Abstract
Background
Gait and mobility aid assessments are important components of rehabilitation. Given the increasing use of telehealth to meet rehabilitation needs, it is important to examine the feasibility of such assessments within the constraints of telerehabilitation.
Objective
The objective of this study was to examine the reliability and validity of the Tinetti Performance-Oriented Mobility Assessment gait scale (POMA-G) and cane height assessment under various video and transmission settings to demonstrate the feasibility of teleassessment.
Design
This repeated-measures study compared the test performances of in-person, slow motion (SM) review, and normal-speed (NS) video ratings at various fixed frame rates (8, 15, and 30 frames per second) and bandwidth (128, 384, and 768 kB/s) configurations.
Methods
Overall bias, validity, and interrater reliability were assessed for in-person, SM video, and NS video ratings, with SM video rating as the gold standard, as well as for different frame rate and bandwidth configurations within NS videos.
Results
There was moderate to good interrater reliability for the POMA-G (intraclass correlation coefficient [ICC] = 0.66–0.77 across all configurations) and moderate validity for in-person (β = 0.62; 95% confidence interval [CI] = 0.37–0.87) and NS video (β = 0.74; 95% CI = 0.67–0.80) ratings compared with the SM video rating. For cane height, interrater reliability was good (ICC = 0.66–0.77), although it was significantly lower at the lowest frame rate (8 frames per second) (ICC = 0.66; 95% CI = 0.54–0.76) and bandwidth (128 kB/s) (ICC = 0.69; 95% CI = 0.57–0.78) configurations. Validity for cane height was good for both in-person (β = 0.80; 95% CI = 0.62–0.98) and NS video (β = 0.86; 95% CI = 0.81–0.90) ratings compared with SM video rating.
Limitations
Some lower frame rate and bandwidth configurations may limit the reliability of remote cane height assessments.
Conclusions
Teleassessment for POMA-G and cane height using typically available internet and video quality is feasible, valid, and reliable.
Restoration of gait and mobility functions is an important aim in rehabilitation as it contributes towards making an individual functionally independent. Individuals who regain mobility experience improve quality of life and lower risk of downstream complications compared with individuals with lower mobility. Therefore, accurate assessment of gait and mobility performance and fitting of mobility aids are integral components of most rehabilitation interventions.
Although formal gait analysis using motion-capture systems is the gold standard for evaluating gait and mobility performance, such analysis is expensive and requires a specialized laboratory setup that may not be feasible or practicable for clinical or home settings. Several simpler gait performance assessment scales have therefore been developed to meet clinical needs in rehabilitation care. Of these, one of the most commonly used is the Tinetti Performance-Oriented Mobility Assessment (POMA) gait scale (POMA-G), developed in 1986, to reliably assess gait functions in older adults with minimal equipment and training, along with a corresponding balance scale.1 The POMA-G tests both gross motor coordination and awareness of spatial relationships during movement and is one of the few qualitative rather than timed measures of gait. The POMA has been used extensively in studies in older populations2,3 and also in other diseases, such as Parkinson’s disease, stroke, and orthopedic conditions.4,5
Canes are one of the most common walking aids prescribed for people with ambulation impairments to improve gait safety and reduce falling. Therapists routinely adjust mobility aids relative to the patient’s height to optimize body mechanics and ensure that the patient’s center of gravity remains over their base of support when using the mobility device. Ideally, cane height should be measured from the floor to the distal wrist crease.6 Fitting cane height therefore also requires accurate assessment of spatial relationships.
Traditional practice requires the in-person assessment of gait and fitting of mobility aid in the clinic setting.4,7 However, rehabilitation services are increasingly offered remotely to meet the needs of persons living in remote locations, enable greater efficiency in provision of health care services, and overcome manpower resource constraints.8–10 Such telerehabilitation interventions have been demonstrated to achieve outcomes as good as or better than traditional rehabilitation interventions in patients with stroke or other neurological and orthopedic conditions.11–13 However, even in these telerehabilitation setups, the bulk of gait and mobility assessment still occurs face to face, in part because providers may lack confidence in the reliability and validity of such assessments using video technology.14
In recent years, there have been efforts to develop teleassessment technologies for remote assessment of functional tests, such as the Six-Meter Walk Test, Timed “Up & Go” Test, Five Times Sit-to-Stand Test, and Balance and Forward Reach Test.15–18 However, these attempts have used additional equipment like accelerometers,15,18 inclinometers,17 specially designed sensors,16 and computer systems with specialized software.15–18 In addition, these previous initiatives have involved synchronous data transmission, where data are transferred in real-time between devices, allowing for 2-way communication. Although synchronous transmission allows for fast and efficient data transfers, it is expensive and requires reliable high-speed internet connectivity. The requirements for high-end technology and high-speed internet connections hinder the reach of teleassessment and telerehabilitation to remote rural communities that need these services the most and where technological infrastructure available for telehealth is limited.19,20 Therefore, it is important to examine the feasibility, reliability, and validity of administering and evaluating commonly used tests like POMA-G and cane height assessment within the constraints of the usual telerehabilitation setups, which typically have low bandwidth and internet speed connections. Synchronous transmission of large amounts of data may not be feasible with such set ups, and asynchronous transmission, where data are first stored locally and subsequently forwarded to the receiving device, may be preferred. Figure 1 depicts these 2 different modes of transmission as they might occur using standard Veterans Affairs (VA) telehealth technology.
