Abstract
Background
A novel coronavirus (SARS-CoV2) outbreak in more than 200 countries recently caused viral pneumonia that was extremely infectious and pathogenic. The Chinese government proposes that both Traditional Chinese medicine (TCM) and Western medicine can be used in combination to treat pneumonia caused by SARS-CoV2, and TCM effectively provides continuous prevention and treatment.
Methods
The present review analyzes and summarizes the prevention and treatment of the novel coronavirus disease (COVID-19) with TCM. A classified analysis of the efficacy and advantages of TCM for the prevention and treatment of COVID-19 was performed, and the mechanisms of TCM in treating COVID-19 are summarized.
Results
TCM is effective in preventing COVID-19, and medical staff can prevent an iatrogenic infection by taking a decoction made based on the principles of TCM. As of March 13, 2020, new cases of COVID-19 in China have decreased in number to single digits. TCM's curative effect was outstanding, with a national participation rate of over 90%. More than 70,000 people were cured of COVID-19 and discharged from the hospital. Only approximately 10,000 patients are currently being treated, and the total treatment time is approximately 2 months.
Conclusions
TCM is currently the best choice for the treatment and prevention of COVID-19, and it is expected that it will be promoted by countries around the world.
Keywords: Novel coronavirus pneumonia, Progress, COVID-19, Traditional Chinese Medicine
Introduction
Infectious diseases are the demons with which human beings have been fighting since the beginning of human history. Several epidemics have occurred in the history of China. But, fortunately, no large numbers of casualties have occurred, due to the prevalence of Traditional Chinese Medicine (TCM). During the epidemic period of severe acute respiratory syndrome (SARS), TCM played a vital role in fighting the epidemic (Luo et al., 2019), and the Chinese medical community accumulated valuable TCM experience (Li et al., 2020; Liu and Wang, 2004). What is the essence of infectious diseases? Is it possible to cure the disease as long as the virus is eliminated? TCM believes that the essence of infectious diseases is not viruses, but “grumpiness.” “Grumpiness” is a kind of evil that appears at the same time as abnormal weather. “Grumpiness” has the characteristics of strong pathogenicity, strong infectivity, entry route to human body through the mouth and nose, and specific lesion location. The current research data show that the novel coronavirus disease (COVID-19), which was prevalent in Wuhan in December 2019 (Cui et al., 2019; Li et al., 2020b; Zhu et al., 2020), has the characteristics of an epidemic due to its infectiousness, which is in line with the category of “plague” in febrile disease. SARS-CoV2 can be understood as the “outcry” in Wen Xie, which is of great significance for screening susceptible people.
A current meta-analysis also showed that the main clinical symptoms of COVID-19 patients are fever (88.5%), cough (68.6%), myalgia or fatigue (35.8%), expectoration (28.2%), and dyspnea (21.9%). The minor symptoms include headache or dizziness (12.1%), diarrhea (4.8%), and nausea and vomiting (3.9%) (Li et al., 2020a). The data showed that although patients with COVID-19 had fever (mainly in the early stage of disease), the fever was not high and had the characteristic of “heat not rising.” In addition, patients have symptoms such as fatigue, tiredness, diarrhea, and thickly coated tongue (Tian et al., 2020), which are consistent with the characteristics of heavy turbidity, stickiness, and depression in TCM. According to TCM, “wet poison” is caused by the combination of evil inside and outside. Thus, people who are cold or wet are very susceptible to the virus. In addition, sex workers may be heavily affected.
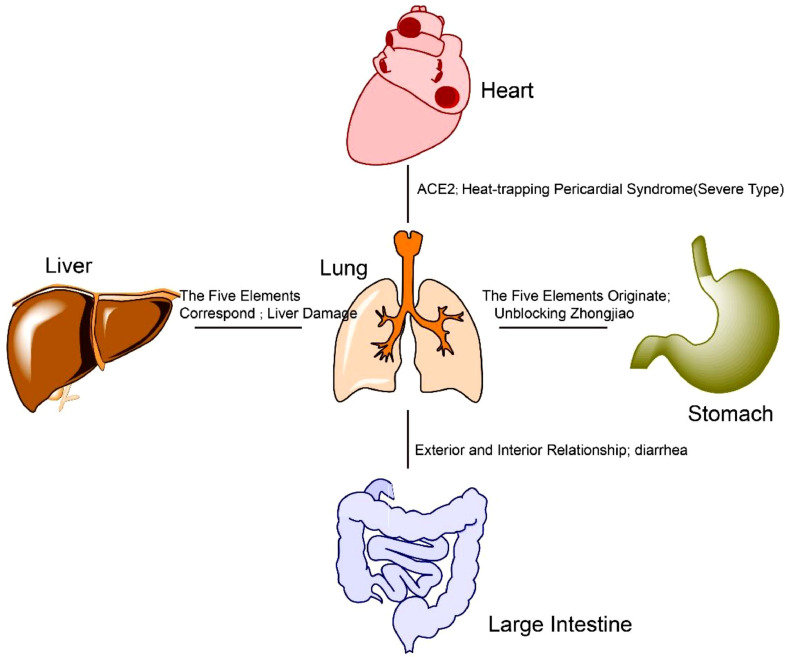
The spread of infectious disease among health care workers during an epidemic is another consequence of its widespread distribution. What has become absolutely clear is that the use of isolation clothing, masks, and eye masks is an effective method to prevent the spread. However, this method puts stress on the supply of materials for this equipment. If there is widespread need, and the protective articles are not replaced in a timely way, infection of medical staff may occur. However, none of the medical staff was infected in the TCM hospitals or when using TCM methods (Xian et al., 2020). The medical staff consumed a Ganjiang Gancao decoction or other preventive prescriptions to prevent the infectious disease. This gratifying result was confirmed in the prevention and treatment of SARS in 2003 (Luo et al., 2020). Youke Wu, a famous Chinese medicine practitioner in the Qing Dynasty of China, systematically furthered the understanding and treatment of infectious diseases and completed the first monograph on infectious diseases of TCM, entitled “Plague Theory”. In view of the law of transmission of infectious diseases, it is believed that the progress of the disease in the human body can be divided into four steps: defense, qi, nutrient, and blood. These steps can be used to summarize the superficial and deep levels of pathological changes and the severity of these changes. Wei Fen syndrome belongs to the category of exogenous exterior syndrome, which is the initial stage of pathological changes caused by exogenous heat evil invading the human body. Qi Fen syndrome refers to the stage of abnormal qi movement in human viscera or tissues without blood circulation. In Wei Fen and Qi Fen, the disease location is mainly in the lung, stomach, intestine, and gallbladder, and most of these diseases are functional disorders of the human body. Ying Fen syndrome refers to the stage of pathogenic heat in Ying Fen caused by the invasion of pathogenic heat. The stage of main pathological change is burning Ying Yin, which is the third stage of pathological change caused by the invasion of pathogenic factors. Blood Fen syndrome refers to the development of pathogenic heat to blood Fen, resulting in hyperactivity of blood heat. Blood consumption is a stage of major pathological change and the fourth stage in the course of disease. The main pathological change in this stage is organ parenchyma damage. This four-step TCM method of defense, qi, nutrient, and blood explains why no case progressed from mild to severe in the treatment of COVID-19 by TCM (Fig. 1 ).
