Hypernatremia due to salt poisoning is clinically rare and standard care procedures have not been established. We report a case of salt poisoning due to massive intake of seasoning soy sauce. Aggressive rapid correction of serum sodium concentration should only be considered in acute phases of hypernatremia within 2–3 h of salt ingestion, before the brain cells adapt to high osmolarity.
![]()
Keywords: Brain CT, hypernatremia, salt poisoning, sodium chloride, sodium correction
Abstract
Background
Hypernatremia due to salt poisoning is clinically rare and standard care procedures have not been established. We report a case of salt poisoning due to massive intake of seasoning soy sauce.
Case Presentation
A 40‐year‐old woman presented to the emergency department with seizures and remarkable hypernatremia with a serum sodium concentration of 183 mEq/L. The initial brain computed tomography scan showed brain shrinkage, which could occur during the acute phase of hypernatremia. We reduced her serum sodium level rapidly, rather than at the recommended slow rate. On day 3, the patient’s brain computed tomography scan showed widespread low‐density areas and edema. The patient died 8 days after admission.
Conclusion
After reviewing instances of resuscitation following salt intoxication, aggressive rapid correction of serum sodium concentration should only be considered in acute phases of hypernatremia within a few hours from ingestion, and 2–3 h could be one of the criteria.
BACKGROUND
Although hypernatremia usually results from hypovolemia, underlying diseases, and iatrogenic results, previous studies have also reported several cases of salt poisoning. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 Nevertheless, standard care procedures for salt poisoning have not yet been established due to a limited number of such cases. Aggressive therapy has been attempted in several cases in order to prevent mortality; however, more studies on salt poisoning are necessary. To fill gaps in knowledge and further elucidate treatment options for salt poisoning, we report a case of fatal acute hypernatremia due to massive ingestion of seasoning soy sauce.
CASE REPORT
A 40‐year‐old woman, previously diagnosed with schizophrenia, presented to our emergency department (ED) with convulsions. Four hours prior to presenting to the ED, she was found with clouding of consciousness. She began convulsing 1.5 h prior to presenting to the ED; the last time she was noted to be in good health was a few hours before her first episode of convulsions. After presenting to the ED, the patient’s tonic‐clonic convulsions continued. Respiratory support with a bag valve mask was necessary as primary treatment. Tachycardia exceeding 170 b.p.m. was confirmed, while the patient’s pulse was fully palpable. Her body temperature exceeded 40.5°C and her consciousness level was evaluated as comatose per the Glasgow Coma Scale, with E1V1M4. Convulsions were stopped with midazolam; however, the patient remained unconscious and was immediately intubated at the ED.
Laboratory findings revealed remarkable hypernatremia with a serum sodium concentration of 183 mEq/L and serum osmolality of 363 mOsm. We did not find another cause for the patient’s convulsions and unconsciousness. The patient’s family mentioned that she might have ingested 500 mL of triple strength Japanese seasoning soy sauce containing 2,393 mEq/L NaCl.
In the first hour, 1,600 mL Ringer’s lactate solution was given to control the serum sodium level; the patient’s serum sodium concentration decreased to 174 mEq/L. In the next 4 h, we administered 600–800 mL/h of 5% dextrose to correct the serum sodium level more rapidly without additional NaCl. Five hours after admission, the patient’s serum sodium concentration decreased to 167 mEq/L. We then adjusted the rate of sodium correction to 0.5–1 mEq/L/h following previously established recommendations. 10
On admission, the initial brain computed tomography (CT) showed brain shrinkage; the following brain CT, which was carried out on the third day, showed diffuse cerebral edema with widespread low‐density areas (Fig. 1). On the fourth day, the patient’s electroencephalogram was flat and brainstem reflexes had disappeared; thus, we diagnosed brain death. On the eighth day, the patient died due to dysfunction of the entire brain.
Fig. 1.
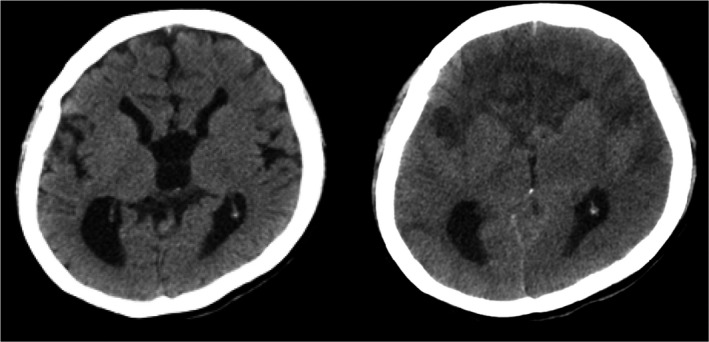
Brain computed tomography in a 40‐year‐old woman on day 1 and day 3 of hypernatremia. Left panel: day 1, brain shrinkage is clearly visible. Right panel: day 3, brain edema and low‐density areas in the frontal lesion have appeared.
