Abstract
Background
The COVID-19 pandemic has introduced further challenges into Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) decisions. Existing evidence suggests success rates for CPR in COVID-19 patients is low and the risk to healthcare professionals from this aerosol-generating procedure complicates the benefit/harm balance of CPR.
Methods
The study is based at a large teaching hospital in the United Kingdom where all DNACPR decisions are documented on an electronic healthcare record (EHR). Data from all DNACPR/TEAL status forms between 1st January 2017 and 30th April 2020 were collected and analysed. We compared patterns of decision making and rates of form completion during the 2-month peak pandemic phase to an analogous period during 2019.
Results
A total of 16,007 forms were completed during the study period with a marked increase in form completion during the COVID-19 pandemic. Patients with a form completed were on average younger and had fewer co-morbidities during the COVID-19 period than in March-April 2019. Several questions on the DNACPR/TEAL forms were answered significantly differently with increases in patients being identified as suitable for CPR (23.8% versus 9.05%; p < 0.001) and full active treatment (30.5% versus 26.1%; p = 0.028). Whilst proportions of discussions that involved the patient remained similar during COVID-19 (95.8% versus 95.6%; p = 0.871), fewer discussions took place with relatives (50.6% versus 75.4%; p < 0.001).
Conclusion
During the COVID-19 pandemic, the emphasis on senior decision making and conversations around ceilings of treatment appears to have changed practice, with a higher proportion of patients having DNACPR/TEAL status documented. Understanding patient preferences around life-sustaining treatment versus comfort care is part of holistic practice and supports shared decision making. It is unclear whether these attitudinal changes will be sustained after COVID-19 admissions decrease.
Keywords: Resuscitation orders, Advance directives, Electronic health records, COVID-19
Introduction
Cardiopulmonary resuscitation (CPR) is a potentially life-saving intervention for patients who go into cardiac arrest. It involves the provision of airway manoeuvres, artificial ventilation, external chest compressions, and, in some cases, electrical defibrillation, until further interventions can be implemented to help return of spontaneous circulation (ROSC). CPR is an appropriate intervention in the case of sudden cardiac arrest in ‘shockable’ ventricular arrythmias (often due to acute myocardial ischaemia), but is less successful in cardiac arrests due to other causes which lead to ‘non-shockable’ rhythms.1, 2 Distinguishing a sudden cardiac arrest from a cardiac cause in the context of a deterioration is difficult, and standard practice is usually to attempt CPR on any inpatient who has a cardiac arrest, regardless of the underlying cause.1 Therefore, CPR is often attempted in many inpatients in whom there is little or no likelihood of benefit, as no anticipatory decisions were made about resuscitation status.3
Non-maleficence is one of the four pillars of medical ethics and this principle of ‘do no harm’ is deeply engrained in the attitudes of healthcare professionals.4 As such, protecting patients from unnecessary and potentially harmful procedures is an important aspect of healthcare provision. Whilst having the potential to prolong survival in some, for many patients CPR is at best futile and at worst degrading and physically harmful to a patient in the dying phase.
Even in successful CPR attempts, the effects of prolonged cerebral hypoxia can result in neurological deficits and a poor quality of life, suggesting that CPR may prolong death rather than prolong life. Due to the vigorous nature of chest compressions, there are also associated physical harms, including rib fractures, and airway manipulation may cause tracheal lesions.5
The COVID-19 pandemic has further complicated the challenges surrounding the decision to perform CPR. As CPR is an aerosol generating procedure, guidance states that staff undertaking CPR should be wearing full personal protective equipment (PPE) to reduce the risk of COVID-19 transmission.6, 7 The time taken to don PPE may delay CPR initiation and the use of bulky protective equipment can make it difficult to perform CPR with effective technique. Patients suffering from COVID-19 are most likely to deteriorate due to respiratory failure and/or sepsis. In an initial case series from Wuhan, China, the majority of cardiorespiratory arrests in COVID-19 inpatients were due to respiratory causes with asystole being the common presenting rhythm, hence long-term survival rates were minimal (3% survival at 30 days).8 This rate of survival to hospital discharge is far lower than usual rates seen after in-hospital cardiac arrests in the United Kingdom.9
Guidance from the National Institute of Health and Care Excellence during the COVID-19 pandemic has emphasised that a sensitive discussion should be undertaken in adult patients with capacity in whom an assessment suggests increased frailty (for example, a Clinical Frailty Score of 5 or more).10 The possible benefits and risks of any critical care treatment options, including CPR, and the possible likely outcomes should be taken into account and form part of the joint decision-making process. These decisions are particularly important in terminally ill patients approaching the end of life, either from a chronic, irreversible disease or an acute, severe illness such as COVID-19.