Fig. 1.
Connections between lung and others organs with TCM theory.
The present review summarizes the advantages of TCM in the prevention and treatment of COVID-19 and answers the following scientific questions: (1) How can we understand the origin of unprecedented new infectious diseases? (2) Why is the TCM so effective for preventing the spread of highly infectious viruses? (3) Which methods of TCM have achieved good results in the treatment of COVID-19? (4) What are the scientific nature and molecular mechanism of TCM in the treatment of COVID-19? (5) For the patients cured by TCM, will they recover Yang, have sequelae, or need to continue taking medicine after recovery?
TCM knowledge of COVID-19
Understanding how COVID-19 is a plague
Infectious diseases are often associated with viruses, such as in the cases of Severe Acute Respiratory Syndrome (SARS) in 2003, Middle East respiratory syndrome (MERS) in 2012, and COVID-19 in 2019. The pathogens associated with these diseases are all coronaviruses. But, TCM does not consider viruses to be the main cause of infectious diseases. As long as the disease is cured, the virus will die out naturally. Further, a negative virus test does not indicate recovery. COVID-19 belongs to the category of ‘epidemic’ disease in TCM (Wang et al., 2020). Plagues have their own properties, and a plague corresponds to a nature (Yang et al., 2020).
COVID-19 was categorized as a cold and dampness epidemic (Sun et al., 2020), and the pathogenic factors are found in the body's mucous membranes (Han et al., 2020). Dampness should be paid more attention to in this epidemic (Li et al., 2020; Zheng et al., 2020). The complexity of COVID-19 lies in the fact that damp evil is dominant and dryness evil is contained (Fan et al., 2020).
In addition, some patients have been infected with the disease without obvious symptoms, which makes the prevention and control of the epidemic more difficult. TCM also has a treatment plan for patients who have been infected with the disease without symptoms (Liu et al., 2020).
Focus on organs other than lungs
Treating patients as an organic whole is the prerequisite for TCM to treat all diseases. COVID-19 is primarily located in the lungs, but there are exterior and interior relationships between the lungs and the large intestine (Xia and Huang, 2020).
The connection between the spleen, stomach, and lungs is extremely strong and should be attended to during treatment (Ding et al., 2020; Wen and Zhang, 2020). More importantly, TCM also attaches great importance to liver damage caused by COVID-19 (Chai et al., 2020; Liu, 2003). During the SARS epidemic, it was recognized that the receptor angiotensin converting enzyme II (ACE2) was activated during the viral infection and subsequently caused a dysfunction in blood clotting. This finding suggested that we should also pay attention to the relationship between the heart and the lungs (Xian et al., 2020).
TCM treatment strategy for COVID-19
TCM divides the disease into four stages according to the law of disease transmission: early stage, advanced stage, critical stage, and recovery stage (Table 1 ). In the early stage, the common syndromes of COVID-19 were the syndrome of dampness repressing the defensive qi of the lungs or of wind heat attacking the lungs. The primary treatment is dredging the exterior and penetrating the pathogen, ventilating the lung qi for lowering adverse qi, and treatment against the cold in the Taiyang meridian (Wang et al., 2020; Xiao et al., 2020). In the advanced stage, the common syndromes were the syndrome of dampness blocking the lungs and stomach or pathogenic heat accumulating in the lungs. The main treatment is increasing clear qi and lowering adverse qi (Shao et al., 2020; Xue et al., 2020). Then, in the critical stage, the common syndromes were the syndrome of epidemic virus closing the lungs, or internal block and outward desertion. The treatment should allow the Yang to recover and open the orifices to induce resuscitation (Bai et al., 2020; Ma et al., 2020; Xiao et al., 2020). Finally, the common syndromes in the recovery stage were the syndromes of qi deficiency of the lungs and spleen. Attention should be paid to qi and yin in the later period (Xie et al., 2020). In addition, in the treatment of plague, both evil and positive are emphasized by TCM (Shao et al., 2020).
Table 1.
Stage differentiation, treatment method and basic formula of COVID-19 in TCM.