DISCUSSION
The lethal dose of salt has been estimated to be <25 g, with serum sodium levels between 175 and 225 mEq/L. 1 , 11 Due to the high risk of osmotic demyelination syndrome, recommendations have been made for the rate at which serum sodium concentration should be corrected. The recommendations from one study stated that serum sodium levels should be reduced by 1.0 mEq/L/h in patients who develop hypernatremia over a period of hours, whereas in the case of patients with hypernatremia that developed over a longer period, the maximum recommended rate for reducing the serum sodium concentration should be 0.5 mEq/L/h. 10 Nine patients are reported to have survived salt intoxication, of which four were treated with the second (slow rate) recommendation (Table 1). Aggressive therapies are needed to succeed where the serum sodium concentrations were corrected rapidly in the early phase of hypernatremia. 3 , 5 In one report, serum sodium concentration was reduced from 196 mEq/L by rapidly infusing 5% dextrose in water over a period of 30 min. 3 In another report, the serum sodium concentration was reduced by 30 mEq/L within 2 h using hemodialysis. 5 In both reports, the patients presented to the ED in the early phase of hypernatremia. The results from these studies indicated that a rapid reduction in the serum sodium concentration could be effective for some patients; nonetheless, the indication is unclear.
Table 1.
Cases that recovered from salt poisoning
| Age (years) | Sex | NaCl ingestion (g) | Peak serum Na+ concentration (mEq/L) | Correction rate | Duration prior to ED arrival from digestion (h) | Reference no. |
|---|---|---|---|---|---|---|
| 39 | F | 60 | 176 | Slow | 0.3 | 7 |
| 20 | F | 150 | 174 | Slow | 3 | 2 |
| 73 | M | Unknown | 188 | Slow | 12 | 4 |
| 85 | F | 60–70 | 193 | Slow | Unknown | 6 |
| 55 | F | 104 † | 161 | Unknown | 0 | 8 |
| 32 | Unknown | 121 † | 150 | Unknown | 0 | 8 |
| 19 | M | 173 | 196 | 37 mEq/0.5 h | 2 | 3 |
| 65 | F | 207 | 176 | 30 mEq/2 h with hemodialysis | 3 | 5 |
| 54 | F | Unknown | 185 | 3 mEq/h | 21 | 9 |
| 40 | F | 70 | 183 | 16 mEq/5 h | >4 | Our case (dead) |
A total of nine cases of hypernatremia resulting from massive salt ingestion have been reported: four of them were treated using a slow sodium reduction rate, and two of them were treated with more aggressive therapy using a more rapid sodium correction rate. The duration of hypernatremia in the latter two cases was short prior to their arrival in the emergency department (ED).
F, female; M, male.
Vomited just after ingestion.
When hypernatremia occurs, the brain cells lose intracellular fluid within 15–30 min, and electrolytes enter the brain cells within a few hours to rapidly adapt to hypertonic stress. The brain volume normalizes within several days by a slow adaptation process in which organic osmolytes accumulate in the cells (Fig. 2). 10 , 12 After initiation of the slow adaptation process, there is risk for cerebral edema to occur due to rapid changes in the brain, as organic osmolytes are not absorbed quickly enough by the brain cells. Thus, a slow reduction in sodium levels is recommended for late‐phase hypernatremia. Using this theory, the aggressive therapy should be considered if the patients’ brain cells have not yet started adapting by taking up organic osmolytes.
Fig. 2.
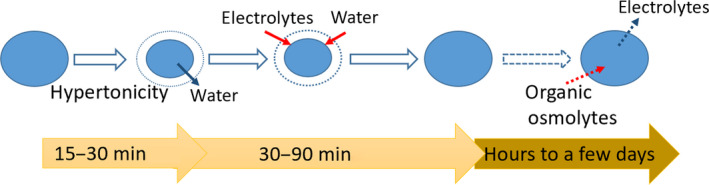
Adaptation of brain cells to hypernatremia. In high osmotic pressure, brain cells lose intracellular fluid and shrink in size during the first 15–30 min. To recover in size, cells take up extracellular electrolytes and water within 30–90 min and completely replace their electrolytes with organic osmolytes in a matter of a few hours to days. As organic osmolytes cannot move in and out of cells rapidly, adaptation to the osmotic change in the extracellular fluid is slower. Hence, rapid correction of hypernatremia puts the patient at risk for brain edema (revised from Strange, 1992 12 ).
