To the Editor:
Physical activity (PA) is a cornerstone of prevention to decrease mortality in patients with chronic cardiovascular disease, including heart failure.1 , 2 Implantable cardiac devices offer the opportunity to monitor PA and data derived from implantable devices have been associated with short- and long-term outcomes.3 , 4 During the severe acute respiratory syndrome coronavirus 2 pandemic, restrictions to outdoor activity were imposed by national authorities. In Italy, after the first case of coronavirus disease-2019 (COVID-19) on February 21, the so-called lockdown act was passed on March 8, 2020.5 These rigorous measures decreased the impact of COVID-19 pandemic on the National Health System,6 but likely resulted in changes in the ability of patients to maintain PA levels. In the current study, we examined the impact of the COVID-19 and regulatory movement restrictions on the PA of patients with an implantable cardioverter defibrillator.
Methods
Consecutive patients who underwent implantable cardioverter defibrillator/cardiac resynchronization therapy defibrillator implantation at ASST-Papa-Giovanni-XXIII, Bergamo, and received a LATITUDE (Boston Scientific) system were included in the analysis. The observation window was set from January 7 to April 6 2020 (91 days) and 3 evaluation periods were defined during the 13 weeks of observation: a reference period (weeks 1–4), a pre-lockdown period (weeks 5–9), and a lockdown period (weeks 10–13). Device-derived daily patient activity level was collected from the implanted devices. Differences in proportions were compared by applying χ2 analysis or Fisher's exact test, as appropriate. Statistical significance level was set at a P value of less than .05.
Results
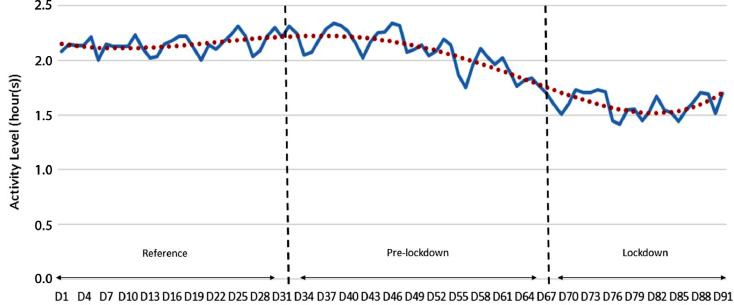
One hundred eighty-four patients with available data during the observation period were included in the analysis (mean age 67 ± 14 years, 73% male, 44% ischemic, 38% cardiac resynchronization therapy defibrillator). Baseline and clinical characteristics are reported in Supplemental Table 1. A total of 16,303 days were analyzed (mean of 89 days per patient). The mean activity level during the observation period was 1.98 ± 1.1 h/d. The activity level was significantly lower during lockdown period (1.62 ± 1.2 h/d) than during the pre-lockdown period and reference period (2.14 ± 1.3 h/d during pre-lockdown, P < .0001; 2.18 ± 1.3 h/d during reference, P < .0001). No difference was found between reference and pre-lockdown period (P = .14). During the observation period, 3 patients were hospitalized for COVID-19 and 8 patients for cardiovascular causes at the enrolling institution (1.6% and 4.3%, respectively) Figure 1 .
Fig. 1.
Trends of the mean day-by-day activity level of the whole study population during the observation period, from day 1 (D1, January 7, 2020) to day 91 (D91, April 6, 2020).
The mean decrease in the activity level observed during lockdown period was of 26.1 ± 25.0% compared with the reference period. The percentage of patients who had a decrease of more than 25% (moderate to substantial) was higher during the lockdown period (range 45.9%–57.2%) compared with the pre-lockdown period (range 6.3%–18.9%). No significant differences during the reference period between female and male patients were found (2.15±1.2 h/d vs 2.19±1.3 h/d, P = .8411). However, the percentage decrease in activity level was greater among males (–28.2% for men vs –19.4% for women, P = .038).