| Stages | TCM Syndrome Differentiation | Treatment Method | Decoction/Chinese Patent Medicines | |
|---|---|---|---|---|
| prevention stage | — | aromatic to avoid filth | Decoction (Shishen Tang, et al); Chinese patent Medicines (Jingfang Baidu San,, et al) | Ni et al., 2020 |
| observation stage | suspected patients and medical observation persons (close contacts) | jie-biao with pungent heat herbs | Chinese patent Medicines (Huoxiang Zhengqi capsule, Yupingfeng San, Lianhua Qingwen capsule, et al) | Jin et al., 2020; Feng et al., 2020 |
| initial stage | cold-damp depression lung | aromatic to resolve dampness, promoting lung and dissipating and expelling evil | Decoction (Maxing Shigan Tang, Maxing Yigan Tang, Shengjiang San, Dayuan Yin, et al) | Yu et al., 2020 |
| middle stage | epidemic toxin closed lung | clearing heat, purging the lungs, detoxifying and smoothing Fu organs | Decoction (Maxing Shigan Tang, Xuanbai Chengqi Tang, Shengjiang San, Dayuan Yin, et al) | Pang et al., 2020 |
| severe stage | inner blocking causing collapse | resuscitation with aromatics, detoxification and eliminating pathogenic factors | Chinese patent Medicines (Angong Niuhuang Wan, Suhexiang Wan and Zixue Dan, et al) | Xu et al., 2020 |
| critical stage | internal block and outward desertion | opening the orifices, returning to yang for emergency treatment | Decoction (Shenfu Tang, Sini Tang); Chinese patent Medicines (Angong Niuhuang Wan, Suhexiang Wan and Zixue Dan, et al) | Sun et al., 2020 |
| recovery stage | qi-deficiency of lung and spleen | nourishing qi and yin | Decoction (Maiwei Buzhong Yiqi Tang, et al) | Zhang et al., 2020; Gu et al., 2019; Zhang et al., 2020 |
TCM prevention of COVID-19
Prediction based on five movements and six qi
Based on the theory of “five movements and six qi,” the science of disaster prediction in ancient China can be used to predict the effect of natural climate change on human organ function based on the combination of the five movements of the sky and the six qi of the earth. Further, based on the theory of “3-year epidemic formation,” it is proposed that if the migration and operation of the climate is abnormal, an epidemic will occur in approximately 3 years (Liu et al., 2013). The Spring Festival of 2020 was affected by excessive jinyun, the minister fire of shaoyin being the celestial manager and the influence of zhuqi and keqi, the lungs (the five element is gold) and liver (the five element is wood) are easily out of balance, and the functions of the spleen are gradually recovering (Li and Du, 2020; Yang and Yu, 2020). In other words, TCM can make relatively accurate predictions before the outbreak of the disease, allowing the hospitals to make emergency plans.
Prevention using TCM decoction
For people who are isolated at home in the community, a TCM decoction can be used for prevention. The composition of the prescription is mainly aromatic and is used to avoid filth and improve autoimmunity (Ali et al., 2013; Angenent et al., 1986; Hosain et al., 1969). COVID-19 prevention prescriptions based on the theory of “Natural Factor” were used to maintain vital qi (Li and Qiu, 2020). Modern pharmacological studies have shown that TCM ingredients are effective in clearing away heat and detoxifying, as well as in relieving surface dampness, thereby inhibiting the virus. As early as the 1970s, the study of TCM against the influenza virus has been undertaken in China. There are two ways that TCM acts as an antiviral. The first is by directly inhibiting the virus, primarily by heat clearing and detoxifying. Lonicera, Folium Isatidis, and Scutellaria are used for inhibition. The second is to indirectly play an antiviral role or inhibit the virus-mediated inflammatory response by regulating the immune function of the body. Astragalus, Salvia, Acanthopanax senticosus, and Gentiana are used as antivirals and induce interferon and immunoglobulin. TCM focuses on the overall regulation of the body. Thus, TCM can play a multi-target role in the regulation of the body's systems (Gao and Wang, 2018).
Prevention of disease with herbal incense
Sachets are made of aromatic herbs. For those who have not been infected with the virus but have been exposed, the most simple and effective method of TCM prevention is by the traditional aromatherapy method with herbs such as Atractylodes lanceolata, Phellodendron amurense, and Artemisia argyi, which have a significant preventive effect (Liang et al., 2003). In addition, the herbs can be made into a sachet to “avoid poisonous gas” (Zhang et al., 2020; Zhang et al., 2003), which is an important principle in TCM (Liu, 2003).
Prevention of infection among medical staff
Insufficient protection increases the risk of COVID-19 in frontline medical staff (Fu et al., 2020). Moreover, once masks, goggles, and protective clothing are contaminated, they cannot be used again.
In TCM hospitals, or hospitals based on TCM treatment methods, medical staff take one or two decoctions every day and burn Artemisia argyi or Atractylodes lanceolata in the hospital to cut off the transmission route.
As reported by CCTV4, 1250 medical staff in Tongxu County Hospital (Henan province) drank Chinese medicine decoctions and burned Artemisia argyi in the hospital corridor. With regard to masks, disposable masks were used for medical personnel, and N95 masks were not used (Hao et al., 2012). In Jingzhou (Hubei province), the worst-hit area of the epidemic, 580 medical staff came from Jingzhou TCM Hospital, and none of them were infected by the disease. In addition, the hospital produces 25,000 preventive Chinese patented medicines for distribution to other hospitals every day (Zhang et al., 2017). In Wuhan, where the epidemic was most severe, Jiangxia Fangcai Hospital also achieved zero infections among medical staff (Seah et al., 1973). Moreover, in Huanggang, Huangshi (Hubei province), and Guangzhou (Guangdong province), TCM methods were used to prevent the epidemic, and there was zero infection among the medical staff there as well. However, more than 3000 medical staff without TCM prevention were infected. Considering the similarity between the COVID-19 epidemic and the SARS epidemic in 2003, it is pertinent to compare the outcomes among medical personnel in China. Three studies were identified including one controlled study (Lau et al., 2005) and two single cohort studies (Luo et al., 2020) conducted during the SARS epidemic. Lau et al designed a controlled study to evaluate an herbal formula for prevention of SARS (no herbal intervention in the control group) and conducted it in Hong Kong, China. The sample size was 16,437 (1063 in the herbal group and 15,374 in the control group), and all participants were hospital care workers including doctors, nurses, and other staff. The results showed that none of the participants who took a modified formula of Yupingfeng Powder and Sangju Decoction contracted SARS, whereas 64 of 15,347 (0.4%) in the control group were infected with SARS (P=0.035). There were 19 cases (1.8%) of minor adverse effects after 14 days of taking the herbal medicine, including diarrhea, sore throat, dizziness, and nausea. Both single cohort studies were conducted in Beijing, China, with sample sizes of 3561 and 163, respectively. All participants were medical staff from two hospitals in which SARS patients were recruited and treated during the study period (Luo et al., 2020). One of the studies included only first-line medical staff treating SARS. The courses of taking the herbal formulae for prevention were 6 days and 12 to 25 days for the two cohort studies, respectively. The decoctions used in these studies were both a classic formula of Yupingfeng Powder and some heat-clearing and detoxifying herbs. The results of the two studies showed that none of the participants who took the preventive herbal medicine contracted SARS.