A ‘Do Not Attempt Cardiopulmonary Resuscitation’ (DNACPR) decision is an aspect of care that provides guidance to medical staff regarding the appropriate course of action in the case of a cardiac arrest. DNACPR decisions may be put in place in the community (‘community DNACPR’) or in hospital, but are not legally binding or signed by the patient or a witness. Importantly, DNACPR decisions differ from an ‘Advance Decision to Refuse Treatment’ (ADRT), which is a legally binding document signed by the patient which details which interventions a patient wishes not to receive in the case that they are unable to express their preferences, and can include decisions around CPR.
Historically, treatment limitation decisions have only been considered in patients where treatment may be futile. Doctors may be hesitant to initiate these difficult conversations due to fear of causing distress or complaints.11 However, due to the unpredictable nature of COVID-19 and who it may affect, at our hospital it was recommended that a conversation should be initiated with all inpatients surrounding ceilings of treatment and CPR, and document the subsequent decision.2
In the UK, many health and social care providers use a Recommended Summary Plan for Emergency Care and Treatment (ReSPECT), which documents the response to an emergency with a summary of recommendations to help make immediate decisions about a person’s care and treatment.12 The ReSPECT form is paper-based and many hospitals use this and other paper records to document decisions during patients’ hospital stays. However, as Electronic Healthcare Records (EHR) are rolled out in hospitals, DNACPR and Treatment Escalation and Limitation (TEAL) decisions are increasingly being documented electronically to provide high visibility and clear communication of the decisions.13 Our institution has adopted DNACPR within the EHR since October 2011.
This study aims to analyse EHR documentation on treatment limitation and DNACPR decisions comparing uptake, decisions and answers to different sections of the form before and during the COVID-19 situation.
Methods
Institution
This analysis was conducted in a large, urban teaching hospital in the West Midlands, UK, with an in-house built clinically-led EHR, PICS (Prescribing, Information and Communication System), which has been described elsewhere.14 The 1250-bed academic teaching hospital consists of a staff of over 7000 employees delivering general, specialist and emergency services to the local population. It has a large 100-bed intensive care unit with a surge capacity within the COVID-19 crisis to provide up to 350 critical care beds. There is no paediatric or obstetric care at the hospital. PICS provides users with clinical decision support, based on user privilege, full clinical documentation, provision of clinical protocols and best practice guidelines.
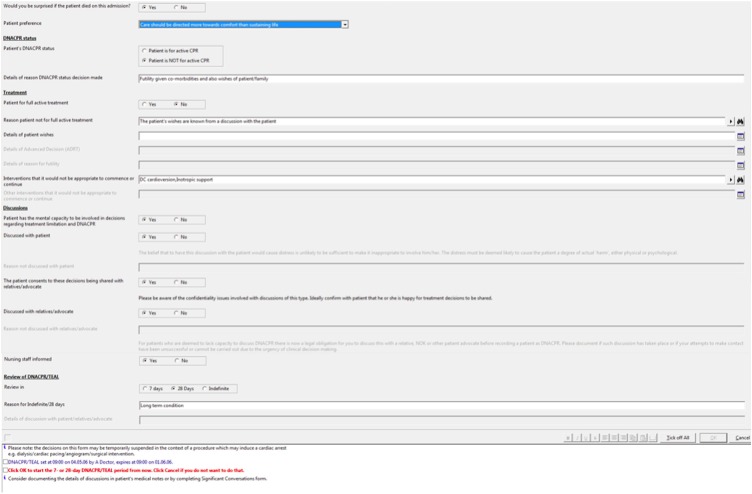
The PICS EHR incorporated a DNACPR/TEAL status form from the 17th October 2011 (Fig. 1 ). This was designed in conjunction with clinical staff including resuscitation services and palliative care. The form has mandated and non-mandated questions, and particular responses open other relevant sections of the form. It commences with the question ‘would you be surprised if the patient died on this admission?’ and then continues to ‘is this patient for full active treatment?’.
Fig. 1.
Screenshot of DNACPR/TEAL form in EHR.