Figure 1.
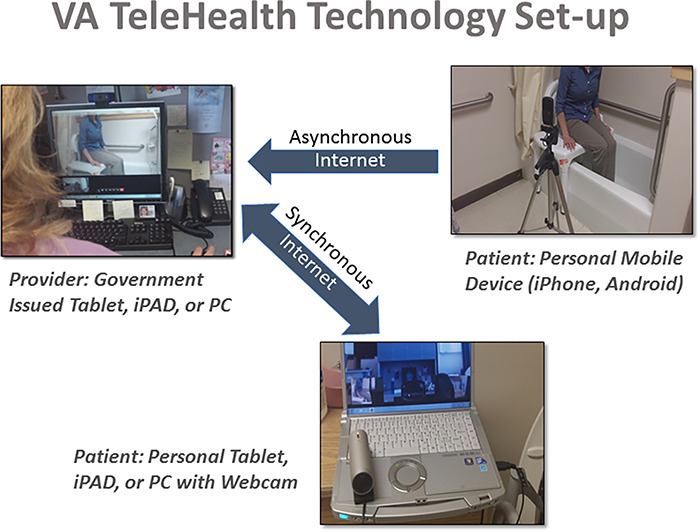
Veterans Affairs TeleHealth Technology setup.
We previously reported that the loss of resolution and reduction in number of frames transmitted per minute because of low bandwidth conditions resulted in the reduction of test validity and reliability when assessing gross and fine motor movements.21–23 Therefore, in this study, we also examined the reliability and validity of standardized observational gait evaluation (POMA-G) and cane height assessment under various asynchronous video and transmission settings to assess their feasibility for use in remote teleassessment. If these tests can be shown to be reliable and valid under a range of video and transmission settings, the rehabilitation community would be enabled to conduct such assessments remotely, using either asynchronous (ie, store and forward videos) or synchronous (ie, live 2-way video) methods for telerehabilitation.
Methods
This evaluation was part of a larger study examining the effects of video and camera characteristics on the performance of various motor, gait, and balance assessment tests. It was designed as a repeated-measures study comparing physical performance under various configurations of bandwidth and frame rate. Details of the study methodology have been published previously.21,23 In brief, study participants were veterans being treated at the occupational/physical therapy, neurology, and rheumatology clinics of the Durham VA Medical Center. Veterans who used a cane/orthosis/prosthesis at least once per week for walking and scored 6 of 10 or higher on the Short Portable Mental Status Questionnaire24 were eligible to participate. Veterans who required human aid to ambulate 3 m (10 ft) or more, to rise from a sitting position to a standing position, or to stand for 10 seconds or more, were excluded, as were those unable to provide informed consent. From a total of 360 potential participants screened, 184 did not meet the eligibility criteria, and 100 declined participation. Of the 76 participants enrolled, data on cane height were available for 1 or more comparisons for 48 participants (Fig. 2); fewer data on the POMA-G were available because of the inability of 2 participants to complete the POMA-G. Sample size was further reduced for POMA-G validity measures because of missing data on in-person ratings for 4 participants, yielding a sample size of 42 for those comparisons.
Figure 2.
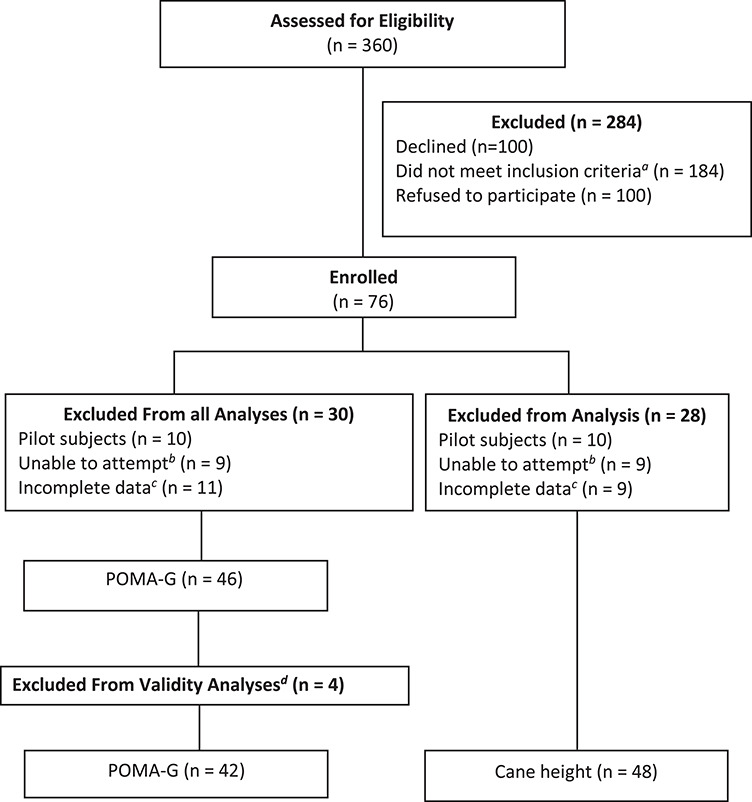
Flowchart for study participants. POMA-G = Tinetti Performance Oriented Mobility Assessment gait scale. aUsed a cane/orthosis/prosthesis at least once per week for walking and scored 6/10 or higher on the Short Portable Mental Status Questionnaire. bParticipants were excluded if they were unable to (1) ambulate 10 feet without assistance from another person, (2) rise from sit to stand, or (3) stand for 30 s or more. cParticipants were excluded due to incomplete video recordings, equipment failure, or missing data. dParticipants were excluded from validity analysis due to missing in-person rating.
