinically flexible, adjunctive protocols. Recent studies have found that even single-session interventions, when featuring psychoeducation aimed at correcting a specific maladaptive belief or behavior, can produce lasting change across the spectrum of youth problem type and severity (Schleider & Weisz, 2017). Future research might seek to increase the implementation dose of each protocol by prescribing that therapists utilize a series of “pull-out” sessions devoted exclusively to delivering protocol content.
Evidence supporting the two protocols’ theoretical mechanisms of change was also mixed. Both conditions featured the CASH-AA academic training protocol; there were cross-sample improvements in homework problems, but not in school grades. Contrary to hypotheses, CASH-AA + MIP did not boost ADHD medication use. Although it was reasonable to predict that introducing a medication education and decision-making protocol among adolescents in usual care – wherein ADHD is typically under-diagnosed and under-attended (Sibley et al., 2012) – would generate a bump in overall medication use, tempering factors include: (1) MIP is designed to promote client-centered medication decisions, not medication use itself; (2) 42% of the sample was on ADHD medication at baseline; and (3) 23% of the sample did not meet full diagnostic criteria for ADHD, a clinical prerequisite for initiating medication. That said, it is important to consider possible means by which CASH-AA + MIP produced observed treatment effects other than increasing medication uptake. As described above, MIP contains a family psychoeducation module that includes tool-guided instruction in ADHD symptoms, executive functioning issues, and stigma concerns; assessment of ADHD-related personality strengths and weaknesses; interventions aimed at diluting negative labels and boosting family motivation and expectations for change regarding ADHD-related problems; and attention to both caregiver and adolescent understanding of medication-related issues (see Schachter, Tharmalingam, & Kleinman, 2011). Any and all of these intervention foci may have contributed to the handful of superior clinical outcomes of CASH-AA + MIP. More research is needed on the complex decision-making calculus used by families when deliberating about ADHD medications (Davis et al., 2012). Overall, further research containing larger samples, and other key clinical subgroups, is needed to confirm and extend study findings regarding the validity and generalizability of main outcome, protocol fidelity, and mechanism of change effects.
Main Study Limitations
Because only three-fourths of the sample met full diagnostic criteria for ADHD, it is not known whether study results would be identical for samples in which every adolescent met full criteria; that said, arguably the full sample reflects those diagnostic characteristics for which clinicians practicing in usual care would deem MIP and CASH-AA suitable, as did the therapists participating in this study. All study outcomes were derived from self-report by adolescents and caregivers who were aware of their treatment condition status, which has been shown to impact research findings for behavioral interventions (Daley et al., 2018); however, families in both conditions were equally aware of receiving active treatment for the teen, and more specifically, active treatment for ADHD-related problems. The number of sites was too small to control for site nesting effects or to determine whether any site performed at a substantially higher or lower level than others. Participating therapists were self-selected and may not have fully represented all staff at a given site. In the absence of a no-treatment control group, the magnitude of research assessment effects on outcomes cannot be estimated, although such effects are presumed equally distributed across conditions. Although pharmacological studies often assess medication use via documentation of prescriptions filled and/or pill counts by physicians, these more rigorous assessment methods were beyond the resources of this study; we also did not employ more granular methods of self-report, such as medication diaries, that could have facilitated analysis of intervention effects on day-to-day medication adherence. Because analyses of moderating effects of baseline substance use involved small subgroups (e.g., CASH-AA Only contained n = 22 SU+ participants), those results should be interpreted with caution pending replication with larger numbers of substance-using and non-substance-using youth.
Clinical Implications
Increasing high-fidelity delivery of research-based behavioral interventions for ADHD is critical to improving quality care standards for adolescent behavioral health. This study provides initial experimental support for family-based ADHD medication decision-making when coupled with academic training in usual care. The treatment protocols, CASH-AA and MIP, showed positive effects in addressing not only ADHD symptoms but also common co-occurring problems, and youth with substance use problems benefitted along with non-using peers. Certainly study findings are preliminary, a first foray in testing the utility of these protocols in the hands of front-line clinicians. Nevertheless, results are promising, indicating that clinically flexible tools for addressing ADHD among teens can be successful in everyday treatment settings with diverse populations. Such tools are especially needed to buttress integrated healthcare models that foster a collaborative approach to combining behavioral and pharmacological interventions, and moreover, to empower behavior therapists to play a lead role in cultivating integrated services (Robiner, Tumlin, & Tompkins, 2013). Further validation and articulation of academic training and medication decision-making interventions in usual care will strengthen our capacity to support the clinical workforce in achieving the best outcomes for this prevalent and difficult-to-treat population.
