Abstract
Purpose
The cornea is highly enriched in sensory neurons expressing the thermal TRP channels TRPV1, TRPA1, and TRPM8, and is an accessible tissue for study and experimental manipulation. The aim of this work was to provide a concise characterization of the expression patterns of various TRP channels and vesicular proteins in the mammalian cornea.
Methods
Immunohistochemistry (IHC) was performed using wholemount and cryostat tissue preparations of mouse and monkey corneas. The expression patterns of TRPV1 and TRPA1 were determined using specific antisera, and further colocalization was performed with antibodies directed against calcitonin-related gene protein (CGRP), neurofilament protein NF200, and the secretogranins ScgII and SCG3. The expression of TRPM8 was determined using corneas from mice expressing EGFP under the direction of a TRPM8 promoter (TRPM8EGFP mice). Laser scanning confocal microscopy and image analysis were performed.
Results
In the mouse cornea, TRPV1 and TRPM8 were expressed in distinct populations of small diameter C fibers extending to the corneal surface and ending either as simple or ramifying terminals, or in the case of TRPM8, as complex terminals. TRPA1 was expressed in large-diameter NF200-positive Aδ axons. TRPV1 and TRPA1 appeared to localize to separate intracellular vesicular structures and were primarily found in axons containing components of large dense vesicles with TRPV1 colocalizing with CGRP and ScgII, and TRPA1 colocalizing with SCG3. Monkey corneas showed similar colocalization of CGRP and TRPV1 on small-diameter axons extending to the epithelial surface.
Conclusions
The mouse cornea is abundant in sensory neurons expressing TRPV1, TRPM8, and TRPA1, and provides an accessible tissue source for implementing a live tissue preparation useful for further exploration of the molecular mechanisms of hyperalgesia. This study showed that surprisingly, these TRP channels localize to separate neurons in the mouse cornea and likely have unique physiological functions. The similar TRPV1 expression pattern we observed in the mouse and monkey corneas suggests that mice provide a reasonable initial model for understanding the role of these ion channels in higher mammalian corneal physiology.
Introduction
Harmful stimuli at the periphery of the body are detected by nociceptive, polymodal sensory neurons with afferents that project from the dorsal root ganglia (DRG) and the trigeminal ganglia (TG). Nociceptive fibers line the epithelium of the esophagus, gut, intestine, and bladder, and are involved in the transmission of pain to the central nervous system. Currently, opiates, which target central pain pathways, are the dominant therapy addressing pain. These treatments are often addictive [1] and only moderately effective [2], yet are still used, in part because we have few useful tissue models with which to research molecular mechanisms transducing pain at the periphery. The mouse cornea is a highly accessible tissue with which to develop such a preparation and has been shown with electrophysiological methods to contain the temperature-sensitive TRP channels TRPV1, TRPA1, and TRPM8 [3-5]. The capsaicin receptor, TRPV1, is activated endogenously by heat (>42 °C), extracellular protons, and the endocannabinoid anandamide. These signals are perceived centrally as heat and pain [6,7]. In some species, TRPA1 also responds to heat [8]. TRPM8 and TRPA1 respond to cold, although cold-dependent activation of TRPA1 remains controversial [8-18]. These channels also detect chemical stimuli. TRPM8 is activated by menthol and icillin, and TRPA1 is activated by pungent compounds like mustard oil and cinnamaldehyde [5,19]. During inflammation, many chemicals are released that increase the number of functional TRP channels. This results in nociceptor sensitization, the cellular correlate of central hyperalgesia [20-22].
The cornea is richly innervated, but the distribution of TRP channels and their localization within sensory neuronal neuropeptide vesicles has not been fully explored. There are two main types of sensory neurons, large-diameter A fibers and small-diameter C fibers. Typically, A fibers are myelinated; however, in the cornea, to preserve transparency, no fibers are myelinated upon entering the stroma. Bundles containing Aδ and C fibers enter the midstromal region equally distributed around the corneal periphery and branch perpendicularly toward the surface through several epithelial layers. The small-diameter C fibers extend through tightly packed epithelial cells to the corneal surface, much like the sensory fibers in the glabrous skin of the rodent hind paw. Some axon terminals are highly branched (complex); others are T-shaped (ramifying) or not branched at all (simple) [3].
The complex degree of innervation makes the cornea highly susceptible to pain, and studies have shown that with recent cornea procedures such as photorefractive surgery, and with the development of dry eye in an increasing elderly population, eye pain has become a significant health issue [23,24]. Immediate damage to the eye, as with surgical procedures, results in acute inflammation and hyperalgesia. In DRG neurons in culture, exposure to nerve growth factor (NGF), a growth factor released during inflammation, results in an increase in functional TRPV1 channels on the cell surface causing sensitization [22]. Others have noted a release of the neuropeptide CGRP in response to inflammation and report that TRPV1 and CGRP are localized to the same axons [25,26]. A recent study found that TRPV1-induced sensitization triggers the release of the neuropeptide substance P from TRPM8-expressing sensory neurons to signal cold nociception [27]. TRPA1 was also proposed to play a role in dry eye in rats [28], although the normal development of dry eye in TRPA1 knockout mice suggested that TRPA1 does not play a significant role in corneal cold nociception in mice [27]. Understanding the expression patterns and interplay of these TRP channels within the cornea will further elucidate their role in corneal pain and cold nociception.
The colocalization pattern of the TRP channels TRPV1, TRPA1, and TRPM8, and the neuropeptide CGRP, has been reported in the axon terminals and cell bodies of several tissues [29-31]. The majority of studies were performed at the level of the DRG cell soma or DRG cell cultures and demonstrated coexpression of two or more TRP channels; many also expressed CGRP. The cornea is innervated by the axon terminals of the ophthalmic branch of the trigeminal ganglia, which resides at the base of the brainstem. The mouse cornea has been used extensively as a model system for understanding human physiology, with modern genetic approaches allowing the role of specific proteins to be readily addressed. However, there are some differences in morphology between mouse and monkey corneas. In mice, there are unmyelinated nerves in the deeper layers of the cornea within micrometers of the endothelium, whereas monkey corneas do not have nerve fibers found deeper than 50 μm from the epithelium [32]. To determine whether the cornea would serve as a representative peripheral tissue model for functional studies to explore the role of inflammatory mediators and hyperalgesia, the expression pattern and colocalization of CGRP and TRP channels were examined in young adult mouse and monkey corneas.
