Abstract
Objectives
Assault by strangulation has the potential for severe brain injury or death. The objectives of this study were to describe the profile of individuals who had strangulation-related emergency department (ED) or acute care visits, and to explore 1-year readmission outcomes among survivors.
Methods
A population-based retrospective cohort study was conducted using health administrative data in Ontario, Canada. Adults aged 15 years and older who were seen in the ED or acute care with assault by strangulation between fiscal years 2002/2003 and 2016/2017 were included in the study. Bivariate analyses were conducted to compare the patient profile and subsequent readmissions within 1 year of discharge, stratified by sex.
Results
A total of 586 patients were included in the study. The majority of these patients were seen in the ED (93%), predominantly female (70%), aged ≤ 39 years (68%), and of lower income quintiles of ≤ 3 (73%). Of the 579 patients who survived the initial admission, 52% had subsequent ED readmission and 21% had acute care readmission within 1 year. In sex-stratified analyses, a higher proportion of females were between 20 to 39 years (58.7% vs. 44.1%, p = 0.001), discharged home (88% vs. 81%, p < 0.001), and had ED readmission within 1 year of discharge (56% vs. 17%, p = 0.002). Males had comparatively higher 1-year acute care readmissions.
Conclusion
The study shows high readmissions with sex differences among individuals with an assault by strangulation, suggesting sex-specific approach to health care practices to support the needs of this vulnerable population, thus reducing health system inefficiencies.
Keywords: Strangulation, Readmission, Acute care, Emergency department
Résumé
Objectifs
Une agression par strangulation peut entraîner de graves lésions cérébrales ou la mort. Les objectifs de cette étude étaient de décrire le profil des personnes ayant eu une visite à l'urgence liée à une strangulation ou aux consultations de soins aigus, et d'explorer les résultats de réadmission après un an chez les survivants.
Méthodes
Une étude de cohorte rétrospective basée sur la population a été menée à l'aide de données administratives sur la santé en Ontario, au Canada. Les adultes âgés de 15 ans et plus qui ont été vus aux urgences ou en soins aigus avec assaut par strangulation entre les années 2002/03 et 2016/17 ont été inclus dans l'étude. Des analyses bivariées ont été effectuées pour comparer le profil du patient et les réadmissions ultérieures dans l'année suivant son congé, stratifiées par sexe.
Résultats
Un total de 586 patients ont été inclus dans l'étude. La majorité de ces patients ont été vus aux urgences (93 %), principalement des femmes (70 %), âgées de ≤ 39 ans (68 %) et des quintiles de revenus inférieurs à ≤3 (73 %). Parmi les 579 patients qui ont survécu à l'admission initiale, 52 % ont été réadmis ultérieurement au service d'urgence et 21 % ont été réadmis en soins aigus durée au bout d'un an. Dans les analyses stratifiées par sexe, une proportion plus élevée de femmes avaient entre 20 et 39 ans (58,7 % contre 44,1 %, p = 0,001), avaient été renvoyées à la maison (88 % contre 81 %, p < 0,001) et avaient été réadmises à l'urgence 1 année de sortie (56 % contre 17 %, p = 0,002). Les hommes avaient comparativement plus de réadmissions en soins aigus durée après un an.
Conclusion
L'étude révèle un nombre élevé de réadmissions avec différences de sexe chez les individus agressés par strangulation, suggérant une approche des pratiques de soins de santé spécifique au sexe pour répondre aux besoins de cette population vulnérable, réduisant ainsi les inefficiences du système de santé.
Mots-clés: Strangulation, Réadmission, Soins actifs, Service des urgences
Introduction
Assault by strangulation is a distinct mechanism of violence that has the potential for severe brain injury or death. Strangulation is defined as external pressure to the neck (ligature or manual), closing blood vessels and/air passages, and deprivation of oxygen to the brain and body (Anscombe & Knight, 1996; Sorenson, Joshi, & Sivitz, 2014). The asphyxia and ischemia that result from vascular and/or airway closure can cause unconsciousness, brain injuries such as hypoxic-ischemic brain injury or other injuries, resulting in serious morbidity and mortality (Clarot, Vaz, Papin, & Proust, 2005; Dunn & Smock, 2017). While the prevalence of strangulation has not been fully determined, current estimates show extreme sex disparity with rates 13 times higher in females than in males (Breiding et al., 2014; Sorenson et al., 2014). It is exceedingly prevalent in women who are in an abusive relationship or with a prior history of intimate partner violence (IPV) and in the age group 30–39 years (Strack, McClane, & Hawley, 2001; Zilkens et al., 2016). Survivors often experience severe negative health outcomes with various physical, mental, and social consequences (Clarot et al., 2005; Joshi, Thomas, & Sorenson, 2012; Le Blanc-Louvry, Papin, Vaz, & Proust, 2013). It is estimated that 2.5% of traumatic deaths worldwide (Wahlen & Thierbach, 2002) and up to 10% of violent deaths in North America (Funk & Schuppel, 2003; Turkel, 2007) are caused by strangulation. In Canada, one in four individuals experience violence over their lifetime (Burczycka & Conroy, 2018), 10–50% of them reported strangulation (Barrett & St Pierre, 2011; Burczycka & Conroy, 2018; Sorenson et al., 2014), and 13% of women killed by their partners were strangled to death (Burczycka & Conroy, 2018; Porter, 2016), making this a significant public health concern.