Acknowledgments
The authors acknowledge the dedicated work of the research assessors on this project: Alison Bloomgarden, Kate Feiner, Cori Hammond, Alma Hidalgo, Naomi Krohner, Alexis Nager, Nkem Osian, and Christopher Tapia. We are grateful to the five outpatient treatment clinics that hosted this study and to the families who agreed to participate.
Funding
Preparation of this article was supported by the Patient-Centered Outcomes Research Institute [CER-1403-13704; PI: Hogue]. The trial is registered at ClinicalTrials.gov: registration number NCT02420990. The opinions expressed are those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Achenbach TM (1991a). Manual for the child behavior checklist/4-18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry. [Google Scholar]
- Achenbach TM (1991b). Manual for the youth self report and 1991 profile. Burlington: University of Vermont Department of Psychiatry. [Google Scholar]
- American Academy of Pediatrics. (2014). Attention-deficit/hyperactivity disorder and substance abuse. E. Harstad, S. Levy, and the committee on substance abuse. Pediatrics, 134, e293–e301. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Arlington, VA: American Psychiatric Pub. [Google Scholar]
- Anesko KM, Schoiock G, Ramirez R, & Levine FM (1987). The homework problem checklist: Assessing children’s homework difficulties. Behavioral Assessment, 9, 179–185. [Google Scholar]
- Asparouhov T (2005). Sampling weights in latent variable modeling. Structural Equation Modeling : A Multidisciplinary Journal, 12(3), 411–434. doi: 10.1207/s15328007sem1203_4 [DOI] [Google Scholar]
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, & Abbott RD (2005). Adolescent substance use outcomes in the raising healthy children project: A two-part latent growth curve analysis. Journal of Consulting and Clinical Psychology, 73, 699. doi: 10.1037/0022-006X.73.4.699 [DOI] [PubMed] [Google Scholar]
- Chan E, Fogler JM, & Hammerness PG (2016). Treatment of attention-deficit/hyperactivity disorder in adolescents: A systematic review. JAMA, 315, 1997–2008. doi: 10.1001/jama.2016.5453 [DOI] [PubMed] [Google Scholar]
- Ciesielski HA, Tamm L, Vaughn AJ, Cyran JE, & Epstein JN (2019). Academic skills groups for middle school children with ADHD in the outpatient mental health setting: An open trial. Journal of Attention Disorders, 23(4), 409–417. doi: 10.1177/1087054715584055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Mahwah, NJ: Erlbaum. [Google Scholar]
- Crockett LJ, Schulenberg JE, & Petersen AC (1987). Congruence between objective and self-report data in a sample of young adolescents. Journal of Adolescent Research, 2(4), 383–392. doi: 10.1177/074355488724006 [DOI] [Google Scholar]
- Daley D, Van Der Oord S, Ferrin M, Cortese S, Danckaerts M, Doepfner M, … Banaschewski T (2018). Practitioner review: Current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder. Journal of Child Psychology and Psychiatry, 59(9), 932–947. doi: 10.1111/jcpp.12825 [DOI] [PubMed] [Google Scholar]
- Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, & Blumberg SJ (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among US children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. doi: 10.1080/15374416.2017.1417860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CC, Claudius M, Palinkas LA, Wong JB, & Leslie LK (2012). Putting families in the center: Family perspectives on decision making and ADHD and implications for ADHD care. Journal of Attention Disorders, 8, 675–684. doi: 10.1177/1087054711413077 [DOI] [PubMed] [Google Scholar]
- Diamond GM, Liddle HA, Hogue A, & Dakof GA (1999). Alliance-building interventions with adolescents in family therapy: A process study. Psychotherapy: Theory, Research, Practice, & Training, 36, 355–368. doi: 10.1037/h0087729 [DOI] [Google Scholar]
- Duncan TE, Duncan SC, & Strycker LA (2006). An introduction to latent variable growth curve modeling: Concepts, issues, and applications. Mahwah, NJ: Erlbaum. [Google Scholar]
- Elliot DS, Ageton SS, Huizinga D, Knowles BA, & Cantor RJ (1983). The prevalence and incidence of delinquent behavior: 1976-1980 (The National Youth Survey Report No. 26). Boulder, CO: Behavioral Research Institute. [Google Scholar]