In our case, although 6–10 h had already passed from the ingestion of soy sauce, the initial brain CT showed brain shrinkage. Hence, it seemed that the patient was still in the early process of adaptation to hypertonic stress. Consequently, we reduced her serum sodium level more rapidly than recommended, which had an unfavorable result.
Several reports describe cases with acute hypernatremia who had a favorable outcome following treatment with the slow sodium correction rate. 2 , 4 , 6 , 7 In light of these findings, aggressive therapy should not be considered for all cases presenting with salt intoxication. In those cases where organic osmolytes have already started accumulating in the brain cells to adapt to hypertonic stress, a more cautious procedure should be selected to correct hypernatremia, that is, using the slow rate sodium correction method. Although it is difficult to estimate the peak time of sodium concentration after salt ingestion, aggressive therapy should only be considered within a few hours from salt ingestion, and 2–3 h could be one of the criteria, as was the case for the limited number of patients with reported salt poisonings.
CONCLUSION
We witnessed a case of lethal hypernatremia as a result of massive ingestion of seasoning soy sauce, even after we used aggressive rapid correction of serum sodium concentration. The limitation of this discussion is that the number of cases of salt intoxication is too small to estimate the best management of acute and late‐phase reactions. Nevertheless, with limited experience, we conclude that such aggressive therapy should only be considered in a few hours from ingestion, and 2–3 h could be one of the criteria.
DISCLOSURE
Approval of the research protocol: N/A.
Informed consent: Informed consent was obtained from the patient’s family.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Conflict of interest: None.
ACKNOWLEDGEMENTS
We would like to thank Editage for language editing.
Funding information
No Funding information provided.
References
- 1. Campbell NRC, Train EJ. A systematic review of fatalities related to acute ingestion of salt. A need for warning labels? Nutrients 2017; 9: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ju HJ, Bae HJ, Choi DE, Na KR, Lee KW, Shin YT. Severe hypernatremia by excessive bamboo salt ingestion in healthy young woman. Electrolyte Blood Press 2013; 11: 53–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carlberg DJ, Borek HA, Syverud SA, Holstege CP. Survival of acute hypernatremia due to massive soy sauce ingestion. J. Emerg. Med. 2013; 45: 228–31. [DOI] [PubMed] [Google Scholar]
- 4. Machino T, Yoshizawa T. Brain shrinkage due to acute hypernatremia. Neurology 2006; 67: 880. [DOI] [PubMed] [Google Scholar]
- 5. Sakai Y, Kato M, Okada T et al Treatment of salt poisoning due to soy sauce ingestion with hemodialysis. Chudoku Kenkyu 2004; 17: 61–3. [PubMed] [Google Scholar]
- 6. Addleman M, Pollard A, Grossman RF. Survival after severe hypernatremia due to salt ingestion by an adult. Am. J. Med. 1985; 78: 176–8. [DOI] [PubMed] [Google Scholar]
- 7. Matsushima S, Okada Y, Tosa R. A case of salt intoxication treated with lactated Ringer injection. Chudoku Kenkyu 1994; 7: 55–8. [Google Scholar]
- 8. Uwadaira C, Endo K, Endo T et al Two cases of salt poisoning with suicidal attempt due to say sauce ingestion. Jpn. J. Psychiatr. Treat. 1994; 9: 1395–400. [Google Scholar]
- 9. Mcgouran RCM. Case of salt overdosage. Br. Med. J. 1975; 4: 386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Adrogué HJ, Madias NE. Hypernatremia. N. Engl. J. Med. 2000; 342: 1493–9. [DOI] [PubMed] [Google Scholar]
- 11. Moder KG, Hurley DL. Fatal hypernatremia from exogenous salt intake: report of a case and review of the literature. Mayo Clin. Proc. 1990; 65: 1587–94. [DOI] [PubMed] [Google Scholar]
- 12. Strange K. Regulation of solute and water balance and cell volume in the central nervous system. J. Am. Soc. Nephrol. 1992; 3: 12–27. [DOI] [PubMed] [Google Scholar]