A much greater proportion of ratings based on a single view (lateral or frontal) was deemed “unable to be rated” than for the final rating based on both frontal and lateral views (1.4% when both views were used vs 16.2% for frontal only and 14.5% for lateral only; P < .05). Therefore, all comparisons for the POMA-G used the overall rating (ie, the final rating based on both frontal and lateral views). All comparisons for cane height were also based on the overall rating, as separate frontal and lateral ratings were not obtained, based on prior research.22
Ethics approval was obtained from the Institutional Review Board at Durham VA Medical Center prior to study initiation, and informed consent was obtained from all participants before enrollment.
Tinetti Performance-Oriented Mobility Assessment Gait Scale
The POMA-G is a 7-item scale requiring only a chair, a stopwatch, and an approximately 4.6-m (15 feet) walkway for administration. The POMA has been shown to have high interrater reliability,25,26 even across raters with various levels of experience and training.27 The POMA-G also has excellent interrater and test-retest reliability28–30 and correlates well with measured gait velocity.31,32
Cane Height
Canes for walking and gait support are usually used on the side opposite to the weak leg. In this study, we used a quad (4-point) cane to examine the reliability and validity of video assessment of cane height. First, the in-person rater measured the optimum cane height with the person standing straight and arms dangling freely at the side. Participants were firmly secured with a gait belt prior to standing. Optimum cane height was measured from the floor to the ulnar styloid process. Then, the cane was adjusted according to randomly assigned predetermined settings (± 0, approximately 2.5, or approximately 5 cm [± 0, 1, or 2 inches] relative to the predetermined optimal height), and the participant was videographed in frontal and lateral views with the arm dangling beside the adjusted cane as well as gripping the cane. This process was repeated for a total of 5 test heights per participant.
Rating Procedures, Rater Training, and Protocol
All ratings were done using standard VA equipment widely available for televideo visits (ie, desktop personal computers) (Fig. 1). Videos were edited by study staff according to various parameters, and raters viewed assigned edited videos. Only the raters allowed to rate via slow motion (SM) were allowed to replay the videos with SM.
Fourteen raters assessed participant performance on the POMA-G and the cane height test in 1 of the 8 configurations detailed below. All raters were Durham VA Medical Center staff and included 8 physical therapists, 4 occupational therapists, 1 physical therapist assistant, and 1 experienced rehabilitation research assistant. To ensure consistent rating, all raters were formally trained using training videos and manuals. All raters had to achieve acceptable scores in rating a final test video to be deemed as a certified rater.
The same rater performed all in-person ratings. Two expert raters reviewed and rated the optional slow-motion videos, deemed the criterion gold standard for this analysis. Raters were randomized across all other configurations and across participants, with each configuration being rated by 2 raters. Each rater rated videos on a 1-time viewing of the videos and without assistance. Frontal and lateral views were rated separately and then combined to give the rater’s overall rating for the POMA-G. For cane height, raters provided only an overall rating for each configuration and participant.
Test Administration, Video Recording, and Editing
A trained research assistant guided participants through each item of the POMA-G and the cane height test. Participant performance was captured in both frontal and lateral views by a Panasonic HD-SD40K camera (Panasonic, Osaka, Japan), positioned approximately 3.6 m (12 feet) away at a height of approximately 1 m (42.6 in) at maximum zoom-out. The POMA-G and cane height were rated simultaneously by the in-person rater and video recorded. Both tests were administered in designated clinic spaces within Durham VA Medical Center.
Final Cut Pro software on an iMac desktop (both from Apple, Cupertino, CA, USA) was used to edit videos and remove irrelevant footage from the raw videos. Next, the frame rate, bandwidth, or both were manipulated using Apple Compressor software (Apple, Cupertino, CA, USA) to achieve the 8 configurations. Each configuration maintained the size and aspect ratio of the original video.
Test Rating
Raters assessed participant performance on the POMA-G and the cane height test in 1 of the following 8 configurations: in-person rating; optional SM review with a fixed bandwidth (768 kB/s) and a fixed frame rate (30 frames per second, ie, the highest definition video); variable frame rates (8, 15, and 30 frames per second) with a fixed bandwidth (768 kB/s) and normal speed (NS) viewing only; and variable bandwidths (128, 384, and 768 kB/s) with a fixed frame rate (30 frames per second) and NS viewing only.