TCM treatment of COVID-19
TCM has achieved good results in the treatment of COVID-19. Thus far, no exacerbations and no cases of recovery yang have been reported. In terms of treatment methods, TCM decoction, acupuncture, and external treatments have been used, among others.
TCM decoction
A TCM study was performed to accurately identify patients infected with COVID-19 (Yu et al., 2020). In the Wanzhou District (Chongqing), 225 common and severe COVID-19 cases were analyzed. Based on TCM theory, the core pathogenesis of COVID-19 is dampness, heat, toxins, and deficiency, and the main treatment principle is strengthening the lungs to prevent dampness, clearing away heat and detoxification, supplementing qi, and nourishing Yin (Gong et al., 2020). Further, there were 209 cases of COVID-19 in Chongqing City with cough (70.81%) and fever (55.50%) as the common symptoms. The primary clinical TCM pathogens are heat obstructing lung syndrome (30.14%), dampness obstructing syndrome (16.27%), and cold dampness stagnating lung syndrome (11.96%) (Ran et al., 2020). In Hunan province, by the end of February 25, 2020, a total of 1016 patients were diagnosed, and 981 of these patients were treated with TCM as part of their treatment, accounting for 96.56%. Of these patients, 779 patients (95.76%) were discharged, and 233 patients were hospitalized. Among them, 233 patients were treated with TCM, accounting for 100% (Huang et al., 2020). Another study of 52 confirmed cases of COVID-19 used TCM intervention (Chen et al., 2020). Except for one death in the extreme stage, the rest of the cases improved or were discharged. Qingfei Paidu decoction was most commonly used in COVID-19 treatment. Ninety-eight cases of COVID-19 in Sichuan province treated using Qingfei Paidu decoction were analyzed. After 9 days of treatment with Qingfei Paidu decoction, the total effective rate was 92.09%, the recovery rate was 41.13%, and the significant efficacy rate was 26.92% (Wang et al., 2020). In another case, in which six patients were treated using Lung-toxin Dispelling Formula (1 version) in combination with Western medicine for 16 days, the polymerase chain reaction (PCR) tests came back negative, and the average hospitalization time was 20 days. All six patients were cured and discharged (Li et al., 2020). A case of COVID-19 in Changchun that was treated using integrated TCM and Western medicine for 7 days resulted in the patient's rent recovery and discharge (Zhao et al., 2020). As of February 17, there were 60,107 confirmed cases treated using TCM in China, accounting for 85.20% of all cases. Outside Hubei, 87% of patients who were cured using TCM and discharged participated in the treatment of cases. There may be a positive correlation between the cure rate of COVID-19 and the rate of TCM use, but there are other factors that affect the cure rate of COVID-19. The exact relationship between the two needs to be further verified by science (Wang et al., 2020). Ang et al. (2020) summarized and analyzed the herbal formulae provided by the guidelines for their pattern identifications (PIs) and compositions of herbs to treat patients with COVID-19. Of the 28 guidelines, there were 26 government-issued Chinese guidelines and 2 Korean guidelines. In the frequency analysis of herbs, Glycyrrhizae Radix et Rhizoma, Armeniacae Semen Amarum, Ephedrae Herba, and Gypsum Fibrosum were found to be the herbs with the highest frequency of use in the Chinese guidelines.
Acupuncture
As an important part of TCM, acupuncture and moxibustion therapy have made vital contributions in the history of anti-epidemic action in China. Modern clinical and experimental studies have shown that acupuncture and moxibustion therapy can regulate the human immune function, preventing inflammation and infection. In the current epidemic of COVID-19, acupuncture and moxibustion therapy were actively used for both prevention and treatment. According to Guidelines on Acupuncture and Moxibustion Intervention for COVID-19 (second edition) (Lin et al., 2020), acupuncture and moxibustion intervention was divided into three phases: medical observation phase (suspected cases), clinical treatment phase (confirmed cases), and convalescence phase. In the medical observation phase, the main points were Fengmen (BLl2), Feishu (BLl3), Pishu (BL20), Hegu (LI4), Quchi (LI11), Chize (LU5), Yuji (LU10), Qihai (CV6), Zusanli (ST36), and Sanyinjiao (SP6). The purpose was to stimulate the vital qi and the functions of the lungs and spleen, enhancing the viscera's defense. During the clinical treatment phase, the main points chosen were as follows: Hegu (LI4), Taichong (LR3), Tiantu (CV22), Chize (LU5), Kongzui (LU6), Zusanli (ST36), Sanyinjiao (SP6), Dazhu (BLll), Fengmen (BLl2), Feishu (BLl3), Xinshu (BLl5), Geshu (BL17), Zhongfu (LU1), Danzhong (CVl7), Qihai (CV6), Guanyuan (CV4), and Zhongwan (CVl2), in order to stimulate the vital qi of the lungs and spleen, protect the viscera, and dispel pathogens. In the convalescence phase, the main points were Neiguan (PC6), Zusanli (ST36), Zhongwan (CVl2), Tianshu (ST25), and Qihai (CV6). The aim in this phase is to remove residual virus, restore vitality, and repair the functions of the lungs and spleen. Scholars have provided other ideas for prevention and treatment of COVID-19. Lin Shiyu (Lin et al., 2020) selected Dazhui (DU14), Fengmen (BLl2), Shaoshang (LU11), Yuji (LU10), Lidui (ST45), and Neiting (ST44) can be used as part of a fire needle treatment plan to prevent COVID-19 and relieve patients’ symptoms. Liu Kaiping (Liu et al., 2020) suggested that moxibustion not only effectively prevents and treats COVID-19, but also improves the quality of life of patients. After the comparative induction and analysis of relevant references, Zhang et al. (2020) pointed out that moxibustion on Dazhui (DU14) and Quchi (LI11) could be selected for fever; moxibustion on Dazhui (DU14), Feishu (BL13), and Dingchuan (EX-B1) could be selected for cough; moxibustion on Zusanli (ST36), Guanyuan (CV4), and Qihai (CV6) could be used for fatigue; and moxibustion on Zhongwan (CV12), Zusanli (ST36), and Tianshu (ST25) could be used for upper digestive system discomfort. Besides, Yang et al. (2020) suggested that Ren and Du meridian moxibustion can play an important role in the prevention of new COVID-19 infectionsand in preventing recurrence after recovery.