Population-level data on survivors of strangulation and the damaging impacts of injury on their subsequent health care utilization is currently lacking. Existing population-based studies are restricted to victims of violence (Brink, 2009) or have mixed strangulation as part of other suffocation injuries, including suicide and self-inflicted asphyxiation (Sasso, Bachir, & El Sayed, 2018). Much of the other extant literature on strangulation is on women within the context of IPV or homicide, and is based on case reports (Clarot et al., 2005; Di Paolo et al., 2009; Funk & Schuppel, 2003; Le Blanc-Louvry et al., 2013), epidemiological surveys (Glass et al., 2008; Joshi et al., 2012; Messing, Patch, Wilson, Kelen, & Campbell, 2018), or mortuary/forensic studies identifying cause of death (Abrahams, Mathews, Lombard, Martin, & Jewkes, 2017; Hlavaty & Sung, 2017; Zilkens et al., 2016). There are limited data on strangulation among men even though men are increasingly being exposed to partner violence (Archer, 2000; Carmo, Grams, & Magalhaes, 2011; Mills, Mills, Taliaferro, Zimbler, & Smith, 2003). As the demographics of victims and the epidemiology of violence are likely to differ substantially by sex (Brink, 2009), it is important to focus on sex differences in this population. Moreover, seeking help following strangulation varies widely and the emergency department (ED) is an easily accessible point of entry to health care for these patients (Ernst, Nick, Weiss, Houry, & Mills, 1997). However, current studies are limited in their ability to provide reliable data on patients seeking care at an ED or acute care and subsequently documented as having an assault by strangulation. Besides, no study has looked at subsequent readmission and reasons for readmission in this group of patients, even though the survivors are highly susceptible to another abrupt violence and are more likely to seek subsequent health care within a short period (Glass et al., 2008). Readmission within 30 days and 1 year are widely accepted as a measure of hospital quality and patient care (Wu & Hall, 2018). To develop a knowledge-to-practice network for prevention strategies, understanding this vulnerable population and prospectively assessing their health care interactions is crucial.
The objectives of this study were to describe the profile of patients who had assault by strangulation-related ED or acute care visits, and to explore subsequent 30-day and 1-year readmissions, stratified by sex.
Methods
Study design
A retrospective cohort study was conducted using population-based health administrative data in Ontario, Canada, between fiscal years 2002/2003 and 2016/2017 (i.e., between April 1, 2002 and March 31, 2017).
Data sources
The Ontario health administrative data capture publicly funded health care services of all residents in the province, representing 39% of the Canadian population (“Statistics Canada Census Profile, 2016 Census”). The National Ambulatory Care Reporting System (NACRS) database contains data on ED service utilization (National Ambulatory Care Reporting System (NACRS) n.d.), the Discharge Abstract Database (DAD) captures information from acute care hospitalization (Acute Care n.d.), the Ontario Mental Health Reporting System (OMHRS) database captures information specific to psychiatric hospitalizations since 2005, and the Ontario Health Insurance Plan (OHIP) database captures data on outpatient visits, including diagnosis, types of physician’s services, and laboratory services (“Health Analyst’s Toolkit. Toronto: Ontario Ministry of Health and Long-Term Care 2012”). All these databases contain patient demographics and clinical data, including diagnoses for up to 24 diagnostic codes using the International Classification of Disease version 10 (ICD-10) or version 9 (ICD-9) codes. The NACRS and DAD databases were used to identify the study cohort. The NACRS, DAD, and OMHRS databases were used to identify the outcome of readmissions. All four databases were used to identify patient clinical characteristics.
ICES (formerly the Institute for Clinical Evaluative Sciences) holds these health administrative databases, and risk-reduced linkable data necessary for the study are provided through a secured platform.
Study cohort
A cohort of adult patients (age ≥ 15 years) with a diagnosis of “assault by strangulation and suffocation” (ICD-10 code X91) in any of the 24 diagnostic fields was identified from the NACRS and DAD databases.
Outcomes
The outcomes of interest were all-cause readmission to ED (NACRS database) or acute care (DAD/OMHRS database) within 30 days and 1 year of strangulation. In the case of multiple readmissions, only the first admission and the corresponding diagnoses were considered. The reasons for readmission were categorized based on the ICD chapter headings due to the broad spectrum of diagnostic codes.
Patient characteristics
The patient characteristics were chosen based on previously reported studies on violence and limited by availability from administrative health data resources. These variables were categorized into two groups, demographic and clinical characteristics.
Demographic characteristics included (a) age, (b) sex, (c) rural residence (yes/no) and (d) neighbourhood income quintile at the census tract level from 1 (lowest) to 5 (highest).
Clinical characteristics included
Comorbidity score using Johns Hopkins Aggregated Diagnosis Groups (ADGs) (The Johns Hopkins Adjusted Clinical Groups Technical Reference Guide, version 10. Baltimore, MD; Johns Hopkins University 2009) (Austin, van Walraven, Wodchis, Newman, & Anderson, 2011; Austin & Walraven, 2011), determined based on diagnoses 2 years prior to index admission, with higher score indicating greater comorbidity illness (0–2, 3–5, and > 5);
History of psychiatric disorders any time prior to index admission (yes/no), determined based on ED/acute care visits for psychiatric disorders ((NACRS/DAD ICD-9 codes 290–318 and ICD-10 codes F00-F99) or any admissions from OMHRS (Jacob, Stock, Chan, Colantonio, & Cullen, 2019; Zaheer et al., 2018);
History of alcohol use disorders any time prior to index admission (yes/no), determined by including subjects who were diagnosed with alcohol use disorders in outpatient setting (OHIP ICD-9 code 291 or 303) or ED/acute care setting (NACRS/DAD ICD-9 codes 303, 291 or ICD-10 codes F100-F109, G312, G621, I426, K292, K700-K703, K709, R780, or T510), or psychiatric inpatient setting (OMHRS ICD-9 code 291 or 303) (Zaheer et al., 2018);
Diagnosis of “assault by bodily force” along with strangulation (yes/no), determined based on diagnosis at the time of index admission to ED/acute care (NACRS/DAD ICD-10 code Y04);
Diagnosis of “traumatic brain injury” (TBI) along with strangulation (yes/no), determined based on diagnosis at the time of index admission to ED/acute care (NACRS/DAD ICD-10 codes S00-S09, T00.0, T01.0, T02.0, T03.0, T04.0, T06.0, T90) (Chan, Zagorski, Parsons, & Colantonio, 2013);
Diagnosis of “other injury and poisoning” along with strangulation (yes/no), determined based on diagnosis at the time of index admission to ED/acute care (NACR/DAD ICD-10 codes S-T);
Prior health care utilization (non-user/healthy, low, moderate, high), as measured by Resource Utilization Bands (ACG-RUB) (“The Johns Hopkins Adjusted Clinical Groups Technical Reference Guide, version 10. Baltimore, MD; Johns Hopkins University” 2009);
Triage category at index ED admission (emergent/less emergent);
Length of stay (LOS) in hours at index ED admission (≤ 1, 2–3, > 3);
Discharge disposition at index admission to ED/acute care (discharged home, signed out, transferred to another facility, died);
Fiscal year of index admission to ED/acute care.