Methods
Corneal tissue
Mouse corneas were obtained from C57BL/6J mice and TRPM8EGFP mice, described by Dhaka [33], 6–9 weeks of age (The University of Washington Institutional Animal Care and Use Committee approved the study). Corneas were fixed in 4% paraformaldehyde (PFA) in PBS (10 mM phosphate buffered saline, 138 mM NaCl, 2.7 mM KCl, pH 7.4; Sigma, St. Louis, MO) solution at room temperature for 5 min before dissection. Isolated corneas were fixed 5–10 min longer. Fixed corneas were placed at 4 °C in PBS until used for wholemount immunostaining. Monkey corneal tissue from Macaca nemestrina was obtained through the Tissue Distribution Program of the Washington National Primate Research Center. Monkey corneas were isolated within 4 h of acute euthanasia of the animal and fixed as a wholemount for 2 h at room temperature, 4% PFA/PBS, and stored at 4 °C in PBS until use. Mice were euthanized using application of carbon dioxide in a closed chamber at a rate of 20% of the chamber volume per minute for at least 5 min, followed by decapitation. Primate samples were from Dr. Fred Rieke’s lab, who received tissues from the Distribution Program of the Regional Primate Research Center at the University of Washington following procedures approved by the Institutional Animal Care and Use Committee. Tissue was prepared for cryostat sectioning by sinking in 30% sucrose (EMD Millipore, Burlington, MA)/PBS followed by Tissue-Tek O.C.T. Compound (Sakura Finetek, Torrance, CA) and cryostat sectioned at 12 µm. All imaging was reproduced from at least three corneas.
Immunohistochemistry
Cornea wholemounts were placed in 10% Triton X-100 (BioWorld, Dublin, OH) /2% bovine serum albumin (BSA, Sigma)/PBS rotating gently at room temperature for 2 h, rinsed with PBS, and placed in primary antisera in 1% Triton/2% BSA/PBS for 24 h at 4 °C. Antibodies used are described in Appendix 1. Corneas were washed five to six times for 10 min with PBS and placed in the appropriate secondary antisera in 1% Triton/2% BSA/PBS for 24 h at 4 °C. Tissue was rinsed using 10 min successive washes with PBS once, 4’,6’-diamidino-2-phenylindole, dilactate (DAPI) once, and PBS three times, and then mounted in Fluoromount G (Southern Biotech, Birmingham, AL). The cryostat sections were treated in a similar manner.
Microscopy
Confocal scanned images were collected using a 63X oil immersion lens and a Zeiss LSM710 microscope using 405, 488, 561, and 633 nm laser lines to excite DAPI (405 nm) or the appropriate secondary antisera. Images were processed using Fiji [34].
Results
TRPV1 was expressed throughout sensory axons terminating in the epithelial layers of the mouse cornea
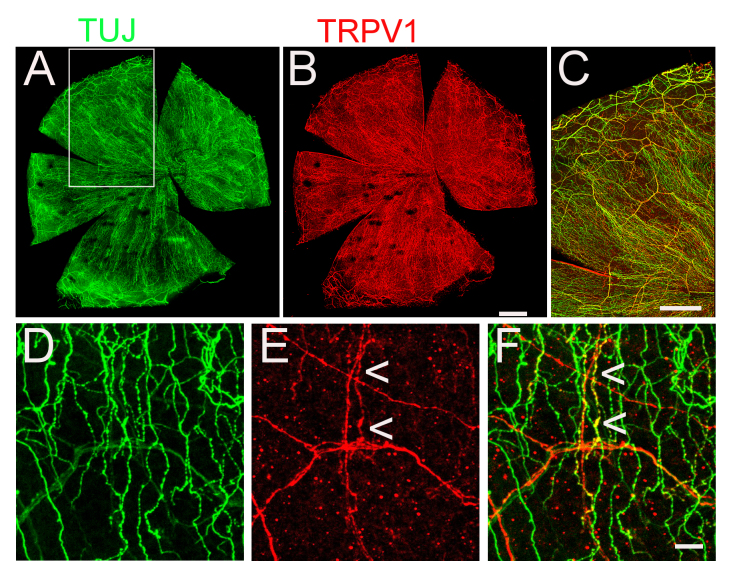
To determine the pattern of TRPV1-expressing axons in the mouse cornea, wholemount coimmunolabeling was performed, with an anti-TRPV1 antibody and an antibody raised against the axonal marker neuronal β-tubulin (TUJ). All fiber bundles entering the cornea around the periphery contained TRPV1-positive axons that branched as they entered the midstroma and the sub-basal epithelial region (the basal cell layer of the corneal epithelium at the stroma interface). Many of the TRPV1 fibers appeared to be the thin, varicose C fibers extending all the way through the epithelial cell layers to the corneal surface (Figure 1).
Figure 1.
TRPV1 is expressed in axons throughout the cornea. A, B: Neuronal β-tubulin (TUJ) and TRPV1 antisera labeled axons in a mouse cornea wholemount. C: Merged section from the wholemount in A, B (boxed area in A) demonstrating many of the axon fiber bundles entering the cornea express TRPV1. D–F: Three-dimensional x,y projection from the sub-basal level to the cornea surface; arrowheads point to small-diameter fibers expressing TRPV1 extending to the surface. Scale bars: (AB) 500 μm; (C) 350 μm; (D–F) 10 μm.