Statistical Methods
A sample size of 39 was deemed adequate to test the hypothesis that the intraclass correlation coefficient (ICC) and the validity coefficient in our sample would be >0.60 and >0.39, respectively, with 80% power.33 Overall bias, validity, and interrater reliability were assessed for in-person, SM video, and NS video ratings at all configurations as well as for the different frame rate and bandwidth configurations within NS videos. Overall bias (mean difference between test and criterion configurations) was assessed by regressing the criterion score on each test score while controlling for rater-related variance as a random effect. Standardized regression coefficients were calculated to obtain “validity coefficients” for each test configuration in relation to the criterion configuration.34 SAS PROC MIXED35 was used for bias and validity analysis.
ICCs for interrater reliability were calculated using SAS PROC VARCOMP35 based on the methods described by Streiner and Norman,36 again while controlling for rater asa random effect. Reliability and criterion estimates of <0.5, 0.5 to 0.75, 0.75 to 0.9, and >0.9 were deemed poor, moderate, good, and excellent, respectively.37
Role of the Funding Source
This study was funded by grants from the Duke Older Americans Independence Center (NIA AG028716) and the Veterans Health Administration Rehabilitation Research and Development Service (RR&D F0900-R). The funders played no role in the design, conduct, or reporting of this study.
Results
Table 1 presents the characteristics of the 42 participants who underwent full assessment for the POMA-G, including in-person evaluation. Participants had a mean age of 60.79 years (SD = 12.25), and 80.9% (n = 40) were men. Arthritis was the most common medical condition among the participants, affecting 61.9% (n = 31), and two-thirds (69.0%; n = 29) had multiple medical conditions. The 2 participants who completed the cane height assessment but not the POMA-G were both men, 48 and 72 years old, with 1 comorbid condition each.
Table 1.
Characteristics of 42 Study Participants
| Characteristic | Value a |
|---|---|
| Age, y, mean (SD) | 60.79 (12.25) |
| Race | |
| White | 24 (57.1) |
| African American | 18 (42.9) |
| Sex | |
| Men | 34 (81.0) |
| Women | 8 (19.0) |
| Diagnosis | |
| Cardiac condition | 2 (4.8) |
| Neurological condition | 10 (23.8) |
| Arthritis | 26 (61.9) |
| Diabetes | 1 (2.4) |
| Cancer diagnosis | 3 (7.1) |
| Presence of ≥3 diagnoses | 29 (69.0) |
aValues are reported as numbers (percentages) of participants unless otherwise noted.
When compared with SM videos, there were no significant differences in the mean POMA-G scores obtained in person and using NS videos (Tab. 2). However, the mean in-person score on the POMA-G was significantly different from the NS video mean score (10.90 [SD = 1.68] vs 9.88 [SD = 2.27]; P = .004). Mean scores for the POMA-G did not vary significantly across the various frame rate and bandwidth configurations (Tab. 2). When comparing cane height assessments, there were no significant differences in the scores obtained in person and through SM and NS videos. There were also no significant differences across frame rates and bandwidths (Tab. 3).
Table 2.
Mean Differences, Reliability, and Validity of POMA-G Between Groups According to Viewing Method, Frame Rate, and Bandwidtha
| Category | No. of Video Ratings b | Mean Difference (SD) | Regression Results for Mean Differences Between Groups | |||
|---|---|---|---|---|---|---|
| Contrast | P | Interrater Reliability, ICC (95% CI) c | Criterion Validity (95% CI) d | |||
| Viewing method | ||||||
| IP | 42 | 10.90 (1.68) | IP vs NS | .004 | NAe | 0.62 (0.37–0.87) |
| SM | 84 | 10.30 (1.86) | IP vs SM | .14 | 0.68 (0.54–0.78) | NAf |
| NS | 436 | 9.88 (2.27) | NS vs SM | .11 | 0.66 (0.61–0.71) | 0.74 (0.67–0.80) |
| Frame rate (at bandwidth of 768 kB/s) (fps) | ||||||
| 30 | 89 | 9.75 (2.45) | 30 vs 8 | .26 | 0.66 (0.52–0.76) | 0.80 (0.63–0.98) |
| 15 | 89 | 10.07 (1.99) | 30 vs 15 | .58 | 0.67 (0.54–0.77) | 0.75 (0.61–0.90) |
| 8 | 86 | 10.13 (2.05) | 15 vs 8 | .33 | 0.77 (0.67–0.84) | 0.79 (0.66–0.93) |
| Bandwidth (at frame rate of 30 fps) (kB/s) | ||||||
| 768 | 86 | 10.13 (2.05) | 768 vs 128 | .27 | 0.77 (0.67–0.84) | 0.80 (0.63–0.98) |
| 384 | 87 | 9.70 (2.41) | 768 vs 384 | .22 | 0.69 (0.57–0.78) | 0.72 (0.58–0.87) |
| 128 | 85 | 9.74 (2.43) | 384 vs 128 | .91 | 0.66 (0.52–0.76) | 0.70 (0.53–0.87) |
aCI = confidence interval; fps = frames per second; ICC = intraclass correlation coefficient; IP = in person; POMA-G = Tinetti Performance-Oriented Mobility Assessment gait scale; NS = normal speed; SM = slow motion.
bNumber of video ratings available for the comparisons, varying according to the number of raters for any given parameter and missing values for that parameter (eg, in-person ratings and/or raters deeming a video “unable to be rated”).
cReliability was based on Streiner and Norman.36(p133) CIs were estimated using the Fisher z transformation.
dValidity was estimated using the standardized regression coefficient for the relationship between test and criterion measures.
eWith a single IP rating, interrater reliability could not be estimated.
fThe criterion group in validity analyses was SM.