Although there are only a few clinical reports about acupuncture and moxibustion treatment in COVID-19 patients, it is expected to be a safe and effective adjuvant therapy.
Treatment by Chinese patented medicine
Chinese patented medicine is widely used in all stages of COVID-19 because of its convenience and good taste. At present, the COVID-19 diagnosis and treatment plan (trial version 7) includes Chinese medicine. During the medical observation period, the clinical manifestation is fatigue. In case of gastrointestinal discomfort, Huoxiang Zhengqi (capsule, pill, water, or oral liquid) is recommended as the Chinese patented medicine with the most effectiveness. In cases of fatigue with fever, a combination of Jinhua Qinggan granules, Lianhua Qingwen capsules (granules), and Shufeng Jiedu capsules (granules) are recommended as the Chinese patented medicines with the most effectiveness. In the clinical treatment period, Qingfei Paidu decoction is used for the treatment of mild, regular, and severe patients. In addition, the corresponding prescriptions are recommended for different syndromes of mild, regular, severe, and critical patients; for severe and critical patients, Xiyanping injection, Xuebijing injection, Reduning injection, Tanreqing injection, and Xingnaojing injection are recommended (Chen et al., 2020). The possible mechanism of Huoxiang Zhengqi in the prevention and treatment of COVID-19 has been discussed. Huoxiang Zhengqi can increase the level of anti-inflammatory cytokine IL-10, regulate the inflammation-related NF-κB pathway, suppress excessive inflammatory response, and resist a variety of viruses. There is in vitro experimental evidence that Huoxiang Zhengqi has a significant inhibitory effect on COVID-19 pathogens (Wang et al., 2020; Huo et al., 2020). TCM injection is widely used in the treatment of COVID-19 (Wang, 2019). There are still some risks of the use of TCM injections. Attention should be paid to its safety, especially standardization, combination, adverse reactions, and use in special populations (Lin and Zhang, 2020; Xiang et al., 2020; Yang et al., 2020; Zhao et al., 2020).
Therapeutic pharmacology and mechanism
Classic pharmacology in animal experiments
Due to time limitations, there have been few animal experiments related to COVID-19. Compound Qinlan Oral Liquid has a certain pharmacological effect in the rat model when combining COVID-19 disease with epidemic toxin closed lung syndrome, through inhibiting virus replication, improving gastrointestinal function, improving immunity, and decreasing inflammatory factor expression. A therapeutic effect was found in Compound Qinlan Oral Liquid in treating a combination of COVID-19 pneumonia with pestilence attacking lung syndrome (Bao et al., 2020). Reyanning Mixture could treat COVID-19 in mice with epidemic toxin closed lung syndrome. It has significant effects such as improving the gastrointestinal function and enhancing the autoimmune function of mice, and decreasing the expression of inflammatory factors in vivo, which would offer reference for clinical research (Bao et al., 2020).
Network pharmacology
At the molecular level, TCM compounds play an all-round and integral role in regulating the body through multi-component and multi-target processes. The herb-target interaction network analysis helps to disclose the molecular mechanisms of TCM (Hopkins, 2008; Zhao et al., 2019).
The national Health Commission and the State Administration of traditional Chinese medicine jointly issued a notice recommending Qing Fei Pai Du Tang (QFPDT) to be used all over the country (Feng et al., 2019). Zhao et al. (2020) explored the mechanism of QFPDT in the treatment of COVID-19 with a network pharmacology analysis, by regulating a series of proteins co-expressed with ACE2 and a series of signaling pathways. QFPDT may act as an antiviral agent by targeting ribosomal proteins that are necessary for viral replication, thus inhibiting viral mRNA translation and inhibiting a group of proteins that interact with viral proteins. Xu et al. (2020) predicted that the first five active ingredients of QFPDT in the treatment of COVID-19 were quercetin, luteolin, kaempferol, naringin, and isorrine. QFPDT mainly regulates targets such as MAPK1, MAPK3, MAPK8, MAPK14, IL-6, RELA, and STA T1, and signaling pathways such as TNF and NF-κB to inhibit inflammatory response, regulate immune function, reduce lung injury, and protect nerve function, thus effectively treating COVID-19. Moreover, it was reported that the components with high oral availability of Qingfei oral solution had good molecular docking results with the targets of RdRp, 3Clpro, and PLpr, and could be used to treat viral pneumonia with fever and cough symptoms by regulating multiple signaling pathways (Yao et al., 2020).
Da-Yuan-Yin is the original prescription of QFPDT and provincial anti-COVID-19 prescriptions. Based on network pharmacology and the molecular docking method, Zong et al. (2020) pointed out that the active compounds in Da-Yuan-Yin may regulate multiple signaling pathways by binding ACE2 and acting on targets such as prostaglandin-endoperoxide synthase 2 (PTGS2), heat shock protein 90 alpha family class a member 1 (HSP90AA1), and estrogen receptor 1 (ESR1) to inhibit COVID-19. On the other hand, as a Chinese patented medicine based on Da-Yuan-Yin, Qingfei Dayuan Granules’ main active ingredients had good binding properties to the receptor according to the molecular docking results (Xiang et al., 2020). The series Chinese patented medicines of Huoxiang Zhengqi, including Huoxiang Zhengqi oral liquid, are recommended as preventive drugs for COVID-19 patients with gastrointestinal discomfort and fatigue during medical observation. Based on network pharmacology and the molecular docking method, Deng yanjun (Deng et al., 2020) suggested that the compounds in Huoxiang Zhengqi Oral Liquid can combine with ACE2 binding to PTGS2, heat shock protein 90 alpha family class b member 1 (HSP90AB1), calmodulin regulated spectrin associated protein family member 2 (CAMSAP2), and other targets to regulate multiple signaling pathways, thus exerting a preventive or therapeutic effect on COVID-19. In addition, based on the analysis of network pharmacology, huanglian jiedu soup (Wang et al., 2020), Qingwen Baidu Yin (Zhang et al., 2020), and Xue's Wuye Lugen Decoction Tea Drink (Xiang and Lü, 2020) may also have a therapeutic effect on COVID-19.