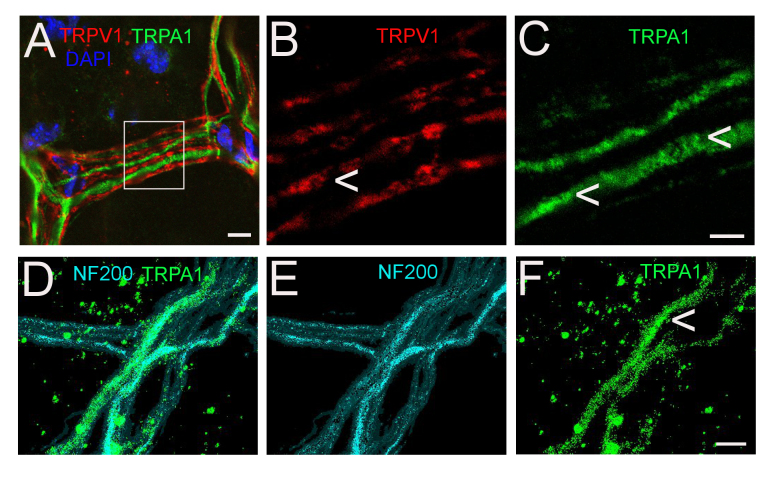
TRPA1 was not expressed in TRPV1-containing mouse corneal axons
TRPA1 activity in response to allyl isothiocyanate has been reported in the cornea [35]. Double immunolabeling for TRPV1 and TRPA1 revealed that fiber bundles entering the periphery of the cornea and midstromal fibers contained axons expressing both TRP channels, but they were in separate axons (Figure 2A–C). The axons expressing TRPA1 appeared to be of a larger diameter compared to the TRPV1-expressing axons, suggesting TRPA1 is confined to Aδ fibers. Coimmunolabeling with TRPA1 and the Aδ-specific neurofilament protein, NF200, completely overlapped (Figure 2D–F). The labeling for TRPA1 and TRPV1 appeared punctate, suggesting much of the protein is likely located in intracellular compartments (Figure 2B,C,F, arrows). Aδ fibers terminate as simple terminals primarily in the stroma and sub-basal regions. In agreement with this, no TRPA1 expression was observed in the epithelial layers of the cornea.
Figure 2.
TRPV1 and TRPA1 are in separate axons in the cornea. A–C: TRPV1 and TRPA1 antisera labeled axons in the stromal region of the cornea. Boxed region of A is shown in B, C. D-F: TRPA1 and NF200 immunolabeling colocalize to the same axons. Arrowheads indicate punctate, intracellular immunostaining in B, C and F. Scale bars: (A, D–F) 5 μm; (B, C) 2 μm.
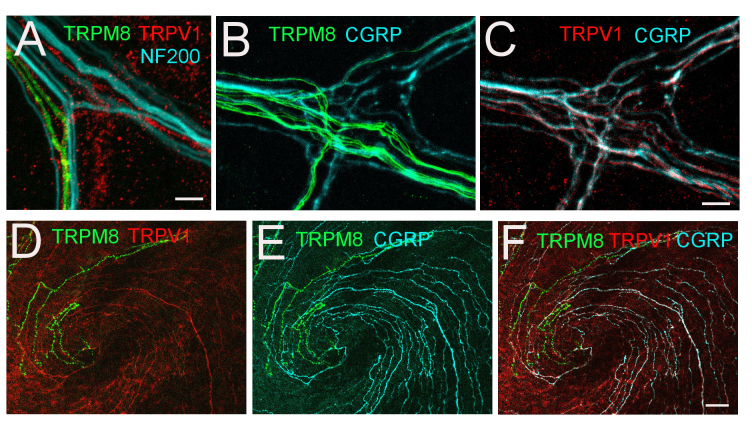
TRPM8 was expressed in mouse corneal C fibers that did not contain TRPV1
The ion channel TRPM8 has been reported to be involved in sensing osmolality and regulation of corneal blinking [36] and is expressed in C fibers in the mouse cornea [5]. Cold and chemical stimuli were found to enhance TRPM8 responses when TRPV1 was coexpressed in TRPM8-positive fibers [27], although the evidence that TRPM8 and TRPV1 colocalize is controversial [3,37]. To determine whether TRPM8 expression overlaps with TRPV1, wholemount, fixed corneas obtained from TRPM8EGFP mice were immunolabeled with TRPV1 antisera and imaged. TRPV1 and TRPM8EGFP were found primarily in C fibers and not in fibers immunolabeled with NF200 (Figure 3A). In all corneas imaged, fewer axons expressed TRPM8 compared to TRPV1, and these TRP channels were found in different neurons (Figure 3D,F).
Figure 3.
TRPV1/CGRP and TRPM8 do not colocalize and are not in NF200-positive axons. A: Stromal fiber bundle from a TRPM8EGFP mouse entering the cornea labeled with antisera directed against NF200 in Aδ fibers and TRPV1. Stromal fiber (B, C) and central-pericentral (D–F) region from the TRPM8EGFP mouse cornea wholemount immunolabeled with CGRP (cyan) and TRPV1 (red). Scale bars: (A–C) 2 μm; (D–F) 10 μm.
TRPV1 mouse corneal axons contained the neuropeptide CGRP
The neuropeptide CGRP is also reported to be expressed in C fibers of other sensory neuronal populations, in the DRG and throughout the gut, and has been shown to colocalize with TRPV1 [26]. Almost all TRPV1-positive axons also contained CGRP throughout the cornea from their entry at the periphery to their termination at the corneal surface (Figure 3C,F). Neither TRPV1 nor CGRP expression appeared to localize to TRPM8EGFP-expressing axons (Figure 3F).