Study population
Data was extracted from the PICS audit system for all DNACPR/TEAL forms completed. Data included the contents of the forms for all patients admitted between 1st January 2017 and 30th April 2020, as well as patient demographics. Patients may have multiple copies of this form as their conditions or situations change over their admission or on subsequent admissions. Therefore, to understand the differences in how the forms were completed and in order to avoid collinearity, only the first form completed for each patient was considered. The data was split into forms completed prior to 1st March 2020 (pre-COVID) and data between 1st March and 30th April 2020 (during COVID). The data collected during the COVID-19 period is compared with a corresponding time period in 2019, between 1st March to 30th April 2019.
To understand the impact on the hospital as a whole, the proportion of admissions with a valid DNACPR/TEAL status form completed during the admission was calculated. All patient episode forms in those who were admitted for at least 24 h were considered in this analysis.
Analytical/statistical methods
Data were analysed using Stata 15.1 (StataCorp). Summary counts and percentages are given for categorical values and median with interquartile range for continuous variables. Chi-Square analysis was performed on categorical variables and the Kruskall Wallis test on continuous variables.
Governance/role of funding source
The work is part of an ongoing institutional audit programme of DNACPR completion registered with the Clinical Audit Registration & Management System within the hospital. There was no external funding for this study.
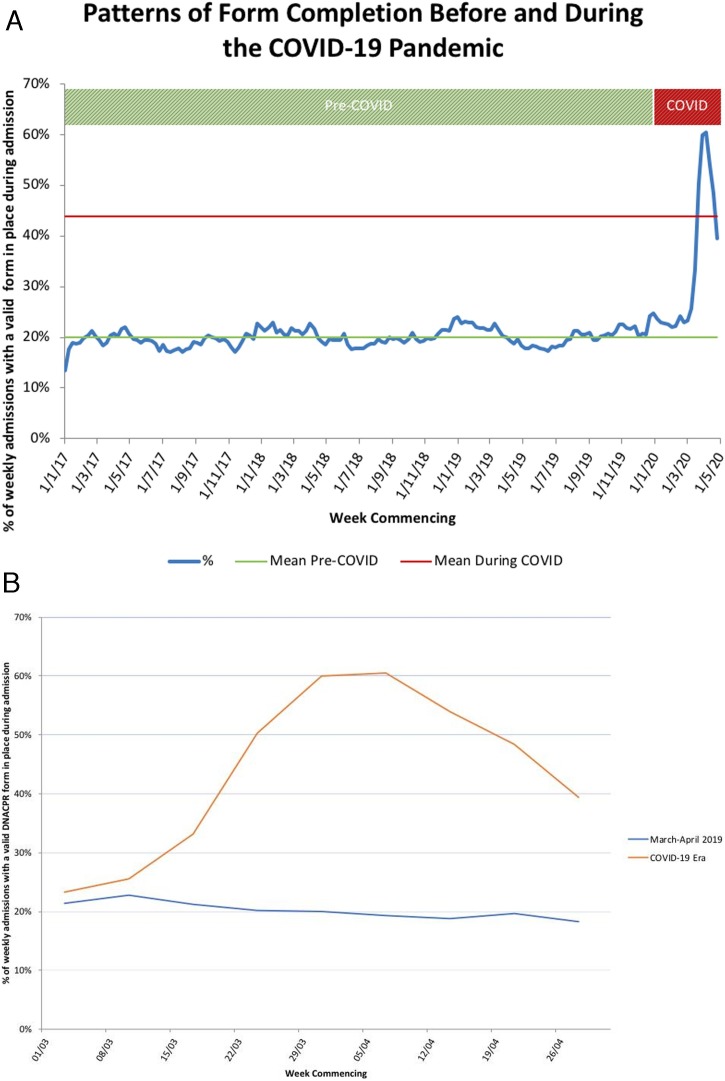
Results
A total of 16,007 forms were identified during the study period, 14,163 in the pre-COVID period, including 729 from 1st March to 30th April 2019. There were 1844 forms in the COVID period, with the rate of new forms more than doubling. There was also a marked increase in the percentage of patients who had spent at least 24 h in the hospital with a DNACPR/TEAL status documented on the EHR during some of their admission (Fig. 2 ).
Fig. 2.
(a) Patterns of form completion before and during the COCID-19 pandemic. (b) Close-up view of COVID-19 period compared to March–April 2019.
Where decisions were recorded about resuscitation in a patient record during the COVID-19 period, patients were younger (79 years pre-COVID vs 74 years during COVID; p < 0.001), less likely to have various co-morbidities and less likely to have a referral to the palliative care team (16.7% vs 28.5%; p < 0.001) (Table 1 ).