Discussion
The Chinese method is the only one that has been proven successful, said Bruce Elwald, senior adviser to the director general of the World Health Organization on February 24. At present, more than 200 countries in the world have experienced COVID-19 outbreaks. In the absence of specific drugs in the world (Cao et al., 2020), China's experience in the application of TCM can be used as a valuable reference. Another advantage of TCM to treat COVID-19 is that the rate of relapse of COVID-19 is lower than that when Western medicine is used. The total rate of relapse of COVID-19 is approximately 0.1% of 8000 cases (Liu et al., 2016). Many hospitals have had no relapse cases to date (Hu et al., 2015). Although pharmacological studies have demonstrated the underlying mechanisms, targets, and biological pathways to treat COVID-19, the only two targets are cathepsin L (CL)-like proteases (CL3) and ACE2. Cluster of differentiation 147 (CD147) is another host cell route that can be explored for possible pharmacological treatments (Suo et al., 2016).
Chinese medicine is playing a vital role in the global fight against COVID-19, and the demand for Chinese medicine has increased substantially (Zhang et al., 2020). Chinese medicine has resisted many large-scale epidemics in Chinese history and has continuously introduced the achievements of modern scientific development. Now that China is helping overseas to fight the pandemic, it is an excellent opportunity to promote Chinese medicine to the world.
Author contributions
ZYZ and YDL designed the review and jointly wrote the paper. LYZ, XTZ, and BWX collected and analyzed literature and made charts. WJZ coordinated and and jointly wrote and revised the paper. JHS put forward core opinions and suggestions. All authors read and approved the manuscript.
Funding
This work was funded by Key project at central government level: The ability establishment of sustainable use for valuable Chinese medicine resources, grant no. [2060302].
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
The authors thank the patients who participated in these interviews.
References
- Ali M.R., Seo J., Lee D., Kim Y. Teratocyte-secreting proteins of an endoparasitoid wasp, Cotesia plutellae, prevent host metamorphosis by altering endocrine signals. Compar. Biochem. Physiol. Part A. 2013;166:251–262. doi: 10.1016/j.cbpa.2013.06.028. [DOI] [PubMed] [Google Scholar]
- Ang L., Lee H.W., Choi J.Y., Zhang J., Lee M.S. Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Integr. Med. Res. 2020 doi: 10.1016/j.imr.2020.100407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angenent G.C., Linthorst H.J., van Belkum A.F., Cornelissen B.J., Bol J.F. RNA 2 of tobacco rattle virus strain TCM encodes an unexpected gene. Nucl. Acids Res. 1986;14:4673–4682. doi: 10.1093/nar/14.11.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai Q.Z., Wang B., Jin D.C., Zhang S.Y., He X.Y., Yang N., Gou Y.J. Progress in the diagnosis and treatment of novel coronavirus pneumonia by traditional Chinese medicine. J. Xi’an Jiaotong Univ. (Med. Sci.) 2020 http://kns.cnki.net/kcms/detail/61.1399.R.20200306.1635.004.html.26 [Google Scholar]
- Bao L., Shi Y.J., Geng Z.H., Sun J., Zhao R.H., Du C.Q., Chu Y.J., Cui X.L. Application of reyanning mixture in evaluating combining disease with syndrome of human coronavirus pneumonia with pestilence attacking lung syndrome. China J. Chin. Materia Medica. 2020;0303:401. doi: 10.19540/j.cnki.cjcmm.2020. [DOI] [PubMed] [Google Scholar]
- Cao B., Wang Y.M., Wen D.N., Liu M., Wang J.L., Fan G.H., Ruan L.G., Song B., Cai Y.P., Wei M., Li X.W., Xia J.A. A Trial of lopinavir–ritonavir in adults hospitalized with severe covid-19. New Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001282. 10.1056/NEJMoa200 1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai X., Hu L., Zhang Y., Han W., Lu Z., Ke A., Zhou J., Shi G., Fang N., Fan J. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv. 2020 doi: 10.1101/2020.02.03.931766. [DOI] [Google Scholar]
- Chen R., Luo Y.P., Xu X.H., Miao Q., Wang Y.G. Preliminary exploration of TCM syndrome and analysis of typical cases based on 52 cases of new coronavirus pneumonia in wuhan. J. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.2166.R.20200220.1443.002.html [Google Scholar]
- Cui J., Li F., Shi Z.L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng, Y.J., Liu, B.W., He, Y.X., Liu, T., Zheng, R.L., Yang, A.D., Huang, A., Li, Y.T., Xu, Y.L., 2020. Exploring the active compounds of huoxiangzhengqi oral liquid for prevention of new coronavirus pneumonia (COVID-19) based on network pharmacology and molecular docking method. Chin. Herbal Med. http://kns.cnki.net/kcms/detail/12.1108.R.20200224.2202.002.html.