Reports that conditions such as psychiatric disorders, alcohol use disorders, and TBI are associated with violence prompted use of these specific comorbidities (Goldin, Haag, & Trott, 2016; Panyayong, Tantirangsee, Bogoian, & Thai National Mental Health Survey, 2018; Smith, Homish, Leonard, & Cornelius, 2012).
Statistical analysis
We performed statistical analysis with SAS (version 9.3) statistic software package. The description of the demographic and clinical characteristics was presented as frequencies and percentages for the categorical variables, mean and SD for continuous variables. Bivariate analyses were done to compare the differences between sexes, chi-square/Mantel-Haenszel test for categorical/ordinal variables and t test for continuous variables. Difference at the value of p < 0.05 was considered statistically significant.
This study was approved by the University Health Network Research Ethics Board.
Results
Patient characteristics
A total of 586 unique patients with a diagnosis of “assault by strangulation” were included in the study. The majority of these patients were identified from the ED setting (92%). Of the remaining 8% who were identified from acute care, 86% had a preceding ED visit that led to the acute care admission, but the strangulation assault was not identified in their initial emergency care. Most patients (86%) were treated and released home. Overall in-hospital mortality, at either ED or acute care, was 1.2%.
Table 1 shows the demographic and clinical characteristics of patients who had an assault by strangulation, stratified by sex. Over half of the patients (68.5%) were younger than 40 years, female (69.8%), and of lower income quintiles of ≤ 3 (73%). A higher proportion of females were of age group 20–39 years, whereas more males were found in either 15–19 years or ≥ 40 years.
Table 1.
Characteristics of patients who had an assault by strangulation, stratified by sex
| Variable | Value | Total | Female | Male | P value |
|---|---|---|---|---|---|
| N = 586 | N = 409 | N = 177 | |||
| Demographic characteristics | |||||
| Age group in years | 15–19 | 83 (14.2%) | 53 (13.0%) | 30 (16.9%) | 0.006 |
| 20–29 | 192 (32.8%) | 141 (34.5%) | 51 (28.8%) | ||
| 30–39 | 126 (21.5%) | 99 (24.2%) | 27 (15.3%) | ||
| 40–49 | 113 (19.3%) | 76 (18.6%) | 37 (20.9%) | ||
| ≥ 50 | 72 (12.3%) | 40 (9.8%) | 32 (18.1%) | ||
| Income quintile | 1 (lowest) | 176 (30.0%) | 132 (32.3%) | 44 (24.9%) | 0.394 |
| 2 | 143 (24.4%) | 99 (24.2%) | 44 (24.9%) | ||
| 3 | 109 (18.6%) | 70 (17.1%) | 39 (22.0%) | ||
| 4 | 93 (15.9%) | 63 (15.4%) | 30 (16.9%) | ||
| 5 (highest) | 65 (11.1%) | 45 (11.0%) | 20 (11.3%) | ||
| Rural area of residence | Yes | 82 (14.0%) | 56 (13.7%) | 26 (14.7%) | 0.749 |
| Clinical characteristics | |||||
| ADG comorbidity score | 0–2 | 197 (33.6%) | 117 (28.6%) | 80 (45.2%) | < 0.001 |
| 3–5 | 214 (36.5%) | 161 (39.4%) | 53 (29.9%) | ||
| > 5 | 175 (29.9%) | 131 (32.0%) | 44 (24.9%) | ||
| Mean ± SD | 4.16 ± 3.08 | 4.45 ± 3.10 | 3.50 ± 2.96 | < 0.001 | |
| History of psychiatric disorders | 175 (29.9%) | 126 (30.8%) | 49 (27.7%) | 0.448 | |
| History of alcohol use disorders | 85 (14.5%) | 51 (12.5%) | 34 (19.2%) | 0.033 | |
| Assault by bodily force along with strangulation | 86 (14.7%) | 75 (18.3%) | 11 (6.2%) | < 0.001 | |
| TBI injury along with strangulation | 98 (16.7%) | 71 (17.4%) | 27 (15.3%) | 0.531 | |
| Other injury, poisoning along with strangulation | 533 (91.0%) | 382 (93.4%) | 151 (85.3%) | 0.002 | |
| Prior health care use | Non-user/healthy | 101 (17.2%) | 55 (13.4%) | 46 (26.0%) | < 0.001 |
| Low user | 102 (17.4%) | 66 (16.1%) | 36 (20.3%) | ||
| Moderate user | 297 (50.7%) | 220 (53.8%) | 77 (43.5%) | ||
| High/very high user | 86 (14.7%) | 68 (16.6%) | 18 (10.2%) | ||
| Triage category at ED | Emergent | 399 (68.1%) | 294 (71.9%) | 105 (59.3%) | 0.003 |
| Less emergent | 187 (31.9%) | 115 (28.1%) | 72 (40.7%) | ||
| ED LOS in hours | ≤ 1 | 227 (38.7%) | 138 (33.7%) | 89 (50.3%) | < 0.001 |
| 2–3 | 196 (33.4%) | 159 (38.9%) | 37 (20.9%) | ||
| > 3 | 163 (27.8%) | 112 (27.4%) | 51 (28.8%) | ||
| Mean ± SD | 2.66 ± 3.27 | 2.48 ± 2.21 | 3.13 ± 4.99 | 0.037 | |
| Discharge disposition | Discharged home | 504 (86.0%) | 360 (88.0%) | 144 (81.4%) | 0.002 |
| Signed out | 28 (4.8%) | ||||
| Transferred to another care facility | 47 (8.0%) | 22 (5.4%) | 25 (14.1%) | ||
| Died | 7 (1.2%) | ||||
ADG Aggregated diagnosis groups, TBI Traumatic brain injury, ED Emergency department, LOS Length of stay
Compared with males, females had higher comorbidity score (4.45 ± 3.10 vs. 3.50 ± 2.96, p < 0.001), assault by bodily force (18.3% vs. 6.2%, p < 0.001), treated as emergent in ED (71.9% vs. 59.3%, p = 0.03), moderate to higher prior health care use (70.4% vs. 53.7%, p < 0.001), and discharged home (88% vs. 81%, p = 0.002). However, a higher proportion of males had alcohol use disorders (19.2% vs. 12.5%, p = 0.03) and longer ED-LOS (3.13 ± 4.99 vs. 2.48 ± 2.21, p = 0.03).