Table 1.
Demographics of patients with a completed form.
| Pre-COVID | Mar–Apr 2019 | During COVID | p Value‡ | ||
|---|---|---|---|---|---|
| n | 14,163 | 729 | 1844 | ||
| Median patient age (IQR) | 79 (67−87) | 79 (68−87) | 74 (61−83) | <0.001 | |
| Age group (years) | Under 66 | 3199 (22.6%) | 160 (21.9%) | 595 (32.3%) | <0.001 |
| 66−77 | 3207 (22.6%) | 180 (24.7%) | 497 (27.0%) | ||
| 78−84 | 2810 (19.8%) | 142 (19.5%) | 345 (18.7%) | ||
| 85−90 | 2809 (19.8%) | 142 (19.5%) | 272 (14.8%) | ||
| Over 90 | 2138 (15.1%) | 105 (14.4%) | 135 (7.3%) | ||
| Sex | Female | 7373 (52.1%) | 366 (50.2%) | 865 (46.9%) | 0.143 |
| Male | 6790 (47.9%) | 363 (49.8%) | 979 (53.1%) | ||
| Co-morbidities | Cancer | 3502 (24.7%) | 203 (27.8%) | 214 (13.1%) | <0.001 |
| Renal disease | 2759 (19.5%) | 135 (18.5%) | 316 (17.1%) | 0.439 | |
| Congestive Cardiac Failure | 2694 (19.0%) | 119 (16.3%) | 189 (10.3%) | <0.001 | |
| Liver Failure | 362 (2.6 %) | 17 (2.3 %) | 15 (0.8 %) | 0.003 | |
| Palliative Care | 3816 (26.9%) | 208 (28.5%) | 308 (16.7%) | <0.001 | |
| Critical Care | 502 (3.5%) | 19 (2.6%) | 62 (3.4%) | 0.387 | |
| SEWS†† Risk | SEWS 0 | 4847 (34.2%) | 255 (35.4%) | 549 (29.8%) | 0.012 |
| Low SEWS | 7056 (49.8%) | 334 (45.8%) | 959 (52.0%) | ||
| Medium SEWS | 1287 (9.1%) | 79 (10.8%) | 196 (10.6%) | ||
| High SEWS | 625 (4.4%) | 53 (7.3%) | 103 (5.6%) | ||
| Missing SEWS Information | 348 (2.5%) | 8 (1.1%) | 37 (2.0%) | ||
| Median Length of Stay (IQR) (Days)† | 14 (6−27) | 14(6−28) | 6 (3−13) | <0.001 | |
| Patient status at discharge† | Alive | 9627 (68.0%) | 505 (69.5%) | 1290 (77.3%) | <0.001 |
| Deceased | 4531 (32.0%) | 222 (30.5%) | 378 (22.7%) | ||
This is only given for the patients who have been discharged when the study was completed.
SEWS — Standardised Early Warning Scoring system.
This P value compares the COVID period to those forms completed in March and April 2019.
There were several findings that suggest that doctors’ behaviours changed during the COVID-19 crisis. Not only were significantly more decisions taken around resuscitation, but questions were answered differently (Table 2 ). Specifically, more doctors completing forms expressed that they would be surprised if patients died during admission (31.2% vs 17.0%, p < 0.001).
Table 2.
Responses on the DNACPR/TEAL form on the PICS EHR.
| Pre-COVID | Mar–Apr 2019 | During COVID | p Value‡ | ||
|---|---|---|---|---|---|
| Completion (total N) | 14,163 | 729 | 1844 | ||
| Doctor would be surprised if patient died on this admission | 2183 (15.4%) | 124 (17.0%) | 575 (31.2%) | <0.001 | |
| DNACPR is in place | 12,650 (89.3%) | 663 (90.9%) | 1406 (76.3%) | <0.001 | |
| Patient is for full active treatment | 3864 (27.3%) | 190 (26.1%) | 563 (30.5%) | 0.028 | |
| Reason not for full active treatment† | Patient’s wishes known | 2079 (20.2%) | 105(19.5%) | 242 (18.9%) | 0.107 |
| Futility | 9174 (89.1%) | 469(87.0%) | 1143 (89.2%) | 0.076 | |
| ADRT | 329 (3.2%) | 23(4.3%) | 22 (1.7%) | 0.711 | |
| Patient has capacity to be involveda | 5729 (44.6%) | 296 (43.9%) | 839 (58.5%) | <0.001 | |
| Decision was discussed with patientb | 5300 (92.5%) | 283 (95.6%) | 804 (95.8%) | 0.871 | |
| Decision was discussed with relativesc | 8520 (70.3%) | 480 (75.4%) | 648 (50.6%) | <0.001 | |
| Review date¹ | 7 days: 43.6% | 7 days: 42.4% | 7 days: 42.4% | 0.133 | |
| 28 days: 20.2% | 28 days: 19.7% | 28 days: 23.1% | |||
| Indefinite: 36.4% | Indefinite: 37.9% | Indefinite: 34.4% | |||
This is only completed when the patient is either not for full active treatment or not for active CPR (n = 15,826).