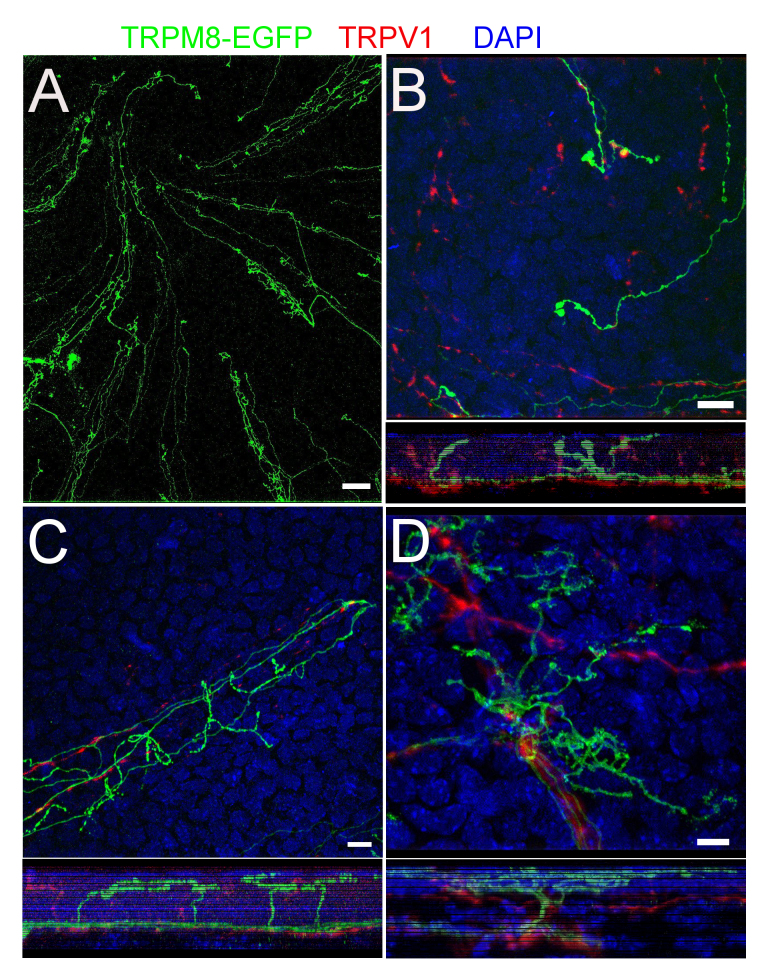
The axon terminal morphology of TRPM8 axons differed from that of TRPV1 axons in mice
TRPV1-/CGRP-containing axon terminals extended throughout the cornea to the corneal surface either as simple or ramifying terminals (Figure 4A,B). TRPM8 axons terminated at the corneal surface as well, as simple, ramifying, or complex termini (Figure 5B–D). Although there was some variability between corneas, simple terminals were seen mostly toward the center of the cornea, ramifying terminals were mostly in the pericentral region, and complex terminals were mostly closer to the periphery (Figure 5A).
Figure 4.
TRPV1 axons terminate in a simple or ramifying morphology. A: The top panel shows axon terminals expressing TRPV1 and CGRP at the surface of the cornea. The orthogonal view below is generated by projecting the z-series below in the x-plane. The arrowhead to the right of the y,z panel below indicates the location of the section above containing ramifying terminals. B: Cross section of the cornea epithelium (12 µm cryosection), sub-basal to surface, demonstrates the colocalization of TRPV1 and CGRP in an axon terminal with simple morphology. As in A, the green arrowhead indicates the surface epithelium, the blue bar indicates the epithelial layers, and the red arrowhead points to the sub-basal epithelium. (A, B) Scale bar: 5 µm.
Figure 5.
TRPM8 axons terminate in simple, ramifying, and complexed branches. A: Wholemount of TRPM8EGFP mouse cornea central-pericentral region. B–D: Terminal morphology; the small panels under each image show orthogonal views generated by projecting the z-series above it in the x-plane. Simple (B), ramifying (C), and complex (D) morphologies are demonstrated. Scale bars: (A) 20 μm; (B–D) 5 μm.
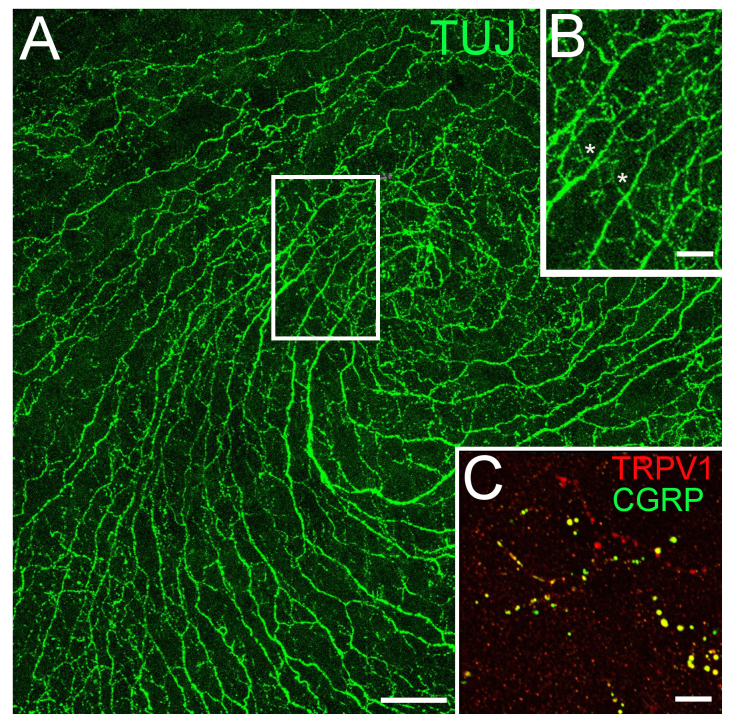
Monkey cornea contained simple TRPV1/CGRP axon terminals extending to the corneal surface
As there are some morphological differences between monkey and mouse corneas, we examined whether the TRPV1 and CGRP neurons are distributed similarly in mice and monkey corneas. The expression pattern and terminal morphology of TRPV1/CGRP-positive axons appeared roughly similar for the mouse (Figure 4) and monkey (Figure 6) tissues. Within the resolution of the confocal microscopy, they appeared to largely localize to the same neurons and to the same intracellular compartments within neurons (Figure 6C). Limited access to monkey tissue prevented further characterization within monkey corneas.
Figure 6.
TRPV1 and CGRP are expressed in epithelial C fibers in the monkey cornea. A: Neuronal β-tubulin (TUJ) immunolabeling of monkey wholemount cornea. B: Boxed area of A, small-diameter C fibers extending to the surface (asterisks). C: TRPV1 and CGRP are expressed in C fibers at the corneal surface. Scale bars: (A) 50 μm; (B) 20 μm; (C) 5 μm.
The secretogranins ScgII and SCG3 were expressed in mouse corneal sensory neurons
As shown in Figure 2A–C, TRPV1 (red) and TRPA1 (green) appeared intracellular and punctate, indicating their likely localization to intracellular vesicles. Neuropeptides, including CGRP, are packaged in chromogranin or secretogranin containing large dense core vesicles (LDCVs) [38]. Secretogranins are a diverse group of LDCV proteins, some of which, like secretogranin II (ScgII), are cytoplasmic and are proteolyzed into several smaller peptides in vesicles [39]. Others, such as SCG3, are small transmembrane protein components of LDCVs [38]. ScgII and SCG3 were shown to be expressed in nociceptive, TRPV1-containing neurons with RNA sequencing and proteomic studies [40]. Using antisera directed against ScgII and SCG3, we found that these secretogranins were expressed in separate axon populations within the mouse cornea, that ScgII labeling colocalized to TRPV1-expressing axons (Figure 7E), and that SCG3 appeared to be contained in NF200-positive Aδ/TRPA1 fibers (Figure 7F).