- Ding R.C., Wang F., Lu H., Liu L., Wang P. Diagnosis and treatment of COVID-19 from spleen and stomach. Acta Chin. Med. 2020:7. doi: 10.1056/NEJMoa200101. http://kns.cnki.net/kcms/detail/41.1411.R.20200303.1218.002.html [DOI] [Google Scholar]
- Fan F.Y., Fan X.R., Wang Y.Z., Jin Z.H., Zhao S.L., Wang W., Yao L.S., Liu Y.J., Tian Y., Liu D., Ge Z.J., Xu Q., Min R. Traditional Chinese medicine characteristics of pneumonia infected by new coronavirus in hunan province and prevention. J. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.2166.r.20200206.1256.004.html [Google Scholar]
- Feng X., Duan X.J., Zhang B., Sarina Su, X.F. Ma, S.Y. Li, Y. Guo. Analysis of programs and guidelines on traditional chinese medicine (TCM) for COVID-19 to provide suggestions for future development of tcm clinical practice guidelines. Chin. J. Exp. Traditional Med. Formulae. 2020 doi: 10.13422/j.cnki.syfjx.20200841. [DOI] [Google Scholar]
- Fu Q., Zhang X.Y., Li S.W. Risk management strategies for occupational exposure of medical staff with nove lcoronavirus infections. Chin. J. Nosocomio. 2020;30(6):801–805. [Google Scholar]
- Gong X., Mou F.Z., Wei D.R., Dou L., Gong X.Y., Wang T., Hu X.S., Liu L., Wang N.N., Deng M.L. The clinical characteristics and medication analysis of Corona Virus Disease 2019. World Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.5529.R.20200309.1431.004.html [Google Scholar]
- Han B., Ding R.C., Li X., Wang P., Li Z.H. Discussion on COVID-19 treatment based on Wenyi Lun. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200306.1003.002.html [Google Scholar]
- Hopkins A.L. Network pharmacology: the next paradigm in drug discovery. Nat. Chem. Biol. 2008;4(11):682. doi: 10.1038/nchembio.118. [DOI] [PubMed] [Google Scholar]
- Huang H.Y., Xiao W.M., Wang Y.Y., Cai H.K., Chen J., Tan H.Y. Analysis report on traditional chinese medicine effectiveness in COVID-19 patients in hunan province. J. Hunan Univ. Chin. Med. 2020 http://kns.cnki.net/kcms/detail/43.1472.R.20200302.0905.002.html [Google Scholar]
- Huo Z.P., Liu Y.X., Hao L., Wang Y., He Y., Zhou W.P., Yan K.J. Research progress on potential application of Huoxiang Zhengqi in prevention and treatment of coronavirus disease 2019. Drugs Clin. 2020;35(3):1–6. [Google Scholar]
- Jin R., Kong L.W., Yan D. Consensus on the safe and rational use of early intervention Chinese patent medicines in the novel corona-virus pneumonia (COVID-19) (Beijing) Chin. J. Hosp. Pharm. 2020 http://kns.cnki.net/kcms/detail/42.1204.R.20200227.2054.004.html [Google Scholar]
- Li J.S., Zhang H.L., Chen Y.L. Expert consensus on rehabilitation of chinese medicine for COVID-19 (First Edition) Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200306.1315.006.html [Google Scholar]
- Li K., Qiu R.L. TCM prevention measures of novel coronavirus pneumonia based on the “natural factor” and the “human factor”. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200219.0957.005.html [Google Scholar]
- Li X.F., Du W.X. Some thoughts on pneumonia caused by new coronavirus infection based on theory of five yun and six qi. Chin. Arch. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/21.1546.R.20200206.1811.002.html [Google Scholar]
- Liang A.J., Ling Y., Liu H.Z. Application of traditional Chinese medicine in the prevention and treatment of infectious atypical pneumonia (SARS) Pharm. J. Chin. PLA. 2003;19(5):367–369. [Google Scholar]
- Lin S.Y., Zhang Y.C., Wei Y.Z., Lin G.H. Exploration of fire-needle therapy on corona virus disease 2019. Chin. Acupuncture Moxibustion. 2020 doi: 10.13703/j.0255-2930.20200223-k0007. [DOI] [PubMed] [Google Scholar]
- Lin Z.J., Zhang B. Strategy of pharmaceutical care services for clinical Chinese pharmacists in novel coronavirus pneumonia. China J. Chin. Materia Medica. 2020 doi: 10.19540/j.cnki.cjcmm.20200211.501. [DOI] [PubMed] [Google Scholar]
- Liu H.N. A Rational Analysis of Traditional Chinese Medicine for SARS. China Pharm. 2003;4(7):82. [Google Scholar]
- Liu K.P., Guan D.D., Li L., Ni H., Chen L. Feasibility analysis of moxibustion whole process intervention in the prevention and treatment of COVID-19. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200306.1528.008.html [Google Scholar]
- Liu M., Wang Q.G. The contribution and reflection of traditional Chinese medicine in the prevention and treatment of SARS. Chin. J. New Drug. 2004;13(S1):1209–1211. [Google Scholar]
- Luo Y., Wang C.Z., Hesse-Fong J., Lin J.G., Yuan C.S. Application of Chinese medicine in acute and critical medical conditions. Am. J. Chin. Med. 2019;47(6):1223–1235. doi: 10.1142/S0192415X19500629. [DOI] [PubMed] [Google Scholar]
- Ma J.J., Chen M., Wang Y.G. New type of coronavirus (2019-ncov) syndrome: a review of TCM syndromes. Beijing J. Trad. Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.5635.R.20200207.1616.002.html [Google Scholar]
- Ni L.Q., Tao H.W., Yang X.L., Zhang J., Ni X.J. Analysis and strategy on prevention plan of corona virus disease 2019 by traditional chinese medicine. Chin. Arch. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/21.1546.R.20200305.0914.002.html [Google Scholar]
- Pang W.T., Jin X.Y., Pang B., Yang F.W., Wang H., Liu C.X., Zheng W.K., Zhang J.H. Analysis on pattern of prescriptions and syndromes of traditional Chinese medicine for prevention and treatment of novel coronavirus pneumonia. China J. Chin. Materia Medica. 2020;20200218:502. doi: 10.19540/j.cnki.cjcmm. [DOI] [PubMed] [Google Scholar]
- Ran, J., Li, Y.P., Li, Q.T., 2020. Study of TCM syndrome in 209 novel coronavirus pneumonia cases of chongqing in 2020. 29(5),753-755.