This question is only answered when it is confirmed that the patient has the mental capacity to be involved in decisions (n = 6568).
This is only completed when the patient has either given consent for their conditions to be discussed with relatives or does not have the mental capacity to be involved in decisions (n = 13,405).
Only for those who are not for full active treatment and multiple options can be chosen per patient.
This P value compares the COVID period to those forms completed in March and April 2019.
Doctors must state on the form whether CPR would be appropriate in the event of cardiopulmonary arrest. During COVID-19, significantly more patients had decisions made that CPR would be appropriate (23.8% vs 9.05% p < 0.001), reflecting active decision-making taking place for more patients. Doctors are then asked if the patient should be for full active treatment, and similarly more cases during COVID-19 were recorded as being for full treatment (30.5% vs 26.1%, p = 0.028). Of note, these three questions are all independent of each other.
Where a decision was made that treatment should be limited, this was due to futility in most cases, with the remainder due to patient’s wishes. Multiple reasons can be chosen, but reasons did not change significantly during COVID-19. However, there do appear to be fewer patients during COVID-19 with an advanced decision to refuse treatment (ADRT) (4.3% vs 1.7%, p = 0.771).
The proportion of discussions that involved the patient remained similar, with 95.6% in 2019 compared to 95.8% during COVID-19 (p = 0.871). There was an increase in the proportion of patients with capacity to be involved in decisions (43.9%–58.5%, p < 0.001). However, there was a significant decrease in DNACPR/TEAL decisions being discussed with the relatives – dropping from 75.4% to 50.6% (p < 0.001).
There was a marginally significant change in when the review dates (7 days, 28 days or indefinite) were set for reviewing the DNACPR/TEAL decisions when initially completing the forms.
Patients who had a DNACPR in place during the COVID-19 pandemic were generally younger than in March–April 2019 (74.5 years vs 79 years, p = 0.015) and had fewer comorbidities, with the exception of renal disease which was similar in the two groups (Table 3 ). The patients who had a form completed but did not have a DNACPR in place were also younger during COVID-19 than in 2019 (54.5 years vs 61.5 years, p = 0.006).
Table 3.
Age and comorbidities of patients before and during COVID-19 and whether they had a DNACPR put in place or not.
| Pre-COVID | Mar–Apr 2019 | During COVID | p Value‡ | ||
|---|---|---|---|---|---|
| DNACPR is in place | 12,650 (89.3%) | 663 (90.9%) | 1406 (76.3%) | <0.001 | |
| Patients with DNACPR in place | Median patient age (IQR) | 81 (70−88) | 79 (69−87.3) | 74.5 (63.3−82) | 0.015 |
| Cancer | 3215 (25.4%) | 191 (28.8%) | 212 (15.1%) | <0.001 | |
| Renal disease | 2630 (20.8%) | 132 (19.9%) | 286 (20.3%) | 0.819 | |
| Congestive Cardiac Failure | 2543 (20.1%) | 116 (17.5%) | 175 (12.4%) | 0.002 | |
| Liver Failure | 340 (2.7%) | 17 (2.6%) | 12 (0.9%) | 0.003 | |
| Patients without DNACPR in place | Median patient age (IQR) | 58 (43−70) | 61.5 (45−75) | 54.5 (44−65) | 0.006 |
| Cancer | 287 (19.0%) | 12 (18.2%) | 29 (6.6%) | 0.006 | |
| Renal disease | 129 (1.0%) | 3 (0.5%) | 30 (2.1%) | 0.349 | |
| Congestive Cardiac Failure | 151 (1.2%) | 3 (0.5%) | 14 (1.0%) | 0.389 | |
| Liver Failure | 22 (0.2%) | 0 (0.0%) | 3 (0.2%) | 0.656 | |
This P value compares the COVID period to those forms completed in March and April 2019.