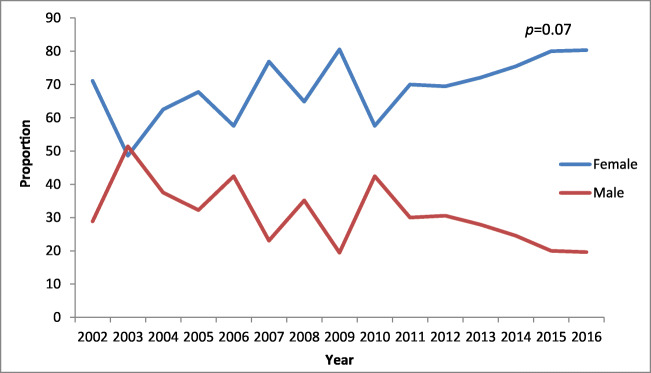
Figure 1 shows the distribution of patients by sex and year. The proportion of strangulation was higher in females throughout the study period and the difference widened over time.
Fig. 1.
Distribution of patients by sex and year
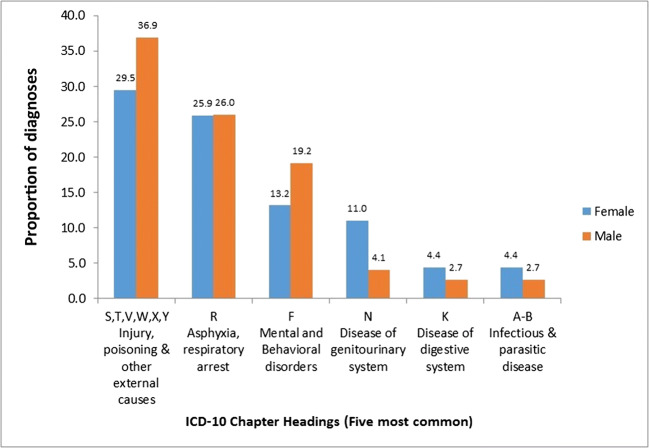
ED readmission after strangulation
Of the 579 patients who survived the index injury, 14.9% had a subsequent ED readmission at 30 days and 51.8% at 1 year of discharge (Table 2). ED readmission was higher among females compared with males at 30 days (16.8% vs. 10.3%, p = 0.04) and 1 year (56% vs. 42%, p = 0.002). The higher risk of ED readmission among females was consistent (OR 1.93, 95% CI 1.29–2.88) even after adjusting for potential confounders, including age, income quintile, ADG comorbidity score, history of alcohol use disorders, ACG-RUB, ED-triage, and ED-LOS using multivariable logistic regression models (results not shown). The most common reason for ED readmission was “injury, poisoning and other external causes” (31%), followed by respiratory arrest (26%), and mental/behavioural disorders (16%) (Fig. 2). There were only 10 patients who were readmitted to either ED or acute care for another assault by strangulation.
Table 2.
Readmissions within 1 year of strangulation, stratified by sex
| Readmissions | 30 days | 1 year | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | P value | Total | Female | Male | P value | |
| N = 579 | N = 405 | N = 174 | N = 579 | N = 405 | N = 174 | |||
| All-cause readmissions | ||||||||
| ED visits | 86 (14.9%) | 68 (16.8%) | 18 (10.3%) | 0.046 | 300 (51.8%) | 227 (56.0%) | 73 (42.0%) | 0.002 |
| Acute care | 35 (6.0%) | 16 (4.0%) | 19 (10.9%) | 0.001 | 120 (20.7%) | 79 (19.5%) | 41 (23.6%) | 0.269 |
| Mental health-related readmissions* | ||||||||
| ED visits | 44 (7.6%) | 30 (7.4%) | 14 (8.1%) | 0.791 | ||||
| Hospital admissions | 43 (7.4%) | 17 (39.5%) | 26 (14.9%) | < 0.0001 | ||||
*Mental health-related readmissions at 30 days were not shown due to small number of cases
Fig. 2.