Table 3.
Mean Differences, Reliability, and Validity of Cane Height According to Viewing Method, Frame Rate, and Bandwidtha
| Category | No. of Video Ratings b | Mean Difference (SD) | Regression Results for Mean Differences Between Groups | |||
|---|---|---|---|---|---|---|
| Contrast | P | Interrater Reliability, ICC (95% CI) c | Criterion Validity (95% CI) d | |||
| Viewing method | ||||||
| IP | 48 | 0.42 (3.28) | IP vs NS | .18 | NAe | 0.80 (0.62–0.98) |
| SM | 94 | 1.14 (3.83) | SM vs IP | .45 | 0.89 (0.85–0.93)f | NAg |
| NS | 443 | 1.53 (3.84) | NS vs SM | .54 | 0.80 (0.77–0.83)f | 0.86 (0.81–0.90) |
| Frame rate (at bandwidth of 768 kB/s) (fps) | ||||||
| 30 | 94 | 1.45 (3.85) | 30 vs 8 | .75 | 0.81 (0.73–0.87) | 0.86 (0.74–0.97) |
| 15 | 93 | 1.54 (3.84) | 30 vs 15 | .91 | 0.88 (0.83–0.92)h | 0.90 (0.84–0.97) |
| 8 | 97 | 1.26 (3.84) | 15 vs 8 | .67 | 0.66(0.54–0.76)h | 0.83 (0.74–0.92) |
| Bandwidth (at frame rate of 30 fps) (kB/s) | ||||||
| 768 | 94 | 1.45 (3.85) | 768 vs 128 | .42 | 0.81 (0.73–0.87) | 0.86 (0.74–0.97) |
| 384 | 80 | 1.53 (3.78) | 768 vs 384 | .89 | 0.89 (0.83–0.92)i | 0.84 (0.72–0.96) |
| 128 | 79 | 1.96 (3.97) | 384 vs 128 | .51 | 0.69 (0.57–0.78)i | 0.80 (0.67–0.93) |
aCI = confidence interval; fps = frames per second; ICC = intraclass correlation coefficient; IP = in person; NS = normal speed; SM = slow motion.
bNumber of video ratings available for the comparisons, varying according to the number of raters for any given parameter and missing values for that parameter (eg, in-person ratings and/or raters deeming a video “unable to be rated”).
cReliability was based on Streiner and Norman.36(p133) CIs were estimated using the Fisher z transformation.
dValidity was estimated using the standardized regression coefficient for the relationship between finger tap test and criterion measures.
eWith a single IP rating, interrater reliability could not be estimated.
fICCs were significantly different between SM and NS (CIs did not overlap).
gThe criterion group in validity analyses was SM.
hICCs were significantly different between frame rates of 15 and 8 fps (CIs did not overlap).
iICCs were significantly different between bandwidths of 384 and 128 kB/s (CIs did not overlap).
Interrater reliability for the POMA-G was similar for SM (ICC = 0.68; 95% CI = 0.54–0.78) and NS (ICC = 0.66; 95% CI = 0.61–0.71) videos, with moderate agreement between raters. ICCs for the various frame rate and bandwidth configurations were not significantly different, ranging from 0.66 to 0.77 (Tab. 2). Interrater reliability for cane height was good for SM (ICC = 0.89; 95% CI = 0.85–0.93) and NS (ICC = 0.80; 95% CI = 0.77–0.83) videos, although the ICC for SM video was significantly better. However, ICCs were significantly lower (nonoverlapping CIs) at the lowest frame rate (ICC = 0.66; 95% CI = 0.5–0.76) and bandwidth (ICC = 0.69; 95% CI = 0.57–0.78) configurations (Tab. 3).
Criterion validity for the POMA-G was moderate for NS videos (β = .74; 95% CI = 0.67–0.80) and slightly (but not significantly) lower for in-person rating (β = .62; 95% CI = 0.37–0.87) compared with gold standard SM videos. Validity coefficients for the frame rate and bandwidth configurations were similar, ranging from 0.70 to 0.80 (Tab. 2). Criterion validity for cane height was good for both NS (β = .80; 95% CI = 0.62–0.98) and SD (β = .86; 95% CI = 0.81–0.90) videos compared with in-person rating. There were also no significant differences in validity across frame rates and bandwidths for cane height (Tab. 3).
Discussion
POMA-G reliability and validity did not differ significantly between in-person and video rating, although total POMA-G scores were significantly lower for NS compared with in-person scores. POMA-G reliability and validity also did not vary significantly across the different bandwidth and frame rate configurations. Indeed, the test had acceptable validity and interrater reliability across all configurations. These data suggest that POMA-G can be validly and reliably assessed remotely using televideo. However, both lateral and frontal views were needed for accurate rating, with around one-sixth of videos unable to be rated when using a single view. For cane height, interrater reliability, but not validity, was significantly lower at the lowest frame rate and bandwidth configurations. This suggests that cane height assessment can be undertaken remotely with adequate validity and reliability so long as reasonable video quality can be assured.