Figure 7.
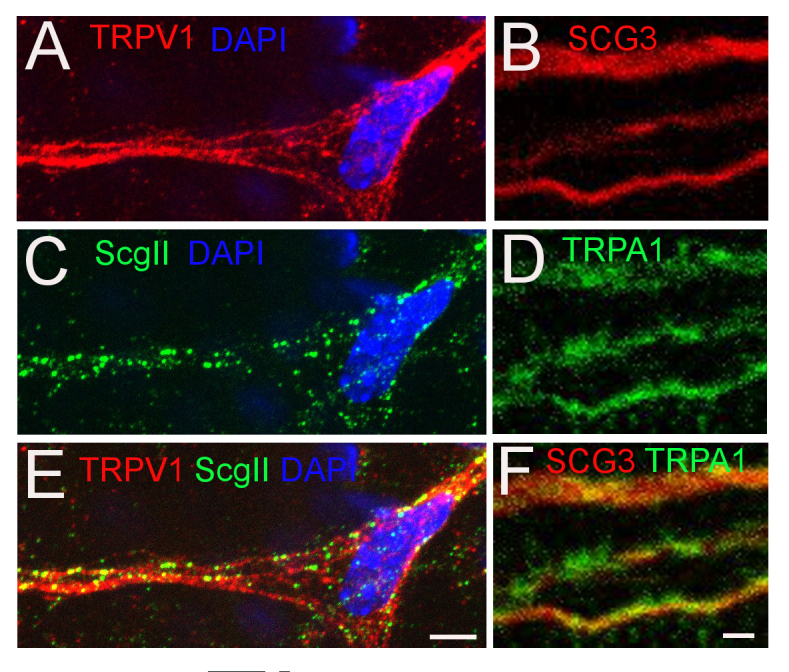
TRPV1 and TRPA1 are colocalized to axons containing the LDCV proteins ScgII and SCG3, respectively. A, C, E: TRPV1 and ScgII expression in stromal axons. B, D, F: TRPA1 and SCG3 expression in stromal axons. Scale bars: (A, C, E) 5 μm; (B, D, F) 2 μm.
Discussion
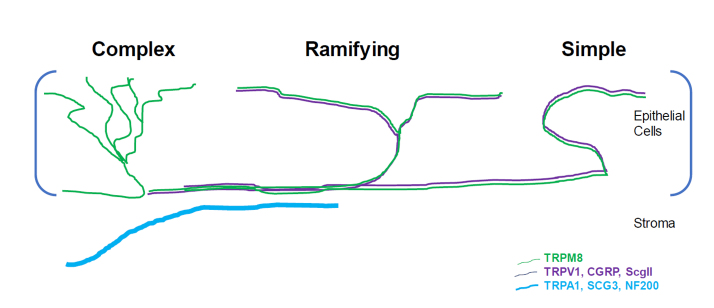
The mouse cornea is densely innervated and contains sensory neurons expressing TRPV1, TRPA1, and TRPM8 primarily in a non-overlapping manner. TRPV1 was found to colocalize with CGRP and with the ScgII member of the secretogranin family. In contrast, TRPA1 colocalized with SCG3 (Figure 8). TRPM8 expression was not directly measured, as the available antisera tested were not sufficiently specific. Instead, expression was determined using corneas from TRPM8EGFP mice [34]. Three different morphologies were observed for TRPM8 axonal terminals, whereas all TRPV1 axons observed terminated in a simple or ramifying manner at the cell surface, and TRPA1 Aδ fibers contained simple terminations in the sub-basal epithelium.
Figure 8.
Schematic of TRP channel and neuropeptide vesicle expression in the cornea. Neurons expressing TRPM8 extend to the periphery with complex terminals, but are also found in ramifying terminals in the pericentral region and simple terminals in the center of the cornea. Neurons expressing TRPV1 colocalize with CGRP and ScgII and extend to the corneal surface as ramifying and simple termini. Neurons expressing TRPA1 colocalize with SCG3 and NF200 and terminate in the stroma and sub-basal regions.
The expression pattern of TRPV1, TRPA1, and TRPM8 varies in different species and in different neuronal populations. In rat DRG, there are reports of colocalization of TRPV1 and TRPA1 in C fibers and in Aδ fibers [30]. In guinea pig gastrointestinal tract and esophagus, C fibers coexpress TRPV1,TRPA1, and TRPM8 with CGRP [31]. In human axons, Aδ fibers were reported to contain TRPA1 and TRPV1, as are mouse dural afferents [29]. A recent paper showed colocalization of TRPV1 and TRPM8 in cell bodies whose axons project to the cornea in mice [27]. In contrast to these results, in the mouse cornea we observed the expression of TRPV1, TRPA1, and TRPM8 to be in separate axons, and CGRP expression was confined to TRPV1 axons and not TRPM8 C fibers or TRPA1 Aδ fibers.
It is difficult to evaluate the meaning of the reported variability in TRP channel expression patterns because studies used different species and tissues [29-31] along with different techniques, including in situ hybridization [3,30], IHC of cell bodies in the ganglion of retrograde labeled peripheral afferents [3,27], and IHC of the axon terminals [5]. In addition, discrepancies have been shown with IHC of the soma versus immunolabeling of the axon terminals [41]. The different antibodies used may also explain differences among studies.
It is somewhat surprising that TRPA1 is not found in the epithelial nerves, where sensory transduction typically takes place. It is always possible that the TRPA1 protein in the epithelial regions could have undergone proteolysis or exists in a conformation inaccessible to the primary antibody, or that there are trace amounts of TRPA1 in the epithelium below the threshold of detection. Consistent with the low expression of TRPA1 observed in the epithelium, functional studies have found that TRPA1 activators activate only a few polymodal terminals from mouse and guinea pig corneas [42,43]. As the mouse cornea contains unmyelinated nerves deep in the cornea close to the endothelium, it is also possible that these fibers can respond to stimuli from the anterior direction. However, it was recently demonstrated that TRPA1 is not important for cold nociception in the cornea, as no difference in reflex blinking or eye closing was observed in Trpa1−/− mice [27]. The exact role that TRPA1 plays in fibers in the stroma is not yet known, although a role in mediating neovascularization and macrophage infiltration following injury has been identified [44].