Diagnoses at first ED visit within 1 year of strangulation, n = 300
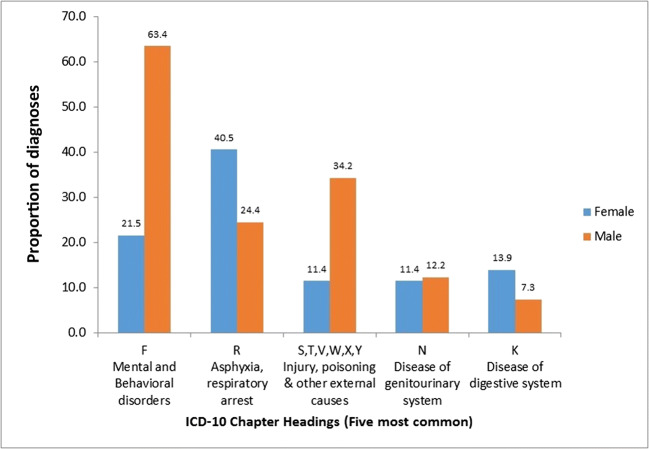
Acute care readmission after strangulation
Of the 579 patients who survived the index injury, 6% had a subsequent acute care readmission at 30 days and 20.7% at 1 year of discharge (Table 2). Compared with females, males had a higher readmission to acute care at 30 days (10.9% vs. 4.0%, p = 0.001) and at 1 year (23.6% vs. 19.5%, p = 0.26). The higher risk of acute care readmission among males was consistent (OR 0.72, 95% CI 0.45–1.15) even after adjusting for potential confounders using multivariable logistic regression models (results not shown). The most common reason for acute care readmission was mental/behavioural disorders (42%), followed by respiratory arrest (33%) (Fig. 3).
Fig. 3.
Diagnoses at first acute care visit within 1 year of strangulation, n = 120
Discussion
This is the first study to our knowledge that presents population-based data on patients with an assault by strangulation, based on ED/acute care data. Our study shows sex differences in the patient profile and subsequent readmissions after strangulation. We found that ED and acute care readmissions occurred at least once in 52% and 21%, respectively, within 1 year of strangulation assault, which is higher than expected. Interestingly, subsequent ED readmission was higher among females, whereas acute care readmissions were higher in males. The main reasons for 1-year readmissions were injury-poisoning and mental health issues.
Strangulation in males was higher in patients 40 years and over, and is consistent with findings of a study which analyzed male survivors of violence who called a domestic base helpline (Hines, Brown, & Dunning, 2007). Older men are vulnerable to violence and have reported high rates of non-fatal assaults and homicides (Logan, Haileyesus, Ertl, Rostad, & Herbst, 2019). Males 15–19 years also had a comparatively higher proportion of strangulation in this study. Reports indicate the prevalence of choking games among adolescents that involve strangulation is higher in males (Egge, Berkowitz, Toms, & Sathyavagiswaran, 2010; Re, Birkhoff, Sozzi, Andrello, & Osculati, 2015). Violence in social media, playing violent games, and cannabinoid use are some other potential factors that might increase aggressive thoughts and behaviours among male youths (Clayton, Lowry, Ashley, Wolkin, & Grant, 2017).
A higher proportion of patients in this study were discharged home, a finding that needs to be tackled with care as it is an ethical concern to release them to a potentially high-risk situation if the abuser is indeed the intimate partner. In this study, it is not clear whether assaults by strangulation are cases of IPV as we do not have data on the type of violence, or the relationship of the victim and abuser. Even though strangulation can occur any time and across genders, evidence indicates it is a highly prevalent form of IPV, particularly in women (Patch, Anderson, & Campbell, 2018; Wiebe, 2003) (Messing et al. 2018; Strack & Gwinn, 2011; Turkel, 2007). Literature suggests that one in three women experience IPV over their lifetime (Black et al., 2011) and 23–80% of these women experience at least one strangulation-related incident at the hands of their male partner (Patch et al. 2018; Wilbur et al., 2001). Based on this strong relationship between IPV and strangulation, assault against females in this study may well be due to IPV with male-to-female violence. By contrast, the male data should be addressed with caution in relation to the possibility of IPV. Existing research suggests that in female-to-male violence, females tend to use methods that are not strength dependent (Carmo et al., 2011), leaving men’s injuries to be not severe enough to seek medical treatment (Carmo et al., 2011). However, this study shows that more males were transferred to another care facility after the index admission, and had longer ED-LOS, suggesting severe injuries. While this is not what is expected in a female-to-male abuse, there is the possibility of assault by strangulation in a same-sex relationship. Literature shows transwomen sex workers are at a much higher risk of assault by an intimate partner. These findings raise interesting questions and suggest a need for more detailed investigation.
The number of individuals included in this study is lower than expected. Strangulation is thought to be highly underestimated within the context of violence for various reasons. Survivors often do not seek care or do not report that strangulation occurred due to fear, stigma, shame, cultural norms, and threats to safety by the abuser (Joshi et al., 2012; McClane, Strack, & Hawley, 2001). They also underestimate the danger or consequence of the situation (Messing et al. 2018). Moreover, the detection of strangulation can be challenging for health care providers as the physical signs and symptoms are not always obvious and can easily be missed, particularly in women, as injury can occur with very little pressure to the neck and leave no visible marks behind (Clarot et al., 2005; Faugno, Waszak, Strack, Brooks, & Gwinn, 2013). Patients reported with violence to ED are not routinely assessed for strangulation, and are often under-evaluated and not addressed with a clinically appropriate work-up (McClane et al., 2001; Valera, 2018). Studies indicate that 75% of survivors who sought hospital care did not receive medical attention subsequent to strangulation, and of those who did, only 24.4% noted that the strangulation was documented in their medical record (“Maine Commission on Domestic and Sexual Abuse. Report from the Task Group on Strangulation” 2012; Patch et al. 2018). Lack of reporting inconsistencies would also contribute to the underreporting of cases, as survivors—especially women survivors of manual strangulation—report the incident as “choking” or “throttling” even though these are different from strangulation (Joshi et al., 2012; McClane et al., 2001).