We reported only moderate interrater reliability for remote assessment of the POMA-G, whereas previous reports suggested excellent interrater reliability on in-person administration.30 Because we found the ICCs to be similar across the various configurations, we hypothesize that the variability between raters arises from the subjective nature of the assessment of the POMA-G rather than any technological differences. Interrater reliability for cane height was good. Few studies have examined interrater reliability for assessing cane height. In our previous work, we found excellent interrater reliability in assessing cane height using a small sample of volunteers who were healthy.22 Our current work demonstrated good interrater reliability for cane height assessment in veterans as well. This finding is important as the reliability and validity of cane height assessment are meaningful only in the clinical context.
Several approaches have been tried in recent years for remote gait assessment. These include the use of wearable motion sensors and trackers, portable equipment for gait assessment, and modifying or testing existing gait assessment tools in telerehabilitation settings. Much of the work around motion sensors has been towards developing and validating measures reported through such sensors38–41 rather than technologies already used in standard clinical practice. Also, those novel protocols and measures are heterogeneous, and normative data to interpret results are lacking.42 In contrast, portable gait assessment systems have been developed commercially and offer the ease of portability with results comparable with gold standard motion analysis.43,44 Unfortunately, the cost of such systems limits their use on a larger scale in telerehabilitation. Disease-specific gait assessment systems have also been developed like a body sensor network-based automatic assessment of the Unified Parkinson Disease Rating Scale45 and a telemonitoring framework for remote assessment of gait recovery in stroke.16 However, none of these options offer the simplicity and ease of administration of video-based tele-technology to support use of measures already in widespread clinical use.
Gait aids can improve mobility and ambulation in patients with neurological, orthopedic, or other conditions that impair muscle strength, balance, and therefore mobility. The use of a quad cane, for example, can improve postural stability while standing and walking, reduce the force needed to switch between sitting and standing, and therefore increase functional capacity and mobility.46–48 However, many users report difficulties using gait aids, and incorrect usage can increase risk of falling.49 Therefore, correct fitting and training are crucial to functional benefit from these devises. To our knowledge, no study to date has examined remote assessment of cane height in patients. By establishing the validity and reliability of remotely assessed POMA-G and cane height, our study provides important new evidence to build teleassessment into telerehabilitation frameworks.
Our study demonstrates that mobility and cane height assessments for people can be conducted validly and reliably using a single fixed video camera and even at lower bandwidths and frame rates. These findings give physical therapists and other professionals in rehabilitation care, as well as patients, the flexibility to schedule such assessments remotely, allowing clinic visits to be more spaced out in time. In addition, the use of asynchronous “store and forward” technology eliminates the need for a therapist to be available in the remote assessing site when the test is conducted. This will facilitate more efficient use of the therapists’ clinical time.
The greatest strength of this study is its real-world context, examining a frequently used physical performance measure, the POMA-G, and a commonly used mobility assistive device, the quad cane, using available clinic space, the typical images that might be available (eg, single-lens camera), and transmission characteristics typical of the bandwidth available for teleassessment in many settings. These strengths also bring limitations with them. This study did not include high technology methods that might enhance accuracy of remote gait assessments (eg, use of Kinect [Microsoft, Redmond, WA, USA] technology50). Another important limitation was that, for purposes of comparability, the in-person rater was positioned immediately adjacent to the video camera and could not move about to gain a better view, as might occur in standard clinical care. Similarly, we did not allow for repetition that might be sometimes used by a clinician in the real world. Finally, we required raters to use their “best judgment” to decide that a given metric could not be rated. Although this differs from standard in-person clinical practice, the characteristics of how the video technology was used closely mimicked its use in clinical situations, making our findings relevant to clinical video-based telerehabilitation.
In summary, we have demonstrated the feasibility, validity, and reliability of conducting teleassessment to measure POMA-G and cane height using typically available internet and video quality. These findings can help to move more services to be delivered remotely, providing greater convenience to patients and greater service reach to health professionals and institutions.
Author Contributions
Concept/idea/research design: L.R. Landerman, K. Caves, H. Hoenig
Writing: K. Venkataraman, K. Caves, G.C. Koh, H. Hoenig
Data collection: K. Amis, K. Caves, H. Hoenig
Data analysis: K. Amis, L.R. Landerman, K. Caves, G.C. Koh, H. Hoenig
Project management: K. Caves, H. Hoenig
Fund procurement: H. Hoenig
Providing participants: H. Hoenig
Providing facilities/equipment: H. Hoenig
Consultation (including review of manuscript before submitting): K. Amis, G.C. Koh
Funding
This study was funded by grants from the Duke Older Americans Independence Center (NIA AG028716) and the Veterans Health Administration Rehabilitation Research and Development Service (RR&D F0900-R).