The three different terminal morphologies described by Alamri et al. [3] were observed in this study: simple, ramifying, and complex. The morphology of TRPM8 afferents and TRPV1/CGRP terminals was distinctly different, possibly due to the different functional roles of the TRPs in the cornea. TRPM8 functions as a humidity sensor, detecting eye wetness involved in tear production, whereas TRPV1 axons are more sensitive to heat and chemical mediators. TRPM8 terminals were complex around the periphery and ramifying pericentrally. The receptive field of each terminal is very small [45,46]; by increasing the surface area of functional receptors by complex branching, minute decreases in temperature due to evaporation are likely to result in the transmission of a signal [36,47]. TRPV1/CGRP C-terminals also protruded through the epithelial layers to the corneal surface, winding between the cells and increasing their surface area to chemical mediators from the environment, released from the epithelial cells or from resident or infiltrating immune cells. A similar morphology for TRPV1-positive fibers in the cornea of the guinea pig was reported by Alamri et al. [3], although they did not find CGRP in simple fibers as we report in this study. This may be a species difference. TRPA1, unlike TRPV1 and TRPM8, was not present in fibers extending to the cell surface and may serve more of a mechanosensory role rather than a chemical or thermal role in the cornea.
The TRP channel proteins in this study in the cornea appear to localize to intracellular compartments, as also reported for TRP channels in DRG neurons [48,49]. Functional and IHC studies demonstrated that inflammatory mediators increase trafficking of functional TRPV1, TRPM8, and TRPA1 to the cell surface simultaneously with LDCV neuropeptides [20]. Chromogranin A and SCG3 are required for vesicle biogenesis in mast cells and have been shown to negatively regulate the inositol triphosphate (IP3) receptor Ca2+ transport [50,51]. To date, we have found no reports of SCG3 affecting TRPA1 activity, but the present study data demonstrating colocalization to the same axons in the cornea, just as TRPA1 and SCG3 are colocalized in mast cells, suggest that SCG3 and TRPA1 may be components of the same vesicular membrane compartments. SCG3 was not found in neuropeptide-containing C fibers (Figure 8).
ScgII is a prohormone processed into several other peptides, including secretoneurin, which has been shown to be present in CGRP-containing neurons in the spinal cord and the periphery [52]. IHC, electron microscopy (EM), and proteomic studies suggest colocalization of ScgII, CGRP, and TRPV1 in the same vesicles in C fibers. The present study data clearly suggested colocalization of TRPV1 and ScgII, and of CGRP and TRPV1, but a definitive result is beyond the limits of resolution with the confocal microscopy used (about 150 nm in x and y and about 350 nm in z), as the size of LDCVs ranges from 150 to 300 nm.
The present results suggest that the expression pattern of TRP channels in the mouse cornea is unique compared to other tissues innervated by polymodal sensory afferents. Whereas the colocalization of CGRP and TRPV1 in axon terminals is typically observed in other tissues, we did not find CGRP in TRPM8 axons (Figure 3) or TRPA1 in TRPV1-positive C fibers (Figure 2), and we did not observe TRPV1 in NF200-/TRPA1-positive Aδ fibers (Figure 2, Figure 3A). Mouse corneas from wild-type and appropriate transgenics will serve as an excellent model to study the effects of inflammatory mediators and their influence on neuropeptide vesicle and TRP channel trafficking to the cell surface in the separate populations of sensory neurons expressing TRPV1, TRPM8, or TRPA1.
Acknowledgments
This study was supported by the National Eye Institute of the National Institutes of Health under award number R01EY017564 to S.E. Gordon, and additionally by the Scan Design Foundation Innovative Pain Research award to L.C. Schecterson. We would like to thank John Bankston and members of the Gordon laboratory for many helpful discussions of the research. We thank Dr. Fred Rieke’s lab for donated excess primate corneas that were not needed for their experiments using the retina.
Appendix 1. Antibodies used for immunohistochemistry.
To access the data, click or select the words “Appendix 1.”
References
- 1.Sehgal N, Manchikanti L, Smith HS. Prescription opioid abuse in chronic pain: a review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician. 2012;15(Suppl):ES67–92. [PubMed] [Google Scholar]
- 2.Fields HL. The doctor’s dilemma: opiate analgesics and chronic pain. Neuron. 2011;69:591–4. doi: 10.1016/j.neuron.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alamri A, Bron R, Brock JA, Ivanusic JJ. Transient receptor potential cation channel subfamily V member 1 expressing corneal sensory neurons can be subdivided into at least three subpopulations. Front Neuroanat. 2015;9:71. doi: 10.3389/fnana.2015.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canner JP, Linsenmayer TF, Kubilus JK. Developmental regulation of trigeminal TRPA1 by the cornea. Invest Ophthalmol Vis Sci. 2014;56:29–36. doi: 10.1167/iovs.14-15035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parra A, Madrid R, Echevarria D, del Olmo S, Morenilla-Palao C, Acosta MC, Gallar J, Dhaka A, Viana F, Belmonte C. Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. Nat Med. 2010;16:1396–9. doi: 10.1038/nm.2264. [DOI] [PubMed] [Google Scholar]
- 6.Caterina MJ. Transient receptor potential ion channels as participants in thermosensation and thermoregulation. Am J Physiol Regul Integr Comp Physiol. 2007;292:R64–76. doi: 10.1152/ajpregu.00446.2006. [DOI] [PubMed] [Google Scholar]