- Evans SW, Langberg JM, Schultz BK, Vaughn A, Altaye M, Marshall SA, & Zoromski AK (2016). Evaluation of a school-based treatment program for young adolescents with ADHD. Journal of Consulting and Clinical Psychology, 84, 15–30. doi: 10.1037/ccp0000057 [DOI] [PubMed] [Google Scholar]
- Evans SW, Owens JS, Wymbs BT, & Ray AR (2018). Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 47(2), 157–198. doi: 10.1080/15374416.2017.1390757 [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods, 14(1), 43. doi: 10.1037/a0014699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrin M, Moreno-Granados JM, Salcedo-Marin MD, Ruiz-Veguilla M, Perez-Ayala V, & Taylor E (2014). Evaluation of a psychoeducation programme for parents of children and adolescents with ADHD: Immediate and long-term effects using a blind randomized controlled trial. European Child & Adolescent Psychiatry, 23, 637–647. doi: 10.1007/s00787-013-0494-7 [DOI] [PubMed] [Google Scholar]
- Hogue A, Bobek M, & Evans SW (2016). Changing academic support in the home for adolescents with ADHD: A family-based clinical protocol for improving school performance. Cognitive and Behavioral Practice, 23, 14–30. doi: 10.1016/j.cbpra.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Bobek M, Tau GZ, & Levin FR (2014). Clinical strategies for integrating medication interventions into behavioral treatment for adolescent ADHD: The medication integration protocol. Child & Family Behavior Therapy, 36, 280–304. doi: 10.1080/07317107.2014.967631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, & Dauber S (2013). Diagnostic profiles among urban adolescents with unmet treatment needs: Comorbidity and perceived need for treatment. Journal of Emotional and Behavioral Disorders, 21, 18–32. doi: 10.1177/1063426611407500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Lichvar E, Bobek M, & Henderson CE (2015). Validity of therapist self-report ratings of fidelity to evidence-based practices for adolescent behavior problems: Correspondence between therapists and observers. Administration and Policy in Mental Health and Mental Health Services Research, 42, 229–243. doi: 10.1007/s10488-014-0548-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Evans SW, & Levin FR (2017). A clinician’s guide to co-occurring ADHD among adolescent substance users: Comorbidity, neurodevelopmental risk, and evidence-based treatment options. Journal of Child & Adolescent Substance Abuse, 26, 277–292. doi: 10.1080/1067828X.2017.1305930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Lichvar E, & Bobek M (2016). Pilot evaluation of the medication integration protocol for adolescents with ADHD in behavioral care: Treatment fidelity, acceptability, and utilization. Journal of Emotional and Behavioral Disorders, 24, 223–234. doi: 10.1177/1063426615611648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Eng T, & Lee SS (2013). Stimulant medication and substance use outcomes: A meta-analysis. JAMA Psychiatry (Chicago, Ill.), 70, 740–749. doi: 10.1001/jamapsychiatry.2013.1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DE, Foster EM & Conduct Problems Prevention Research Group. (2009). Service use patterns for adolescents with ADHD and comorbid conduct disorder. The Journal of Behavioral Health Services & Research, 36, 436–449. doi: 10.1007/s11414-008-9133-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreft I, & de Leeuw J (1998). Introducing multilevel modeling. Thousand Oaks, CA: Sage. [Google Scholar]
- Langberg JM, Dvorsky MR, Molitor SJ, Bourchtein E, Eddy LD, Smith ZR, … Eadeh HM (2018). Overcoming the research-to-practice gap: A randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. Journal of Consulting and Clinical Psychology, 86(1), 39. doi: 10.1037/ccp0000265 [DOI] [PubMed] [Google Scholar]
- Langer DA, & Jensen-Doss A (2018). Shared decision-making in youth mental health care: Using the evidence to plan treatments collaboratively. Journal of Clinical Child & Adolescent Psychology, 47(5), 821–831. doi: 10.1080/15374416.2016.1247358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, … Dunbar GC (1997). The mini international neuropsychiatric interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12 (5), 224–231. doi: 10.1016/S0924-9338(97)83296-8 [DOI] [Google Scholar]