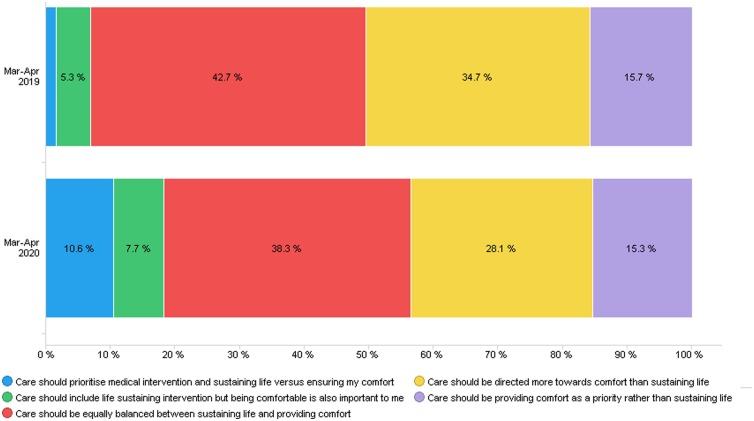
Information on patients’ preferences regarding treatments and their limitations can also be captured by the form, although it is not a compulsory question. During the COVID-19 era, significantly fewer clinicians completed this question than in 2019 (49.7% vs 56.9%, p = 0.001.
Discussion
The data would support the notion that clinicians have followed the recommendations to initiate treatment limitation conversations with more inpatients during this period. 1844 decisions involving CPR were made in an eight-and-a-half-week period, compared to 14,163 in the previous 165 weeks, reflecting an increase in the mean proportion of inpatients who had a form completed from 20% to 50%.
The National Confidential Enquiry into Patient Outcome and Death suggested that clear documentation for ceilings of care facilitates early decision making and improves clarity of intent.3 Nevertheless, it is apparent from this data that DNACPR forms were previously only completed in a small minority of patients in whom there is more likely to be an indication for treatment limitation. This suggests that there was a shift during the COVID-19 pandemic from undertaking decisions only in critically ill patients to a much wider group of inpatients. Of patients with treatment limitation documentation in place, clinicians previously believed 83% of patients were likely to die during admission in the similar period in 2019; this decreased to 70% during COVID-19. Similarly, during the pandemic 30.5% of patients were for full treatment, compared to 26.1% in 2019. This suggests that these conversations were being had with more patients who were not thought to be nearing the end of life and so CPR would be appropriate. This is supported by the fact that during COVID-19, patients who had a form in place were generally younger, had fewer co-morbidities and were less likely to have a palliative care referral. This increase in discussions about treatment limitations with a wider patient group than usual seems very appropriate during a pandemic period. However, it is difficult to establish whether the threshold for a DNACPR decision has changed as there was a parallel increase in both form completion and DNACPR decisions in younger patients.
Reasons for patients not being for full active treatment were similar between the two time periods. However significantly fewer patients had an ADRT during the COVID-19 era, 1.7% compared with 4.3% in 2019. It is unclear whether this is a true lack of advanced decision making or purely a lack of communication of any advanced directive during this crisis period. It may also reflect the younger, fitter cohort who are less likely to have an ADRT in place.
Shared decision making is a concept that has grown in popularity in recent times.15 Discussions around ceilings of care should involve patients where possible, and people should be included in decisions about their care.16 The proportion of discussions that involved the patient was roughly similar. However, significantly more patients were deemed to have capacity, increasing from 43.9% to 58.5%. This is possibly due to the change from traditional practice of only initiating decisions when patients are either extremely frail, and may have lost capacity due to their disease or comorbidities, or are already too critically ill to be communicated with. Despite the change in circumstances since COVID-19, it appears that doctors are still involving patients in these key decisions where possible. Including patients in discussions about their care allows them to clarify what their preferences are with regards to ceilings of care and treatment escalation.