- 7.Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, Koltzenburg M, Basbaum AI, Julius D. Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science. 2000;288:306–13. doi: 10.1126/science.288.5464.306. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Kang D, Xu J, Lake M, Hogan JO, Sun C, Walter K, Yao B, Kim D. Species differences and molecular determinant of TRPA1 cold sensitivity. Nat Commun. 2013;4:2501. doi: 10.1038/ncomms3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bautista DM, Siemens J, Glazer JM, Tsuruda PR, Basbaum AI, Stucky CL, Jordt SE, Julius D. The menthol receptor TRPM8 is the principal detector of environmental cold. Nature. 2007;448:204–8. doi: 10.1038/nature05910. [DOI] [PubMed] [Google Scholar]
- 10.Caspani O, Heppenstall PA. TRPA1 and cold transduction: an unresolved issue? J Gen Physiol. 2009;133:245–9. doi: 10.1085/jgp.200810136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.del Camino D, Murphy S, Heiry M, Barrett LB, Earley TJ, Cook CA, Petrus MJ, Zhao M, D’Amours M, Deering N, Brenner GJ, Costigan M, Hayward NJ, Chong JA, Fanger CM, Woolf CJ, Patapoutian A, Moran MM. TRPA1 contributes to cold hypersensitivity. J Neurosci. 2010;30:15165–74. doi: 10.1523/JNEUROSCI.2580-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fajardo O, Meseguer V, Belmonte C, Viana F. TRPA1 channels mediate cold temperature sensing in mammalian vagal sensory neurons: pharmacological and genetic evidence. J Neurosci. 2008;28:7863–75. doi: 10.1523/JNEUROSCI.1696-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karashima Y, Talavera K, Everaerts W, Janssens A, Kwan KY, Vennekens R, Nilius B, Voets T. TRPA1 acts as a cold sensor in vitro and in vivo. Proc Natl Acad Sci USA. 2009;106:1273–8. doi: 10.1073/pnas.0808487106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowlton WM, Bifolck-Fisher A, Bautista DM, McKemy DD. TRPM8, but not TRPA1, is required for neural and behavioral responses to acute noxious cold temperatures and cold-mimetics in vivo. Pain. 2010;150:340–50. doi: 10.1016/j.pain.2010.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwan KY, Allchorne AJ, Vollrath MA, Christensen AP, Zhang DS, Woolf CJ, Corey DP. TRPA1 contributes to cold, mechanical, and chemical nociception but is not essential for hair-cell transduction. Neuron. 2006;50:277–89. doi: 10.1016/j.neuron.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 16.Memon T, Chase K, Leavitt LS, Olivera BM, Teichert RW. TRPA1 expression levels and excitability brake by KV channels influence cold sensitivity of TRPA1-expressing neurons. Neuroscience. 2017;353:76–86. doi: 10.1016/j.neuroscience.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyake T, Nakamura S, Zhao M, So K, Inoue K, Numata T, Takahashi N, Shirakawa H, Mori Y, Nakagawa T, Kaneko S. Cold sensitivity of TRPA1 is unveiled by the prolyl hydroxylation blockade-induced sensitization to ROS. Nat Commun. 2016;7:12840. doi: 10.1038/ncomms12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ran C, Hoon MA, Chen X. The coding of cutaneous temperature in the spinal cord. Nat Neurosci. 2016;19:1201–9. doi: 10.1038/nn.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jordt SE, Bautista DM, Chuang HH, McKemy DD, Zygmunt PM, Högestätt ED, Meng ID, Julius D. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature. 2004;427:260–5. doi: 10.1038/nature02282. [DOI] [PubMed] [Google Scholar]
- 20.Ferrandiz-Huertas C, Mathivanan S, Wolf CJ, Devesa I, Ferrer-Montiel A. Trafficking of ThermoTRP Channels. Membranes (Basel) 2014;4:525–64. doi: 10.3390/membranes4030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flynn R, Chapman K, Iftinca M, Aboushousha R, Varela D, Altier C. Targeting the transient receptor potential vanilloid type 1 (TRPV1) assembly domain attenuates inflammation-induced hypersensitivity. J Biol Chem. 2014;289:16675–87. doi: 10.1074/jbc.M114.558668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stein AT, Ufret-Vincenty CA, Hua L, Santana LF, Gordon SE. Phosphoinositide 3-kinase binds to TRPV1 and mediatesNGF-stimulated TRPV1 trafficking to the plasma membrane. J Gen Physiol. 2006;128:509–22. doi: 10.1085/jgp.200609576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Belmonte C, Acosta MC, Merayo-Lloves J, Gallar J. What Causes Eye Pain? Curr Ophthalmol Rep. 2015;3:111–21. doi: 10.1007/s40135-015-0073-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shaheen BS, Bakir M, Jain S. Corneal nerves in health and disease. Surv Ophthalmol. 2014;59:263–85. doi: 10.1016/j.survophthal.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan XQ, Gonzalez JA, Chang S, Chacko S, Wein AJ, Malykhina AP. Experimental colitis triggers the release of substance P and calcitonin gene-related peptide in the urinary bladder via TRPV1 signaling pathways. Exp Neurol. 2010;225:262–73. doi: 10.1016/j.expneurol.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharrad DF, Hibberd TJ, Kyloh MA, Brookes SJ, Spencer NJ. Quantitative immunohistochemical co-localization of TRPV1 and CGRP in varicose axons of the murine oesophagus, stomach and colorectum. Neurosci Lett. 2015;599:164–71. doi: 10.1016/j.neulet.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 27.Li F, Yang W, Jiang H, Guo C, Huang AJW, Hu H, Liu Q. TRPV1 activity and substance P release are required for corneal cold nociception. Nat Commun. 2019;10:5678. doi: 10.1038/s41467-019-13536-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katagiri A, Thompson R, Rahman M, Okamoto K, Bereiter DA. Evidence for TRPA1 involvement in central neural mechanisms in a rat model of dry eye. Neuroscience. 2015;290:204–13. doi: 10.1016/j.neuroscience.2015.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang D, Li S, Dhaka A, Story GM, Cao YQ. Expression of the transient receptor potential channels TRPV1, TRPA1 and TRPM8 in mouse trigeminal primary afferent neurons innervating the dura. Mol Pain. 2012;8:66. doi: 10.1186/1744-8069-8-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobayashi K, Fukuoka T, Obata K, Yamanaka H, Dai Y, Tokunaga A, Noguchi K. Distinct expression of TRPM8, TRPA1, and TRPV1 mRNAs in rat primary afferent neurons with adelta/c-fibers and colocalization with trk receptors. J Comp Neurol. 2005;493:596–606. doi: 10.1002/cne.20794. [DOI] [PubMed] [Google Scholar]