Ethics Approval
Ethics approval was obtained from the Institutional Review Board at Durham VA Medical Center prior to study initiation, and informed consent was obtained from all participants prior to enrollment.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. [DOI] [PubMed] [Google Scholar]
- 2. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Van Ness PH. A prehabilitation program for the prevention of functional decline: effect on higher-level physical function. Arch Phys Med Rehabil. 2004;85:1043–1049. [DOI] [PubMed] [Google Scholar]
- 3. Borowicz A, Zasadzka E, Gaczkowska A, Gawlowska O, Pawlaczyk M. Assessing gait and balance impairment in elderly residents of nursing homes. J Phys Ther Sci. 2016;28:2486–2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Llorens R, Noe E, Colomer C, Alcaniz M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96:418–425.e2. [DOI] [PubMed] [Google Scholar]
- 5. Martin-Martin LM, Arroyo-Morales M, Sanchez-Cruz JJ, Valenza-Demet G, Valenza MC, Jimenez-Moleon JJ. Factors influencing performance-oriented mobility after hip fracture. J Aging Health. 2015;27:827–842. [DOI] [PubMed] [Google Scholar]
- 6. Kumar R, Roe MC, Scremin OU. Methods for estimating the proper length of a cane. Arch Phys Med Rehabil. 1995;76:1173–1175. [DOI] [PubMed] [Google Scholar]
- 7. Housley SN, Garlow AR, Ducote K, et al. Increasing access to cost effective home-based rehabilitation for rural veteran stroke survivors. Austin J Cerebrovasc Dis Stroke. 2016;3:1–11. [PMC free article] [PubMed] [Google Scholar]
- 8. Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377:1585–1592. [DOI] [PubMed] [Google Scholar]
- 9. Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. 2017;4:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jesus TS, Landry MD, Dussault G, Fronteira I. Human resources for health (and rehabilitation): six rehab-workforce challenges for the century. Hum Resour Health. 2017;15:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27:2306–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang S, Xiang J, Gao X, Guo K, Liu B. The comparison of telerehabilitation and face-to-face rehabilitation after total knee arthroplasty: a systematic review and meta-analysis. J Telemed Telecare. 2018;24:257–262. [DOI] [PubMed] [Google Scholar]
- 13. Pastora-Bernal JM, Martin-Valero R, Baron-Lopez FJ, Estebanez-Perez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017;19:e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Veras M, Kairy D, Rogante M, Giacomozzi C, Saraiva S. Scoping review of outcome measures used in telerehabilitation and virtual reality for post-stroke rehabilitation. J Telemed Telecare. 2017;23:567–587. [DOI] [PubMed] [Google Scholar]
- 15. Jehn M, Prescher S, Koehler K, et al. Tele-accelerometry as a novel technique for assessing functional status in patients with heart failure: feasibility, reliability and patient safety. Int J Cardiol Heart Vasc. 2013;168:4723–4728. [DOI] [PubMed] [Google Scholar]
- 16. Jagos H, David V, Haller M, et al. A framework for (tele-) monitoring of the rehabilitation progress in stroke patients: eHealth 2015 special issue. Appl Clin Inform. 2015;6:757–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yozbatiran N, Harness ET, Le V, Luu D, Lopes CV, Cramer SC. A tele-assessment system for monitoring treatment effects in subjects with spinal cord injury. J Telemed Telecare. 2010;16:152–157. [DOI] [PubMed] [Google Scholar]
- 18. Rau CL, Chen YP, Lai JS, et al. Low-cost tele-assessment system for home-based evaluation of reaching ability following stroke. Telemed J E Health. 2013;19:973–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Edgar MC, Monsees S, Rhebergen J et al. Telerehabilitation in stroke recovery: a survey on access and willingness to use low-cost consumer technologies. Telemed J E Health. 2017;23:421–429. [DOI] [PubMed] [Google Scholar]
- 20. Sarfo FS, Adamu S, Awuah D, Sarfo-Kantanka O, Ovbiagele B. Potential role of tele-rehabilitation to address barriers to implementation of physical therapy among west African stroke survivors: a cross-sectional survey. J Neurol Sci. 2017;381:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Venkataraman K, Morgan M, Amis KA et al. Tele-assessment of the Berg Balance Scale. Effects of transmission characteristics. Arch Phys Med Rehabil. 2017;98:659–664.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hoenig H, Tate L, Dumbleton S et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94:998–1002. [DOI] [PubMed] [Google Scholar]
- 23. Hoenig HM, Amis K, Edmonds C, Morgan MS, Landerman L, Caves K. Testing fine motor coordination via telehealth: effects of video characteristics on reliability and validity. J Telemed Telecare. 2018;24:365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fillenbaum GG. Comparison of two brief tests of organic brain impairment, the MSQ and the short portable MSQ. J Am Geriatr Soc. 1980;28:381–384. [DOI] [PubMed] [Google Scholar]