Patients’ preferences continue to be documented; there has been a small decrease from 56.9% to 49.7% of clinicians documenting patient wishes. There is a shift from patients prioritising comfort to opting for life-sustaining treatments as shown in Fig. 3 . As previously discussed, this may be due to an increase in these conversations with relatively well patients who are younger and therefore more likely to want full life-sustaining treatment. It is important to note that documenting patient wishes is not mandatory in the electronic form, thus explaining the overall low percentage of completion. Over 90% of decisions were discussed with the patient, therefore patient wishes may be considered but not explicitly documented in this form. Especially during times of increased pressure on clinicians’ time, non-compulsory questions are likely to be ignored Documenting patient preferences should be encouraged to ensure that there is a shared understanding of where the balance between active medical interventions and comfort care is considered appropriate.
Fig. 3.
Patient preferences on treatment priorities.
Patients may normally choose to involve their families in discussions surrounding ceilings of care. To reduce the spread of COVID-19 and maintain social distancing, during the pandemic visitors were no longer allowed in our hospital, apart from exceptional circumstances. This may explain the reduction in discussions with relatives from 75.4% to 50.6%, as they are no longer available for face-to-face discussions. Our experience suggested that treatment limitation discussions did tend to take place during patient admissions with their relatives by telephone as we employed dedicated family liaison personnel. However, these discussions were noted in the narrative patient record and not revisited on the DNACPR/TEAL status form. It is also possible that as a smaller proportion of patients are having decisions advising treatment limitation, that clinicians may decide that the decisions do not need to be discussed with the family, as full active treatment would be the care they would expect.
Although there is a statistically significant difference between the review date set between the pre-COVID era and during the pandemic, this may not be clinically significant as proportions were not dissimilar. Without greater scrutiny into the decision-making process of clinicians, it is difficult to establish the justifications for review date decisions.
We are quite reassured by the apparent change in practice during the COVID-19 pandemic and recognise that making early decisions surrounding ceilings of care has multiple benefits. Patients and their families are prepared for the possibility of deterioration, giving them time to consider their wishes and concerns, and thus allowing patient autonomy, which is particularly important to remember in a time of such uncertainty. In-hospital CPR is managed by a team of healthcare professionals and during the COVID-19 situation, where healthcare systems are under increased pressure, the inappropriate initiation of CPR may remove critical care staff from other patients where their expertise may be more beneficial. Furthermore, PPE is a precious resource in this time,17 and it is therefore important to minimize potential ‘wastage’ by avoiding inappropriate CPR.
Study limitations
There are some limitations to this study. The information submitted on the electronic form is only what is reported at the time. It is possible that due to social responsibility bias that what was said to happen (discussion with patient and/or relatives) may not have actually happened. As with any electronic form it is impossible to uncover these responses, however we cannot see why COVID-19 would have considerably affected the rate of such responses. We only addressed the first DNACPR/TEAL form for each patient to prevent double counting responses. However, if a patient had several admissions during the time period, with different decisions on the DNACPR/TEAL this would have been missed. Clinicians can re-enter and change the forms as many times as they like within an episode. Therefore, we miss the nuances of data if clinicians have altered forms when, for example, relatives have been communicated with at a later stage. Our experience tells us that even when communication by telephone happens with relatives, that people usually document this in the noting section of the EHR and do not re-enter the DNACPR/TEAL form itself. Lastly, despite the positive response to early senior decision making in the COVID-19 pandemic, we will have to collect ongoing data to see if this effect is sustained in the post−COVID period.
Conclusion
Decisions about cardiopulmonary resuscitation and treatment escalation are a key part of modern hospital care. Whilst the main clinical focus should always be on prevention of cardiac arrest – which is the first link in the chain of survival18 – there are inevitable cases where sudden unexpected deterioration requires institution of life support. However, avoiding unnecessary CPR attempts which would lead to a degrading situation at the end of life, is also key. Whilst there should be a discussion about all inpatients surrounding treatment limitation or escalation, evidence remains that this does not always occur. It is heartening to see that DNACPR/TEAL decisions are being made in a greater proportion of patients. We hope that the attitudinal changes seen persist after COVID-19 to provide ongoing patient-centred decision making and avoid potentially futile CPR attempts in the future.
Conflicts of interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) (JJC) and all authors want to declare (1) No financial support for the submitted work (2) No financial relationships with commercial entities that might have an interest in the submitted work; (3) No spouses, partners, or children with relationships with commercial entities that might have an interest in the submitted work; (4) No non-financial interests that may be relevant to the submitted work.