- 31.Yu X, Yu M, Liu Y, Yu S. TRP channel functions in the gastrointestinal tract. Semin Immunopathol. 2016;38:385–96. doi: 10.1007/s00281-015-0528-y. [DOI] [PubMed] [Google Scholar]
- 32.Henriksson JT, McDermott AM, Bergmanson JP. Dimensions and morphology of the cornea in three strains of mice. Invest Ophthalmol Vis Sci. 2009;50:3648–54. doi: 10.1167/iovs.08-2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dhaka A, Earley TJ, Watson J, Patapoutian A. Visualizing cold spots: TRPM8-expressing sensory neurons and their projections. J Neurosci. 2008;28:566–75. doi: 10.1523/JNEUROSCI.3976-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez JY, White DJ, Hartenstein V, Eliceiri K, Tomancak P, Cardona A. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–82. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Acosta MC, Luna C, Quirce S, Belmonte C, Gallar J. Corneal sensory nerve activity in an experimental model of UV keratitis. Invest Ophthalmol Vis Sci. 2014;55:3403–12. doi: 10.1167/iovs.13-13774. [DOI] [PubMed] [Google Scholar]
- 36.Quallo T, Vastani N, Horridge E, Gentry C, Parra A, Moss S, Viana F, Belmonte C, Andersson DA, Bevan S. TRPM8 is a neuronal osmosensor that regulates eye blinking in mice. Nat Commun. 2015;6:7150. doi: 10.1038/ncomms8150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alamri AS, Wood RJ, Ivanusic JJ, Brock JA. The neurochemistry and morphology of functionally identified corneal polymodal nociceptors and cold thermoreceptors. PLoS One. 2018;13:e0195108. doi: 10.1371/journal.pone.0195108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartolomucci A, Possenti R, Mahata SK, Fischer-Colbrie R, Loh YP, Salton SR. The extended granin family: structure, function, and biomedical implications. Endocr Rev. 2011;32:755–97. doi: 10.1210/er.2010-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helle KB. Regulatory peptides from chromogranin A and secretogranin II: putative modulators of cells and tissues involved in inflammatory conditions. Regul Pept. 2010;165:45–51. doi: 10.1016/j.regpep.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 40.Goswami SC, Mishra SK, Maric D, Kaszas K, Gonnella GL, Clokie SJ, Kominsky HD, Gross JR, Keller JM, Mannes AJ, Hoon MA, Iadarola MJ. Molecular signatures of mouse TRPV1-lineage neurons revealed by RNA-Seq transcriptome analysis. J Pain. 2014;15:1338–59. doi: 10.1016/j.jpain.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharrad DF, Chen BN, Brookes SJ. Neurochemical coding compared between varicose axons and cell bodies of myenteric neurons in the guinea-pig ileum. Neurosci Lett. 2013;534:171–6. doi: 10.1016/j.neulet.2012.10.049. [DOI] [PubMed] [Google Scholar]
- 42.Acosta MC, Luna C, Quirce S, Belmonte C, Gallar J. Changes in sensory activity of ocular surface sensory nerves during allergic keratoconjunctivitis. Pain. 2013;154:2353–62. doi: 10.1016/j.pain.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez-Gonzalez O, Bech F, Gallar J, Merayo-Lloves J, Belmonte C. Functional Properties of Sensory Nerve Terminals of the Mouse Cornea. Invest Ophthalmol Vis Sci. 2017;58:404–15. doi: 10.1167/iovs.16-20033. [DOI] [PubMed] [Google Scholar]
- 44.Usui-Kusumoto K, Iwanishi H, Ichikawa K, Okada Y, Sumioka T, Miyajima M, Liu CY, Reinach PS, Saika S. Suppression of neovascularization in corneal stroma in a TRPA1-null mouse. Exp Eye Res. 2019;181:90–7. doi: 10.1016/j.exer.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 45.Hirata H, Fried N, Oshinsky ML. Quantitative characterization reveals three types of dry-sensitive corneal afferents: pattern of discharge, receptive field, and thermal and chemical sensitivity. J Neurophysiol. 2012;108:2481–93. doi: 10.1152/jn.00523.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.MacIver MB, Tanelian DL. Free nerve ending terminal morphology is fiber type specific for A delta and C fibers innervating rabbit corneal epithelium. J Neurophysiol. 1993;69:1779–83. doi: 10.1152/jn.1993.69.5.1779. [DOI] [PubMed] [Google Scholar]
- 47.Hall DH, Treinin M. How does morphology relate to function in sensory arbors? Trends Neurosci. 2011;34:443–51. doi: 10.1016/j.tins.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shang S, Zhu F, Liu B, Chai Z, Wu Q, Hu M, Wang Y, Huang R, Zhang X, Wu X, Sun L, Wang Y, Wang L, Xu H, Teng S, Liu B, Zheng L, Zhang C, Zhang F, Feng X, Zhu D, Wang C, Liu T, Zhu MX, Zhou Z. Intracellular TRPA1 mediates Ca2+ release from lysosomes in dorsal root ganglion neurons. J Cell Biol. 2016;215:369–81. doi: 10.1083/jcb.201603081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Turner H, Fleig A, Stokes A, Kinet JP, Penner R. Discrimination of intracellular calcium store subcompartments using TRPV1 (transient receptor potential channel, vanilloid subfamily member 1) release channel activity. Biochem J. 2003;371:341–50. doi: 10.1042/BJ20021381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choe CU, Harrison KD, Grant W, Ehrlich BE. Functional coupling of chromogranin with the inositol 1,4,5-trisphosphate receptor shapes calcium signaling. J Biol Chem. 2004;279:35551–6. doi: 10.1074/jbc.M311261200. [DOI] [PubMed] [Google Scholar]
- 51.Prasad P, Yanagihara AA, Small-Howard AL, Turner H, Stokes AJ. Secretogranin III directs secretory vesicle biogenesis in mast cells in a manner dependent upon interaction with chromogranin A. J Immunol. 2008;181:5024–34. doi: 10.4049/jimmunol.181.7.5024. [DOI] [PubMed] [Google Scholar]
- 52.Marksteiner J, Mahata SK, Pycha R, Mahata M, Saria A, Fischer-Colbrie R, Winkler H. Distribution of secretoneurin immunoreactivity in the spinal cord and lower brainstem in comparison with that of substance P and calcitonin gene-related peptide. J Comp Neurol. 1994;340:243–54. doi: 10.1002/cne.903400209. [DOI] [PubMed] [Google Scholar]