Future implications
Although many unanswered questions regarding the identification and care for strangulation remain, this study provides a framework for many future steps. Further studies are needed to answer questions, such as what services are currently provided during ED admission and who provides care and facilitates discharge planning. As “discharge home” can be more problematic when the abuser is indeed the intimate partner, it would seem that a future study should involve a chart review to complete the data obtained in this particular study. This will make improvements in the management of strangulation that will keep survivors safer and more effectively hold perpetrators accountable. The results of this study highlight the importance of initiating policies that educate both the general public and health care professionals on the consequences of strangulation. The public should be educated about the delayed sequelae and increased risk of future violence associated with strangulation (Glass et al., 2008; Strack & Gwinn, 2011). Emergency care providers should be educated about the importance of screening for strangulation when assessing abused patients and on proper documentation. Injuries to the head, neck, and face are often indicative of a violent encounter (Brink, 2009), and it is strongly recommended that health care providers consider these types of injuries as such. Considering the medical and legal implications, the health care team should also be educated on appropriate discharge planning. We recommend future studies to establish a reliable, valid, and standardized screening tool to identify strangulation in survivors of violence (Haag, Jones, Joseph, & Colantonio, 2019). In summary, more research is needed on this understudied population that would develop patient-centered and clinically effective approaches to enhance safety and care.
Strengths and limitations
Because this was a secondary data analysis using administrative data, some important information regarding strangulation was not assessed. For example, we do not have the context of strangulation such as IPV, or indication of the nature of the relationship between the survivor and offender. Further, we are limited to looking at this through a sex lens, while it may be that gender also plays a significant role in this situation, as gender expectations for women and men are different. The binary of male and female is in and of itself a limitation as the reality of life is a spectrum. Another limitation of the study is that we do not have information on the range of service providers available or accessed across various hospitals in the province. Thus, it would be difficult to explain the service delivery process or how the patients were handled in the ED/acute care given the indications of violence. We also acknowledge that the prevalence numbers shown in this study are highly understated. Our sample does not reflect the actual number of survivors who never seek care, or who sought care but were not diagnosed with an assault by strangulation, nor does it cover persons accessing care through community-based clinics. Moreover, as the inclination to contact ED increases with the seriousness of the injury, this study might underreport injuries with less serious injury. Regardless, this is the first study to provide a population-level perspective of patients specific to assault by strangulation and highlight the importance of violence prevention strategies, bringing awareness to a long-overlooked public health concern.
Conclusion
The study shows significant sex differences in patient profile and subsequent 1-year readmissions among individuals who had an assault by strangulation-related ED/acute care visit in Ontario, Canada. Results indicate high ED readmissions among females and high acute care readmissions among males within 1 year of strangulation. This underscores the need to improve health care practices related to strangulation assessment and discharge planning to support appropriate care with a sex-specific approach, thereby reducing subsequent readmissions. The study also highlights the need for further research to support the development of evidence-based optimal care for this population.
Acknowledgements
This study made use of de-identified data from the ICES Data Repository, which is managed by ICES (formerly the Institute for Clinical Evaluative Sciences) with support from its funders and partners: Canada’s Strategy for Patient-Oriented Research (SPOR), the Ontario SPOR Support Unit, and the Canadian Institutes of Health Research (CIHR) and the Government of Ontario. The opinions, results, and conclusions reported are those of the authors. No endorsement by ICES or any of its funders or partners is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the author, and not necessarily those of CIHI. The authors thank ICES for providing the data required for the study and the staff of TRI-UHN for their support. The authors also thank CIHR for providing funding (Funding Reference Number: PJT-153129) for this study. We would like to acknowledge patient collaborator Michelle Bartlett for her contributions in interpreting the findings for this study.
Funding information
This study was funded by the Canadian Institutes of Health Research (CIHR) Project Grant (201610PJT-377880-PJT-ADHD-136768).
Compliance with ethical standards
This study was approved by the University Health Network Research Ethics Board.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abrahams N, Mathews S, Lombard C, Martin LJ, Jewkes R. Sexual homicides in South Africa: a national cross-sectional epidemiological study of adult women and children. PLoS One. 2017;12(10):e0186432. doi: 10.1371/journal.pone.0186432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acute Care. (n.d.). [Accessed July 2018]. https://www.cihi.ca/en/acute-care.
- Anscombe AM, Knight BH. Case report. Delayed death after pressure on the neck: possible causal mechanisms and implications for mode of death in manual strangulation discussed. Forensic Science International. 1996;78(3):193–197. doi: 10.1016/0379-0738(95)01886-7. [DOI] [PubMed] [Google Scholar]
- Archer J. Sex differences in aggression between heterosexual partners: a meta-analytic review. Psychological Bulletin. 2000;126(5):651–680. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- Austin PC, van Walraven C, Wodchis WP, Newman A, Anderson GM. Using the Johns Hopkins Aggregated Diagnosis Groups (ADGs) to predict mortality in a general adult population cohort in Ontario, Canada. Medical Care. 2011;49(10):932–939. doi: 10.1097/MLR.0b013e318215d5e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin, P. C., & van Walraven, C. (2011). The mortality risk score and the ADG score: two points-based scoring systems for the Johns Hopkins aggregated diagnosis groups to predict mortality in a general adult population cohort in Ontario, Canada. Medical Care, 49(10), 940–947. 10.1097/MLR.0b013e318229360e. [DOI] [PMC free article] [PubMed]
- Barrett BJ, St Pierre M. Variations in women's help seeking in response to intimate partner violence: findings from a Canadian population-based study. Violence Against Women. 2011;17(1):47–70. doi: 10.1177/1077801210394273. [DOI] [PubMed] [Google Scholar]
- Black, M. C., Basile, K. C., Breiding, M. J., Smith, S. G., Walters, M. L., Merrick, M. T., & Stevens, M. R. (2011). National intimate partner and sexual violence survey: 2010 summary report. Atlanta, GA. Centers for Disease Control and Prevention.
- Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization--national intimate partner and sexual violence survey, United States, 2011. MMWR Surveillance Summaries. 2014;63(8):1–18. [PMC free article] [PubMed] [Google Scholar]
- Brink O. When violence strikes the head, neck, and face. The Journal of Trauma. 2009;67(1):147–151. doi: 10.1097/TA.0b013e318182f77f. [DOI] [PubMed] [Google Scholar]
- Burczycka, M., & Conroy, S. (2018). Family violence in Canada: a statistical profile, 2016. Statistics Canada.
- Carmo R, Grams A, Magalhaes T. Men as victims of intimate partner violence. Journal of Forensic and Legal Medicine. 2011;18(8):355–359. doi: 10.1016/j.jflm.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Chan V, Zagorski B, Parsons D, Colantonio A. Older adults with acquired brain injury: a population based study. BMC Geriatrics. 2013;13:97. doi: 10.1186/1471-2318-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarot F, Vaz E, Papin F, Proust B. Fatal and non-fatal bilateral delayed carotid artery dissection after manual strangulation. Forensic Science International. 2005;149(2–3):143–150. doi: 10.1016/j.forsciint.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Clayton, H. B., Lowry, R., Ashley, C., Wolkin, A., & Grant, A. M. (2017). Health risk behaviors with synthetic cannabinoids versus marijuana. Pediatrics, 139(4). 10.1542/peds.2016-2675. [DOI] [PMC free article] [PubMed]
- Di Paolo M, Guidi B, Bruschini L, Vessio G, Domenici R, Ambrosino N. Unexpected delayed death after manual strangulation: need for careful examination in the emergency room. Monaldi Archives for Chest Disease. 2009;71(3):132–134. doi: 10.4081/monaldi.2009.359. [DOI] [PubMed] [Google Scholar]
- Dunn, R. J., & Smock, W. (2017). Strangulation injuries. [Internet] Treasure Island, FL: StatPearls Publishing. [PubMed]
- Egge MK, Berkowitz CD, Toms C, Sathyavagiswaran L. The choking game: a cause of unintentional strangulation. Pediatric Emergency Care. 2010;26(3):206–208. doi: 10.1097/PEC.0b013e3181d1e3e3. [DOI] [PubMed] [Google Scholar]
- Ernst AA, Nick TG, Weiss SJ, Houry D, Mills T. Domestic violence in an inner-city ED. Annals of Emergency Medicine. 1997;30(2):190–197. doi: 10.1016/s0196-0644(97)70141-0. [DOI] [PubMed] [Google Scholar]
- Faugno D, Waszak D, Strack GB, Brooks MA, Gwinn CG. Strangulation forensic examination: best practice for health care providers. Advanced Emergency Nursing Journal. 2013;35(4):314–327. doi: 10.1097/TME.0b013e3182aa05d3. [DOI] [PubMed] [Google Scholar]
- Funk, M., & Schuppel, J. (2003). Strangulation injuries. WMJ, 102(3), 41–45. [PubMed]
- Glass N, Laughon K, Campbell J, Block CR, Hanson G, Sharps PW, Taliaferro E. Non-fatal strangulation is an important risk factor for homicide of women. The Journal of Emergency Medicine. 2008;35(3):329–335. doi: 10.1016/j.jemermed.2007.02.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin Y, Haag HL, Trott CT. Screening for history of traumatic brain injury among women exposed to intimate partner violence. PM & R : The Journal of Injury, Function, and Rehabilitation. 2016;8(11):1104–1110. doi: 10.1016/j.pmrj.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Haag, H. L., Jones, D., Joseph, T., & Colantonio, A. (2019). Battered and Brain Injured: Traumatic Brain Injury Among Women Survivors of Intimate Partner Violence-A Scoping Review. Trauma Violence Abuse, 1524838019850623. 10.1177/1524838019850623 [DOI] [PMC free article] [PubMed]
- Health Analyst’s Toolkit. Toronto: Ontario Ministry of Health and Long-Term Care 2012.
- Hines DA, Brown J, Dunning E. Characteristics of callers to the domestic abuse helpline for men. Journal of Family Violence. 2007;22(2):63. doi: 10.1007/s10896-006-9052-0. [DOI] [Google Scholar]
- Hlavaty L, Sung L. Strangulation and its role in multiple causes of death. The American Journal of Forensic Medicine and Pathology. 2017;38(4):283–288. doi: 10.1097/paf.0000000000000341. [DOI] [PubMed] [Google Scholar]
- Jacob, B., Stock, D., Chan, V., Colantonio, A., & Cullen, N. (2019). Predictors of in-hospital mortality following hypoxic-ischemic brain injury: a population-based study. Brain Inj, 1-9. doi:10.1080/02699052.2019.1683897. [DOI] [PubMed]
- The Johns Hopkins Adjusted Clinical Groups Technical Reference Guide, version 10. Baltimore, MD: Johns Hopkins University. (2009).