- Meyers K, McLellan AT, Jaeger JL, & Pettinati HM (1995). The development of the comprehensive addiction severity index for adolescents (CASI-A): An interview for assessing multiple problems of adolescents. Journal of Substance Abuse Treatment, 12(3), 181–193. doi: 10.1016/0740-5472(95)00009-T [DOI] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Arnold LE, Swanson JM, Pelham WE, Hechtman L, … Hoza B (2013). Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child & Adolescent Psychiatry, 52(3), 250–263. doi: 10.1016/j.jaac.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE Jr., Gnagy EM, Sibley MH, Kipp HL, Smith BH, Evans SW, & Bukstein O (2017). Attributions and perception of methylphenidate effects in adolescents with ADHD. Journal of Attention Disorders, 21 (2), 129–136. doi: 10.1177/1087054713493320 [DOI] [PubMed] [Google Scholar]
- Power TJ, Mautone JA, Soffer SL, Clarke AT, Marshall SA, Blum NJ, … Jawad AF (2012). A family-school intervention for children with ADHD: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 80, 611–623. doi: 10.1037/a0028188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robiner WN, Tumlin TR, & Tompkins TL (2013). Psychologists and medications in the era of interprofessional care: Collaboration is less problematic and costly than prescribing. Clinical Psychology: Science and Practice, 20(4), 489–507. [Google Scholar]
- Schachter D, Tharmalingam S, & Kleinman I (2011). Informed consent and stimulant medication: Adolescents’ and parents’ ability to understand information about benefits and risks of stimulant medication for the treatment of attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 21(2), 139–148. doi: 10.1089/cap.2010.0037 [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham J (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. doi: 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 107–115. doi: 10.1016/j.jaac.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, … Dunbar GC (1998). The mini-international neuropsychiatric interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. [PubMed] [Google Scholar]
- Sibley MH, Coxe SJ, Campez M, Morley C, Olson S, Hidalgo-Gato N, … Pelham WE (2018). High vs low intensity summer treatment for ADHD delivered at secondary school transitions. Journal of Clinical Child & Adolescent Psychology, 47(2), 248–265. doi: 10.1080/15374416.2018.1426005 [DOI] [PubMed] [Google Scholar]
- Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, … Ward A (2016). Parent-teen behavior therapy + motivational interviewing for adolescents with ADHD. Journal of Consulting and Clinical Psychology, 84, 699–712. doi: 10.1037/ccp0000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Garefino AC, … Karch KM (2012). Diagnosing ADHD in adolescence. Journal of Consulting and Clinical Psychology, 80, 139–150. doi: 10.1037/a0026577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BH (2000). The efficacy, safety, and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD). Clinical Child and Family Psychology Review, 3, 243–267. doi: 10.1023/A:1026477121224 [DOI] [PubMed] [Google Scholar]
- Swanson J, Nolan W, & Pelham W (1992). The SNAP-IV rating scale. Retrieved from http://www.adhd.net [Google Scholar]
- Turner WC, Muck RD, Muck RJ, Stephens RL, & Sukumar B (2004). Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs, 36, 455–462. [DOI] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, … Blumberg SJ (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry, 53, 34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker JS, Coleman D, Lee J, Squire PN, & Friesen BJ (2008). Children’s stigmatization of childhood depression and ADHD: Magnitude and demographic variation in a national sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 912–920. [DOI] [PubMed] [Google Scholar]
- Yeh M, Aarons GA, Ho J, Leslie LK, McCabe K, Tsai K, & Hough R (2014). Parental etiological explanations and longitudinal medication use for youths with attention-deficit/hyperactivity disorder. Administration and Policy in Mental Health and Mental Health Services Research, 41, 401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]