- Shao C.C., Wang H.J., Meng P.F., Ma X.X., Ding X., Wei Z., Chen G.Z., Zhang S.X., Xu L.R. Analysis of TCM Understanding and Treatment Status of COVID-19. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200309.1435.002.html [Google Scholar]
- Sun L.M., Chen J.S., Xue Y.X. Thought on COVID-19 in traditional Chinese medicine by TCM Master XUE Bo-Shou. World J. Integr. Traditional Western Med. 2020:1–10. http://kns.cnki.net/kcms/detail/11.5511.R.20200304.1800.002.html [Google Scholar]
- Wang K., Chen W., Zhou Y.S. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv. 2020 doi: 10.1038/s41392-020-00426-x. https://www.biorxiv.org/content/10.1101/2020.03.14.988345v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen P.P., Zhang S.S. Combination with “Wenzhou Epidemic” on prevention and treatment of new coronavirus pneumonia from spleen and stomach. Beijing Traditional Chin. Med. 2020;09:1529. http://kns.cnki.net/kcms/detail/11.5635.R.202003.004.html [Google Scholar]
- Xia Y.J., Huang Y.H. A brief discussion on COVID-19 based on the theory of exterior and interior relationship between lung and large intestine. Inf. Traditional Chin. Med. 2020;224:1103. http://kns.cnki.net/kcms/detail/23.1194.R.20200002.html [Google Scholar]
- Xian N.X., Zhang Z., Li N., Liu N. Study on treatment from heart for severe patients based on etiology and pathogenesis transmission of Corona Virus Disease 2019. Chin. Arch. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/21.1546.R.20200304.2151.004.html [Google Scholar]
- Xiang Q., Mo Z.B., Song E.F. Traditional chinese medicine theory and clinical study on novel coronavirus pneumonia infection. Herald Med. 2020 http://kns.cnki.net/kcms/detail/42.1293.R.20200212.2049.002.html [Google Scholar]
- Xiao D.S., Fang H., Yang J.Z. Some principles in TCM For the patients with severe pneumonia induced by novel coronavirus (2019-nCoV) Clin. J. Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.5895.R.20200220.0747.004.html [Google Scholar]
- Xie Y., Wang J.J., Zhao H.L., Li S.Y., Li J.S. Expert questionnaire analysis of tcm syndrome differentiation standard for COVID-19 based on delphi method. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200303.1454.005.html [Google Scholar]
- Xu D.Y., Xu Y.L., Wang Z.W., Lu Y.L., Zhu H.L., Song T. Mechanism of qingfeipaidu decoction on COVID-19 based on network pharmacology. Pharmacol. Clin. Chin. Materia Medica. 2020 doi: 10.13412/j.cnki.zyyl.20200305.001. [DOI] [Google Scholar]
- Xue Y., Zhang W., Xu G.H., Chen X.R., Lu Y.F., Wang Z.W., Shi K.H., Wu H., Yu J. Dampness disease is a disease, clear and easy to understand——Traditional Chinese medicine clinical analysis of new type of coronavirus pneumonia in Shanghai. Shanghai J. Traditional Chin. Med. 2020 doi: 10.16305/j.1007-1334.2020.03.005. [DOI] [Google Scholar]
- Yang C., Yuan L., Liu C.Y., Shi J.H., Wang P., Luo M.H. Rational use and pharmaceutical care of Chinese patent medicines based on diagnosis and treatment plan for Corona Virus Disease 2019. J. Jinan Univ. (Nat. Sci. Med. Ed.) 2020 http://kns.cnki.net/kcms/detail/44.1282.N.20200302.1234.002.html [Google Scholar]
- Yang W., Yu C.H. Analysis and discussion on the prevention and treatment of new pneumonia based on the theory of “Five Movements and Six Qi”. Chin. J. Basic Med. Traditional Chin. Med. 2020;0849:002. http://kns.cnki.net/kcms/detail/11.3554.r.20200207html [Google Scholar]
- Yao W.F., Zhai Y.Y., Lin L.L., Yang B., Zhuang L., Zhang L., Xie T., Zhao X., Shan J.J., Wang S.C. Preliminary study on active ingredients of qingfei oral liquid combining “composition-target-common pathway” network and molecular docking technology against new coronavirus pneumonia. Nanjing J. Univ. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/32.1247.R.20200225.1351.002.html [Google Scholar]
- Yu M.K., Chai Q.Y., Liang C.H., Ding Y.Q., Lin Z.Y., Gao J.Q., Wang H., Zhang L.S., Liu J.P., Fei Y.T. An analyze of the traditional Chinese medicine prevention and treatment interventions for COVID-19. J. Traditional Chin. Med. 2020;61(5):383–387. [Google Scholar]
- Zhang C.L., Li B., Li J.G., Zou S.S., Dong Z.X., Wang X.T. Syndrome differentiation and treatment of COVID-19 based on wenbing theory in chinese medicine. Acta Chin. Med. 2020 http://kns.cnki.net/kcms/detail/41.1411.R.20200225.1505.006.html [Google Scholar]
- Zhang Z.C., Su M., Wu Q.Z. Observation on the application of traditional Chinese medicine “sachet” in prevention of atypical pneumonia. Neimenggu J. Traditional Chin. Med. 2003;21(4):17–18. [Google Scholar]
- Zhao D.K., Cai H.Y., Luo W., Huang Y.X., Ma Y., Chen Y.Y., Gong X.Y. One case of COVID-19 in Changchun treated by integrated Traditional Chinese and Western Medicin. Jilin J. Chin. Med. 2020 doi: 10.13463/j.cnki.jlzyy.2020.05.001. [DOI] [Google Scholar]
- Zhao J., Lv C., Wu Q., Zeng H., Guo X., Yang J., Tian S., Zhang W. Computational systems pharmacology reveals an antiplatelet and neuroprotective mechanism of Deng-Zhan-Xi-Xin injection in the treatment of ischemic stroke. Pharmacol. Rese. 2019;147 doi: 10.1016/j.phrs.2019.104365. [DOI] [PubMed] [Google Scholar]
- Zheng W.K., Zhang J.H., Yang F.W., Huang M., Miao Q., Qi W.S., Wang Y.G., Liu Q.Q., Zhang B.L. Treating respiratory diseases infected by new coronavirus from the wet poison epidemic. J. Traditional Chin. Med. 2020 http://kns.cnki.net/kcms/detail/11.2166.R.20200304.1405.006.html [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R. A novel coronavirus from patients with pneumonia in China. New Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zong Y., Ding M.L., Jia K.K., Ma S.T., Ju W.Z. Exploring the active compounds of Da-Yuan-Yin in treatment of novel coronavirus (2019-nCoV) pneumonia based on network pharmacology and molecular docking method. Chin. Traditional Herbal Drugs. 2020 http://kns.cnki.net/kcms/detail/12.1108.r.20200209.1038.002.html [Google Scholar]