- Joshi M, Thomas KA, Sorenson SB. “I Didn’t Know I Could Turn Colors”: Health problems and health care experiences of women strangled by an intimate partner. Social Work in Health Care. 2012;51(9):798–814. doi: 10.1080/00981389.2012.692352. [DOI] [PubMed] [Google Scholar]
- Le Blanc-Louvry I, Papin F, Vaz E, Proust B. Cervical arterial injury after strangulation--different types of arterial lesions. Journal of Forensic Sciences. 2013;58(6):1640–1643. doi: 10.1111/1556-4029.12197. [DOI] [PubMed] [Google Scholar]
- Logan, J. E., Haileyesus, T., Ertl, A., Rostad, W. L., & Herbst, J. H. (2019). Nonfatal assaults and homicides among adults aged ≥60 years - United States, 2002-2016. MMWR. Morbidity and Mortality Weekly Report, 68(13), 297–302. 10.15585/mmwr.mm6813a1. [DOI] [PMC free article] [PubMed]
- Maine Commission on Domestic and Sexual Abuse. Report from the Task Group on Strangulation. (2012). Report to the Joint Standing Committee on Criminal Justice and Public Safety. Retrieved from http://www.mecasa.org/wp-content/uploads/2016/04/strangulation-commission-report-2012.pdf
- McClane GE, Strack GB, Hawley D. A review of 300 attempted strangulation cases part II: clinical evaluation of the surviving victim. The Journal of Emergency Medicine. 2001;21(3):311–315. doi: 10.1016/s0736-4679(01)00400-0. [DOI] [PubMed] [Google Scholar]
- Messing JT, Patch M, Wilson JS, Kelen GD, Campbell J. Differentiating among attempted, completed, and multiple nonfatal strangulation in women experiencing intimate partner violence. Womens Health Issues. 2018;28(1):104–111. doi: 10.1016/j.whi.2017.10.002. [DOI] [PubMed] [Google Scholar]
- Mills LD, Mills TJ, Taliaferro E, Zimbler A, Smith D. The prevalence of female-to-male intimate partner violence in an urban emergency department. The Journal of Emergency Medicine. 2003;25(2):215–218. doi: 10.1016/S0736-4679(03)00178-1. [DOI] [PubMed] [Google Scholar]
- National Ambulatory Care Reporting System (NACRS). (n.d.). [Accessed July 2018]. https://www.popdata.bc.ca/data/health/nacrs.
- Panyayong B, Tantirangsee N, Bogoian RRD, Thai National Mental Health Survey, T Psychiatric disorders associated with intimate partner violence and sexual violence in Thai women: a result from the Thai National Mental Health Survey. General Psychiatry. 2018;31(2):e000008. doi: 10.1136/gpsych-2018-000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patch M, Anderson JC, Campbell JC. Injuries of women surviving intimate partner strangulation and subsequent emergency health care seeking: an integrative evidence review. Journal of Emergency Nursing. 2018;44(4):384–393. doi: 10.1016/j.jen.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter, C. (2016). It’s time to consider a stronger strangulation law. https://www.thespec.com/news-story/6324747-it-s-time-to-consider-a-stronger-strangulation-law-porter/.
- Re L, Birkhoff JM, Sozzi M, Andrello L, Osculati AM. The choking game: a deadly game. Analysis of two cases of “self-strangulation” in young boys and review of the literature. Journal of Forensic and Legal Medicine. 2015;30:29–33. doi: 10.1016/j.jflm.2014.12.008. [DOI] [PubMed] [Google Scholar]
- Sasso R, Bachir R, El Sayed M. Suffocation injuries in the United States: patient characteristics and factors associated with mortality. The Western Journal of Emergency Medicine. 2018;19(4):707–714. doi: 10.5811/westjem.2018.4.37198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Homish GG, Leonard KE, Cornelius JR. Intimate partner violence and specific substance use disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychology of Addictive Behaviors. 2012;26(2):236–245. doi: 10.1037/a0024855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorenson SB, Joshi M, Sivitz E. A systematic review of the epidemiology of nonfatal strangulation, a human rights and health concern. American Journal of Public Health. 2014;104(11):e54–e61. doi: 10.2105/AJPH.2014.302191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada Census Profile, 2016 Census.
- Strack GB, Gwinn C. On the edge of homicide: strangulation as a prelude. Criminal Justice. 2011;26(3):32–36. [Google Scholar]
- Strack GB, McClane GE, Hawley D. A review of 300 attempted strangulation cases. Part I: criminal legal issues. The Journal of Emergency Medicine. 2001;21(3):303–309. doi: 10.1016/s0736-4679(01)00399-7. [DOI] [PubMed] [Google Scholar]
- Turkel A. “And Then He Choked Me”: understanding and investigating strangulation. American Prosecutors Research Institute. 2007;20(8):1–2. [Google Scholar]
- Valera EM. Increasing our understanding of an overlooked public health epidemic: traumatic brain injuries in women subjected to intimate partner violence. Journal of Women's Health (Larchmt) 2018;27(6):735–736. doi: 10.1089/jwh.2017.6838. [DOI] [PubMed] [Google Scholar]
- Wahlen BM, Thierbach AR. Near-hanging. European Journal of Emergency Medicine. 2002;9(4):348–350. doi: 10.1097/01.mej.0000043845.56375.12. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ. Sex differences in the perpetrator-victim relationship among emergency department patients presenting with nonfatal firearm-related injuries. Annals of Emergency Medicine. 2003;42(3):405–412. doi: 10.1067/mem.2003.324. [DOI] [PubMed] [Google Scholar]
- Wilbur L, Higley M, Hatfield J, Surprenant Z, Taliaferro E, Smith DJ, Jr, Paolo A. Survey results of women who have been strangled while in an abusive relationship. The Journal of Emergency Medicine. 2001;21(3):297–302. doi: 10.1016/S0736-4679(01)00398-5. [DOI] [PubMed] [Google Scholar]
- Wu V, Hall SF. Rates and causes of 30-day readmission and emergency room utilization following head and neck surgery. Journal of Otolaryngology - Head & Neck Surgery. 2018;47(1):36. doi: 10.1186/s40463-018-0283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaheer, J., Jacob, B., de Oliveira, C., Rudoler, D., Juda, A., & Kurdyak, P. (2018). Service utilization and suicide among people with schizophrenia spectrum disorders. Schizophrenia Research. 10.1016/j.schres.2018.06.025. [DOI] [PubMed]
- Zilkens RR, Phillips MA, Kelly MC, Mukhtar SA, Semmens JB, Smith DA. Non-fatal strangulation in sexual assault: a study of clinical and assault characteristics highlighting the role of intimate partner violence. Journal of Forensic and Legal Medicine. 2016;43:1–7. doi: 10.1016/j.jflm.2016.06.005. [DOI] [PubMed] [Google Scholar]