Discussion
The present study demonstrates the impact of COVID-19 pandemic on activity: an average decrease in PA of 0.5 hours per day, a decrease of more than 25% compared with the activity during the 2 reference periods. The decrease was observed in every subgroup of patients and in a substantial proportion of them (up to 60% of all patients over the 12 weeks of the study). The imposed lockdown corresponded with a shift in the activity of subjects from week 8 (last week of pre-lockdown period), indicating that patients’ behavioral changes anticipated the imposed restrictions, possibly a response to media coverage of the epidemic outbreak.
Patients decreased their PA irrespective of age, cardiomyopathy, or device implanted, although females showed a lesser decrease in activity level during the COVID-19 pandemic. The activity level of patients during the reference period did not predict a decrease of more than 25% of PA after the lockdown.
The substantial decrease in PA during the pandemic is noteworthy because it may expose patients to a higher risk of adverse outcomes.5 , 7 In addition, it may lead to deconditioning and decreased exercise tolerance in a population that already has limited reserve. In this context, insufficient PA and sedentary behavior have been associated with frailty.8 To minimize the risk for these untoward outcomes, patients should be encouraged to maintain PA levels if at all possible while adhering to the social distancing constraints imposed by the pandemic.
Declaration of Competing Interest
Maurizio Malacrida is a Boston Scientific employee; no other conflicts of interest exist.
Declaration of interest
No external funding was obtained for this project. Maurizio Malacrida is a Boston Scientific employee; no other conflicts of interest exist.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.cardfail.2020.08.005.
Appendix. Supplementary materials
References
- 1.Arnett D.K., Blumenthal R.S., Albert M.A., Buroker A.B., Goldberger Z.D., Hahn E.J. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:1376–1414. doi: 10.1016/j.jacc.2019.03.009. [published correction appears in J Am Coll Cardiol. 2019 Sep 10;74(10):1428-1429] [published correction appears in J Am Coll Cardiol. 2020 Feb 25;75(7):840] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee D.C., Pate R.R., Lavie C.J., Sui X., Church T.S., Blair S.N. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64:472–481. doi: 10.1016/j.jacc.2014.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly J.P., Ballew N.G., Lin L., Hammill B.G., Stivland T.M., Jones P.W. Association of implantable device measured physical activity with hospitalization for heart failure. JACC Heart Fail. 2020;8:280‐288. doi: 10.1016/j.jchf.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Conraads V.M., Spruit M.A., Braunschweig F., Cowie M.R., Tavazzi L., Borggrefe M. Physical activity measured with implanted devices predicts patient outcome in chronic heart failure. Circ Heart Fail. 2014;7:279–287. doi: 10.1161/CIRCHEARTFAILURE.113.000883. [DOI] [PubMed] [Google Scholar]
- 5.DPCM . Containing Urgent Measures Regarding the Containment and Management of the Epidemiological Emergency from COVID-19 (in Italian) President of the Council of Ministers of the Italian Republic; Rome, Italy: 2020. Decree of the President of the Council of Ministers of the Italian Republic of March 8, 2020 - Further ImplementingProvisions of the Decree-Law of 23 February 2020, n. 6.https://www.gazzettaufficiale.it/eli/id/2020/03/08/20A01522/sg Available at: [Google Scholar]
- 6.Gatto M., Bertuzzo E., Mari L., Miccoli S., Carraro L., Casagrandi R., Rinaldo A. Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures. Proc Natl Acad Sci U S A. 2020;117:10484–10491. doi: 10.1073/pnas.2004978117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biswas A., Oh P.I., Faulkner G.E., Bajaj R.R., Silver M.A., Mitchell M.S. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis [published correction appears in Ann Intern Med. 2015 Sep 1;163:400] Ann Intern Med. 2015;162:123–132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 8.da Silva V.D., Tribess S., Meneguci J., Sasaki J.E., Garcia-Meneguci C.A., Carneiro J.A.O. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health. 2019;19:709. doi: 10.1186/s12889-019-7062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.