CRediT authorship contribution statement
Jamie J. Coleman: Conceptualization, Methodology, Supervision, Writing - review & editing. Adam Botkai: Writing - original draft. Ella J. Marson: Writing - original draft. Felicity Evison: Methodology, Formal analysis, Investigation. Jolene Atia: Methodology, Formal analysis, Investigation. Jingyi Wang: Methodology, Formal analysis, Investigation. Suzy Gallier: Methodology, Formal analysis, Investigation. John Speakman: Conceptualization, Writing - review & editing. Tanya Pankhurst: Conceptualization, Writing - review & editing.
Acknowledgements
The views expressed in this publication are not necessarily those of the Department of Health, University Hospital Birmingham or the University of Birmingham.
References
- 1.Smith G., Pitcher D. Resuscitation Council; UK: 2015. Prevention of cardiac arrest and decisions about CPR.https://www.resus.org.uk/resuscitation-guidelines/prevention-of-cardiac-arrest-and-decisions-about-cpr/ [cited 01/05/2020]. Available from: [Google Scholar]
- 2.Grunau B., Reynolds J.C., Scheuermeyer F.X. Comparing the prognosis of those with initial shockable and non-shockable rhythms with increasing durations of CPR: informing minimum durations of resuscitation. Resuscitation. 2016;101:50–56. doi: 10.1016/j.resuscitation.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Findlay Gp, Shotton H., Kelly K., Mason M. National confidential enquiry into patient outcome and death. 2012. Time to intervene? A review of patients who underwent cardiopulmonary resuscitation as a result of an in-hospital cardiorespiratory arrest. [Google Scholar]
- 4.Beauchamp T., Childress J. 8 ed. Oxford University Press; 2019. Principles of biomedical ethics. [Google Scholar]
- 5.Buschmann C.T., Tsokos M. Frequent and rare complications of resuscitation attempts. Intensive Care Med. 2009;35:397–404. doi: 10.1007/s00134-008-1255-9. [DOI] [PubMed] [Google Scholar]
- 6.Resuscitation Council (UK) 2020. Resuscitation Council UK Statement on COVID-19 in relation to CPR and resuscitation in acute hospital settings.https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid-19-coronavirus-cpr-and-resuscitation/covid-healthcare/ [updated 06/04/2020; cited 28/04/2020]. Available from: [Google Scholar]
- 7.Public Health England . 2020. COVID-19: personal protective equipment use for aerosol generating procedures.https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures [updated 10/04/2020; cited 28/04/2020]. Available from: [Google Scholar]
- 8.Shao F., Xu S., Ma X. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nolan J.P., Soar J., Smith G.B. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85:987–992. doi: 10.1016/j.resuscitation.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Health and Care Excellence . 2020. COVID-19 rapid guideline: critical care in adults.https://www.nice.org.uk/guidance/ng159/chapter/4-Clinical-decision-making [updated 29/04/2020; cited 30/04/2020]. NICE Guideline (NG159)]. Available from: [PubMed] [Google Scholar]
- 11.Mentzelopoulos S.D., Bossaert L., Raffay V. A survey of key opinion leaders on ethical resuscitation practices in 31 European Countries. Resuscitation. 2016;100:11–17. doi: 10.1016/j.resuscitation.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Resuscitation Council (UK). ReSPECT. [updated August 2019; cited 28/04/2020]. Available from: https://www.resus.org.uk/respect/.
- 13.Johnson M., Whyte M., Loveridge R., Yorke R., Naleem S. A unified electronic tool for CPR and emergency treatment escalation plans improves communication and early collaborative decision making for acute hospital admissions. BMJ Qual Improv Rep. 2017;6 doi: 10.1136/bmjquality.u213254.w6626. u213254.w216626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nightingale P.G., Adu D., Richards N.T., Peters M. Implementation of rules based computerised bedside prescribing and administration: intervention study. BMJ. 2000;320:750–753. doi: 10.1136/bmj.320.7237.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elwyn G., Frosch D., Thomson R. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Health . 2012. Liberating the NHS: no decision about me, without me.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216980/Liberating-the-NHS-No-decision-about-me-without-me-Government-response.pdf [cited 13/05/2020]. Available from: [Google Scholar]
- 17.Iacobucci G. Covid-19: doctors still at “considerable risk” from lack of PPE, BMA warns. BMJ. 2020:m1316. doi: 10.1136/bmj.m1316. [DOI] [PubMed] [Google Scholar]
- 18.Nolan J., Soar J., Eikeland H. The chain of survival. Resuscitation. 2006;71:270–271. doi: 10.1016/j.resuscitation.2006.09.001. [DOI] [PubMed] [Google Scholar]