- 25. Kegelmeyer DA, Kloos AD, Thomas KM, Kostyk SK. Reliability and validity of the Tinetti mobility test for individuals with Parkinson disease. Phys Ther. 2007;87:1369–1378. [DOI] [PubMed] [Google Scholar]
- 26. Thomas JI, Lane JV. A pilot study to explore the predictive validity of 4 measures of falls risk in frail elderly patients. Arch Phys Med Rehabil. 2005;86:1636–1640. [DOI] [PubMed] [Google Scholar]
- 27. Cipriany-Dacko LM, Innerst D, Johannsen J, Rude V. Interrater reliability of the Tinetti balance scores in novice and experienced physical therapy clinicians. Arch Phys Med Rehabil. 1997;78:1160–1164. [DOI] [PubMed] [Google Scholar]
- 28. Daly JJ, Roenigk K, Holcomb J, et al. A randomized controlled trial of functional neuromuscular stimulation in chronic stroke subjects. Stroke. 2006;37:172–178. [DOI] [PubMed] [Google Scholar]
- 29. Faber MJ, Bosscher RJ, Wieringen PC. Clinimetric properties of the performance-oriented mobility assessment. Phys Ther. 2006;86:944–954. [PubMed] [Google Scholar]
- 30. Behrman AL, Light KE, Miller GM. Sensitivity of the Tinetti gait assessment for detecting change in individuals with Parkinson's disease. Clin Rehabil. 2002;16:399–405. [DOI] [PubMed] [Google Scholar]
- 31. Canbek J, Fulk G, Nof L, Echternach J. Test-retest reliability and construct validity of the Tinetti performance-oriented mobility assessment in people with stroke. J Neurol Phys Ther. 2013;37:14–19. [DOI] [PubMed] [Google Scholar]
- 32. Shore WS, deLateur BJ, Kuhlemeier KV, Imteyaz H, Rose G, Williams MA. A comparison of gait assessment methods: Tinetti and GAITRite electronic walkway. J Am Geriatr Soc. 2005;53:2044–2045. [DOI] [PubMed] [Google Scholar]
- 33. Donner A, Eliasziw M. Sample size requirements for reliability studies. Stat Med. 1987;6:441–448. [DOI] [PubMed] [Google Scholar]
- 34. Spreen O, Strauss EA. Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 2nd ed. New York, NY, USA: Oxford University Press; 1998. [Google Scholar]
- 35. SAS Institute Inc. SAS STAT 9.2 User’s Guide. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- 36. Streiner D, Norman G. Health Measurement Scales: A Practical Guide to Their Development and Use. 3rd ed. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- 37. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ, USA: Prentice Hall; 2000. [Google Scholar]
- 38. Donath L, Faude O, Lichtenstein E, Pagenstert G, Nuesch C, Mundermann A. Mobile inertial sensor based gait analysis: validity and reliability of spatiotemporal gait characteristics in healthy seniors. Gait Posture. 2016;49:371–374. [DOI] [PubMed] [Google Scholar]
- 39. Macleod CA, Conway BA, Allan DB, Galen SS. Development and validation of a low-cost, portable and wireless gait assessment tool. Med Eng Phys. 2014;36:541–546. [DOI] [PubMed] [Google Scholar]
- 40. Kluge F, Gassner H, Hannink J, Pasluosta C, Klucken J, Eskofier BM. Towards mobile gait analysis: concurrent validity and test-retest reliability of an inertial measurement system for the assessment of spatio-temporal gait parameters. Sensors (Basel). 2017;17:E1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Byun S, Han JW, Kim TH, Kim KW. Test-retest reliability and concurrent validity of a single tri-axial accelerometer-based gait analysis in older adults with normal cognition. PloS One. 2016;11:e0158956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vienne A, Barrois RP, Buffat S, Ricard D, Vidal PP. Inertial sensors to assess gait quality in patients with neurological disorders: a systematic review of technical and analytical challenges. Front Psychol. 2017;8:817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture. 2003;17:68–74. [DOI] [PubMed] [Google Scholar]
- 44. Webster KE, Wittwer JE, Feller JA. Validity of the GAITRite walkway system for the measurement of averaged and individual step parameters of gait. Gait Posture. 2005;22:317–321. [DOI] [PubMed] [Google Scholar]
- 45. Parisi F, Ferrari G, Giuberti M, et al. Body-sensor-network-based kinematic characterization and comparative outlook of UPDRS scoring in leg agility, sit-to-stand, and gait tasks in Parkinson's disease. IEEE J Biomed Health Inform. 2015;19:1777–1793. [DOI] [PubMed] [Google Scholar]
- 46. Laufer Y. Effects of one-point and four-point canes on balance and weight distribution in patients with hemiparesis. Clin Rehabil. 2002;16:141–148. [DOI] [PubMed] [Google Scholar]
- 47. Laufer Y. The effect of walking aids on balance and weight-bearing patterns of patients with hemiparesis in various stance positions. Phys Ther. 2003;83:112–122. [PubMed] [Google Scholar]
- 48. Li TC, Tu KH, Shiue HS, Lin MR. Effects of cane use and position on performance of the sit-to-stand task in stroke patients. Am J Phys Med Rehabil. 2018;97:476–481. [DOI] [PubMed] [Google Scholar]
- 49. Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil. 2005;86:134–145. [DOI] [PubMed] [Google Scholar]
- 50. Tan KK, Narayanan AS, Koh CH, Caves K, Hoenig H. Extraction of spatial information for low-bandwidth telerehabilitation applications. J Rehab Res Dev. 2014;51:825–840. [DOI] [PubMed] [Google Scholar]


